Influenza Infection Fall 2017 Influenza The flu is


- Slides: 23

Influenza & Infection Fall 2017
Influenza • The flu is a highly contagious respiratory illness • Affects 5 to 20% of American population annually • Flu season is September to April –Peak November to March • 20, 000 deaths annually • Vaccination of high-risk groups can prevent many of these deaths
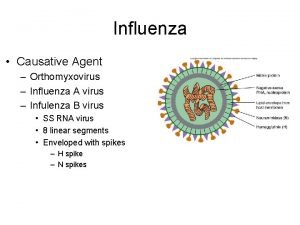
Influenza • 3 serotypes of influenza viruses • A, B, C; A & B cause significant illness in humans • Type A is most virulent • • May mutate from animals to humans Transmission via direct or indirect contact with infected animals Epidemic and/or pandemic may occur Human transmission primarily droplet and inhaled aerosolized particles
Influenza • Incubation of 1 to 4 days • Peak transmission 1 day prior to onset of symptoms and continues for 5 to 7 days after a person first becomes sick • The most effective management strategy is prevention!
Influenza • Onset abrupt • • Cough, fever, myalgia, HA, fatigue, exhaustion Dyspnea and crackles = signs of pulmonary complications Usually symptoms subside within 7 days Most common complication: pneumonia • High risk: elderly and chronic disease • Diagnosis • Rapid flu test (nasal secretions) • Office or lab, results same day

Influenza • Who should not be vaccinated? • History of Guillain-Barre syndrome • Allergy to eggs (? ) • Transmission • Health care workers can transmit to our patients • Don’t expose our patients to this! • Get immunized! • Effectiveness • Different every year; two weeks for full protection
Influenza • Treatment • Symptomatic therapy & prevent secondary infection • Rest, hydration, analgesics and antipyretics (older adult possible hospitalization) • Antivirals (Tamiflu) • Shorten duration of the flu • Reduce the risk of complications
Infections Emerging & Reemerging
Emerging Infections • Ebola • H 1 N 1 • HIV • West Nile virus • Zika
Zika • Brazil reported the first cases of local transmission in May 2015. • Mosquitoes are the main vector for Zika transmission. • There is no prevention or treatment for the infection. • Travelers are urged to prevent mosquito bites by using repellent (DEET) and covering exposed skin. • Travelers need to reapply repellent often.
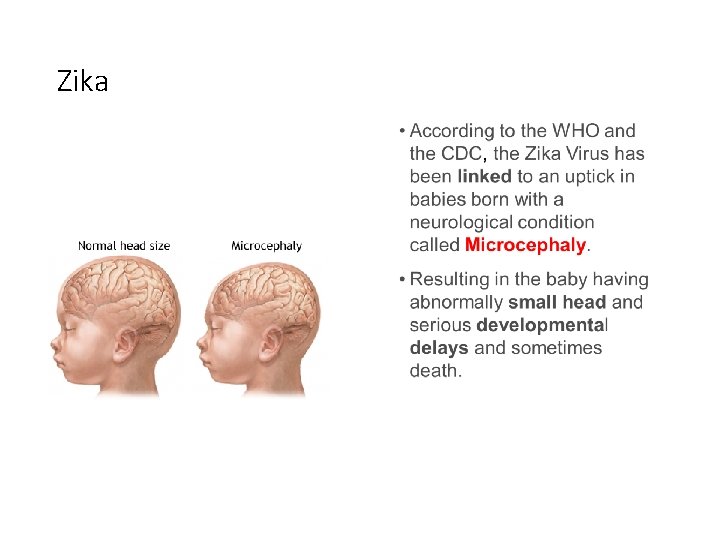
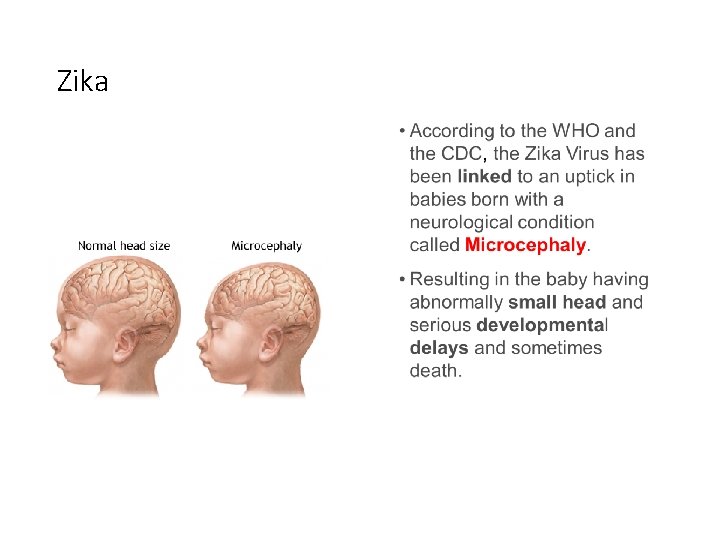
Zika
Zika • Signs and Symptoms • • Mild fever Skin rash Conjunctivitis Symptoms last for 2 -7 days • Treatment • Drink plenty of fluids • Treat pain and fever • No current vaccine
Zika • Prevention • • Repellent with DEET-reapply prn Bed nets Clothing barriers Avoidance
Ebola • First seen in 1976 and again in 2014 • Causes hemorrhagic fever • Usually lethal • Reservoir and path of transmission are unknown • Impossible to combat the virus and diseases it causes
Ebola • From the CDC • PLEASE see the posted pdf Ebola Basics from the CDC • • How is Ebola NOT spread? How is Ebola spread? What are the early symptoms of Ebola? When is someone contagious? • Why do patient’s die from this virus?
Reemerging Infections • Diphtheria • Pertussis • Tuberculosis • HIV population • International travel – • Low vaccination rates in developing countries • Measles
Antibiotic Resistant • MRSA-organism remains viable for days on environmental surfaces and clothing • HA MRSA or CA MRSA • VRE – remains viable for weeks on environmental surfaces • Resistant strains initially seen in health care settings (HA), but now also in community (CA) • Patient teaching is important
Why is this happening? • Health-care providers contribution • Administering antibiotics for viral infections • Succumbing to pressures from patients to prescribe unnecessary antibiotic therapy • Using inadequate drug regimens to treat infections • Using broad-spectrum or combination agents for infections that should be treated with first-line medications
Why is this happening? • Patients contribution • • Skipping doses Not taking antibiotics for the full duration Saving unused antibiotics “in case I need them later” Limited resources and access to medications make it difficult for some to get adequate treatment
Patient Teaching Decrease Risk for Antibiotic-Resistant Infection 1) 2) 3) 4) 5) 6) Do not take antibiotics to prevent illness Wash your hands frequently Follow directions when taking antibiotics Do not request an antibiotic for flu or colds Finish your antibiotic Do not take leftover antibiotics
Health Care-Associated Infections • Formerly known as “nosocomial infections”— infection acquired in health care setting • Surgical and immunocompromised patients at highest risk • Multiple organisms are responsible
Infections in Older Adults • Rate is 2 -3 times higher for HAI’s • Risk factors • Age related changes • Co-morbidities • Long term care facilities • Common infections • Pneumonia, UTI’s; TB; skin infections • Atypical presentations • Suspect when change in ADL’s or cognitive function
 Stomach flu vs influenza
Stomach flu vs influenza 2017 dvhimss annual fall conference
2017 dvhimss annual fall conference Mec flu
Mec flu Decoding the flu case study answers
Decoding the flu case study answers The european economy
The european economy Oraciones con fla fle fli flo flu
Oraciones con fla fle fli flo flu Flu timeline
Flu timeline Palabras con pla ple pli plo plu
Palabras con pla ple pli plo plu Suppose a student carrying a flu virus
Suppose a student carrying a flu virus Causative organism
Causative organism Flu produit chimique
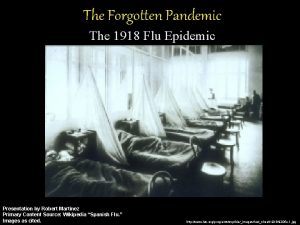
Flu produit chimique Spanish flu
Spanish flu Flu root word definition
Flu root word definition Spanish flu
Spanish flu Flu definition
Flu definition Flu watch canada
Flu watch canada Homophone of tail
Homophone of tail Enunciados con xa xe xi xo xu
Enunciados con xa xe xi xo xu Flu
Flu Influenza ww1
Influenza ww1 Spinte metallostatiche
Spinte metallostatiche Is influenza a airborne disease
Is influenza a airborne disease Influenza virus replication
Influenza virus replication The great influenza rhetorical analysis
The great influenza rhetorical analysis