Integrating care to reduce PUTZ Dr Teresa O



- Slides: 58

Integrating care to reduce PUTZ Dr. Teresa O Callaghan, Ph. D National Quality Improvement Division, HSE. 1
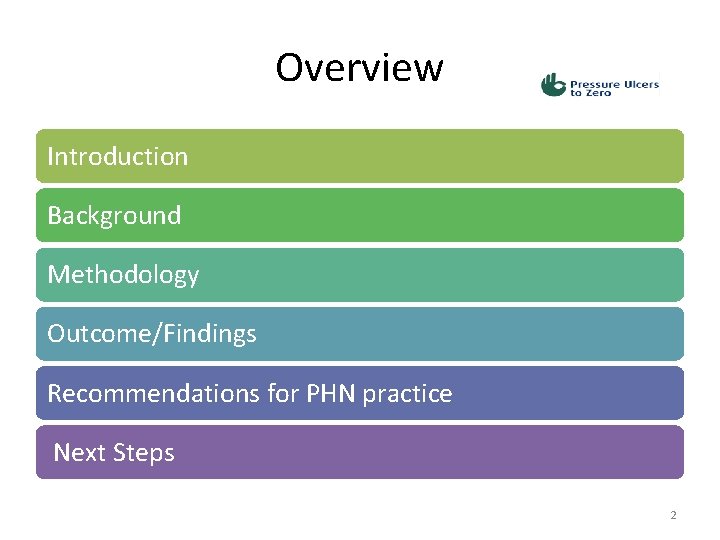
Overview Introduction Background Methodology Outcome/Findings Recommendations for PHN practice Next Steps 2
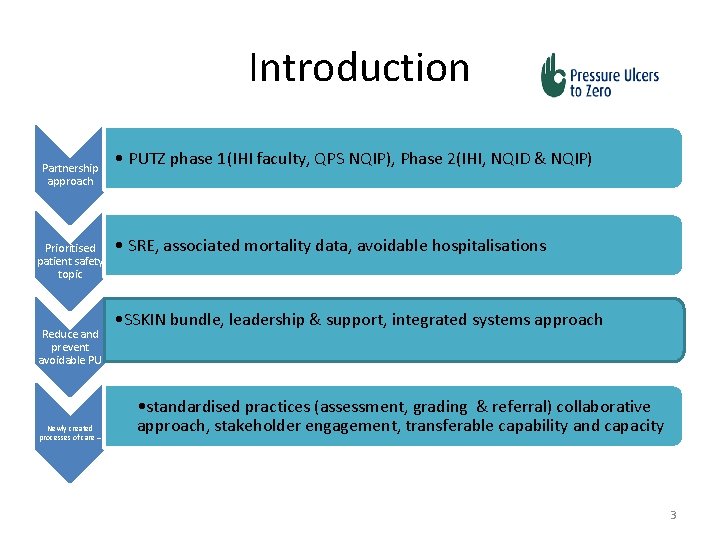
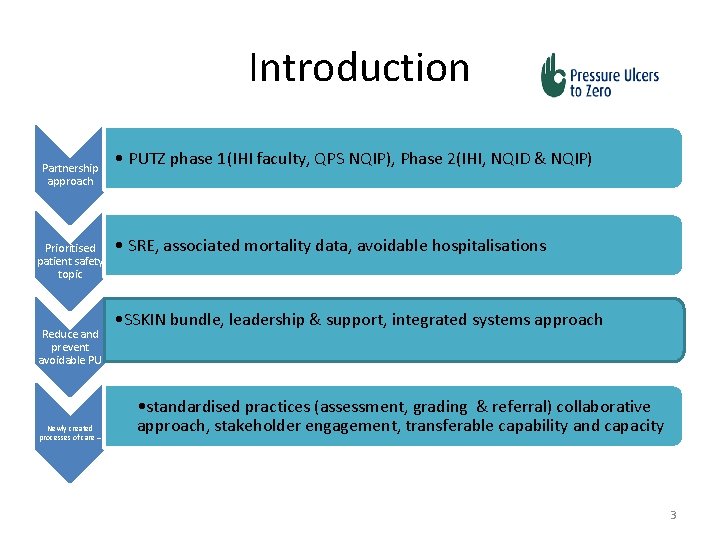
Introduction Partnership approach Prioritised patient safety topic Reduce and prevent avoidable PU Newly created processes of care – • PUTZ phase 1(IHI faculty, QPS NQIP), Phase 2(IHI, NQID & NQIP) • SRE, associated mortality data, avoidable hospitalisations • SSKIN bundle, leadership & support, integrated systems approach • standardised practices (assessment, grading & referral) collaborative approach, stakeholder engagement, transferable capability and capacity 3

Background 2014, First large scale collaborative in Irish health services - A partnership approach (QPS DNE, NQIP- all services and settings ) 2015, Second large scale collaborative (NQID& NQIP Ireland East HG, CHO 5, 7, 8, 9) 2016, Third large scale collaborative (NQID SSWHG & DMLHG) Pressure Ulcer = SRE Healthcare policy – integration of care 4
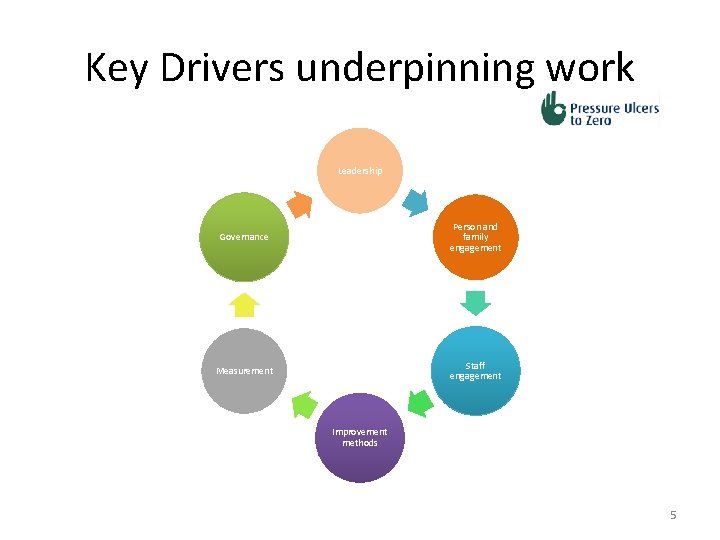
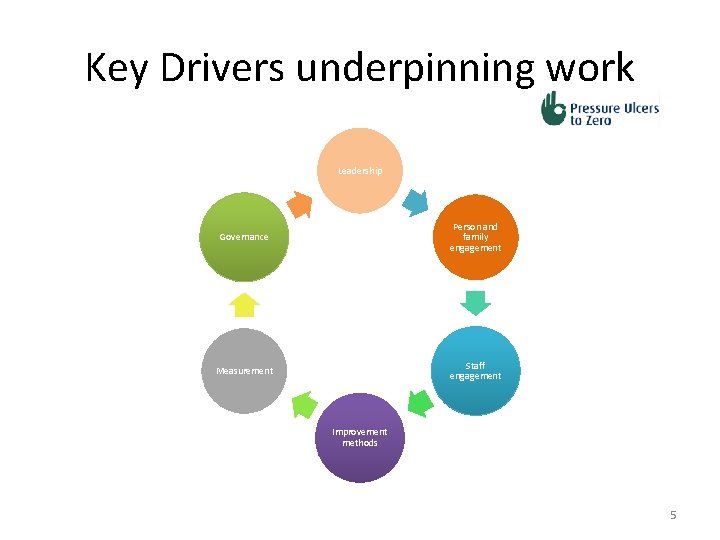
Key Drivers underpinning work Leadership Governance Person and family engagement Measurement Staff engagement Improvement methods 5
Quality Improvement in Healthcare • “Doing the right thing, at the right time, in the right way, for the right person and getting the best possible results”, and doing it in the right place! • www. ahrq. gov. . . 6
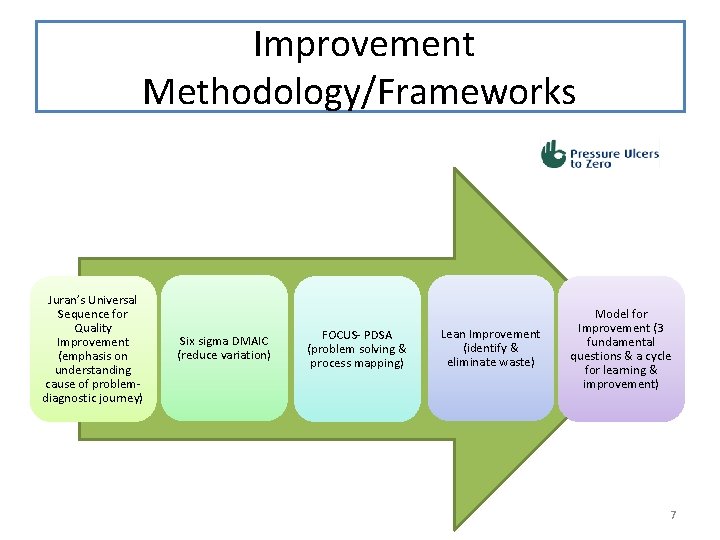
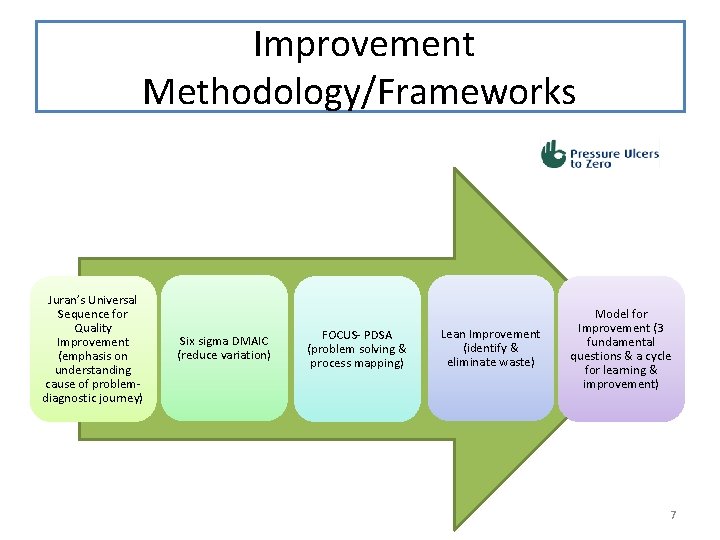
Improvement Methodology/Frameworks Juran’s Universal Sequence for Quality Improvement (emphasis on understanding cause of problemdiagnostic journey) Six sigma DMAIC (reduce variation) FOCUS- PDSA (problem solving & process mapping) Lean Improvement (identify & eliminate waste) Model for Improvement (3 fundamental questions & a cycle for learning & improvement) 7
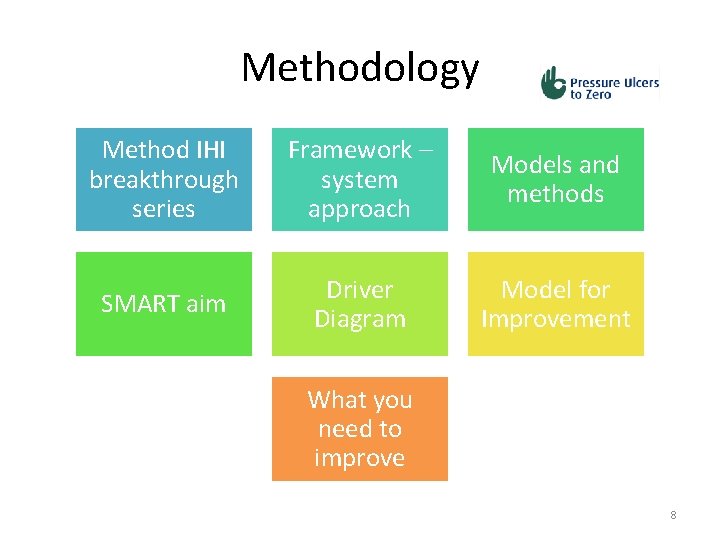
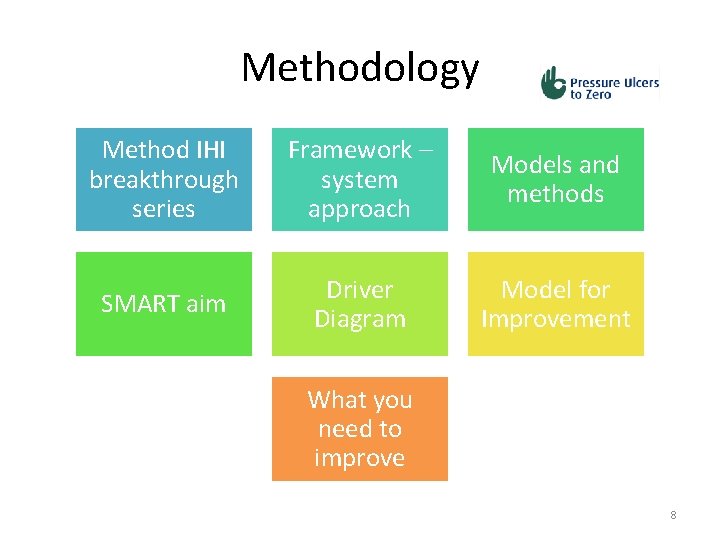
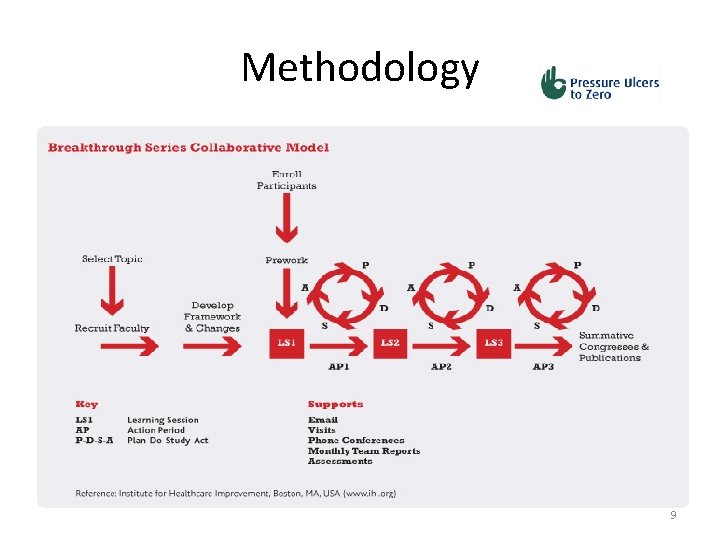
Methodology Method IHI breakthrough series Framework – system approach Models and methods SMART aim Driver Diagram Model for Improvement What you need to improve 8
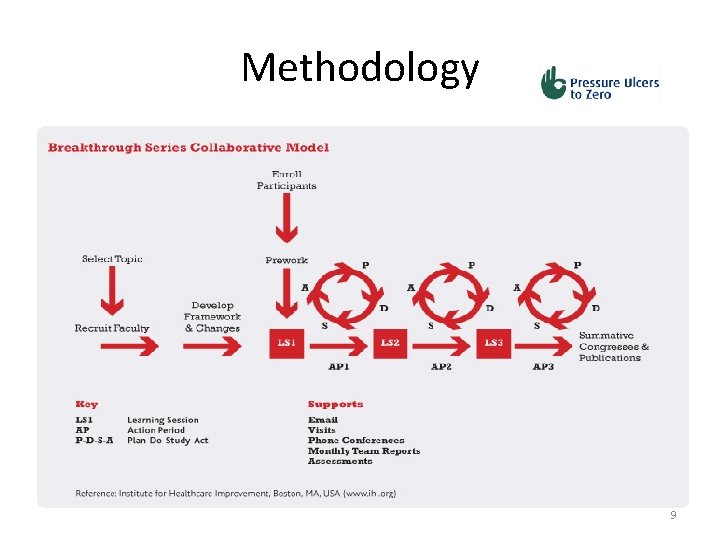
Methodology 9
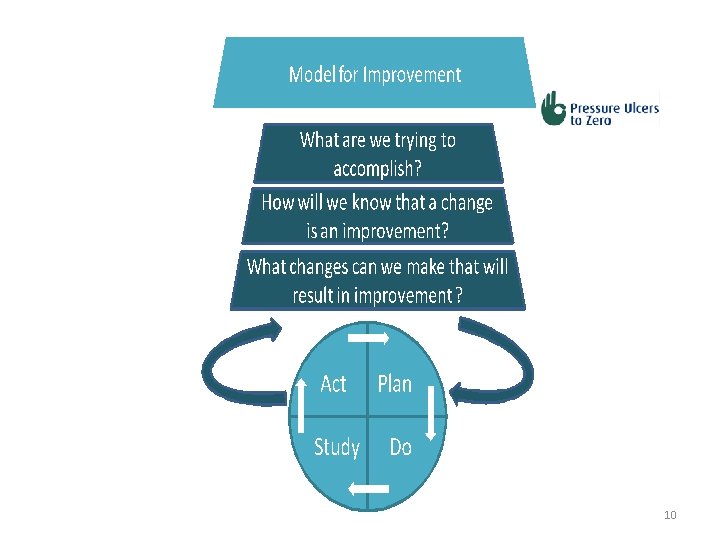
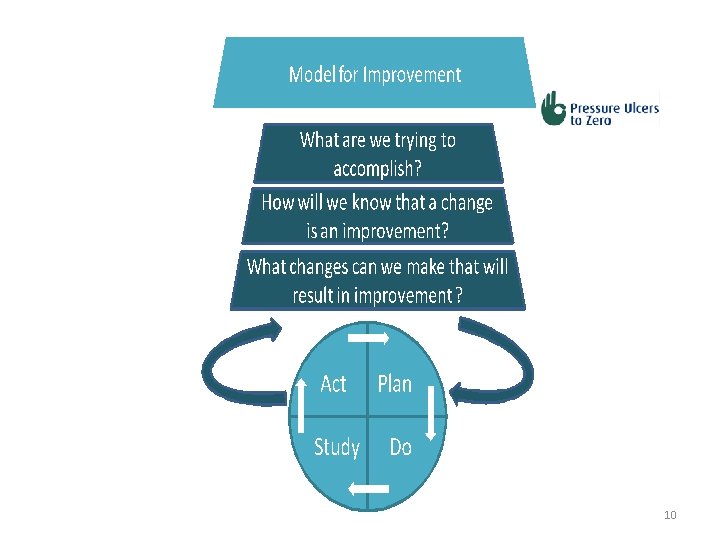
10
A framework for Improvement STRUCTURE + PROCESS + CULTURE = OUTCOMES • *Added to Donabedian’s original formulation by R. Lloyd and R. Scoville 11
Quality Improvement Models and Methods Deming’s Lens of Profound Knowledge Driver diagram The Model for improvement Measurement for improvement Improving flow Reducing waste and variation The Science of reliability 12
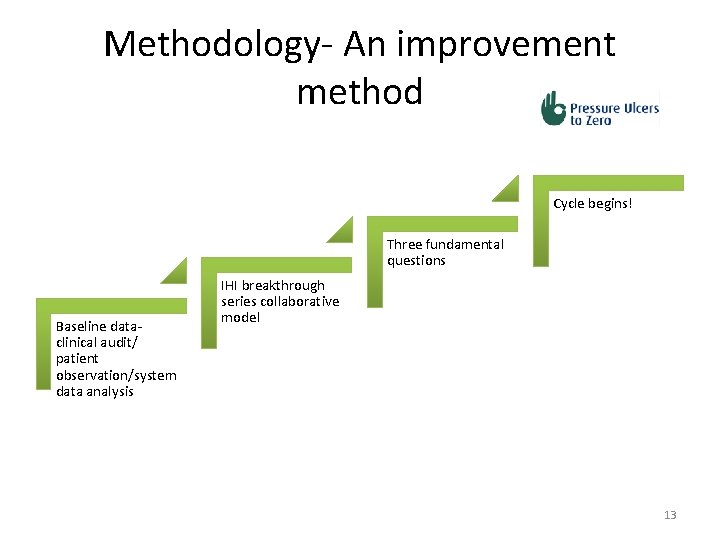
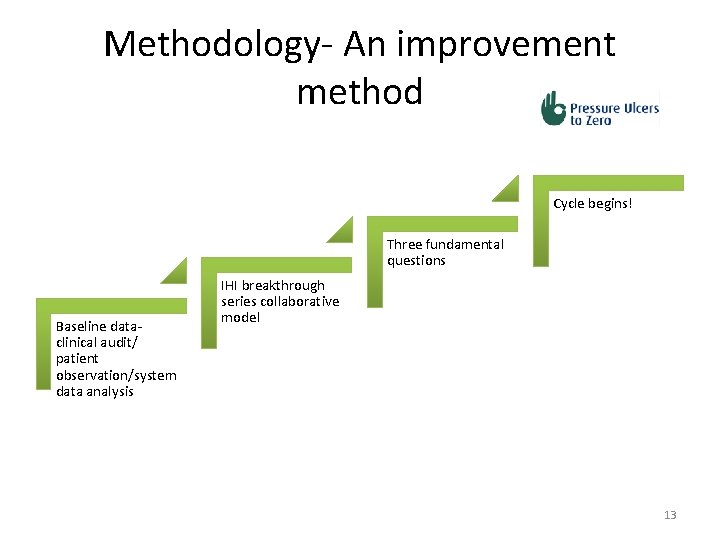
Methodology- An improvement method Cycle begins! Three fundamental questions Baseline dataclinical audit/ patient observation/system data analysis IHI breakthrough series collaborative model 13
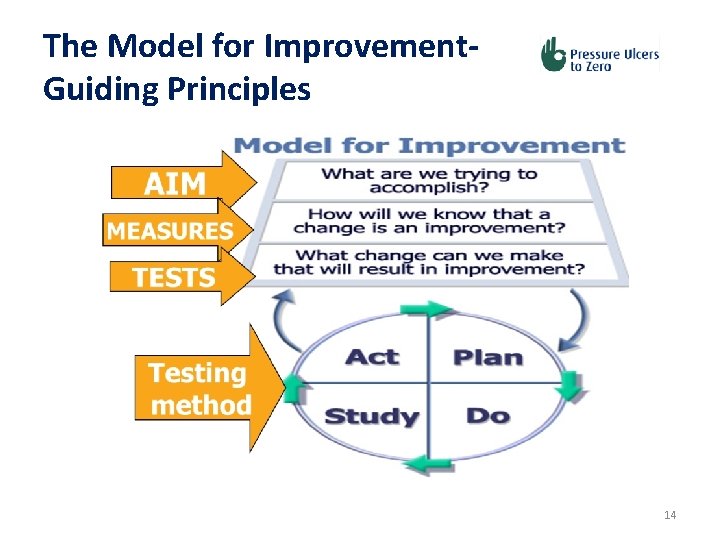
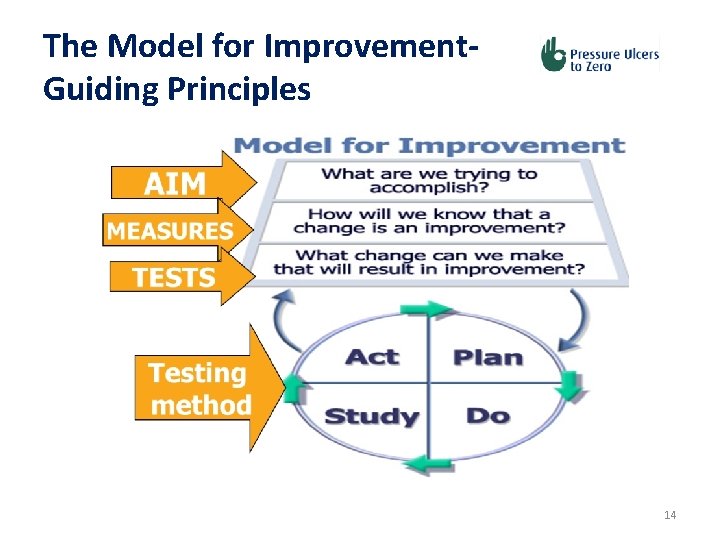
The Model for Improvement. Guiding Principles 14
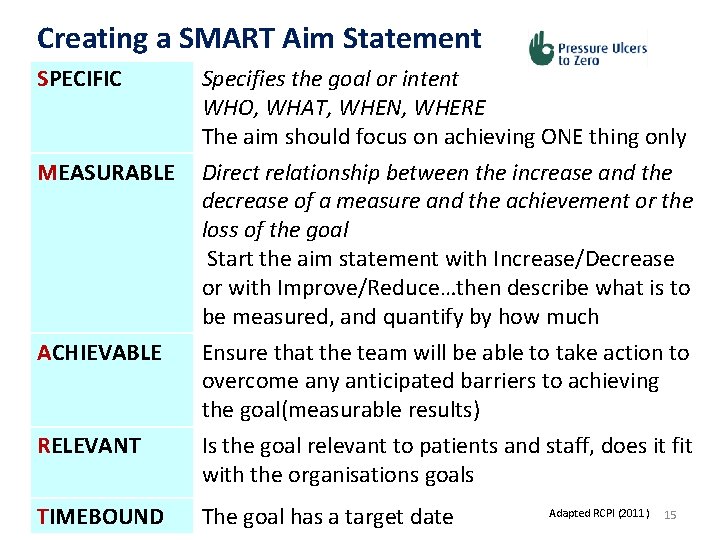
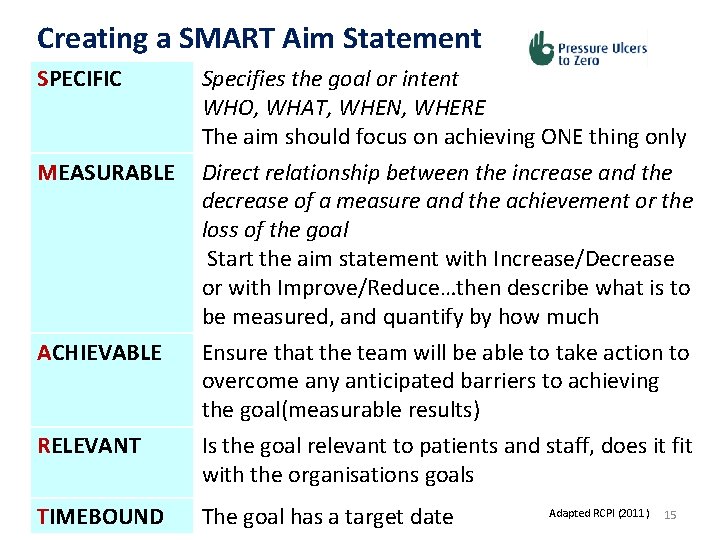
Creating a SMART Aim Statement SPECIFIC Specifies the goal or intent WHO, WHAT, WHEN, WHERE The aim should focus on achieving ONE thing only MEASURABLE Direct relationship between the increase and the decrease of a measure and the achievement or the loss of the goal Start the aim statement with Increase/Decrease or with Improve/Reduce…then describe what is to be measured, and quantify by how much ACHIEVABLE Ensure that the team will be able to take action to overcome any anticipated barriers to achieving the goal(measurable results) RELEVANT Is the goal relevant to patients and staff, does it fit with the organisations goals TIMEBOUND The goal has a target date Adapted RCPI (2011) 15
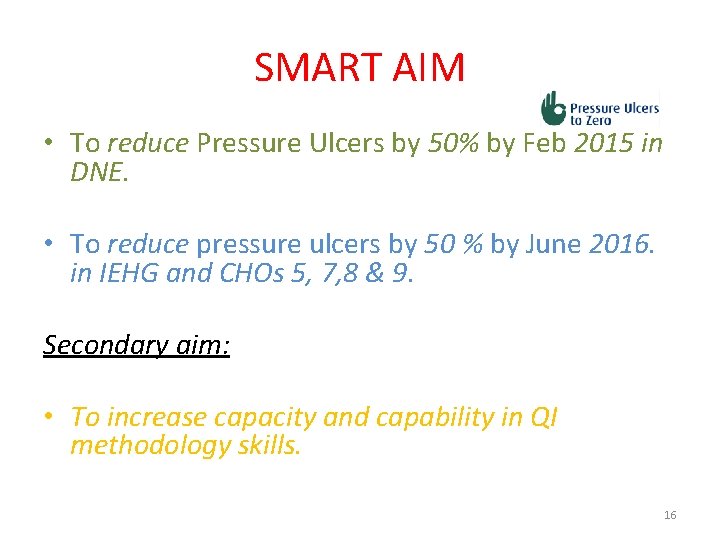
SMART AIM • To reduce Pressure Ulcers by 50% by Feb 2015 in DNE. • To reduce pressure ulcers by 50 % by June 2016. in IEHG and CHOs 5, 7, 8 & 9. Secondary aim: • To increase capacity and capability in QI methodology skills. 16
Component parts of a driver diagram Ø SMART Aim Ø Primary drivers - system components in the system that directly influence the chosen aim or goal. This are the big areas -processes Ø Secondary drivers – are elements of the primary drivers which can be used to create change projects. Components and activities Ø Change ideas - ideas to test, in order to help move towards the aim and should affect at last one secondary driver Ø Relationship arrows - show the connection between the primary and secondary drivers. 17
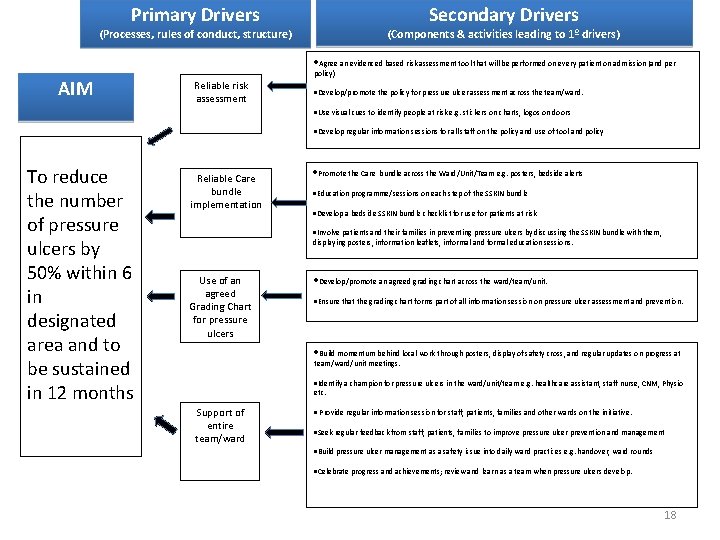
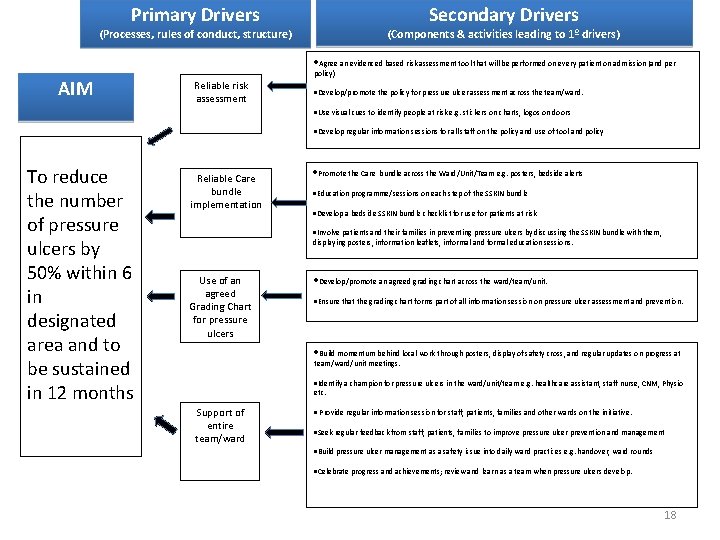
Primary Drivers Secondary Drivers (Processes, rules of conduct, structure) (Components & activities leading to 1º drivers) Agree an evidenced based risk assessment tool that will be performed on every patient on admission (and per AIM policy) Reliable risk assessment Develop/promote the policy for pressure ulcer assessment across the team/ward. Use visual cues to identify people at risk e. g. stickers on charts, logos on doors Develop regular information sessions for all staff on the policy and use of tool and policy To reduce the number of pressure ulcers by 50% within 6 in designated area and to be sustained in 12 months Reliable Care bundle implementation Promote the Care bundle across the Ward/Unit/Team e. g. posters, bedside alerts Education programme/sessions on each step of the SSKIN bundle Develop a bedside SSKIN bundle checklist for use for patients at risk Involve patients and their families in preventing pressure ulcers by discussing the SSKIN bundle with them, displaying posters, information leaflets, informal and formal education sessions. Use of an agreed Grading Chart for pressure ulcers Develop/promote an agreed grading chart across the ward/team/unit. Ensure that the grading chart forms part of all information session on pressure ulcer assessment and prevention. Build momentum behind local work through posters, display of safety cross, and regular updates on progress at team/ward/unit meetings. Identify a champion for pressure ulcers in the ward/unit/team e. g. healthcare assistant, staff nurse, CNM, Physio etc. Support of entire team/ward Provide regular information session for staff, patients, families and other wards on the initiative. Seek regular feedback from staff, patients, families to improve pressure ulcer prevention and management Build pressure ulcer management as a safety issue into daily ward practices e. g. handover, ward rounds Celebrate progress and achievements; review and learn as a team when pressure ulcers develop. 18
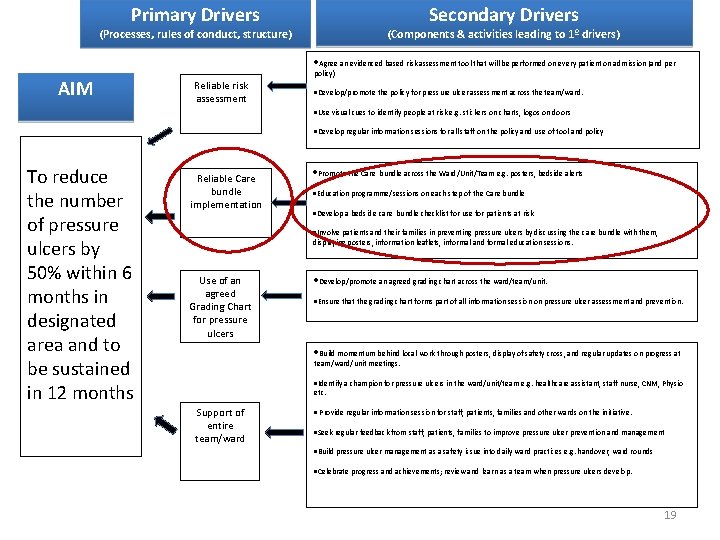
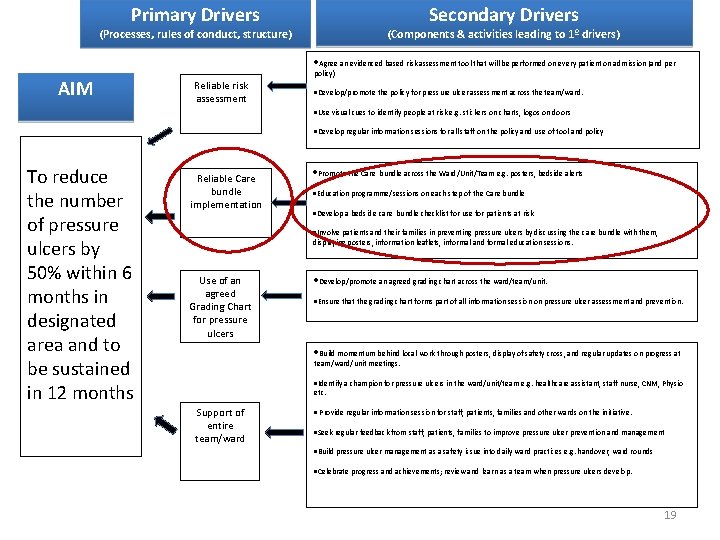
Primary Drivers Secondary Drivers (Processes, rules of conduct, structure) (Components & activities leading to 1º drivers) Agree an evidenced based risk assessment tool that will be performed on every patient on admission (and per AIM policy) Reliable risk assessment Develop/promote the policy for pressure ulcer assessment across the team/ward. Use visual cues to identify people at risk e. g. stickers on charts, logos on doors Develop regular information sessions for all staff on the policy and use of tool and policy To reduce the number of pressure ulcers by 50% within 6 months in designated area and to be sustained in 12 months Reliable Care bundle implementation Promote the Care bundle across the Ward/Unit/Team e. g. posters, bedside alerts Education programme/sessions on each step of the Care bundle Develop a bedside care bundle checklist for use for patients at risk Involve patients and their families in preventing pressure ulcers by discussing the care bundle with them, displaying posters, information leaflets, informal and formal education sessions. Use of an agreed Grading Chart for pressure ulcers Develop/promote an agreed grading chart across the ward/team/unit. Ensure that the grading chart forms part of all information session on pressure ulcer assessment and prevention. Build momentum behind local work through posters, display of safety cross, and regular updates on progress at team/ward/unit meetings. Identify a champion for pressure ulcers in the ward/unit/team e. g. healthcare assistant, staff nurse, CNM, Physio etc. Support of entire team/ward Provide regular information session for staff, patients, families and other wards on the initiative. Seek regular feedback from staff, patients, families to improve pressure ulcer prevention and management Build pressure ulcer management as a safety issue into daily ward practices e. g. handover, ward rounds Celebrate progress and achievements; review and learn as a team when pressure ulcers develop. 19
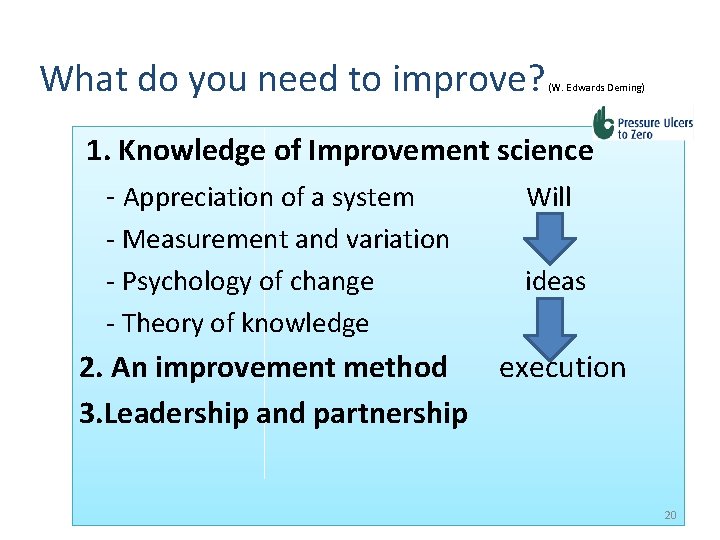
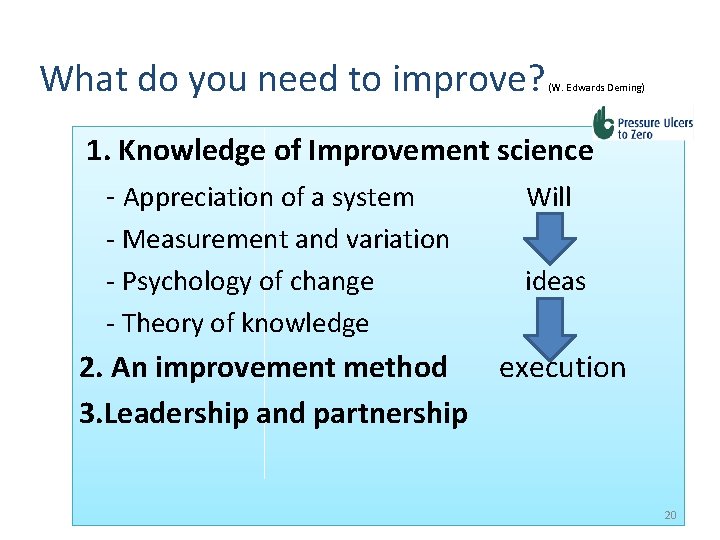
What do you need to improve? (W. Edwards Deming) 1. Knowledge of Improvement science - Appreciation of a system Will - Measurement and variation - Psychology of change - Theory of knowledge ideas 2. An improvement method execution 3. Leadership and partnership 20
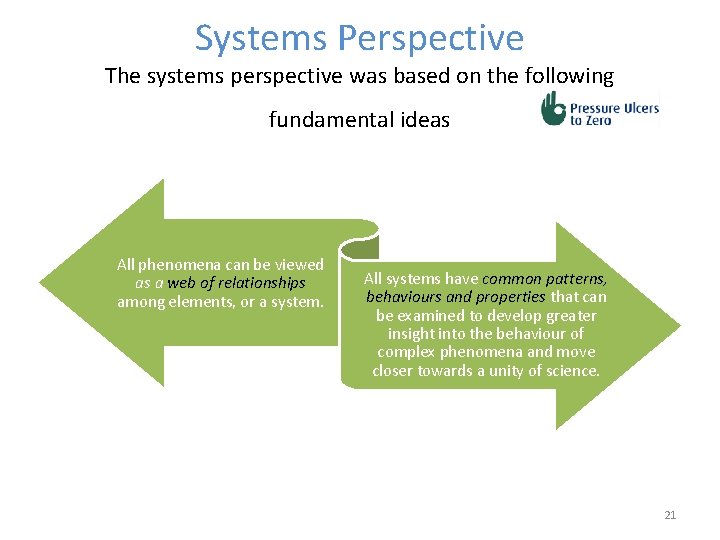
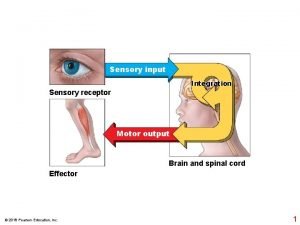
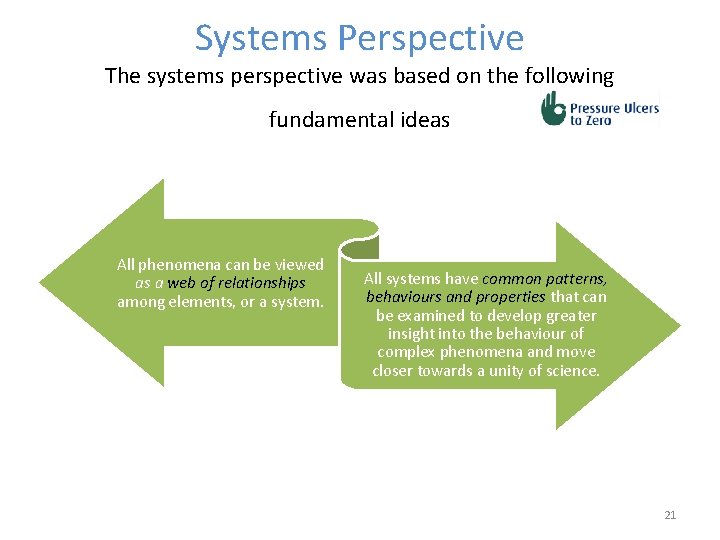
Systems Perspective The systems perspective was based on the following fundamental ideas All phenomena can be viewed as a web of relationships among elements, or a system. All systems have common patterns, behaviours and properties that can be examined to develop greater insight into the behaviour of complex phenomena and move closer towards a unity of science. 21
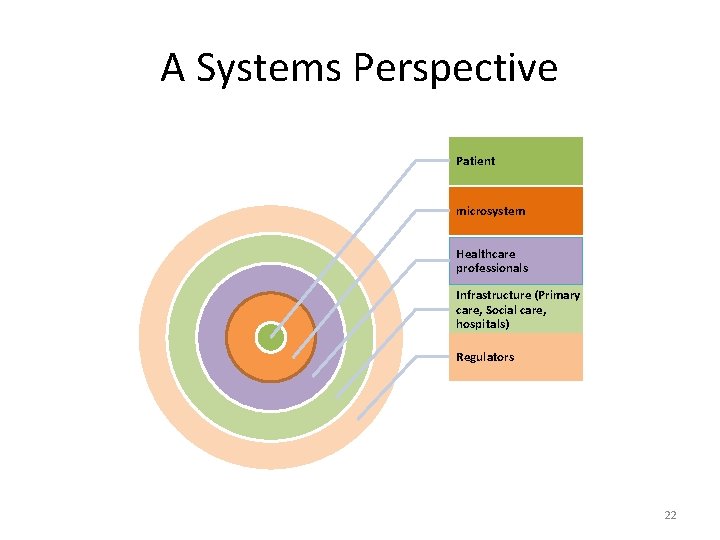
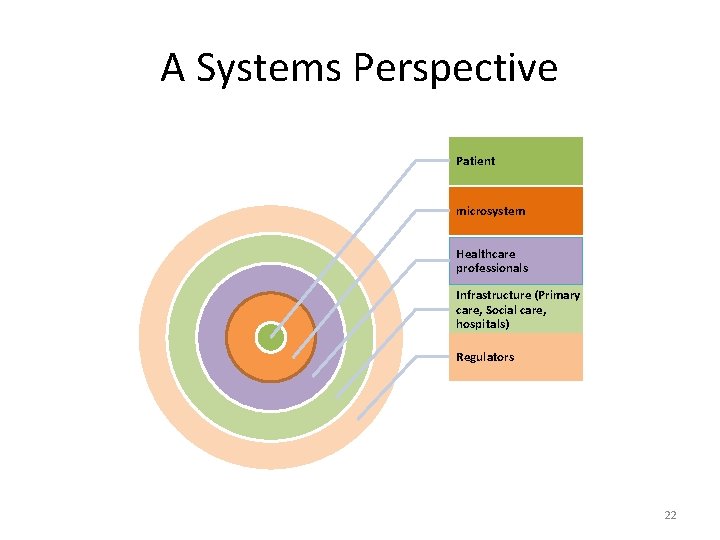
A Systems Perspective Patient microsystem Healthcare professionals Infrastructure (Primary care, Social care, hospitals) Regulators 22
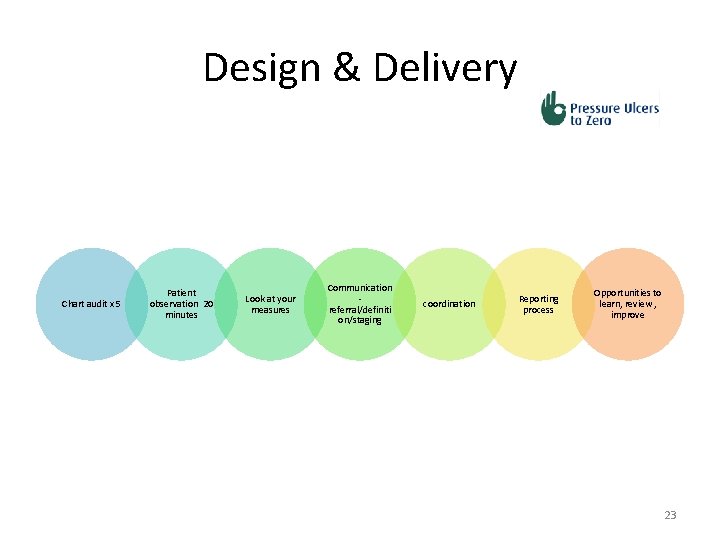
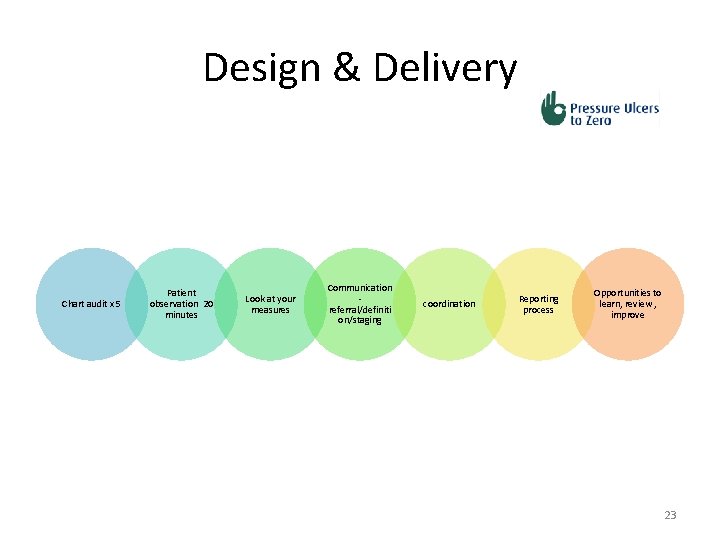
Design & Delivery Chart audit x 5 Patient observation 20 minutes Look at your measures Communication referral/definiti on/staging coordination Reporting process Opportunities to learn, review , improve 23
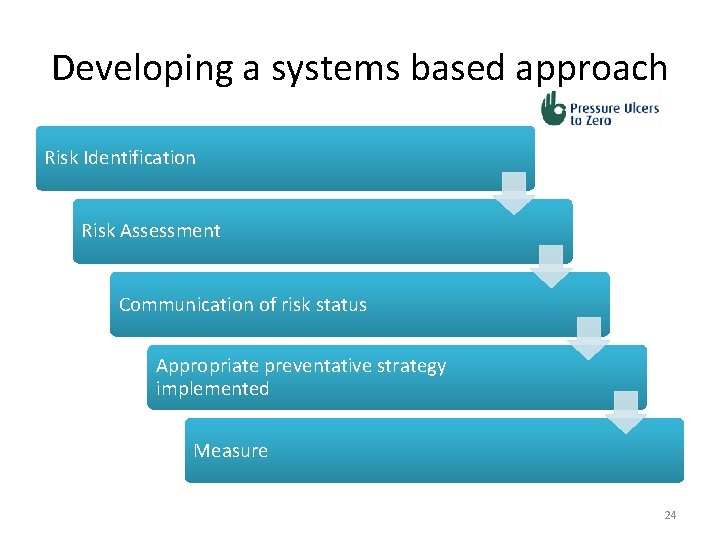
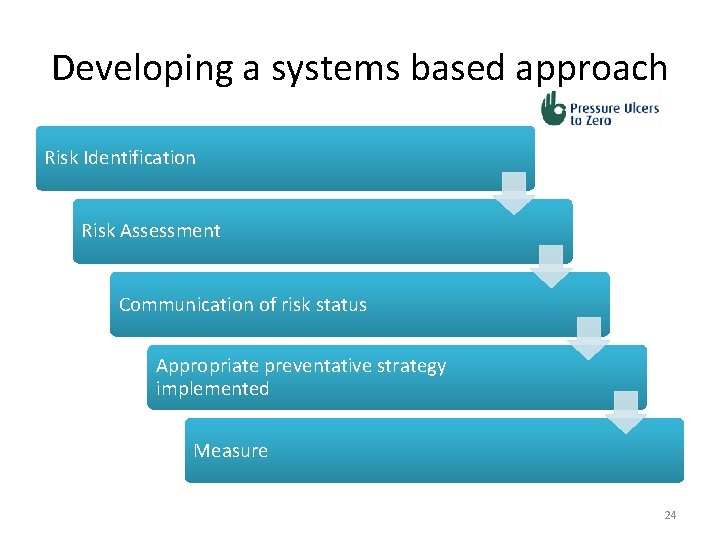
Developing a systems based approach Risk Identification Risk Assessment Communication of risk status Appropriate preventative strategy implemented Measure 24
Data “In God we trust. All others bring data” W. E. Deming • Research vs Audit vs QI – Research is what’s possible – Audit is what’s actual – Quality Improvement is making what’s possible actual 25
Why are we measuring ? 26
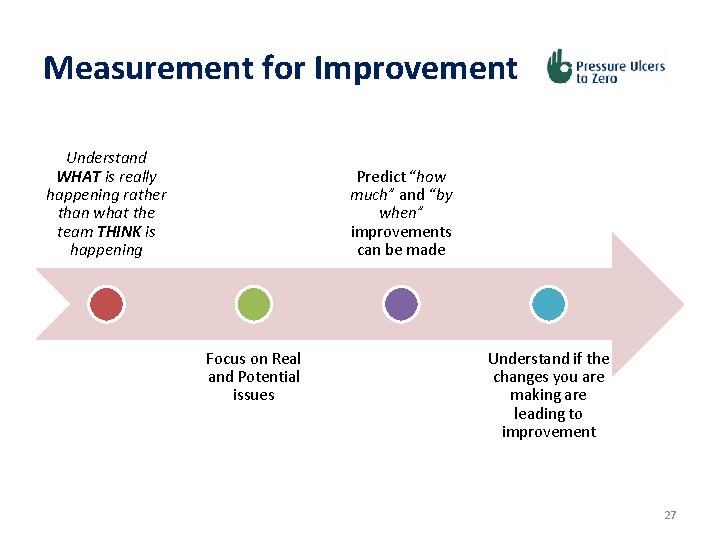
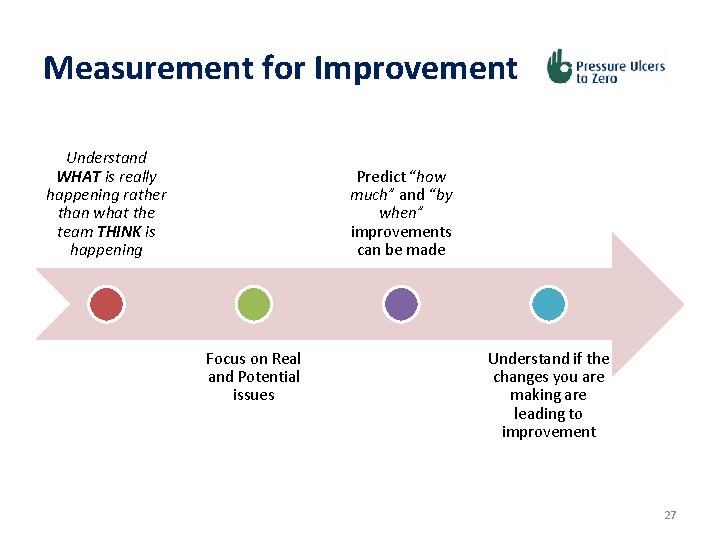
Measurement for Improvement Understand WHAT is really happening rather than what the team THINK is happening Predict “how much” and “by when” improvements can be made Focus on Real and Potential issues Understand if the changes you are making are leading to improvement 27
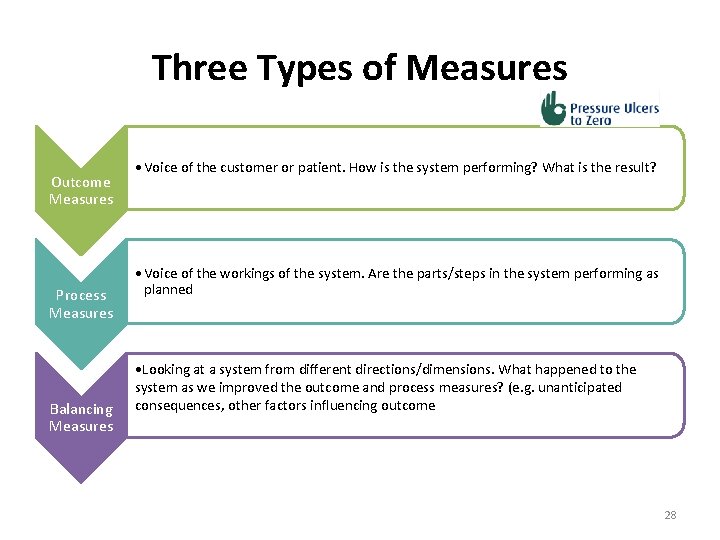
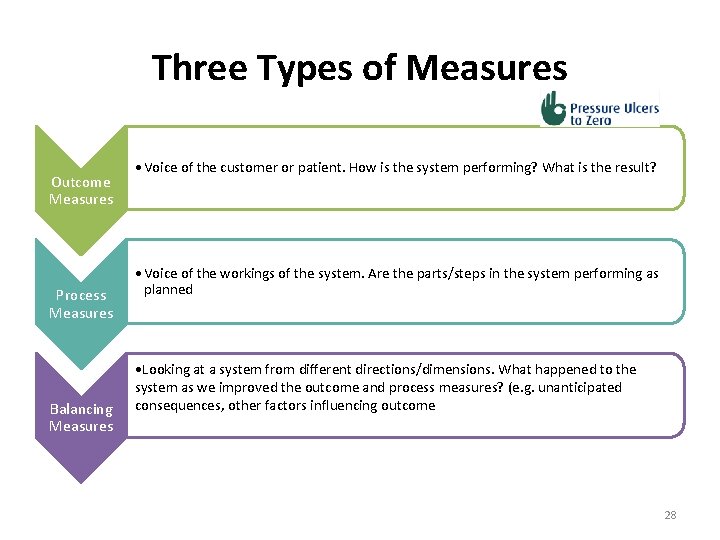
Three Types of Measures Outcome Measures Process Measures Balancing Measures • Voice of the customer or patient. How is the system performing? What is the result? • Voice of the workings of the system. Are the parts/steps in the system performing as planned • Looking at a system from different directions/dimensions. What happened to the system as we improved the outcome and process measures? (e. g. unanticipated consequences, other factors influencing outcome 28
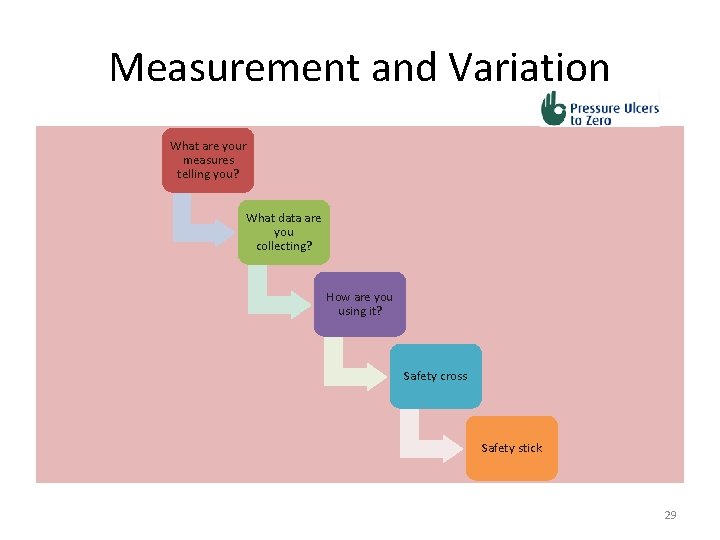
Measurement and Variation What are your measures telling you? What data are you collecting? How are you using it? Safety cross Safety stick 29
Standardised data tool • Only include New Pressure Ulcers • All grades of PU are included (1 -4 inclusive) • PUs are only counted once and colour coded 30
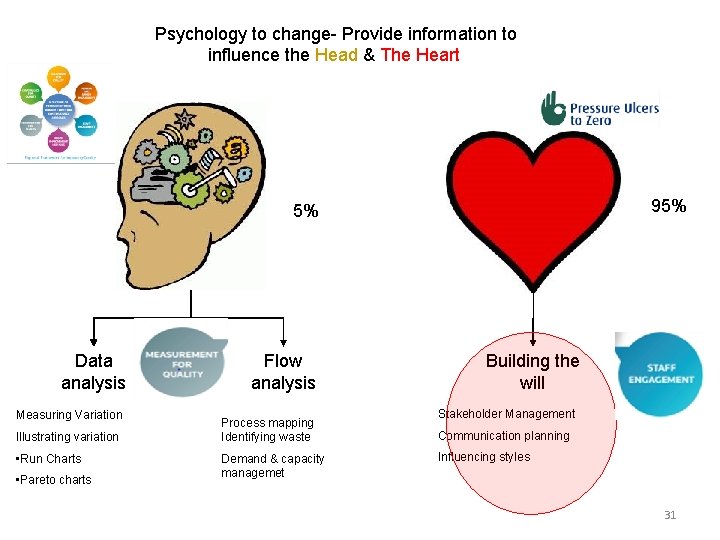
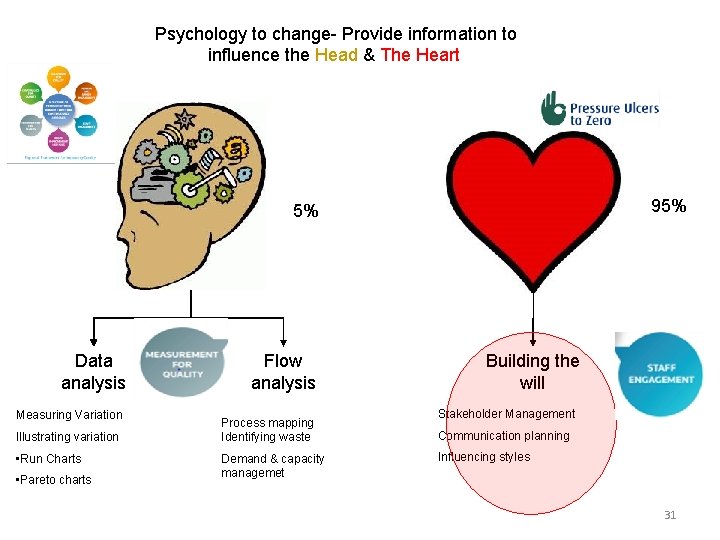
Psychology to change- Provide information to influence the Head & The Heart 95% 5% Data analysis Measuring Variation Illustrating variation • Run Charts • Pareto charts Flow analysis Process mapping Identifying waste Demand & capacity managemet Building the will Stakeholder Management Communication planning Influencing styles 31
People • Most healthcare involves complex adaptive systems • Change requires engagement with people – Front line ownership 32
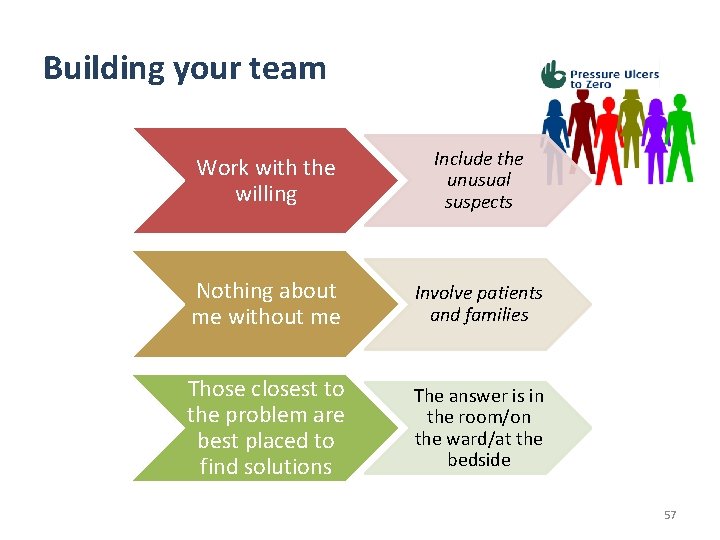
Front Line Ownership • Work with the willing – Include the unusual supects • Triggers for change usually unpredictable – Build on what grows • Nothing about me without me • Those closest to the problem are best placed to find solutions – The answer is in the room • Focus on minimum specifications 33
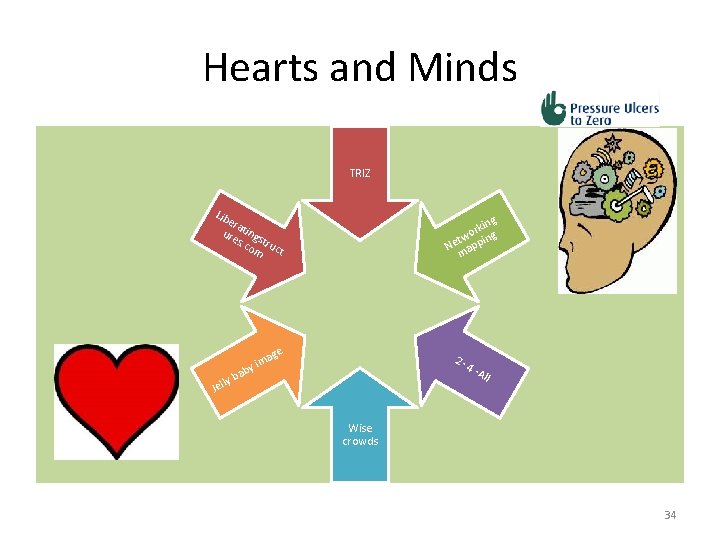
Hearts and Minds TRIZ Lib era ure tings s. c tru om ct ng rki g o tw in Ne app m ge a y im 2 - ab ly b Jel 4 - All Wise crowds 34
Staff engagement Staff are engaged when they feel valued, are emotionally connected, fully involved, enthusiastic and committed to providing a good service. . . when each person knows that what they do and say matters and makes a difference. National Staff Engagement Forum (2016) 35
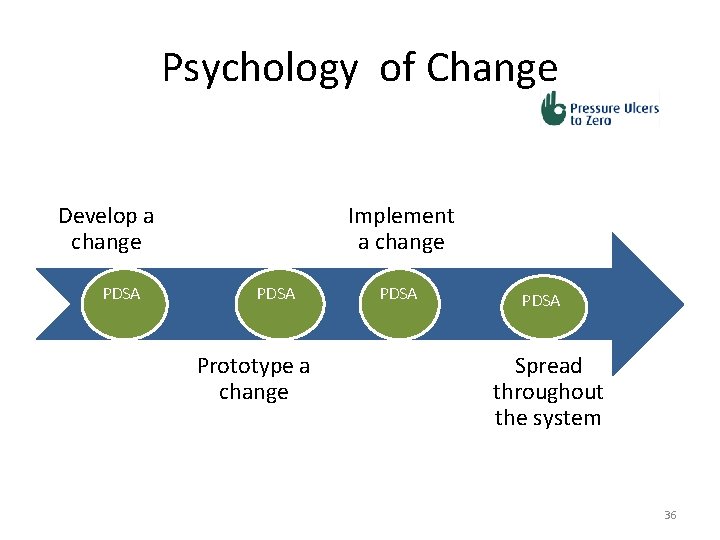
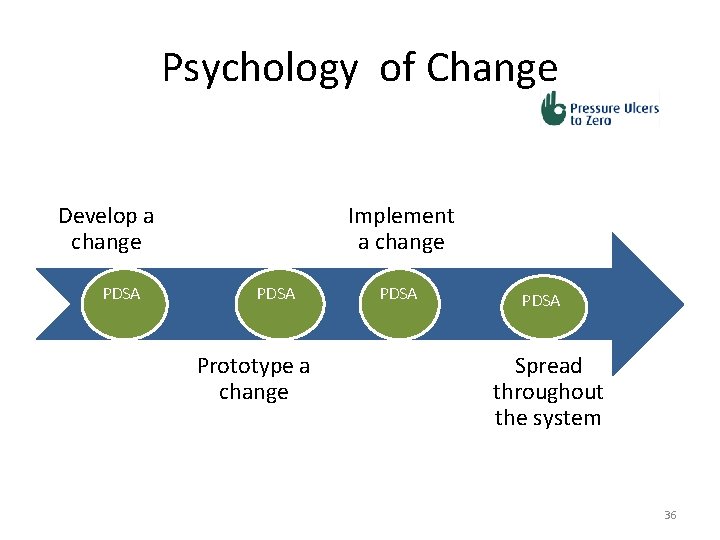
Psychology of Change Develop a change PDSA Implement a change PDSA Prototype a change PDSA Spread throughout the system 36

Steps to Change -Key rules! Identify prerequisites for changes Test under a variety of conditions Embed in daily life 37
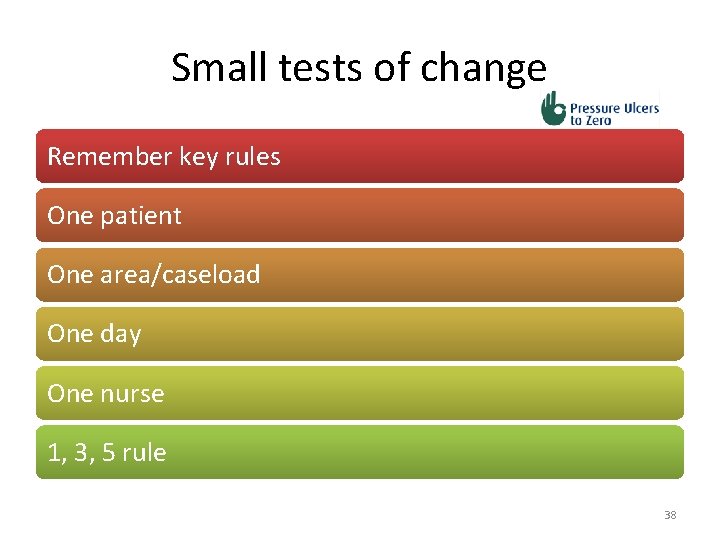
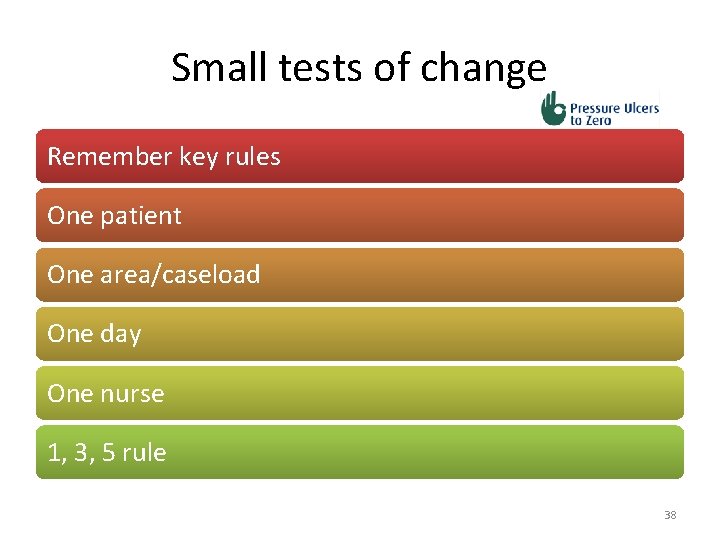
Small tests of change Remember key rules One patient One area/caseload One day One nurse 1, 3, 5 rule 38
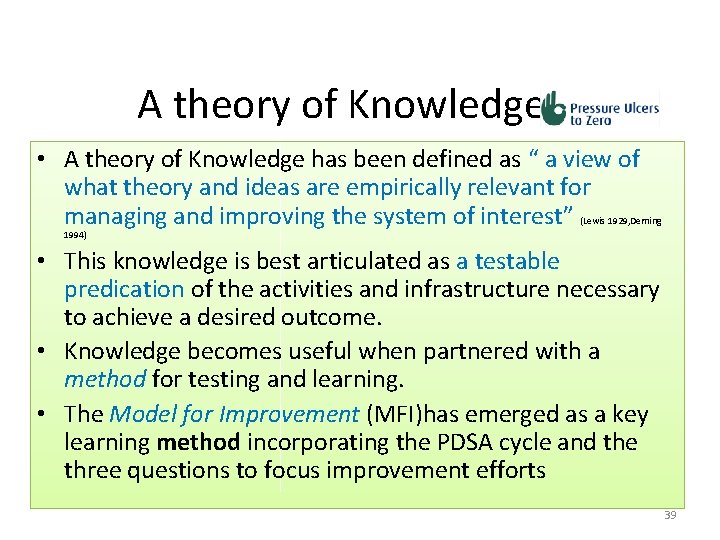
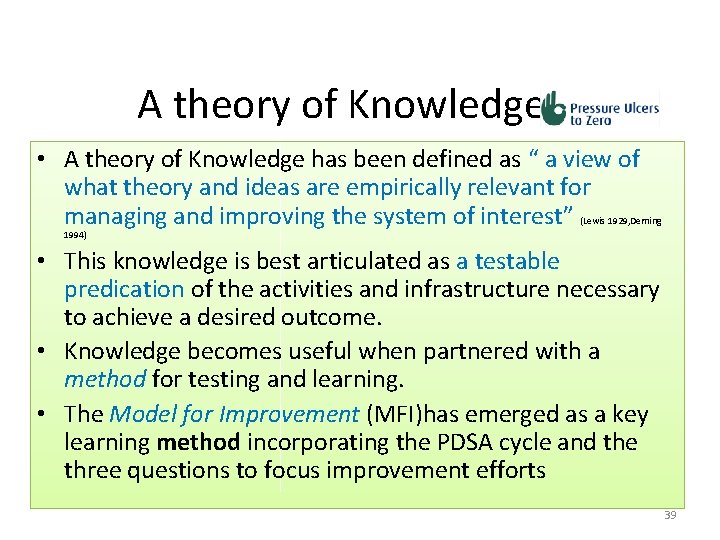
A theory of Knowledge • A theory of Knowledge has been defined as “ a view of what theory and ideas are empirically relevant for managing and improving the system of interest” (Lewis 1929, Deming 1994) • This knowledge is best articulated as a testable predication of the activities and infrastructure necessary to achieve a desired outcome. • Knowledge becomes useful when partnered with a method for testing and learning. • The Model for Improvement (MFI)has emerged as a key learning method incorporating the PDSA cycle and the three questions to focus improvement efforts 39
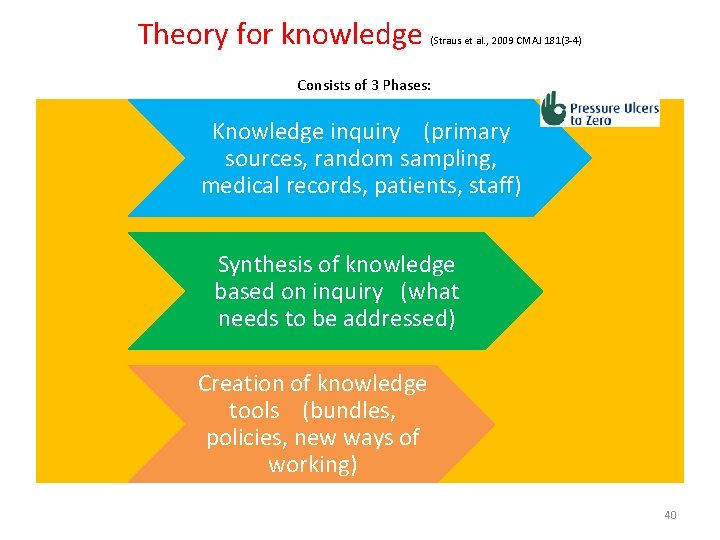
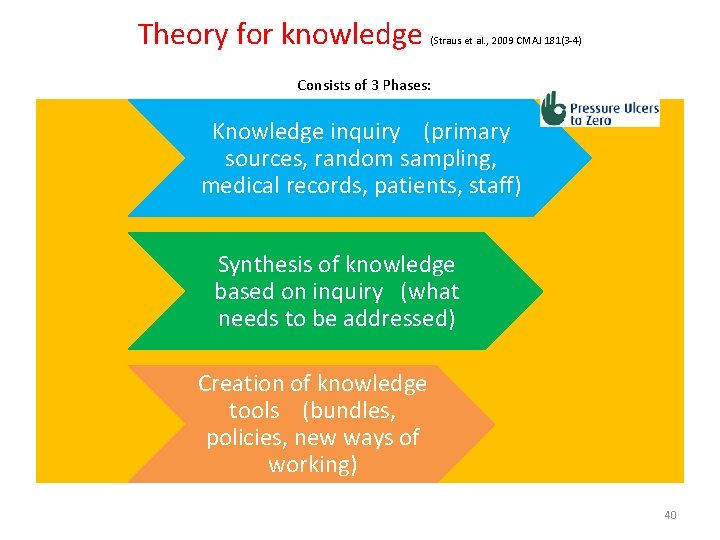
Theory for knowledge (Straus et al. , 2009 CMAJ 181(3 -4) Consists of 3 Phases: Knowledge inquiry (primary sources, random sampling, medical records, patients, staff) Synthesis of knowledge based on inquiry (what needs to be addressed) Creation of knowledge tools (bundles, policies, new ways of working) 40
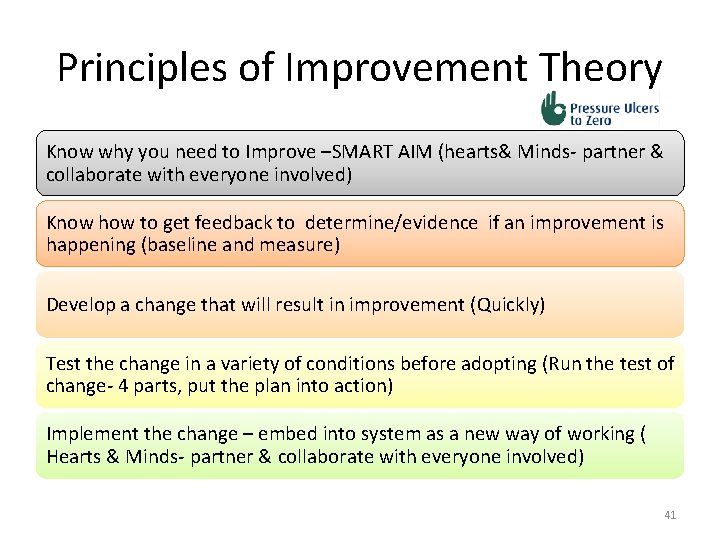
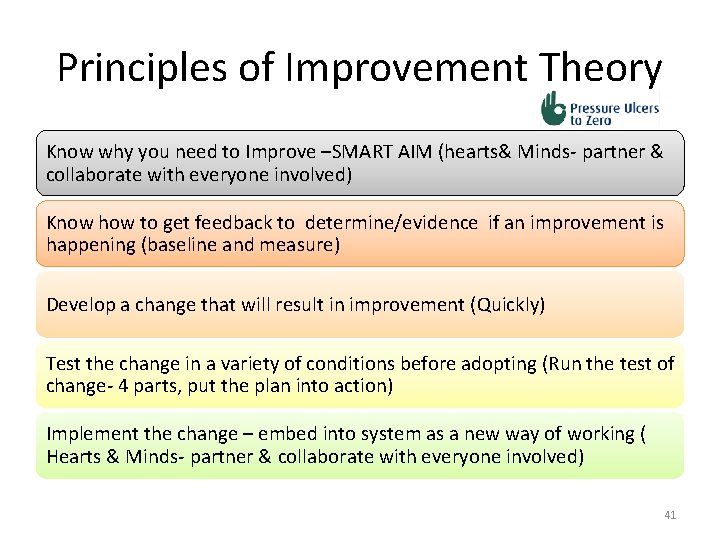
Principles of Improvement Theory Know why you need to Improve –SMART AIM (hearts& Minds- partner & collaborate with everyone involved) Know how to get feedback to determine/evidence if an improvement is happening (baseline and measure) Develop a change that will result in improvement (Quickly) Test the change in a variety of conditions before adopting (Run the test of change- 4 parts, put the plan into action) Implement the change – embed into system as a new way of working ( Hearts & Minds- partner & collaborate with everyone involved) 41
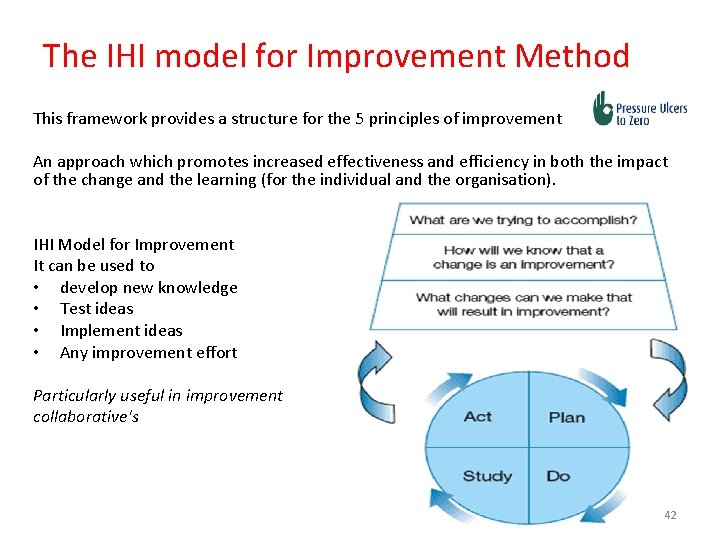
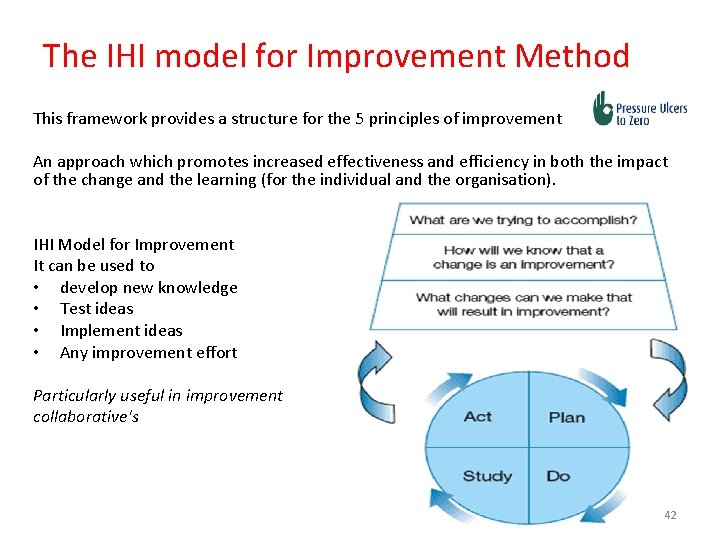
The IHI model for Improvement Method This framework provides a structure for the 5 principles of improvement An approach which promotes increased effectiveness and efficiency in both the impact of the change and the learning (for the individual and the organisation). IHI Model for Improvement It can be used to • develop new knowledge • Test ideas • Implement ideas • Any improvement effort Particularly useful in improvement collaborative's 42
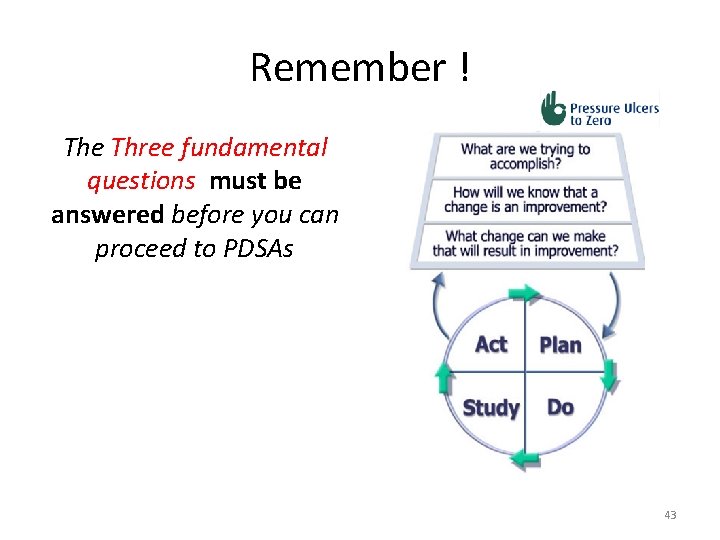
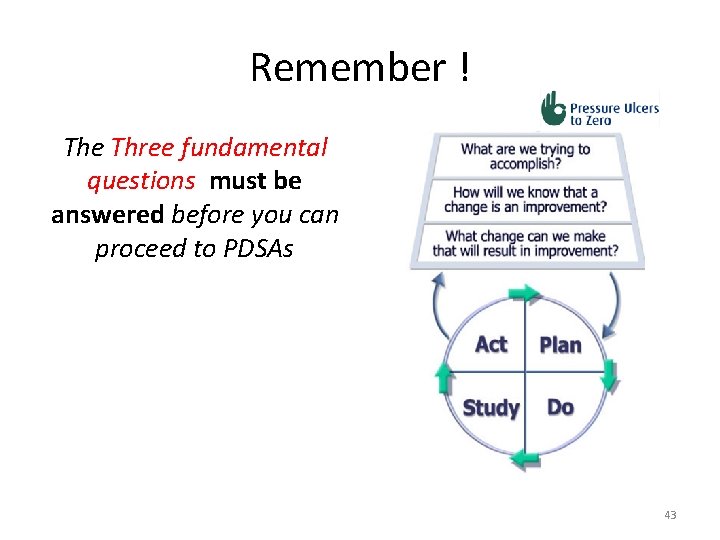
Remember ! The Three fundamental questions must be answered before you can proceed to PDSAs 43
Improvement methods “Insanity: doing the same thing over and over again and expecting different results. ” Albert Einstein 44
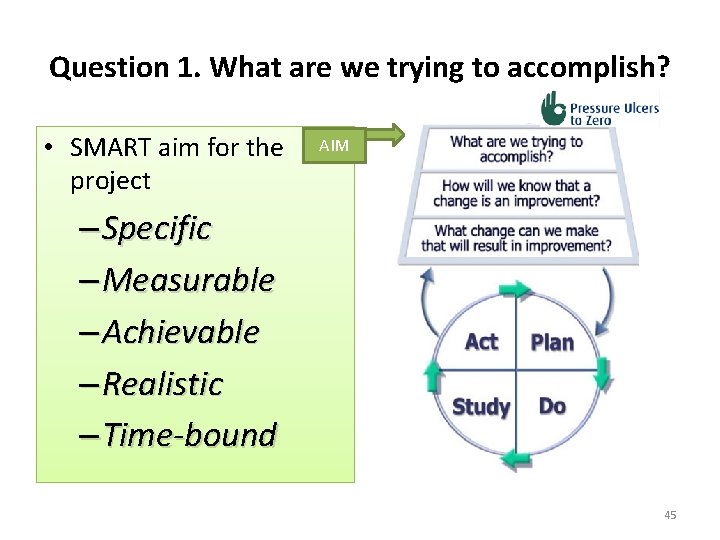
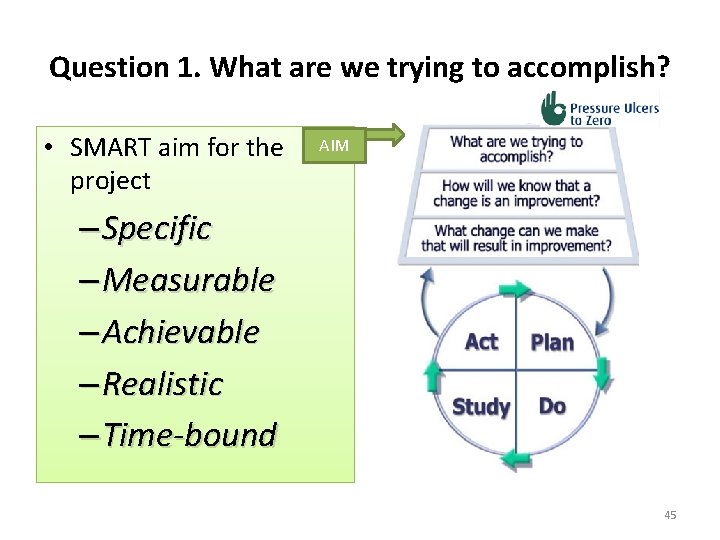
Question 1. What are we trying to accomplish? • SMART aim for the project AIM – Specific – Measurable – Achievable – Realistic – Time-bound 45
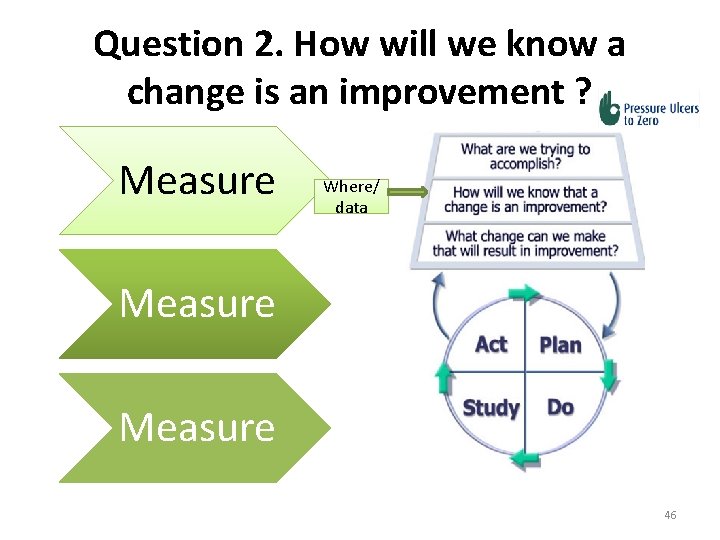
Question 2. How will we know a change is an improvement ? Measure Where/ data Measure 46
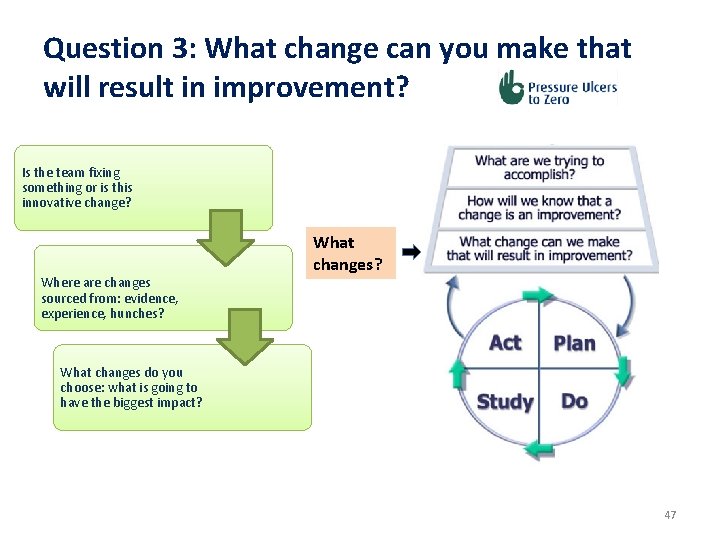
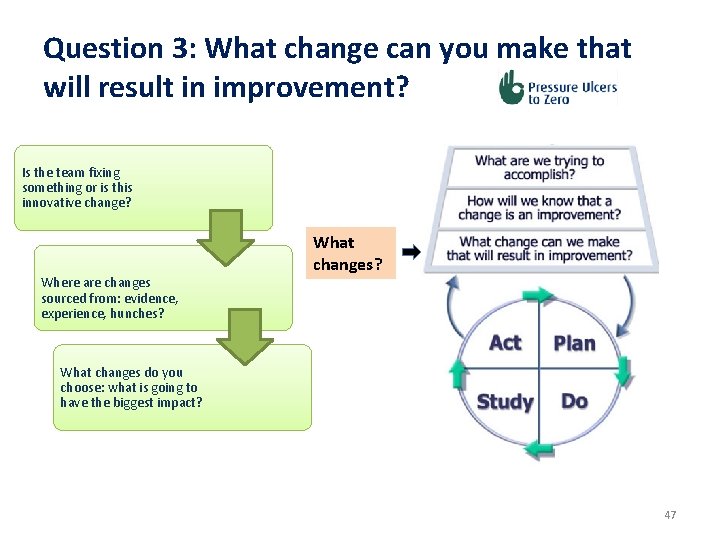
Question 3: What change can you make that will result in improvement? Is the team fixing something or is this innovative change? Where are changes sourced from: evidence, experience, hunches? What changes do you choose: what is going to have the biggest impact? 47
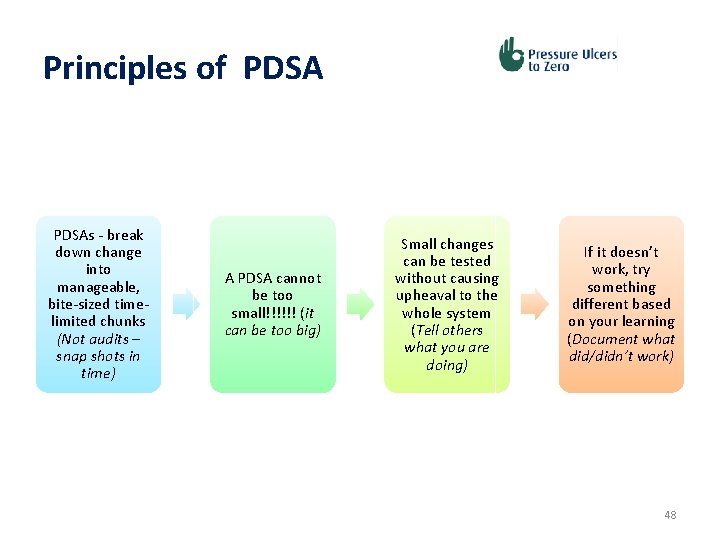
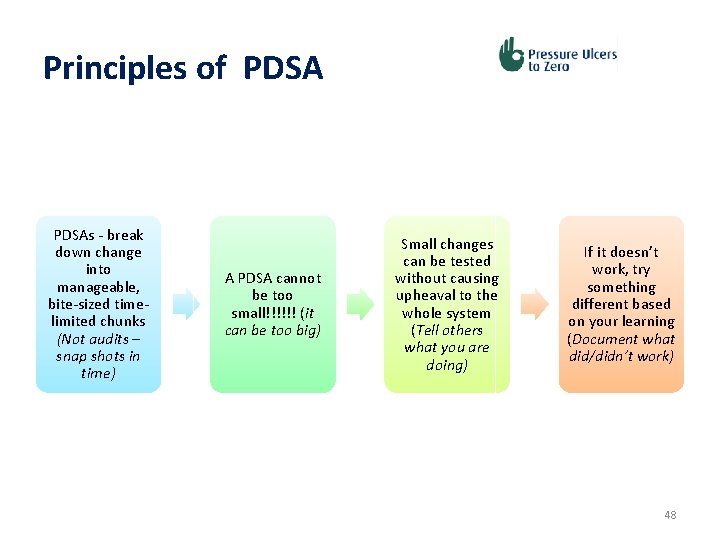
Principles of PDSAs - break down change into manageable, bite-sized timelimited chunks (Not audits – snap shots in time) A PDSA cannot be too small!!!!!! (it can be too big) Small changes can be tested without causing upheaval to the whole system (Tell others what you are doing) If it doesn’t work, try something different based on your learning (Document what did/didn’t work) 48
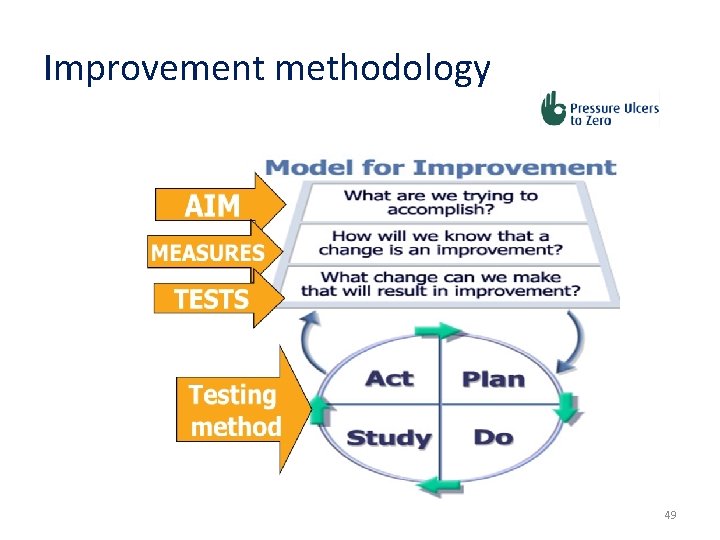
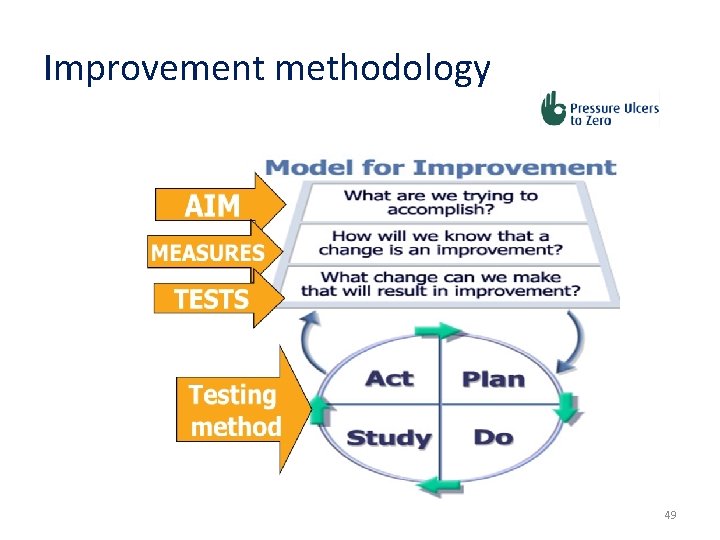
Improvement methodology 49
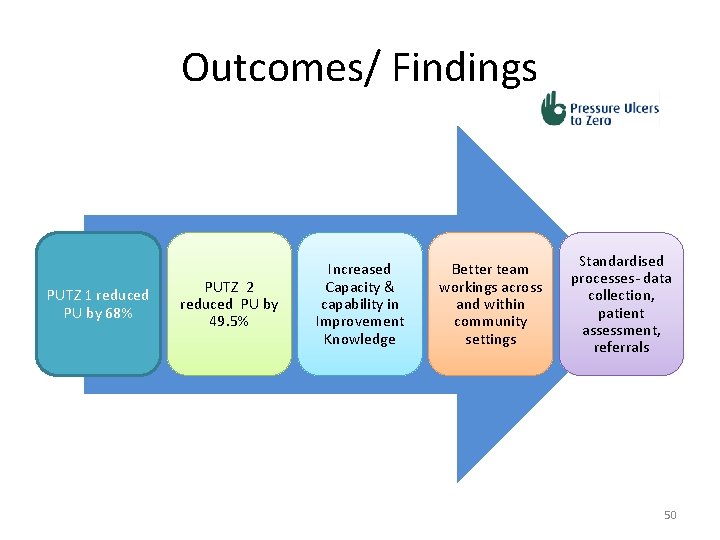
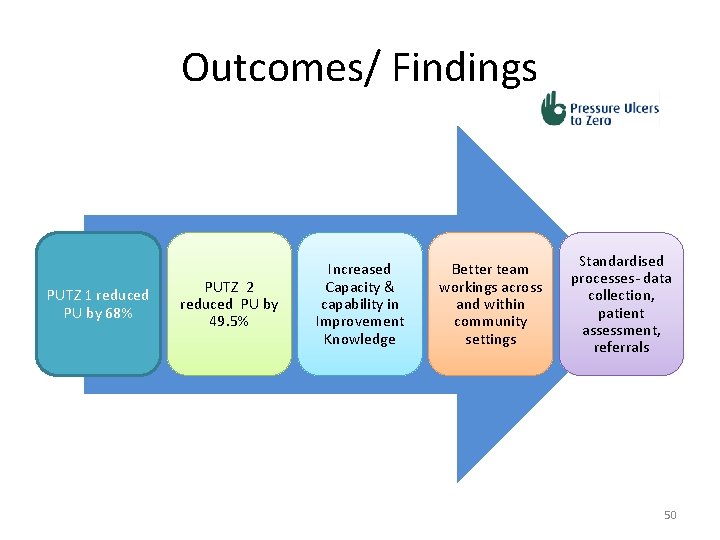
Outcomes/ Findings PUTZ 1 reduced PU by 68% PUTZ 2 reduced PU by 49. 5% Increased Capacity & capability in Improvement Knowledge Better team workings across and within community settings Standardised processes- data collection, patient assessment, referrals 50
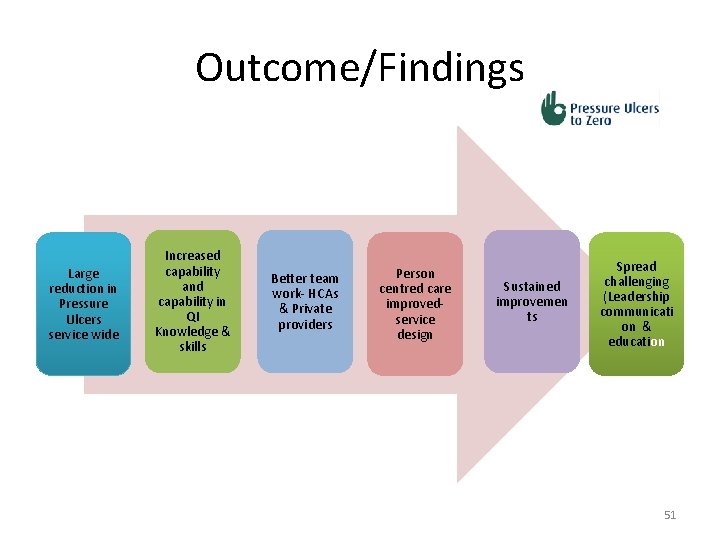
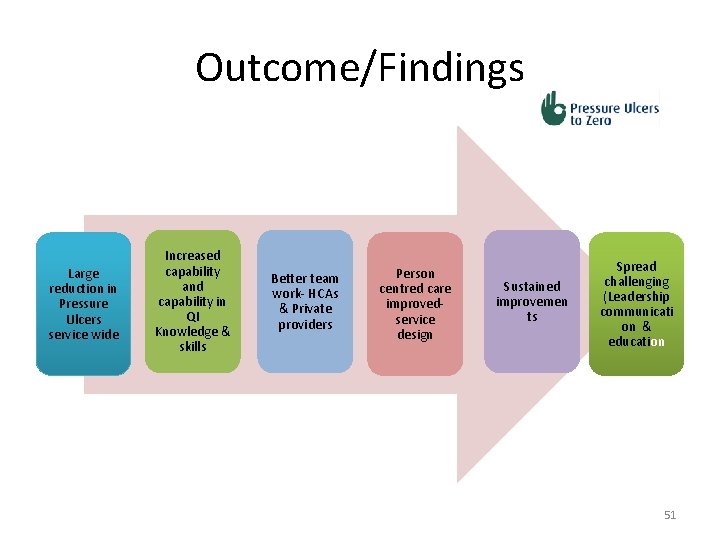
Outcome/Findings Large reduction in Pressure Ulcers service wide Increased capability and capability in QI Knowledge & skills Better team work- HCAs & Private providers Person centred care improvedservice design Sustained improvemen ts Spread challenging (Leadership communicati on & education 51
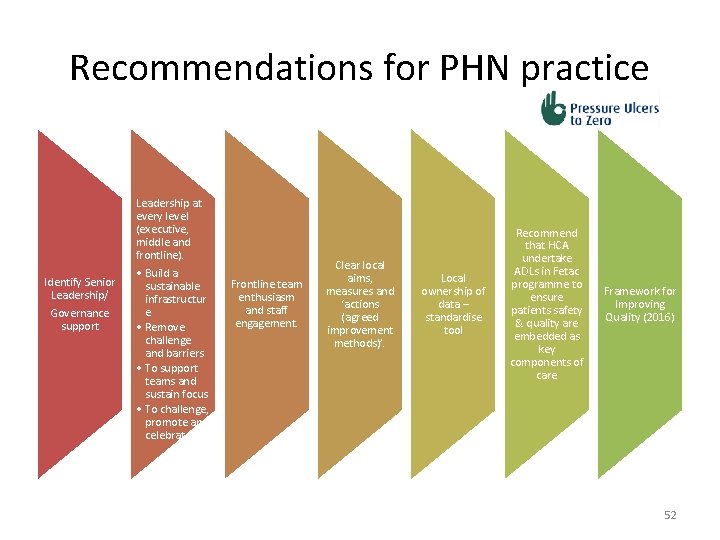
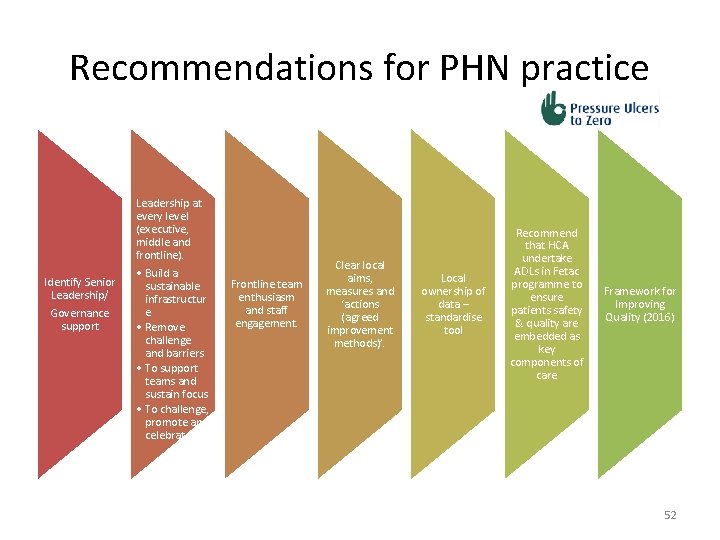
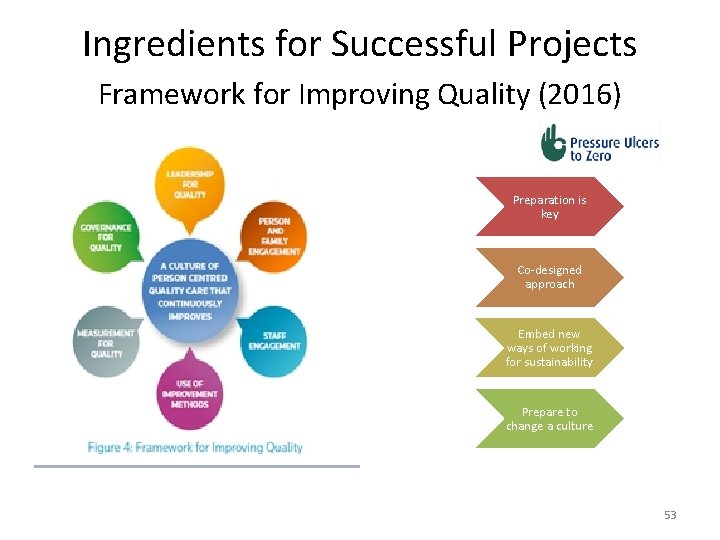
Recommendations for PHN practice Leadership at every level (executive, middle and frontline). Identify Senior Leadership/ Governance support • Build a sustainable infrastructur e • Remove challenge and barriers • To support teams and sustain focus • To challenge, promote and celebrate Frontline team enthusiasm and staff engagement. Clear local aims, measures and ‘actions (agreed improvement methods)’. Local ownership of data – standardise tool Recommend that HCA undertake ADLs in Fetac programme to ensure patients safety & quality are embedded as key components of care Framework for Improving Quality (2016) 52
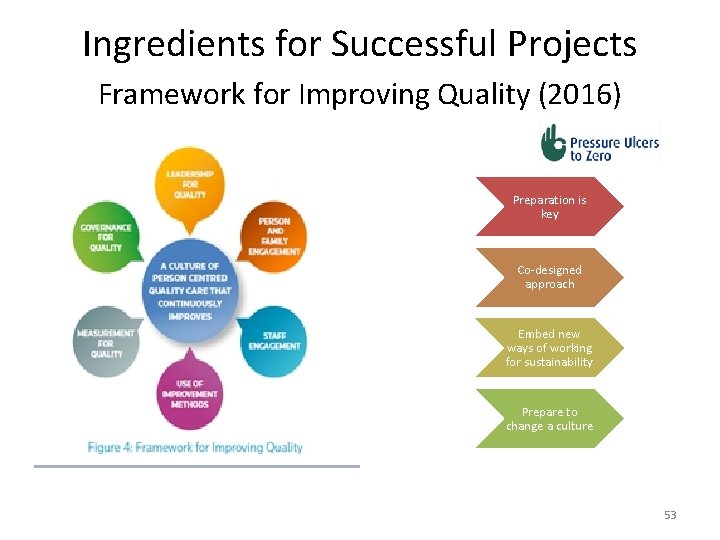
Ingredients for Successful Projects Framework for Improving Quality (2016) Preparation is key Co-designed approach Embed new ways of working for sustainability Prepare to change a culture 53
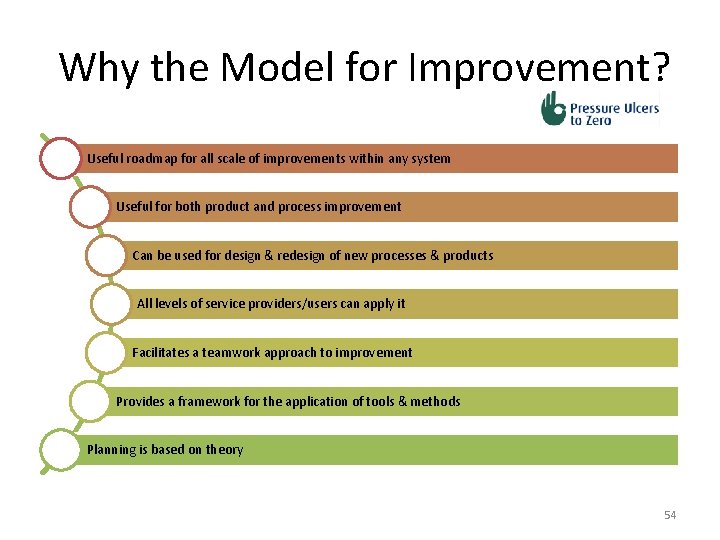
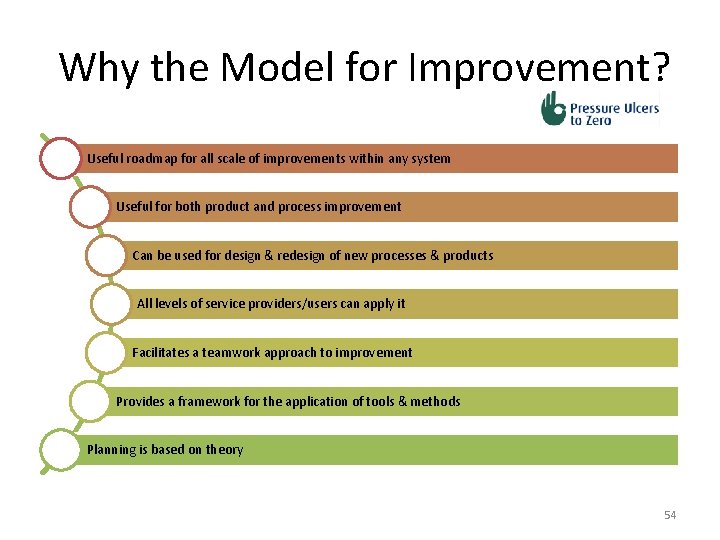
Why the Model for Improvement? Useful roadmap for all scale of improvements within any system Useful for both product and process improvement Can be used for design & redesign of new processes & products All levels of service providers/users can apply it Facilitates a teamwork approach to improvement Provides a framework for the application of tools & methods Planning is based on theory 54
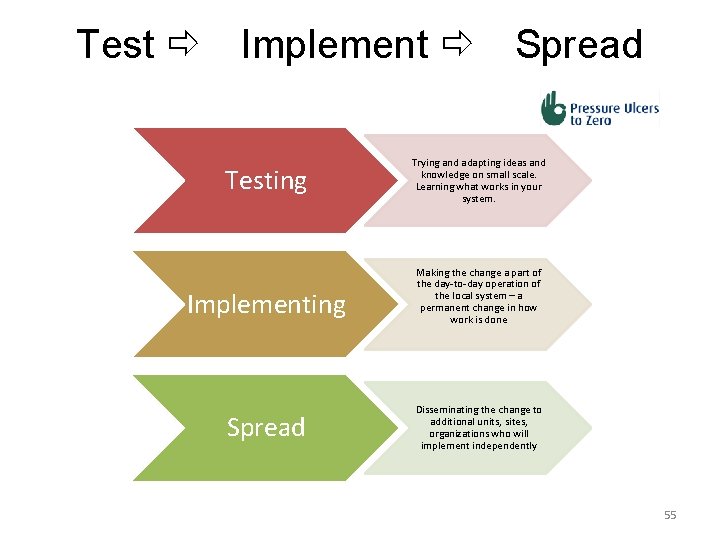
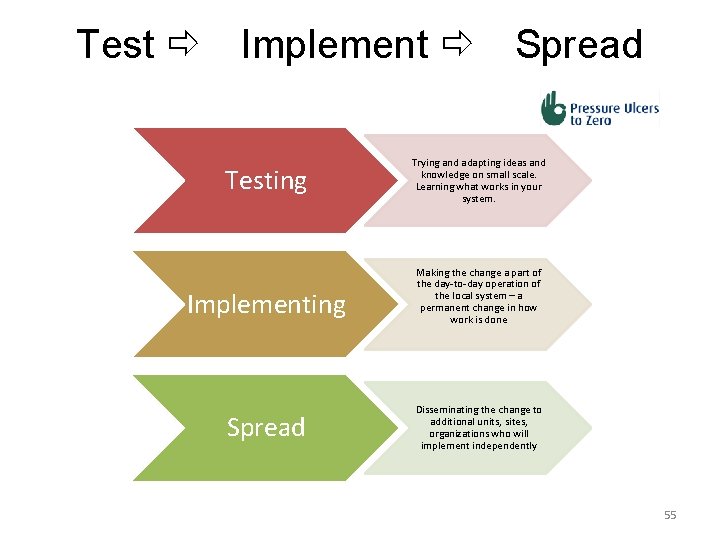
Test Implement Testing Implementing Spread Trying and adapting ideas and knowledge on small scale. Learning what works in your system. Making the change a part of the day-to-day operation of the local system – a permanent change in how work is done Disseminating the change to additional units, sites, organizations who will implement independently 55
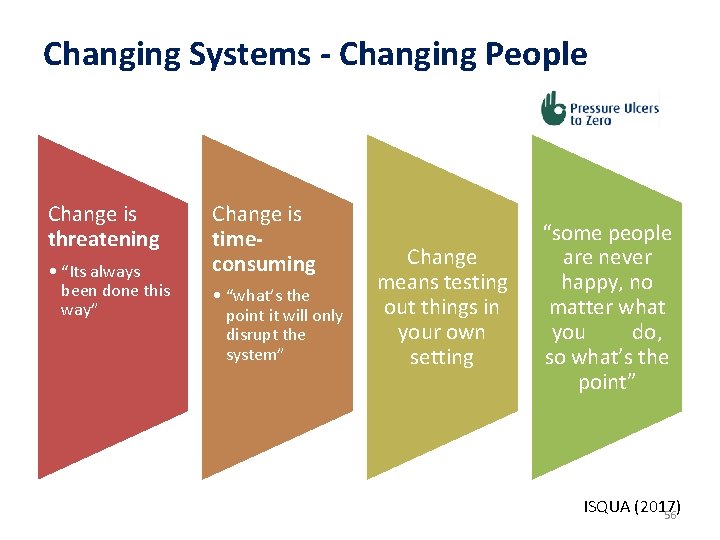
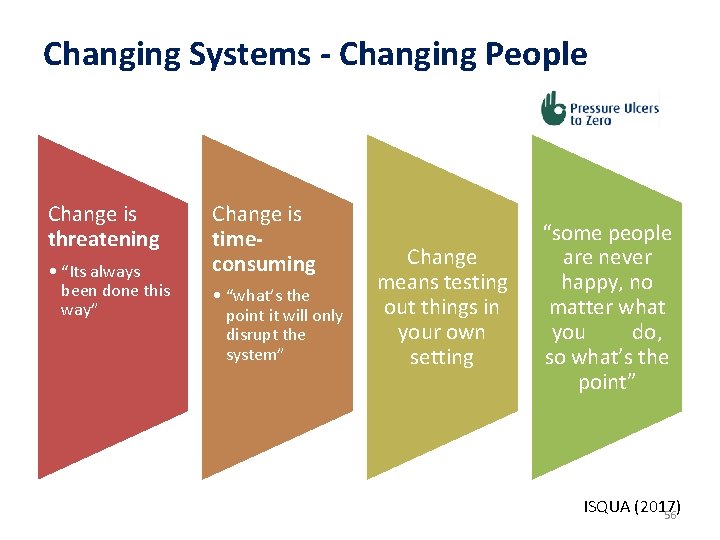
Changing Systems - Changing People Change is threatening • “Its always been done this way” Change is timeconsuming • “what’s the point it will only disrupt the system” Change means testing out things in your own setting “some people are never happy, no matter what you do, so what’s the point” ISQUA (2017) 56
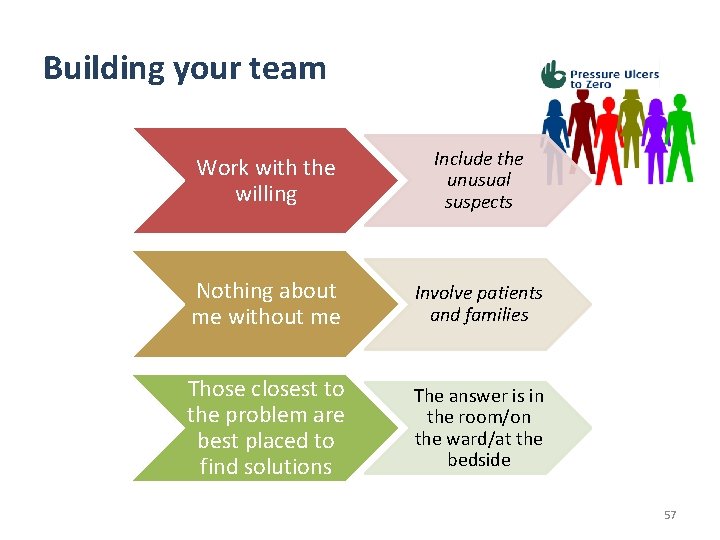
Building your team Work with the willing Include the unusual suspects Nothing about me without me Involve patients and families Those closest to the problem are best placed to find solutions The answer is in the room/on the ward/at the bedside 57
To conclude: A Commitment “It’s not enough to do your best ; you must know what to do, and then do your best” W. Edwards Deming 58
 Raft casting
Raft casting Bruno putz
Bruno putz Putz józsef
Putz józsef Integrating public health and primary care
Integrating public health and primary care Levels of nursing care primary secondary tertiary
Levels of nursing care primary secondary tertiary Blending quotations
Blending quotations Integrating quotes mla
Integrating quotes mla Integrating by parts
Integrating by parts Microsoft dynamics ax plm
Microsoft dynamics ax plm Integration of composite functions
Integration of composite functions Integrating concepts in biology
Integrating concepts in biology Integrating factor of differential equation
Integrating factor of differential equation When should firms introduce conscious marketing?
When should firms introduce conscious marketing? Key internal forces
Key internal forces Integrating sel and pbis
Integrating sel and pbis Integrating business perspectives
Integrating business perspectives Axon
Axon Knapp's model of relational development
Knapp's model of relational development Middle level integration
Middle level integration Integrating factor
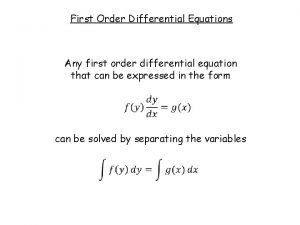
Integrating factor First ode
First ode Integrating factor exact equations
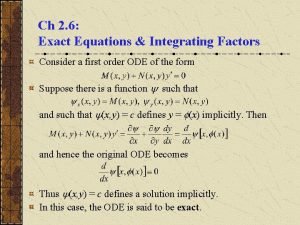
Integrating factor exact equations Integrating sources into your writing
Integrating sources into your writing Differential equation exponential solution
Differential equation exponential solution Strategic management internal assessment
Strategic management internal assessment Integrating factor of differential equation
Integrating factor of differential equation Integrating factor of linear differential equation
Integrating factor of linear differential equation Integrating qualitative and quantitative methods
Integrating qualitative and quantitative methods Project indicators enable a software project manager to
Project indicators enable a software project manager to Indirect quotation
Indirect quotation Integrating type dvm
Integrating type dvm Integration of partial differential equation
Integration of partial differential equation Integrating science and social studies
Integrating science and social studies Integrating classification and association rule mining
Integrating classification and association rule mining Integrate quotes
Integrate quotes Integrating marketing communication to build brand equity
Integrating marketing communication to build brand equity Integrating communications assessment and tactics
Integrating communications assessment and tactics Palliative care versus hospice care
Palliative care versus hospice care Hip fracture clinical care standard
Hip fracture clinical care standard Nasc pui vii
Nasc pui vii Care value base health and social care
Care value base health and social care Standard 3 duty of care
Standard 3 duty of care Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate Magneții atrag corpuri care conțin
Magneții atrag corpuri care conțin Care certificate standard 1 answers
Care certificate standard 1 answers Excess heat reduce
Excess heat reduce How to reduce cognitive dissonance in the workplace
How to reduce cognitive dissonance in the workplace Google map reduce
Google map reduce Enlarging formula
Enlarging formula Types of pulley
Types of pulley Blender reduce vertices
Blender reduce vertices External fragmentation
External fragmentation 3r reduce reuse recycle
3r reduce reuse recycle Enlarge shapes
Enlarge shapes What is the primary lever to reduce cycle inventory
What is the primary lever to reduce cycle inventory How to reduce sulfur dioxide
How to reduce sulfur dioxide Rman compression ratio
Rman compression ratio Adverbial clause
Adverbial clause Reduce funciona
Reduce funciona