Human Reproduction Topic 11 4 Human Reproduction Males



- Slides: 36
Human Reproduction Topic 11. 4
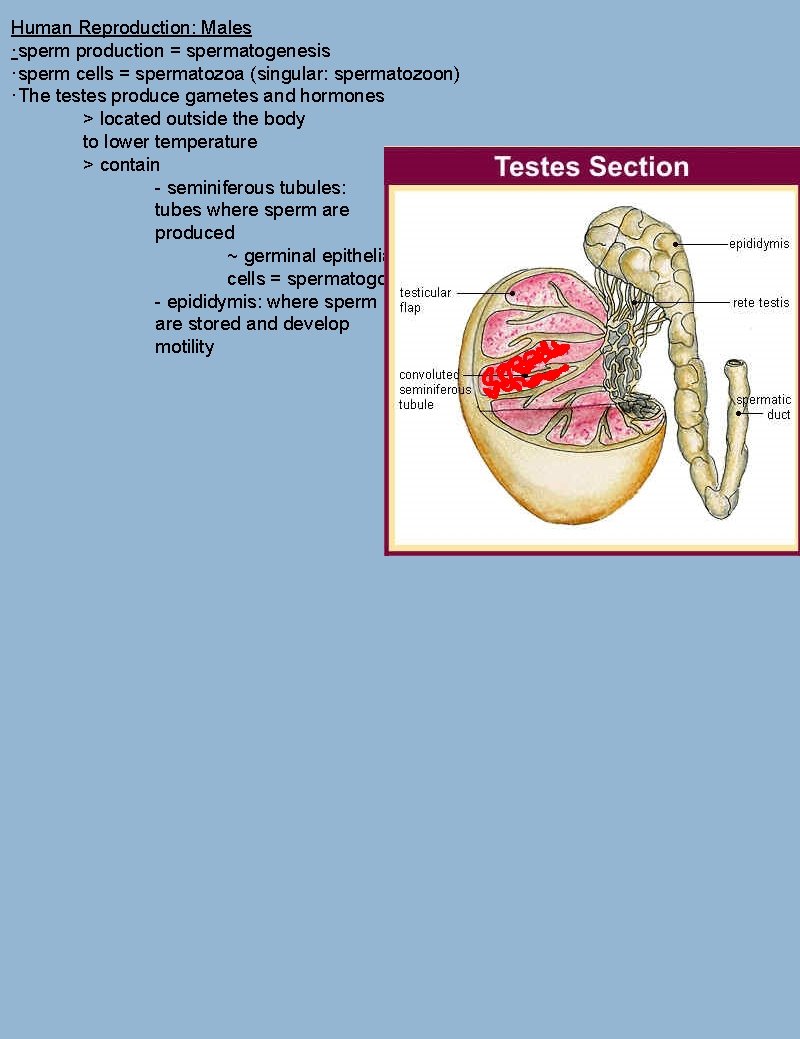
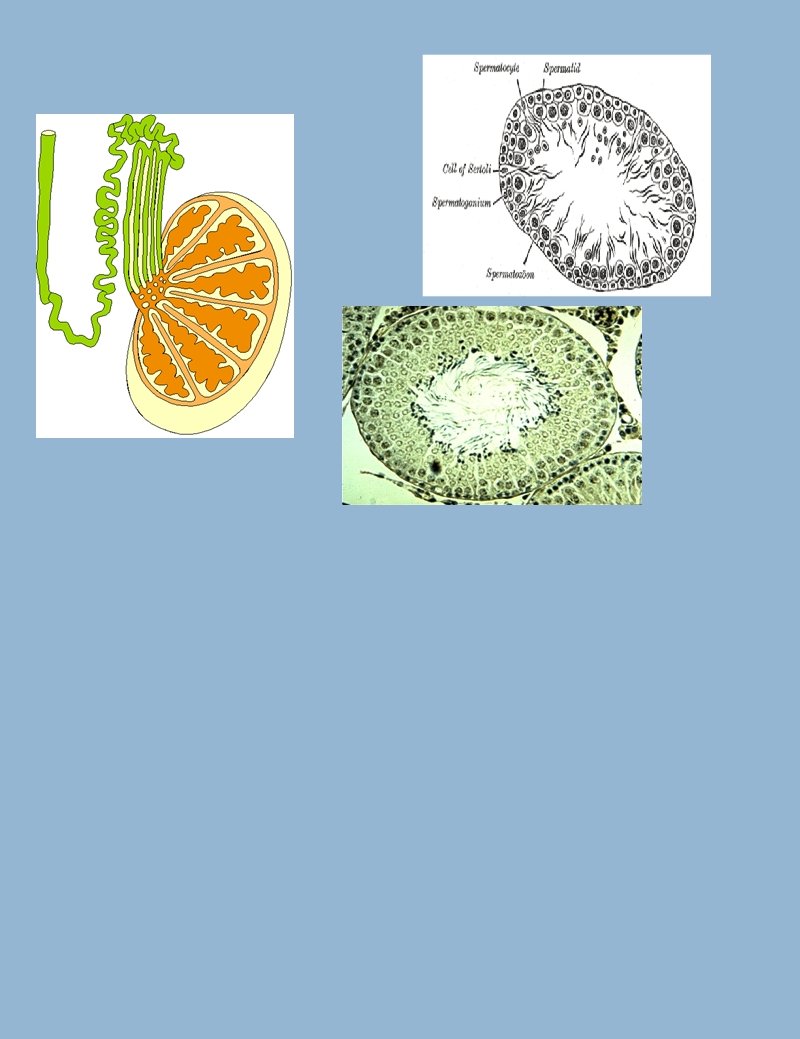
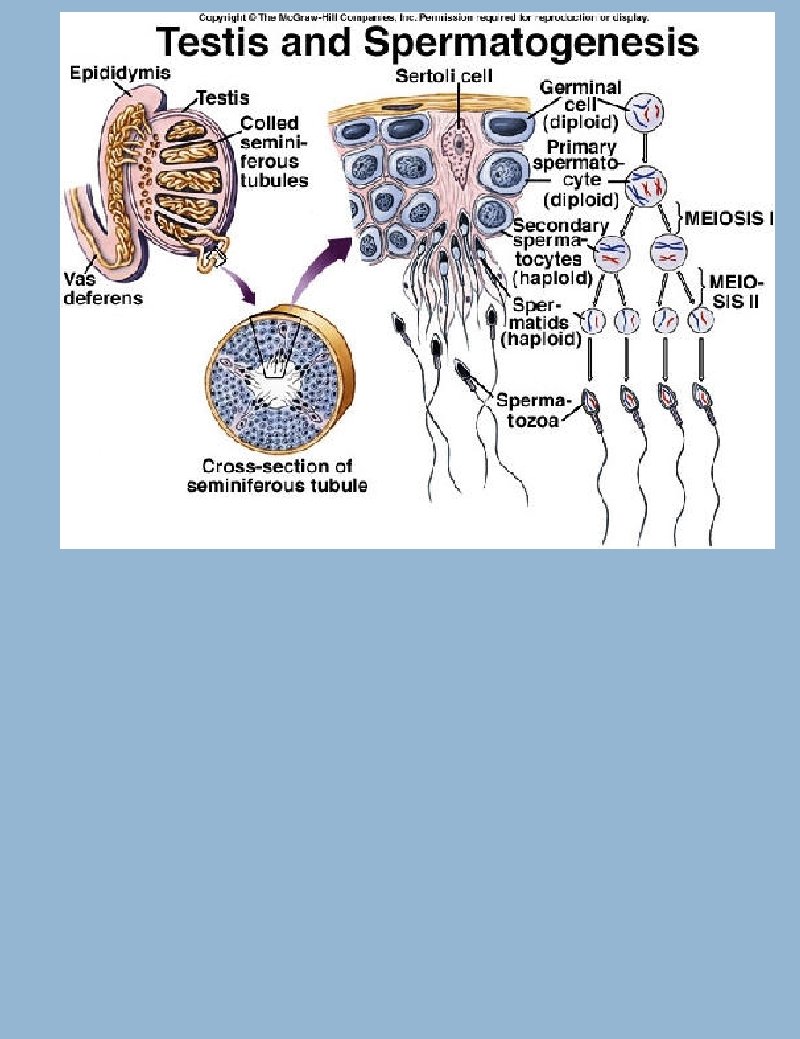
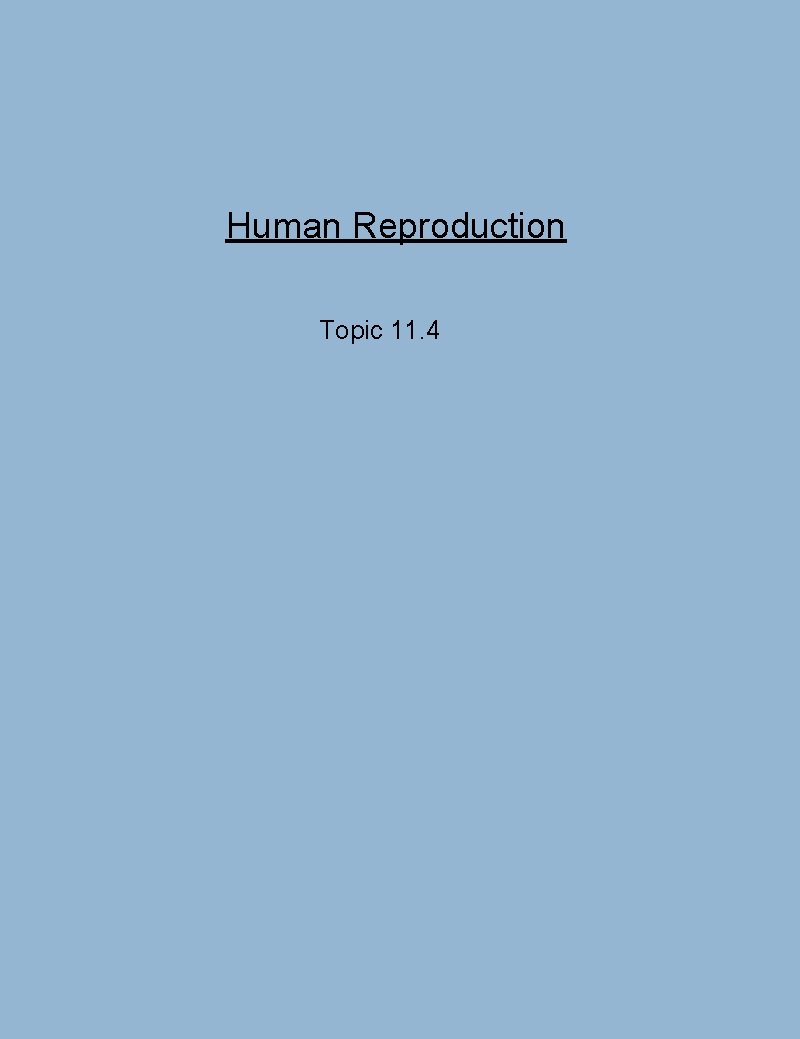
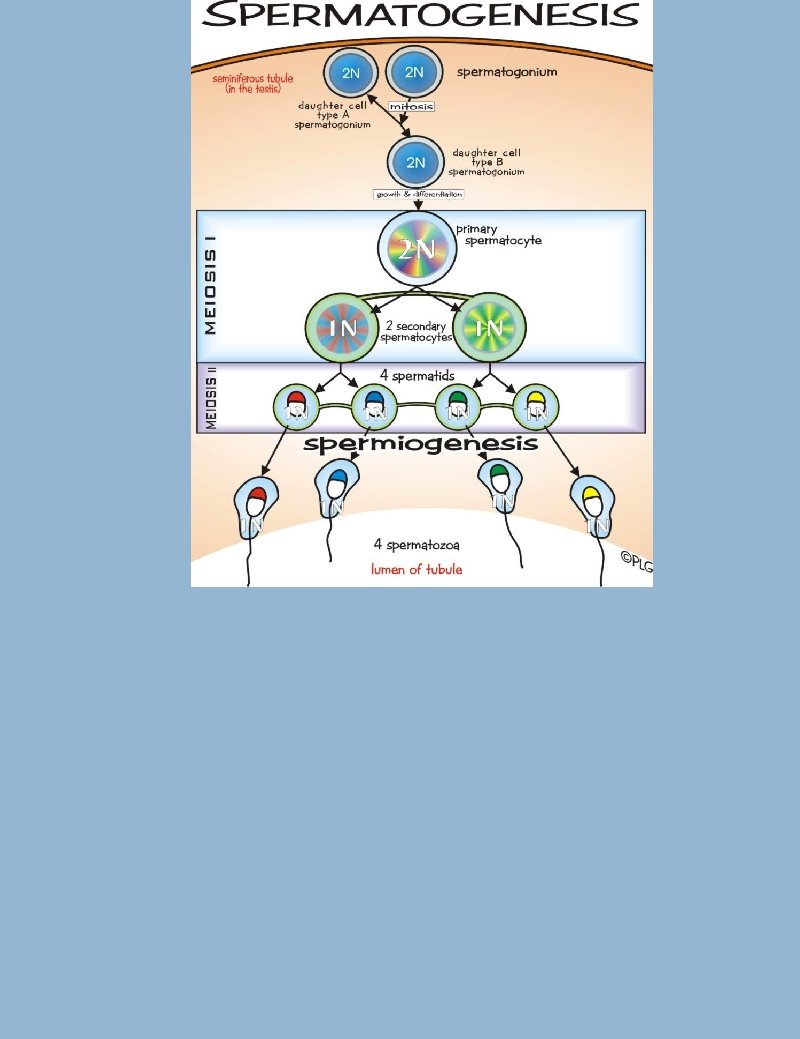
Human Reproduction: Males ·sperm production = spermatogenesis ·sperm cells = spermatozoa (singular: spermatozoon) ·The testes produce gametes and hormones > located outside the body to lower temperature > contain - seminiferous tubules: tubes where sperm are produced ~ germinal epithelial cells = spermatogonia - epididymis: where sperm are stored and develop motility
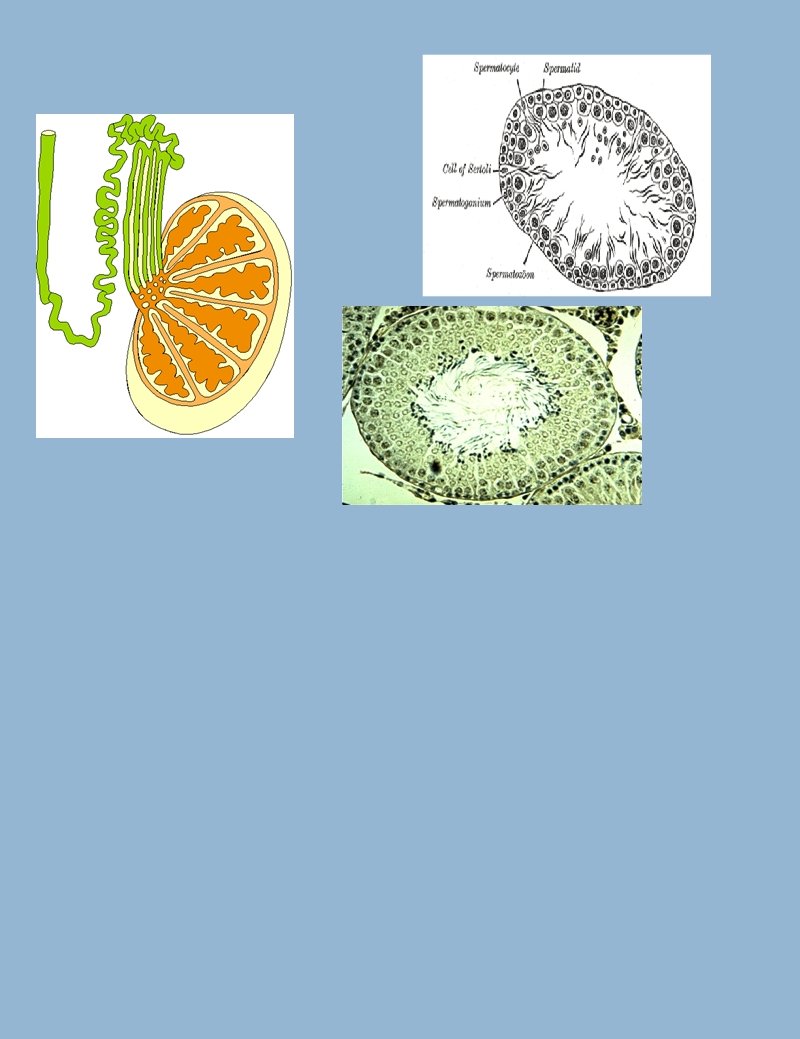
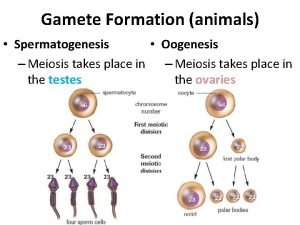
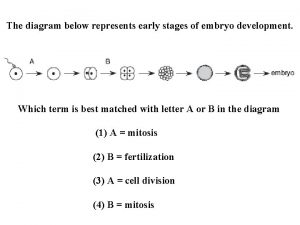
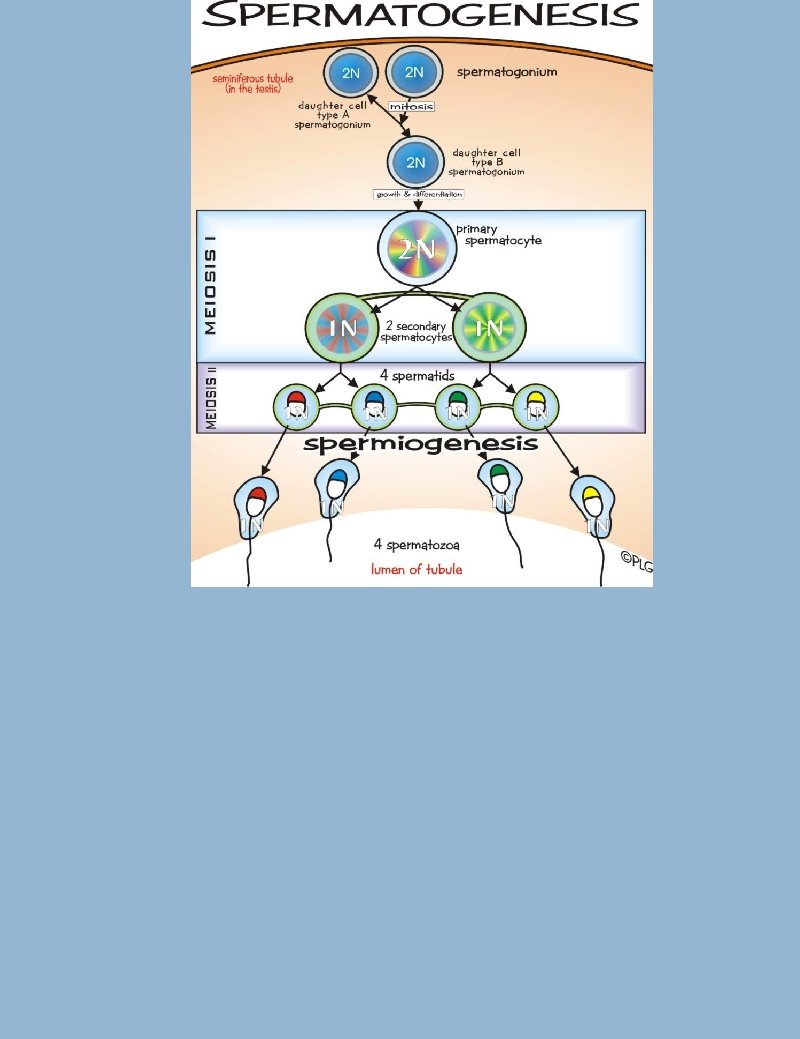
Spermatogenesis and cell division ·Mitosis: > spermatogonia undergo mitosis to replenish their numbers. > millions of sperm are produced daily after puberty > after mitosis two half sized diploid cells are produces that can then grow. ·Meiosis: > spermatogonia undergo meiosis to produce spermatozoa (singular spermatozoon) > after meiosis 4 very small haploid cells are produced.
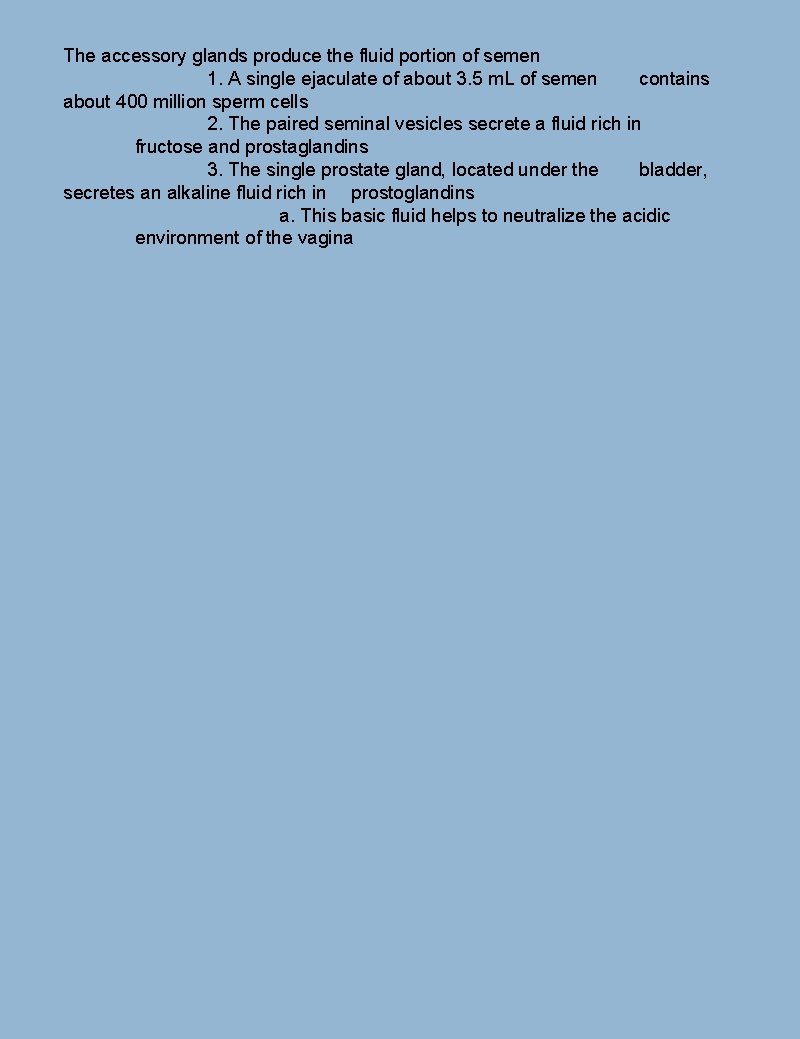
The accessory glands produce the fluid portion of semen 1. A single ejaculate of about 3. 5 m. L of semen contains about 400 million sperm cells 2. The paired seminal vesicles secrete a fluid rich in fructose and prostaglandins 3. The single prostate gland, located under the bladder, secretes an alkaline fluid rich in prostoglandins a. This basic fluid helps to neutralize the acidic environment of the vagina
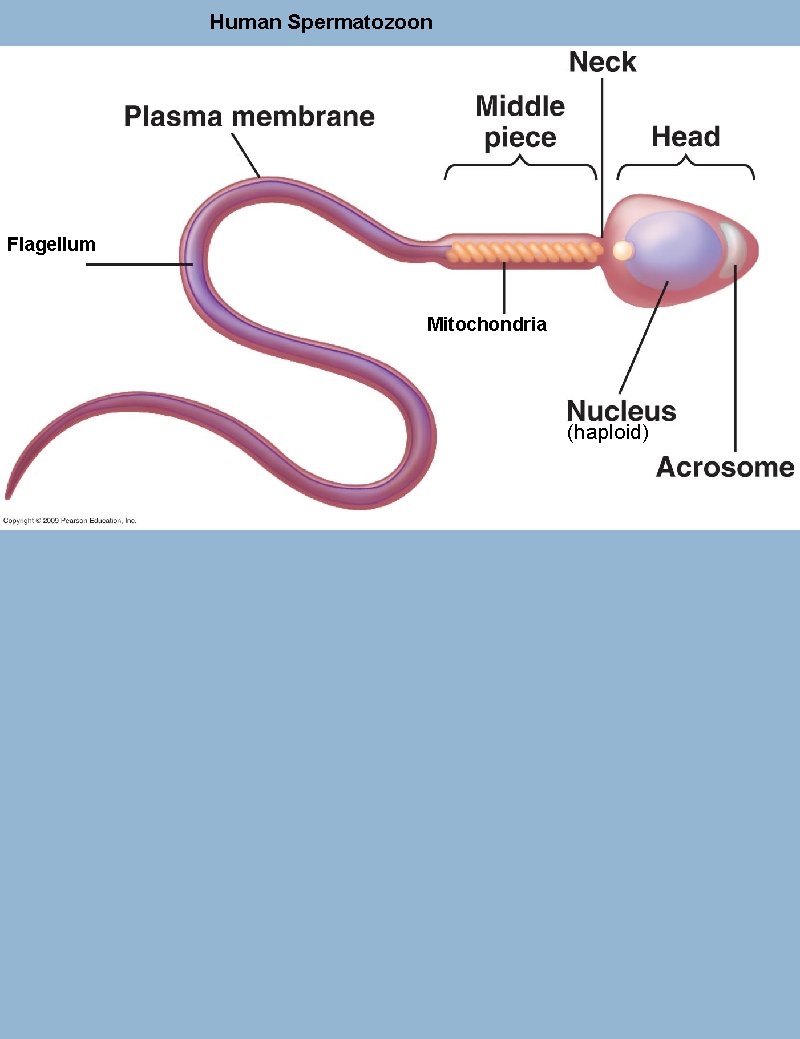
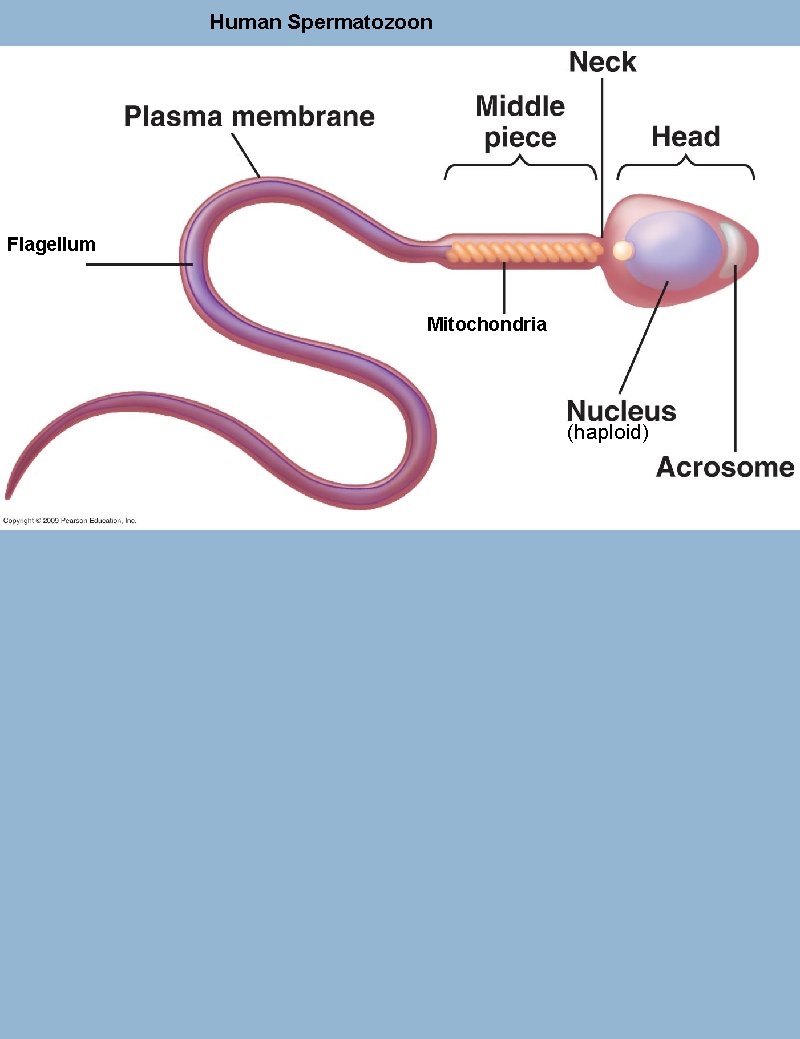
Human Spermatozoon Flagellum Mitochondria (haploid)
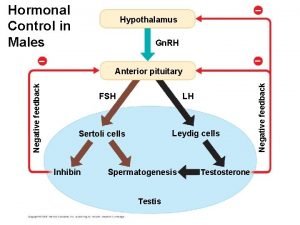
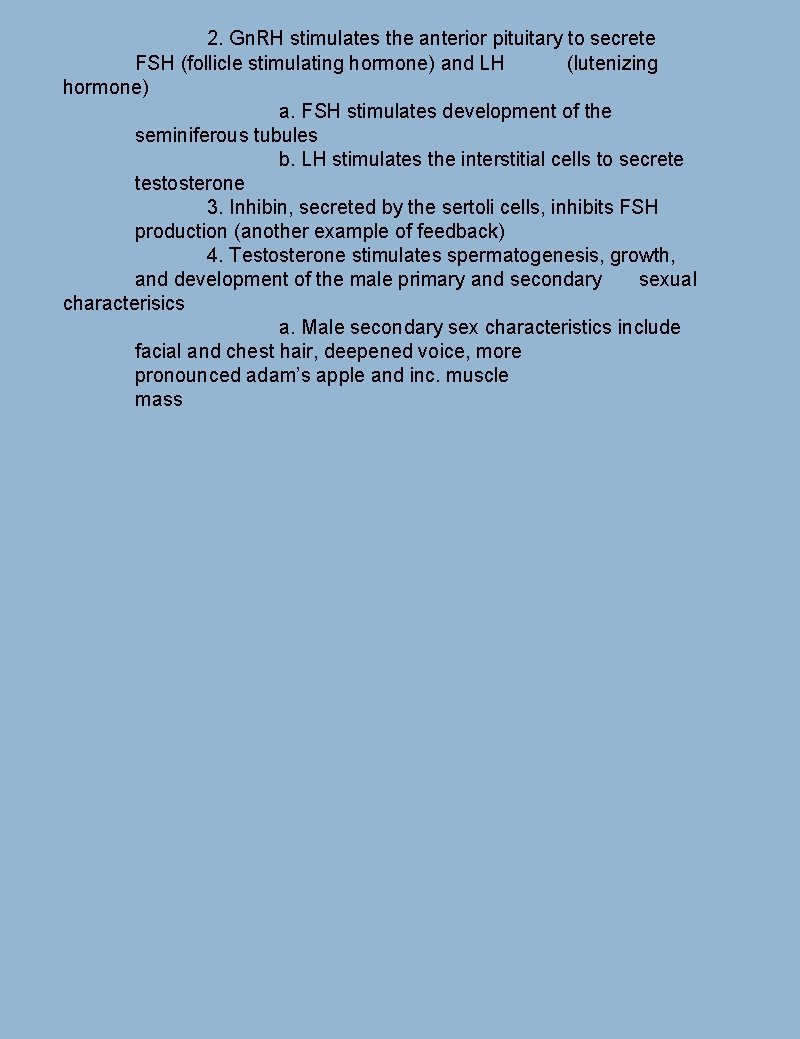
2. Gn. RH stimulates the anterior pituitary to secrete FSH (follicle stimulating hormone) and LH (lutenizing hormone) a. FSH stimulates development of the seminiferous tubules b. LH stimulates the interstitial cells to secrete testosterone 3. Inhibin, secreted by the sertoli cells, inhibits FSH production (another example of feedback) 4. Testosterone stimulates spermatogenesis, growth, and development of the male primary and secondary sexual characterisics a. Male secondary sex characteristics include facial and chest hair, deepened voice, more pronounced adam’s apple and inc. muscle mass
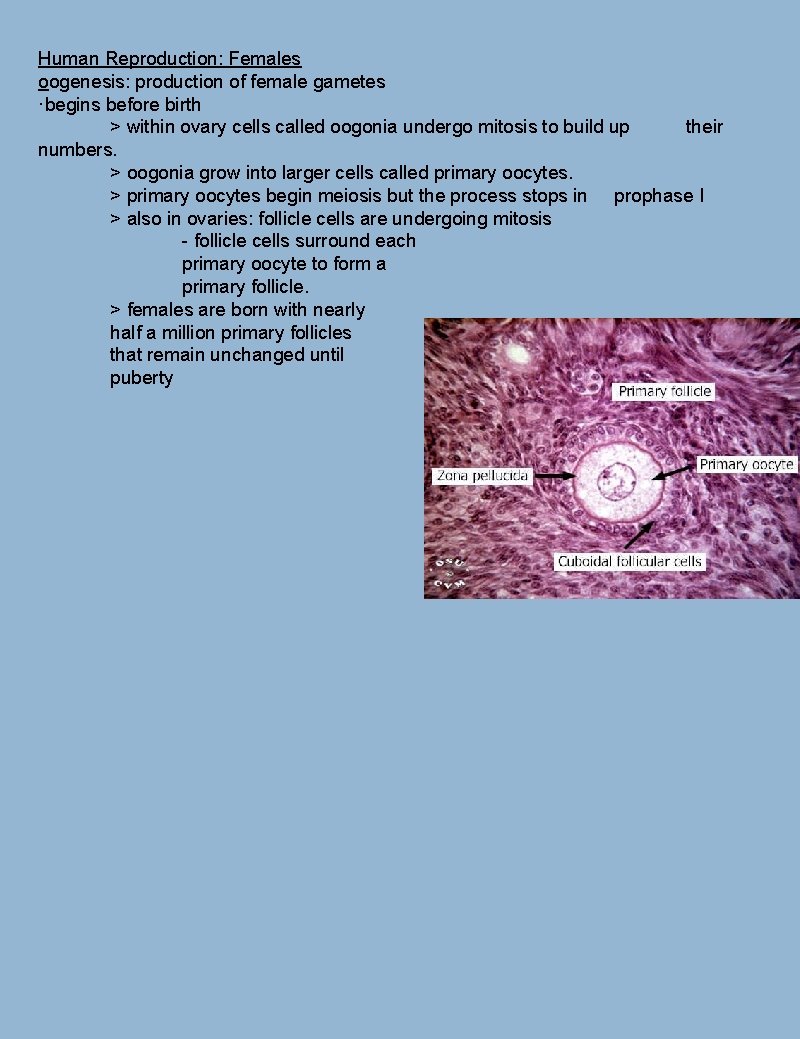
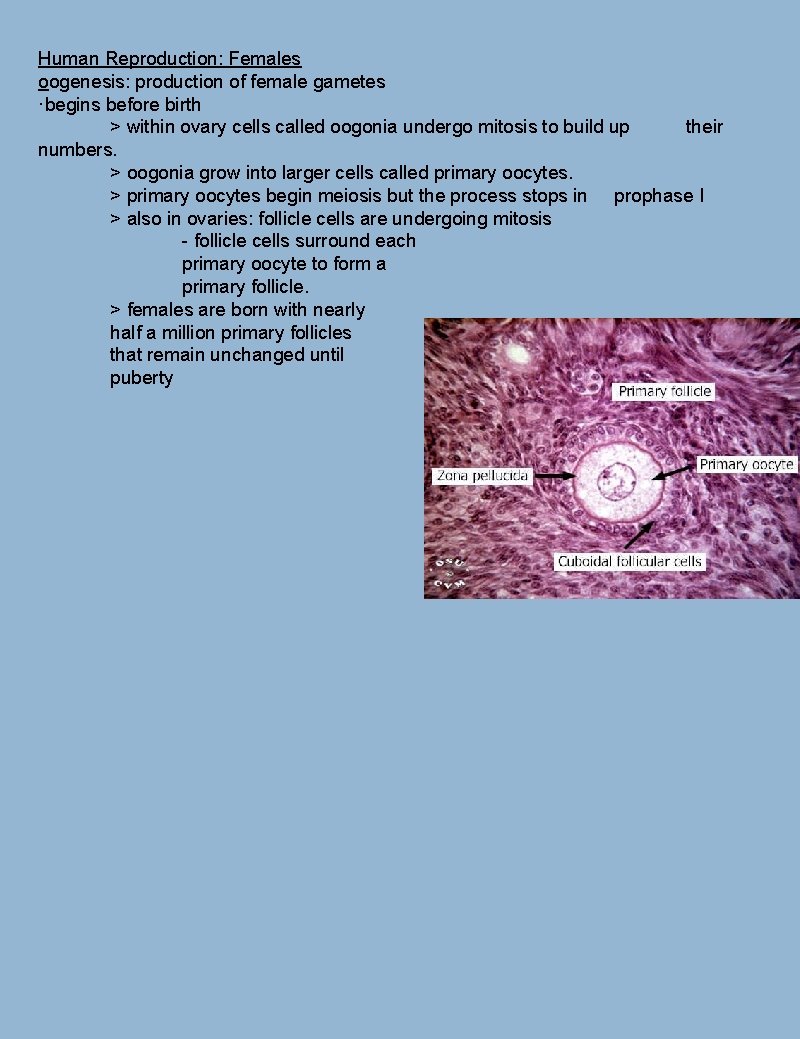
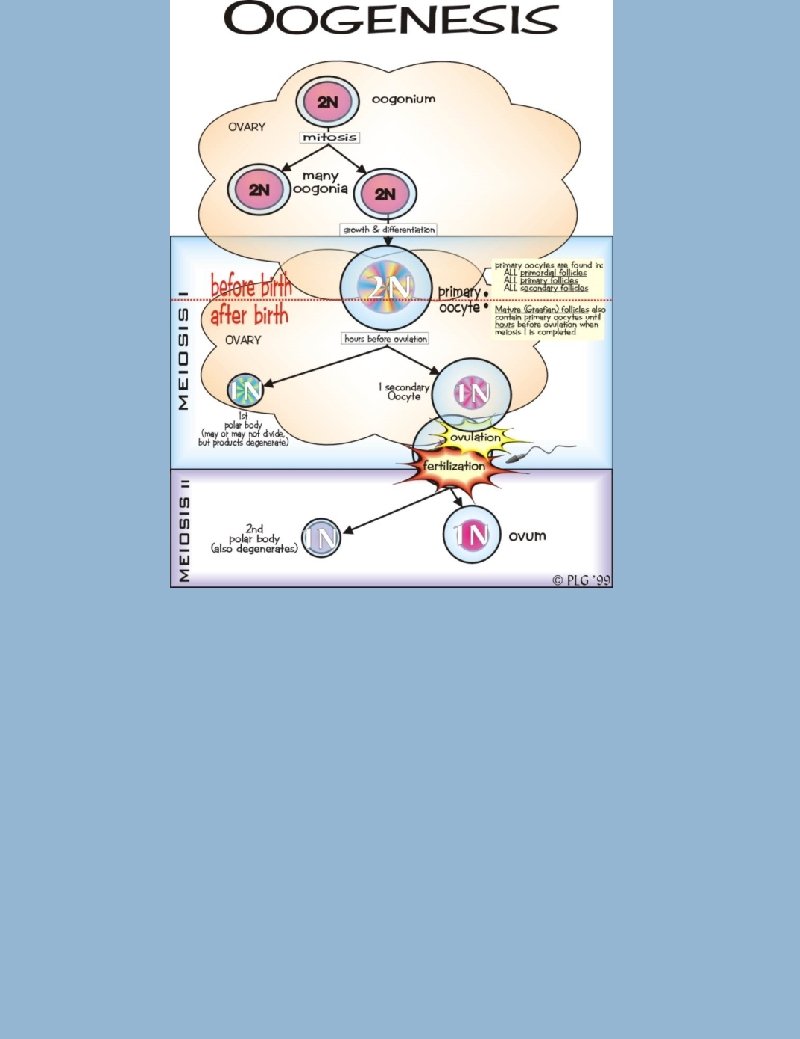
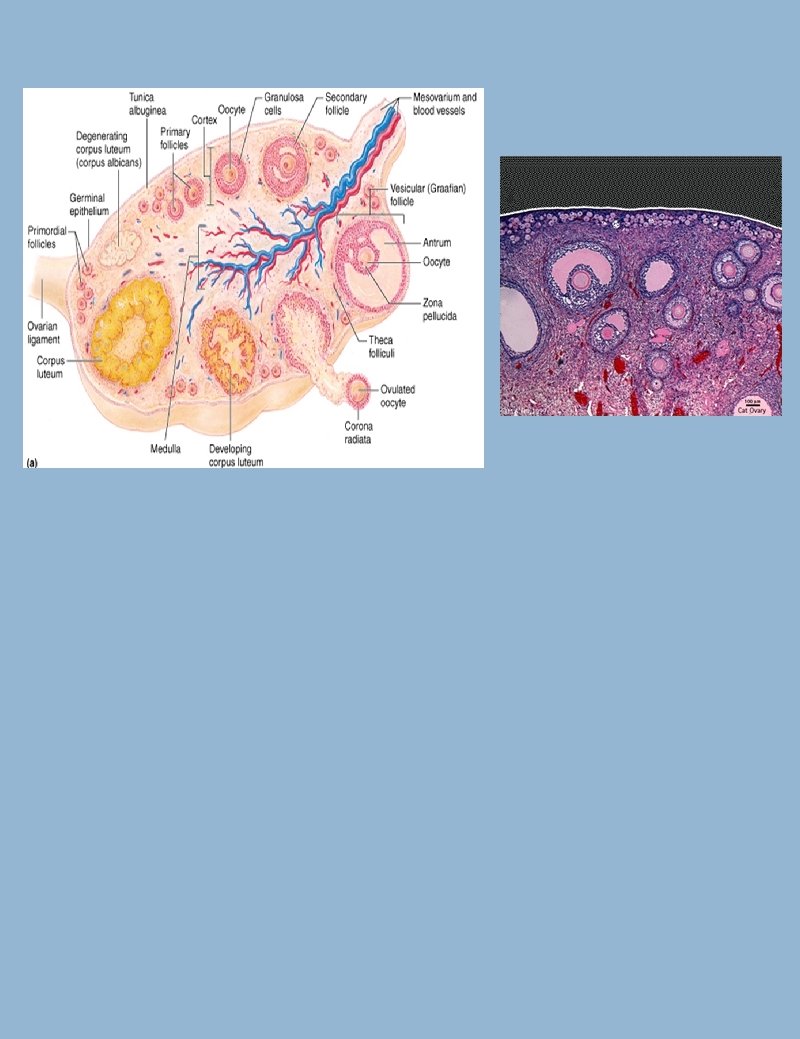
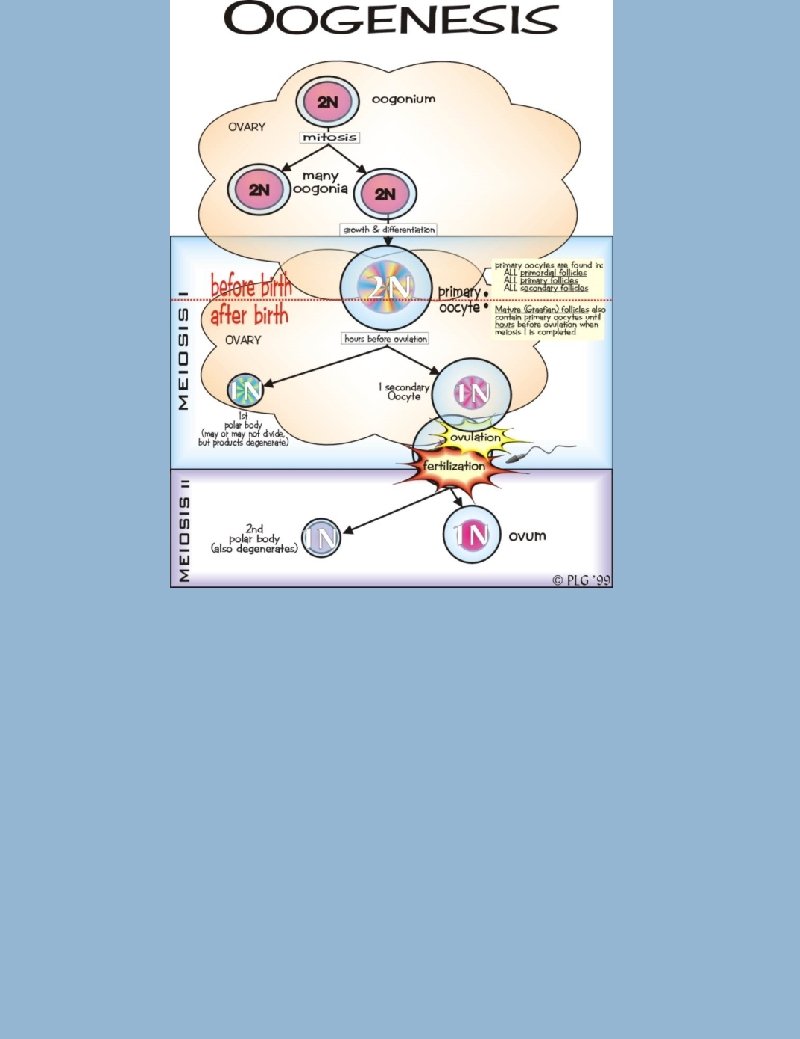
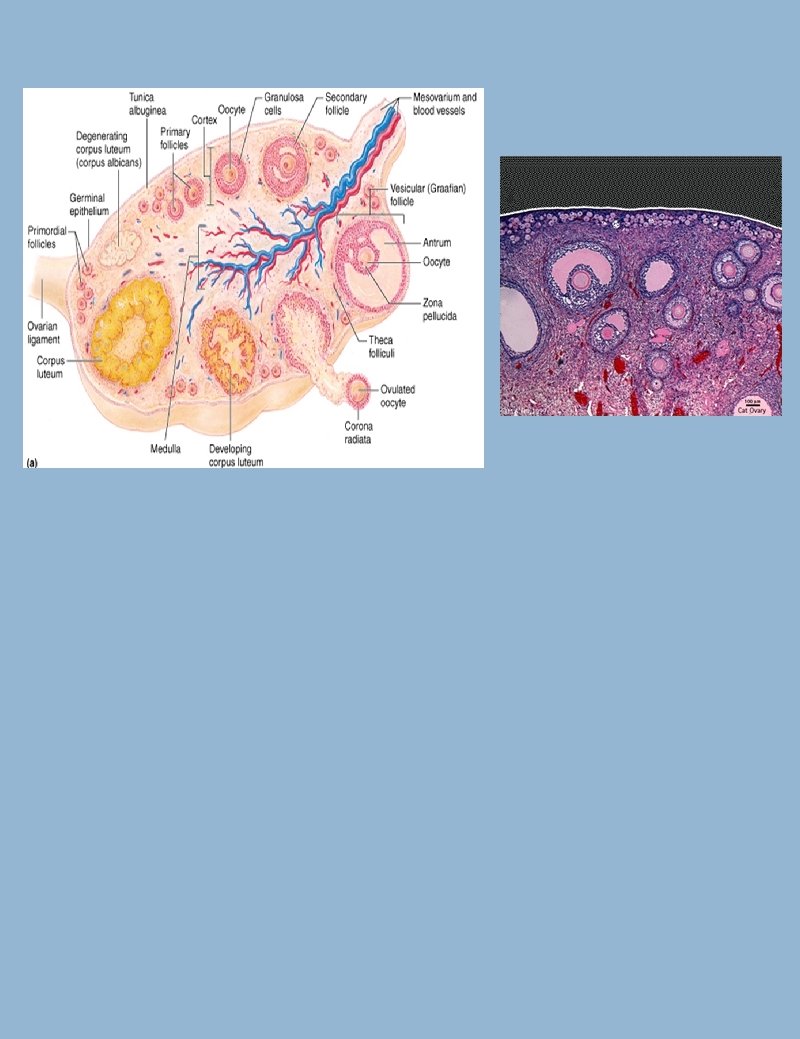
Human Reproduction: Females oogenesis: production of female gametes ·begins before birth > within ovary cells called oogonia undergo mitosis to build up their numbers. > oogonia grow into larger cells called primary oocytes. > primary oocytes begin meiosis but the process stops in prophase I > also in ovaries: follicle cells are undergoing mitosis - follicle cells surround each primary oocyte to form a primary follicle. > females are born with nearly half a million primary follicles that remain unchanged until puberty
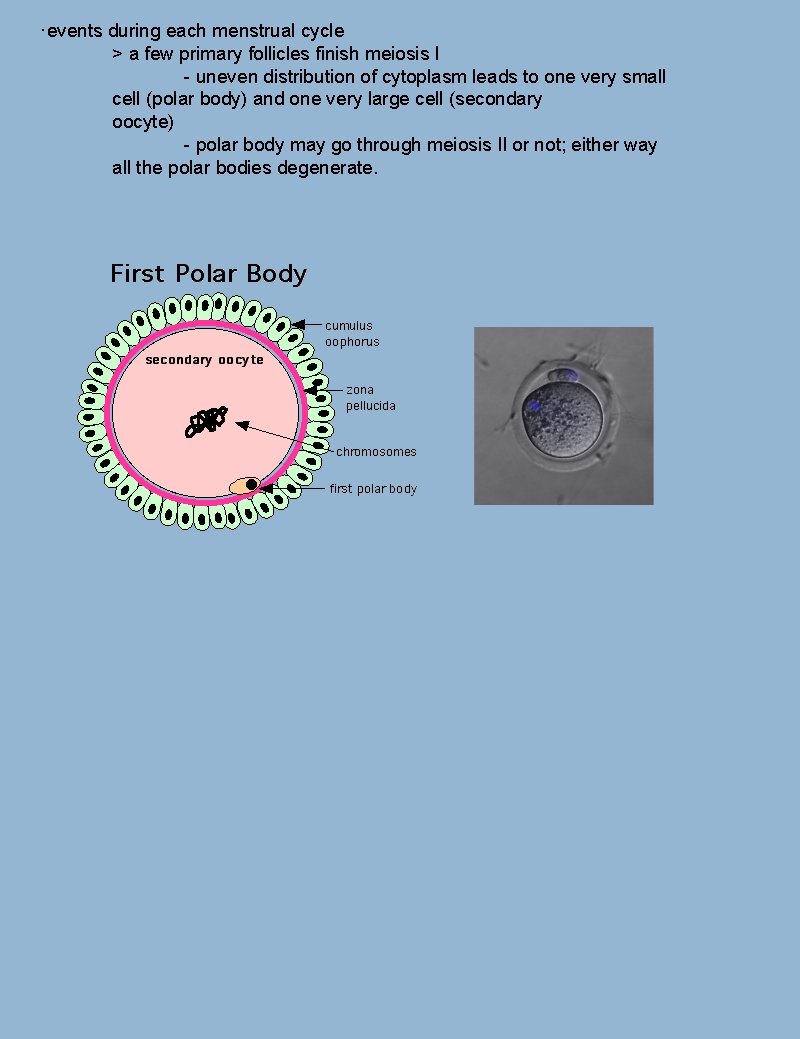
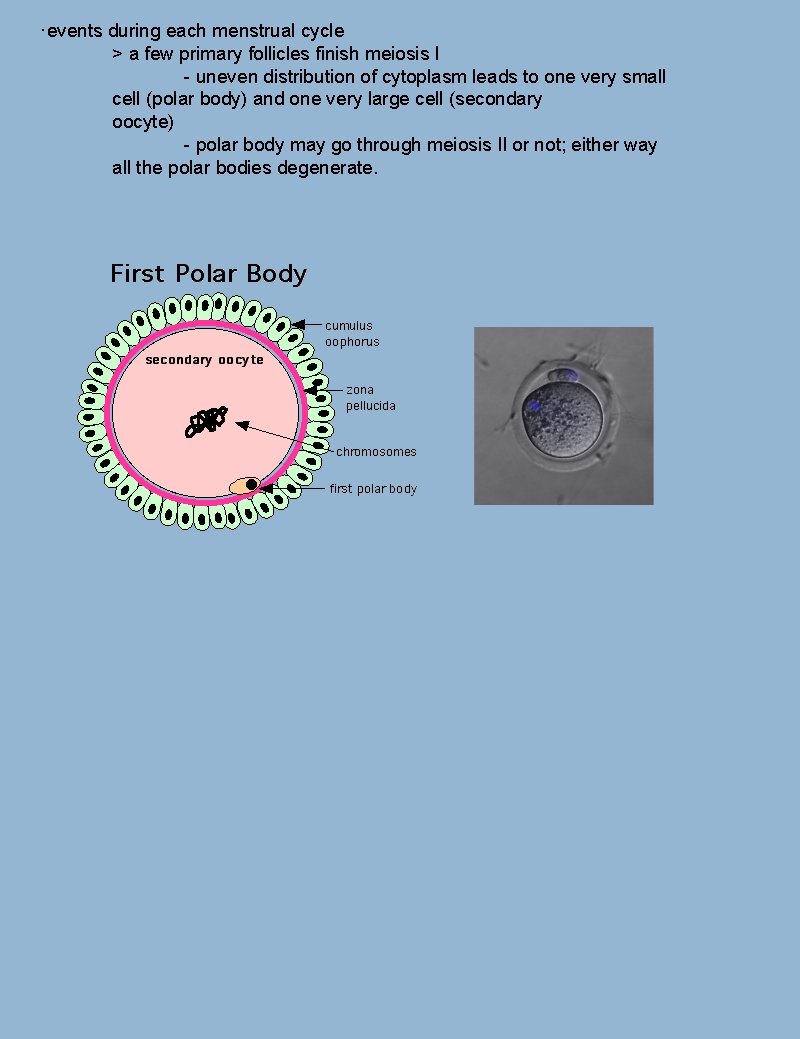
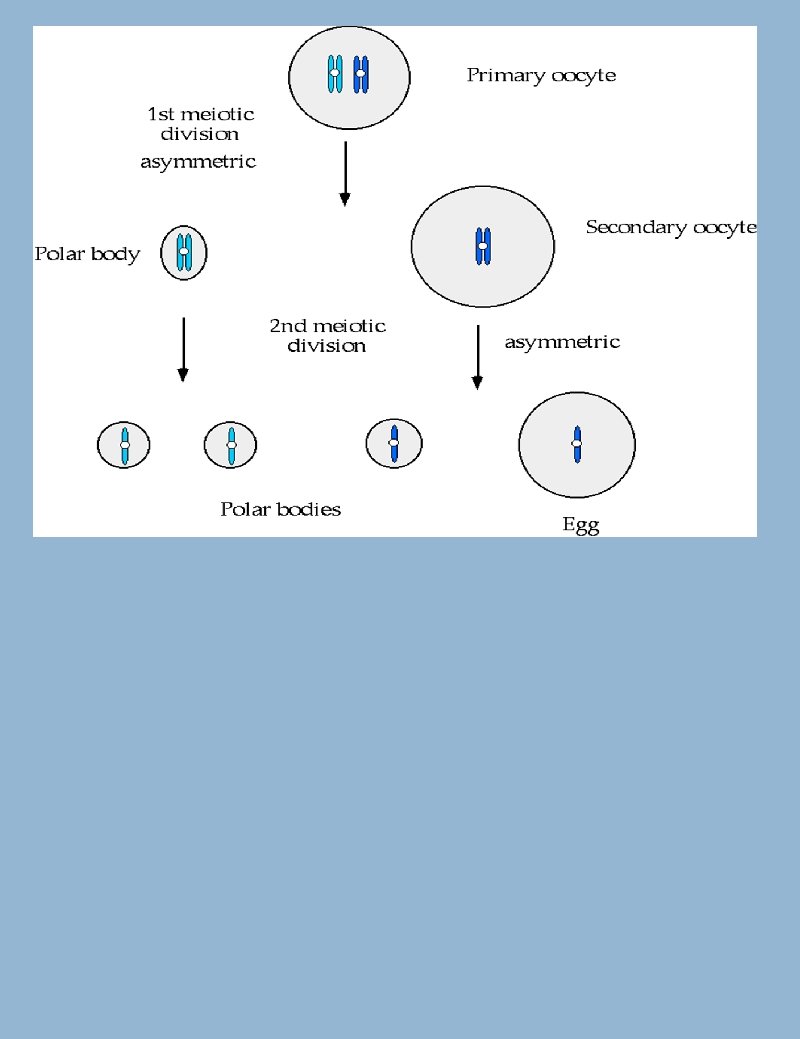
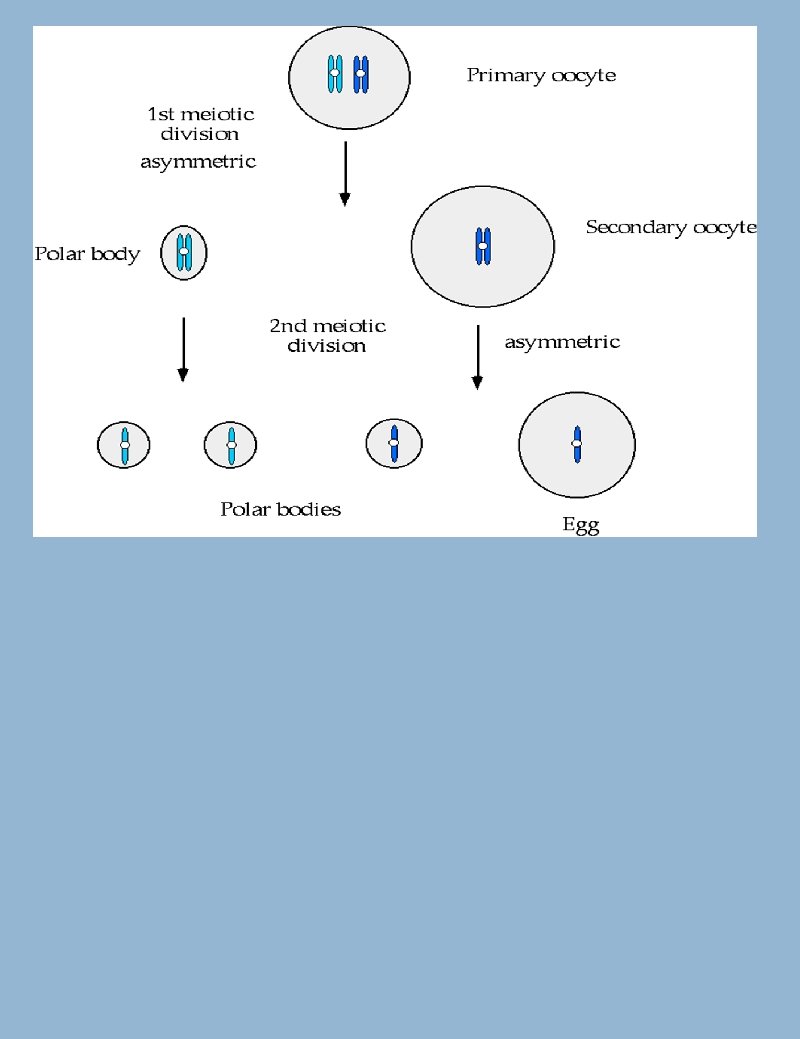
·events during each menstrual cycle > a few primary follicles finish meiosis I - uneven distribution of cytoplasm leads to one very small cell (polar body) and one very large cell (secondary oocyte) - polar body may go through meiosis II or not; either way all the polar bodies degenerate.
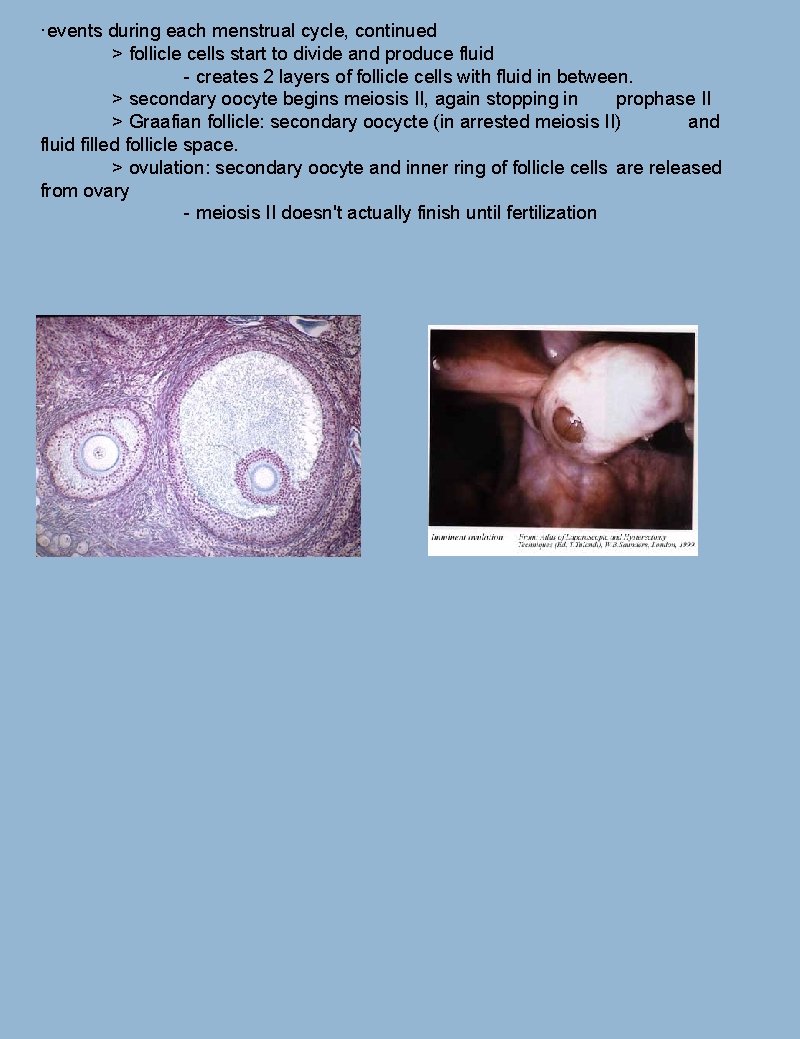
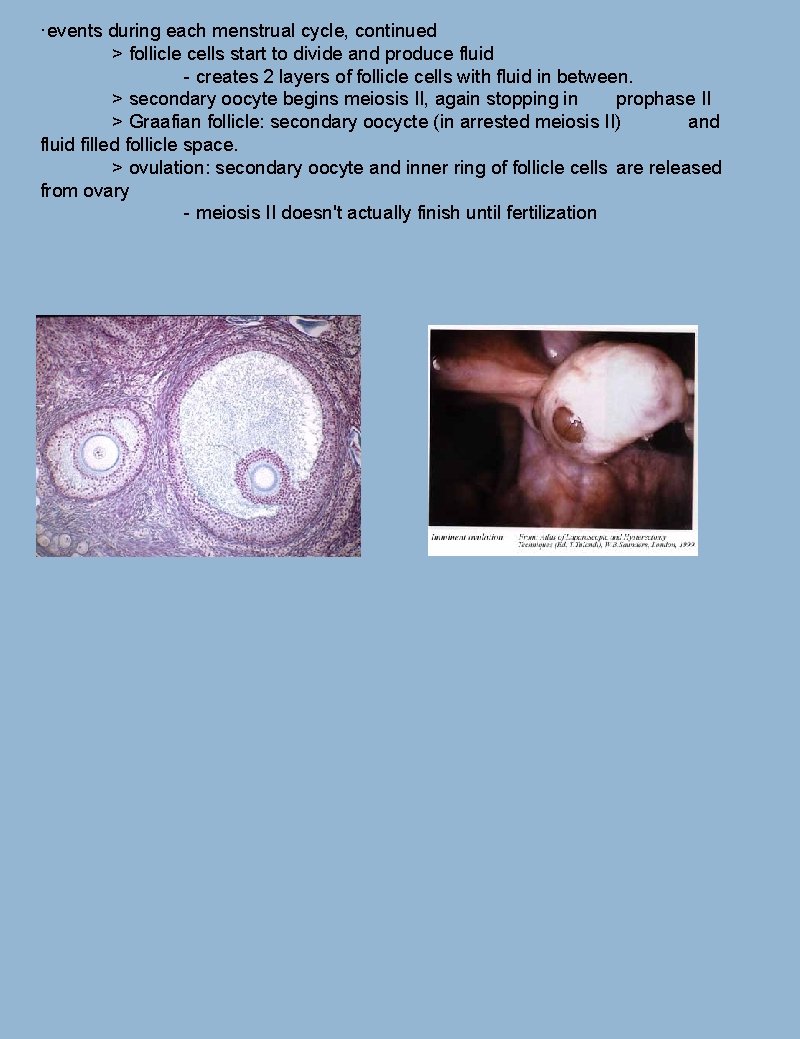
·events during each menstrual cycle, continued > follicle cells start to divide and produce fluid - creates 2 layers of follicle cells with fluid in between. > secondary oocyte begins meiosis II, again stopping in prophase II > Graafian follicle: secondary oocycte (in arrested meiosis II) and fluid filled follicle space. > ovulation: secondary oocyte and inner ring of follicle cells are released from ovary - meiosis II doesn't actually finish until fertilization
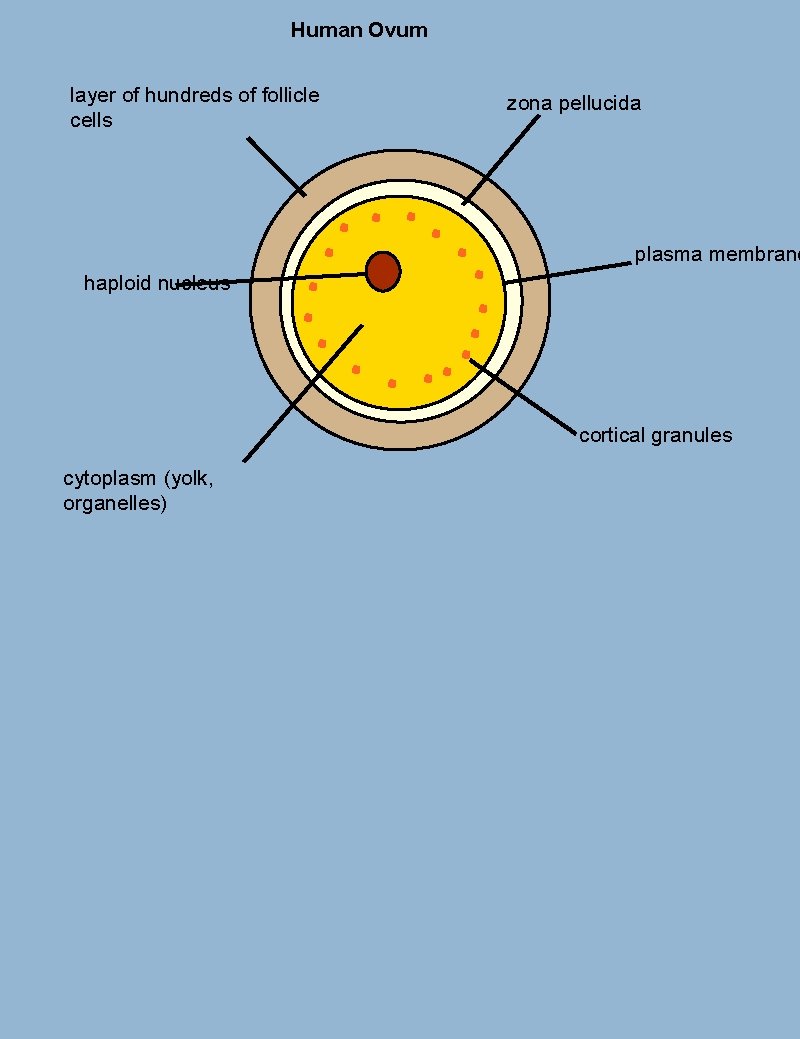
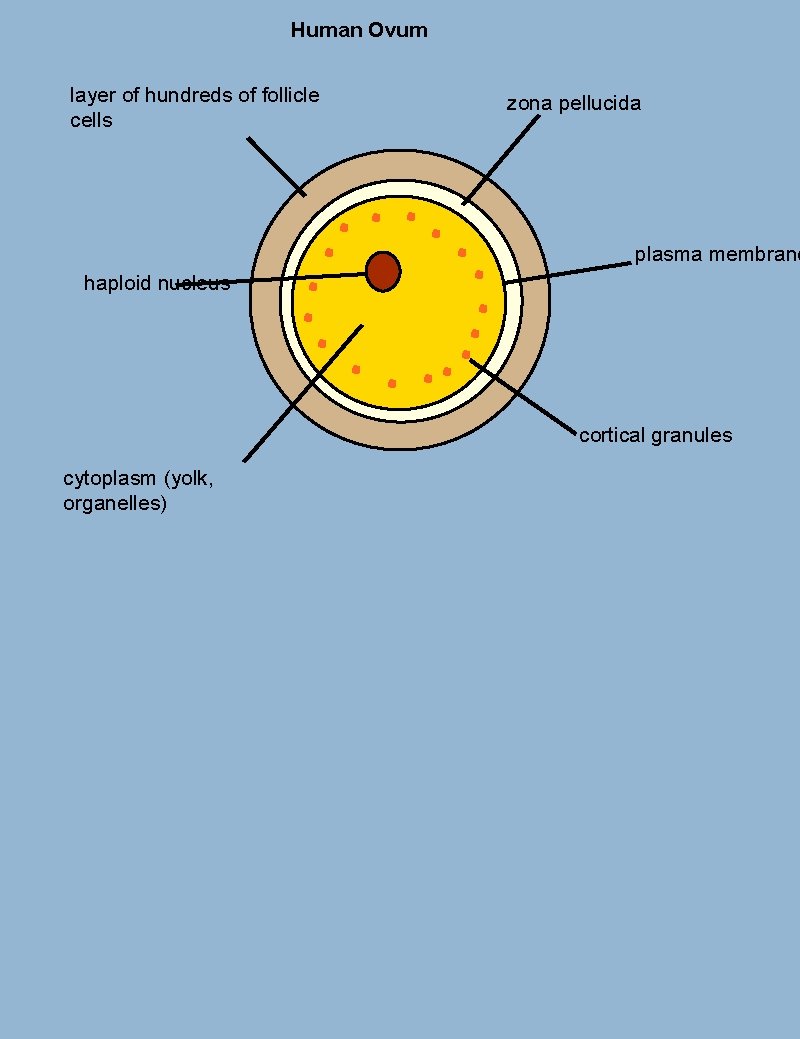
Human Ovum layer of hundreds of follicle cells zona pellucida plasma membrane haploid nucleus cortical granules cytoplasm (yolk, organelles)
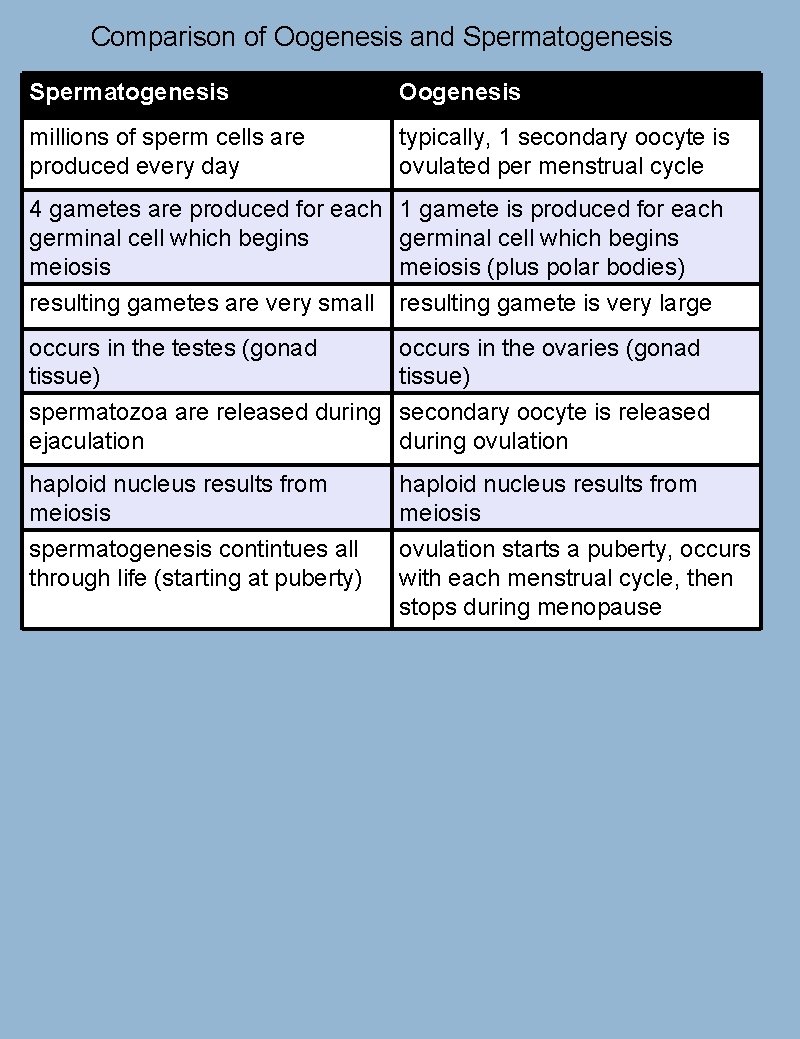
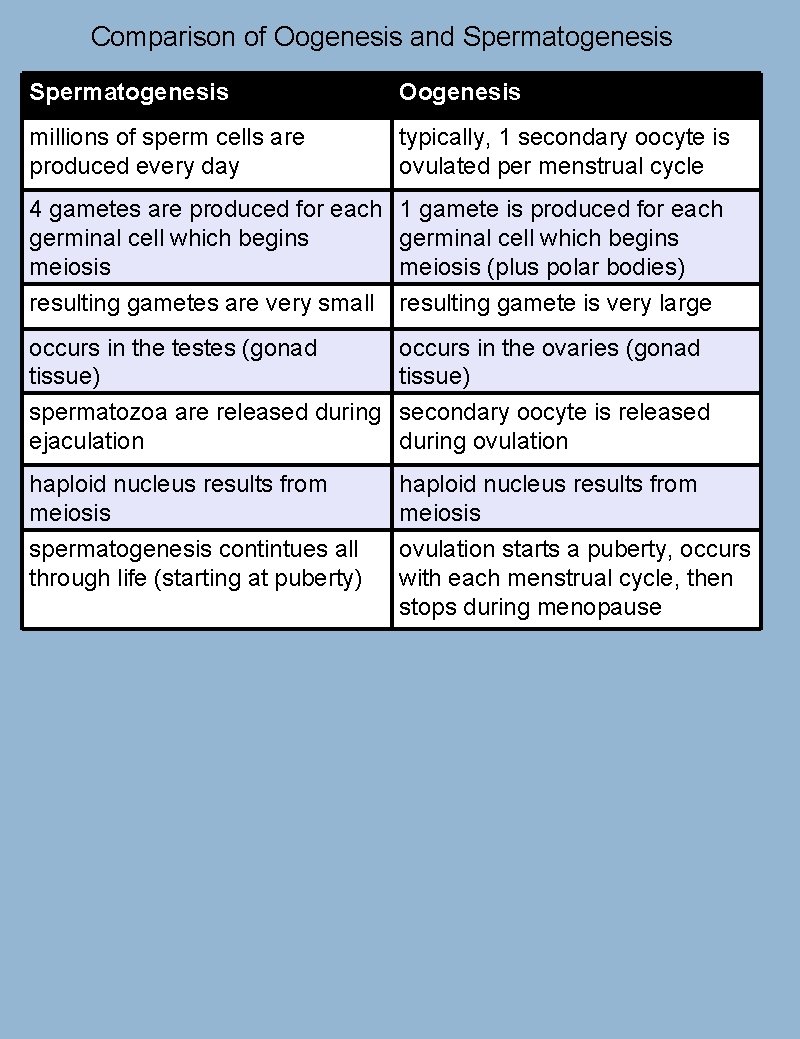
Comparison of Oogenesis and Spermatogenesis Oogenesis millions of sperm cells are produced every day typically, 1 secondary oocyte is ovulated per menstrual cycle 4 gametes are produced for each germinal cell which begins meiosis resulting gametes are very small 1 gamete is produced for each germinal cell which begins meiosis (plus polar bodies) resulting gamete is very large occurs in the testes (gonad tissue) occurs in the ovaries (gonad tissue) spermatozoa are released during secondary oocyte is released ejaculation during ovulation haploid nucleus results from meiosis spermatogenesis contintues all through life (starting at puberty) haploid nucleus results from meiosis ovulation starts a puberty, occurs with each menstrual cycle, then stops during menopause
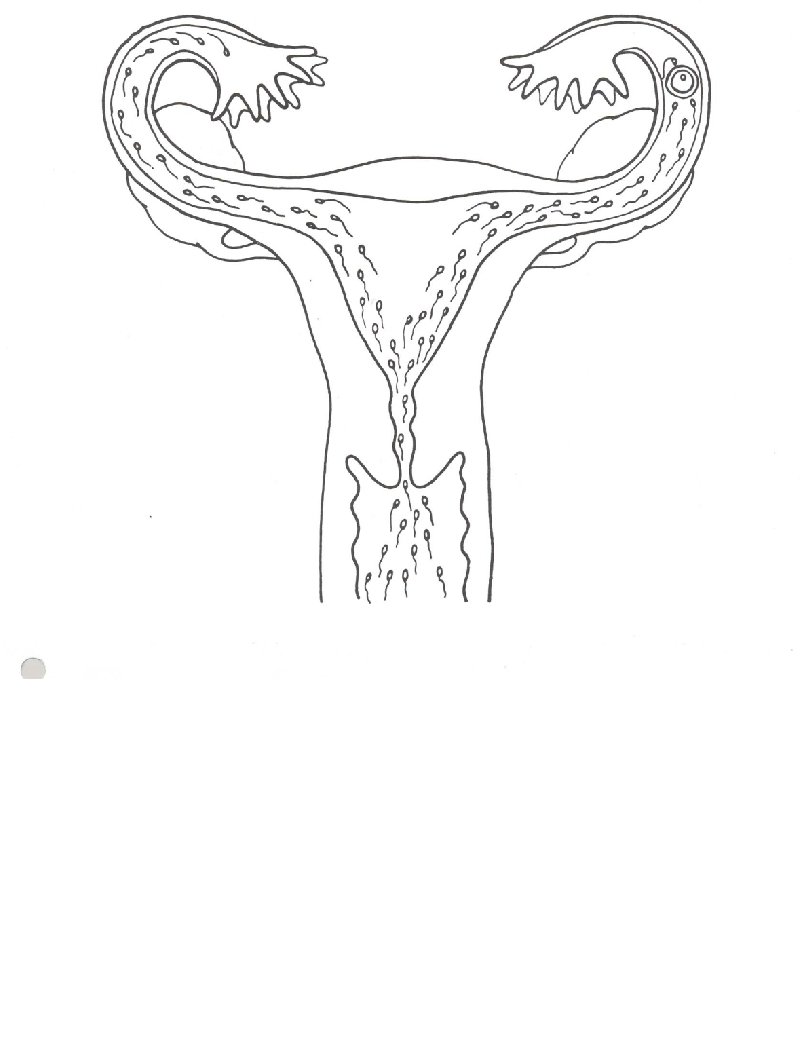

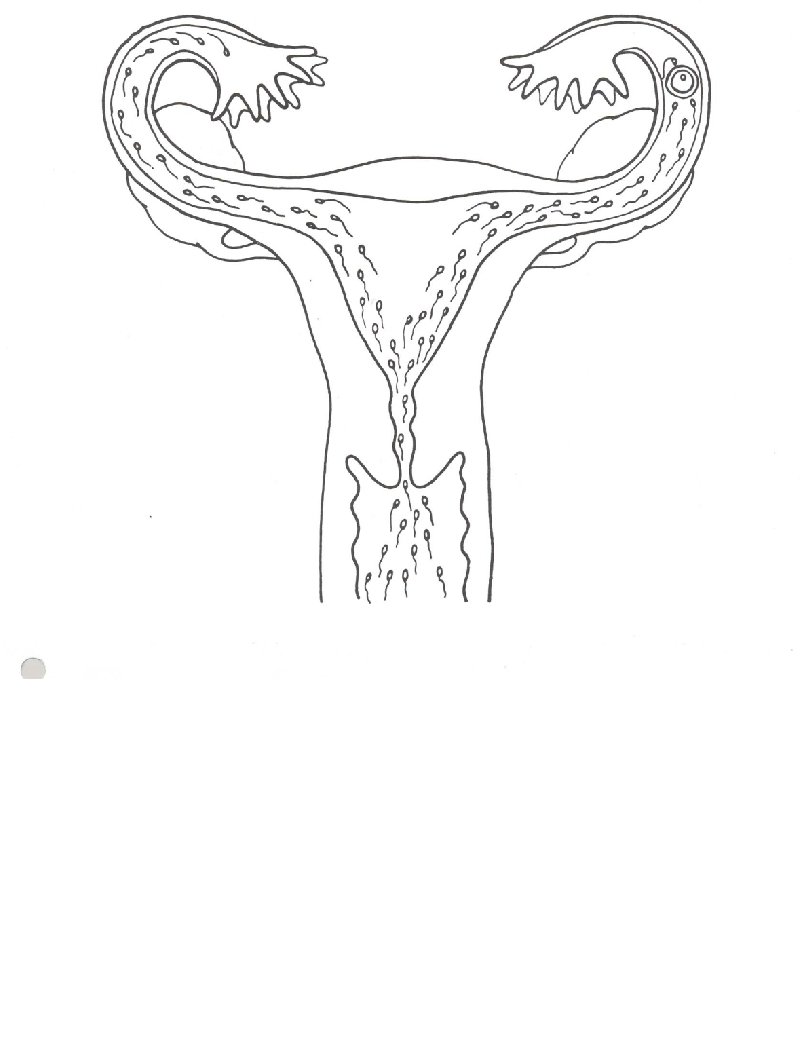
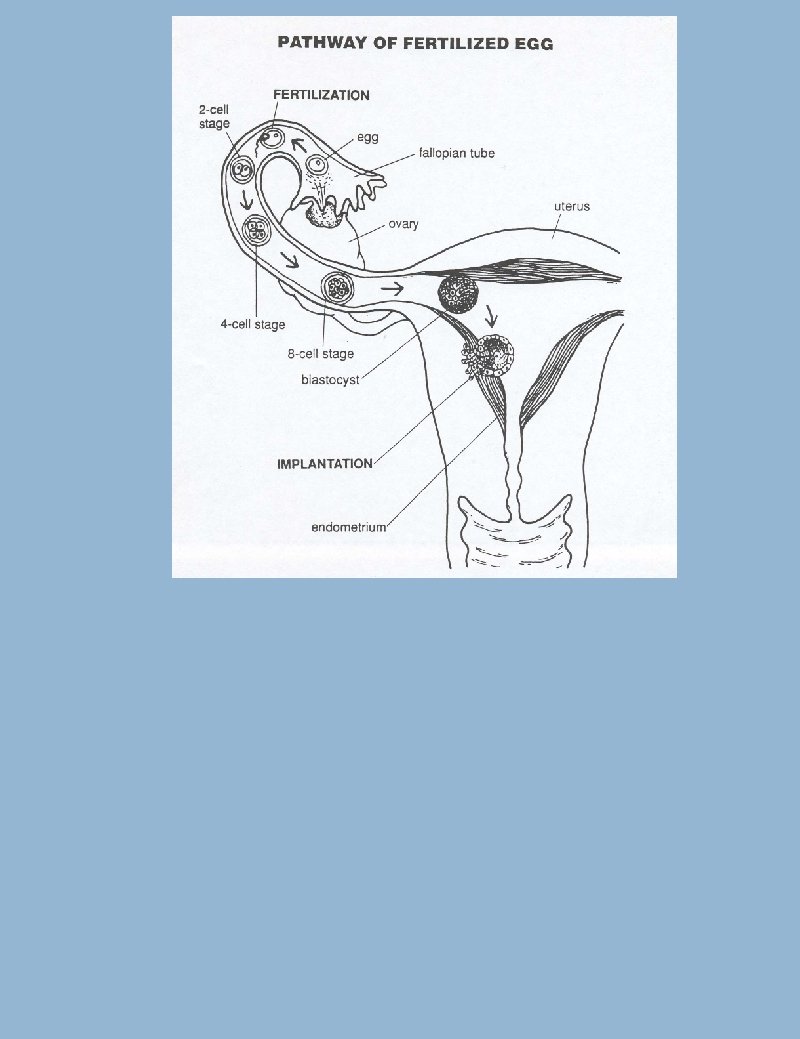
Fertilization: ·successful fertilization occurs in the oviduct (fallopian tube) ·Many sperm cells are needed to penetrate the follicle cell layer ·Several sperm cells make it to the zona pellucida (glycoprotein gel layer) > release hydrolytic enzymes from acrosomes ·First sperm cell through fuses its plasma membrane with the plasma membrane of the secondary oocyte.
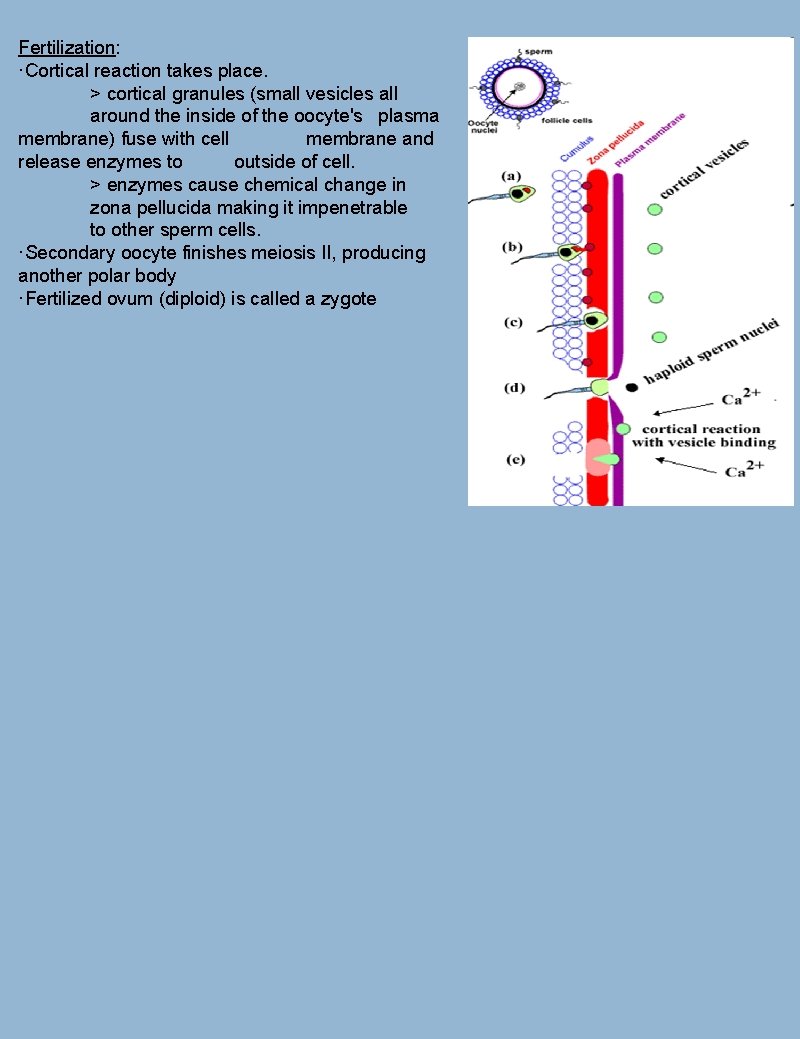
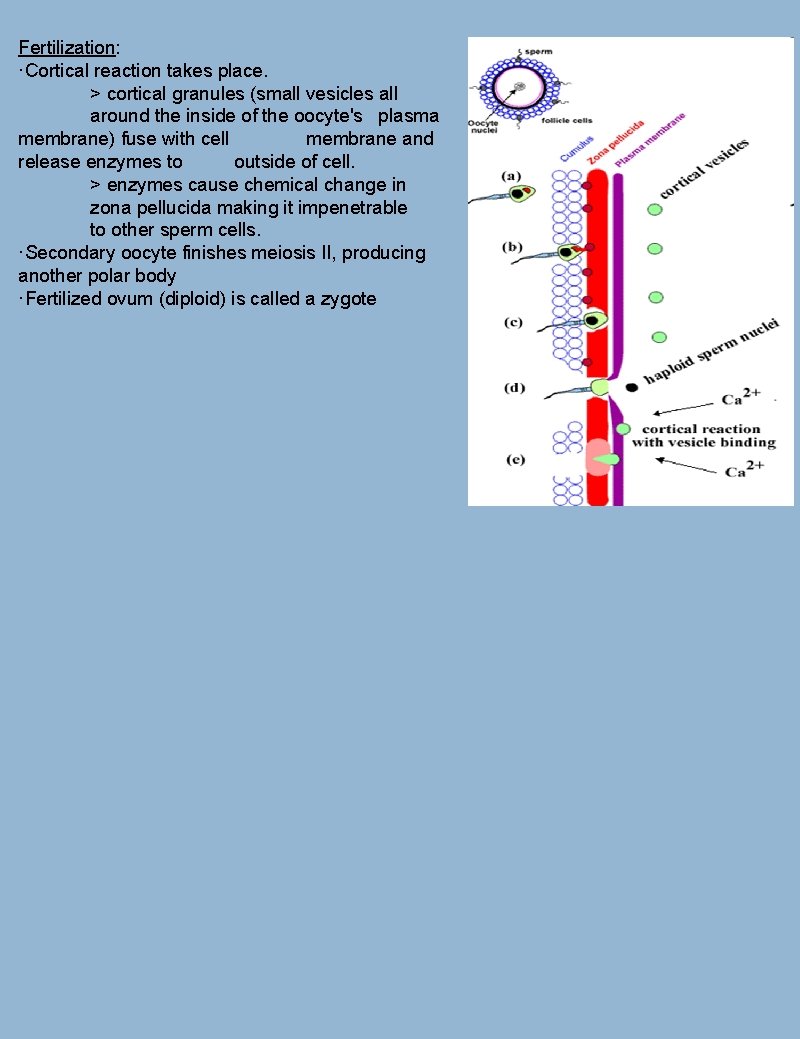
Fertilization: ·Cortical reaction takes place. > cortical granules (small vesicles all around the inside of the oocyte's plasma membrane) fuse with cell membrane and release enzymes to outside of cell. > enzymes cause chemical change in zona pellucida making it impenetrable to other sperm cells. ·Secondary oocyte finishes meiosis II, producing another polar body ·Fertilized ovum (diploid) is called a zygote
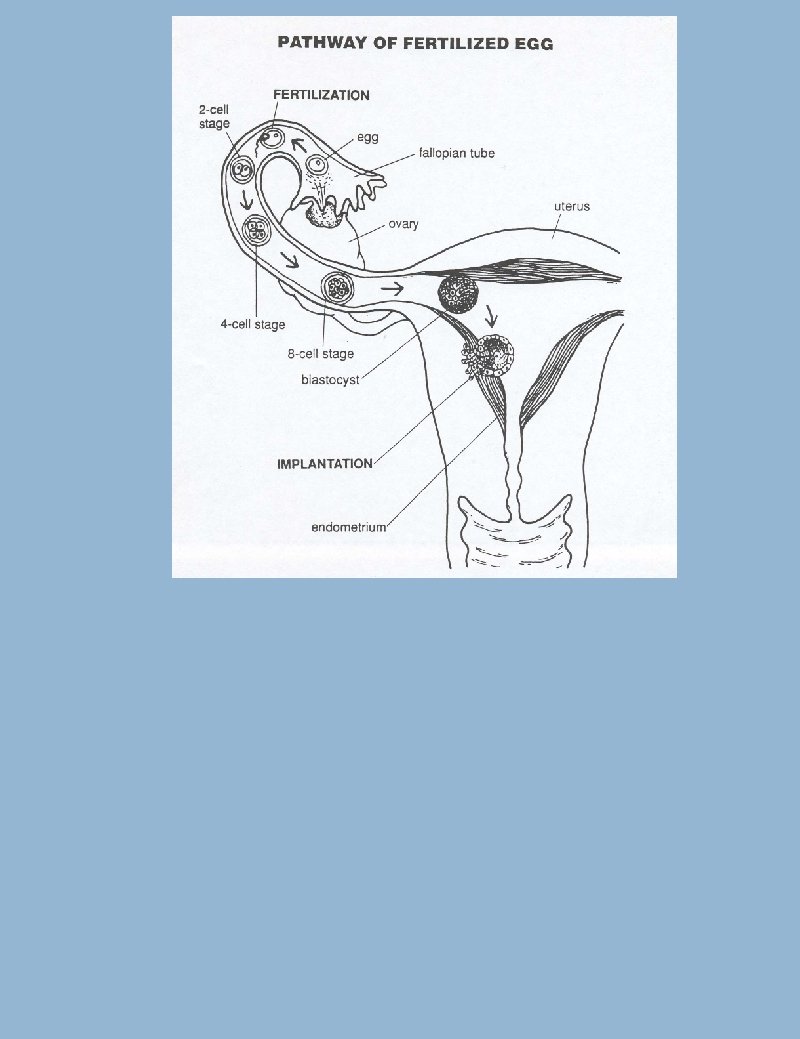
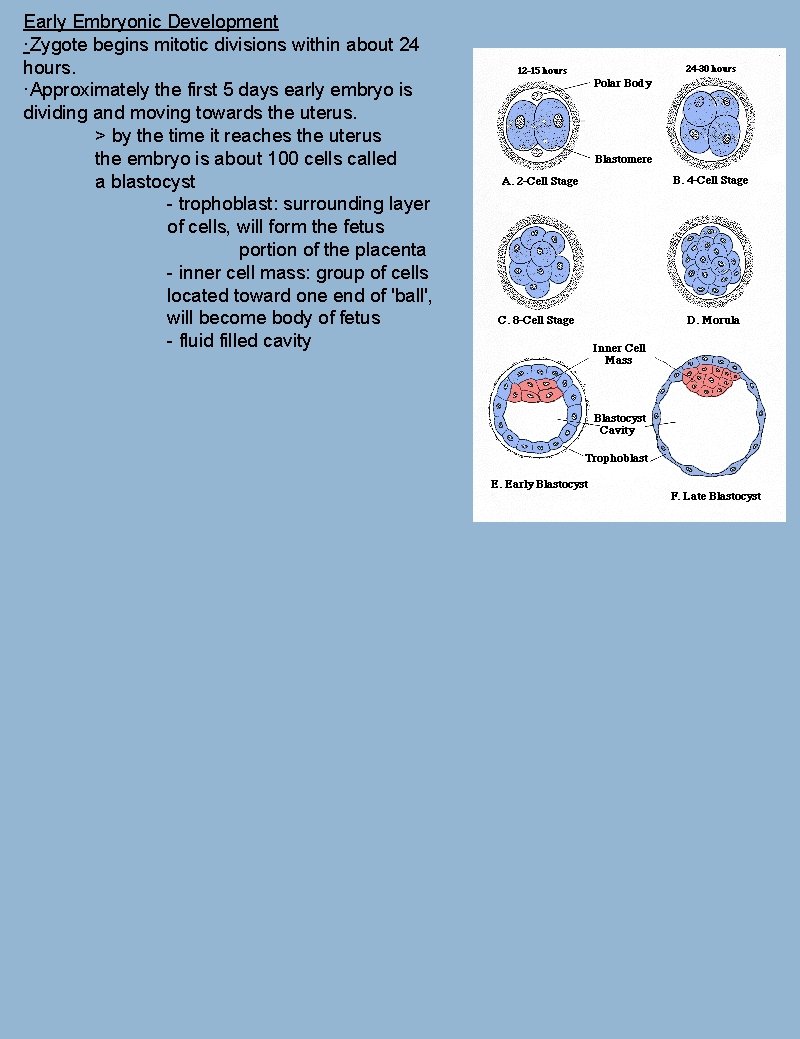
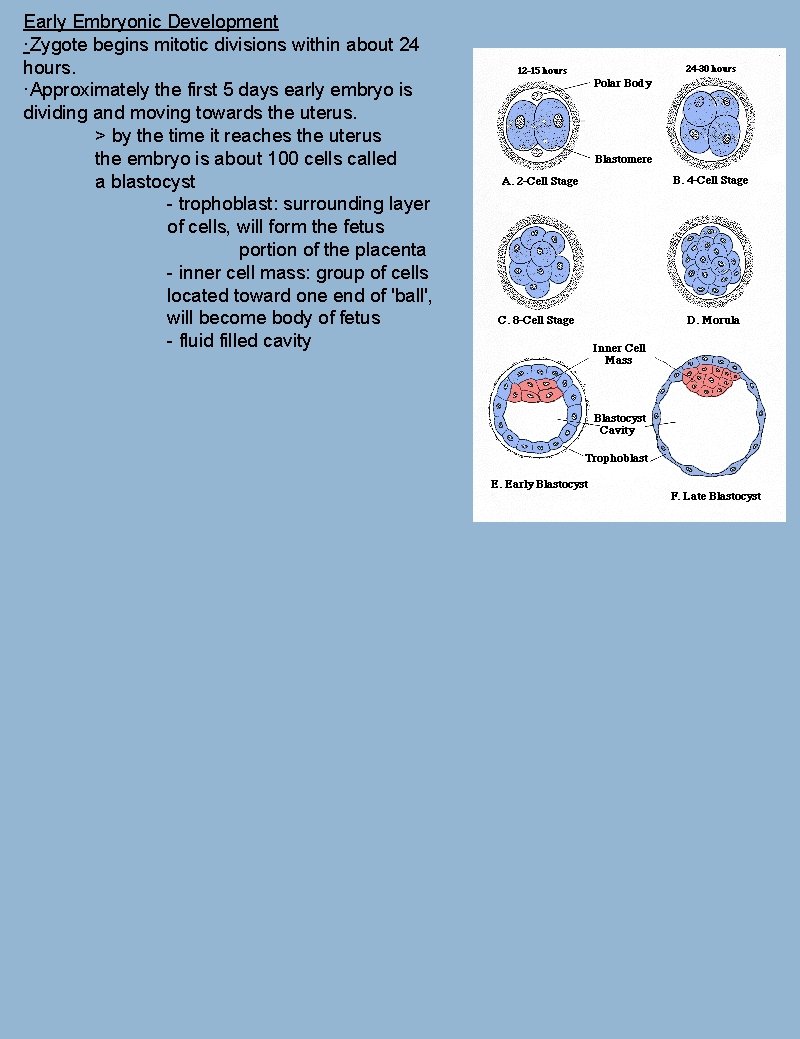
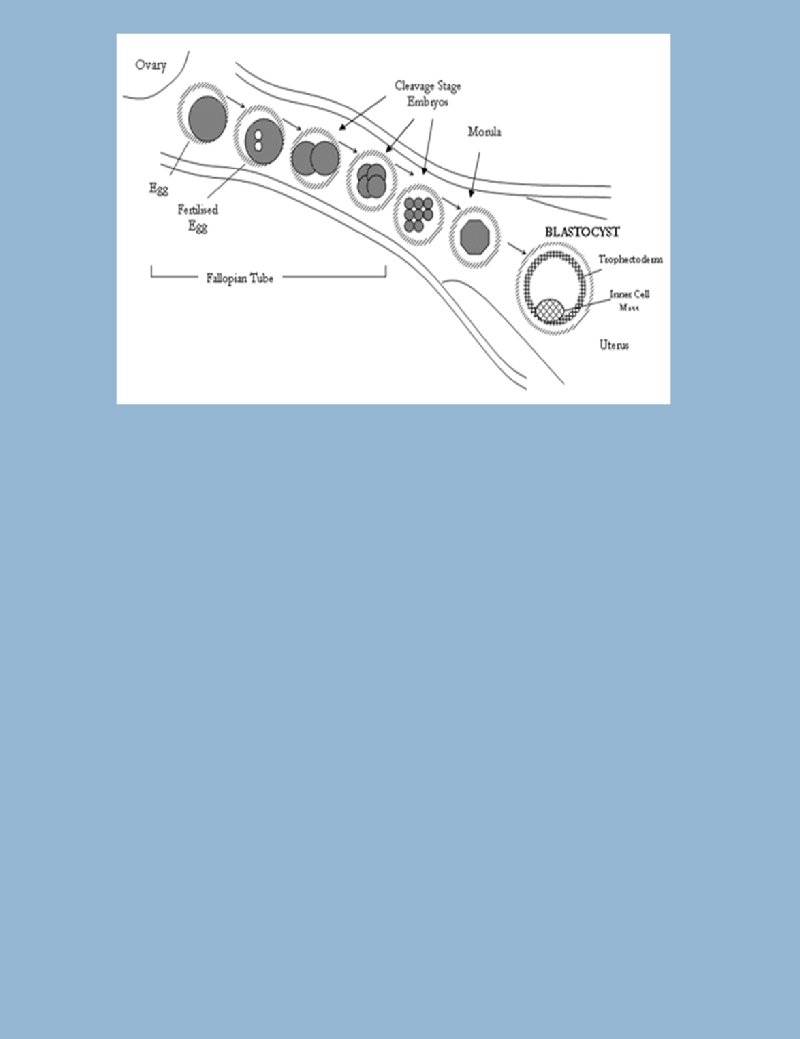
Early Embryonic Development ·Zygote begins mitotic divisions within about 24 hours. ·Approximately the first 5 days early embryo is dividing and moving towards the uterus. > by the time it reaches the uterus the embryo is about 100 cells called a blastocyst - trophoblast: surrounding layer of cells, will form the fetus portion of the placenta - inner cell mass: group of cells located toward one end of 'ball', will become body of fetus - fluid filled cavity
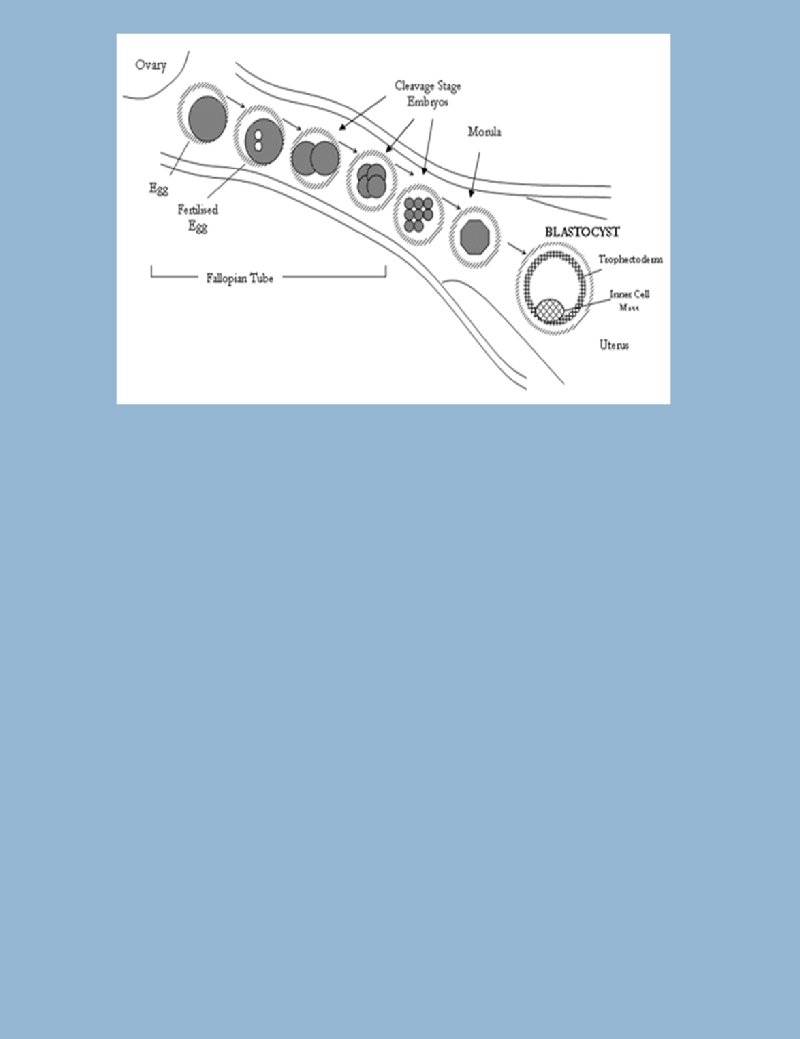
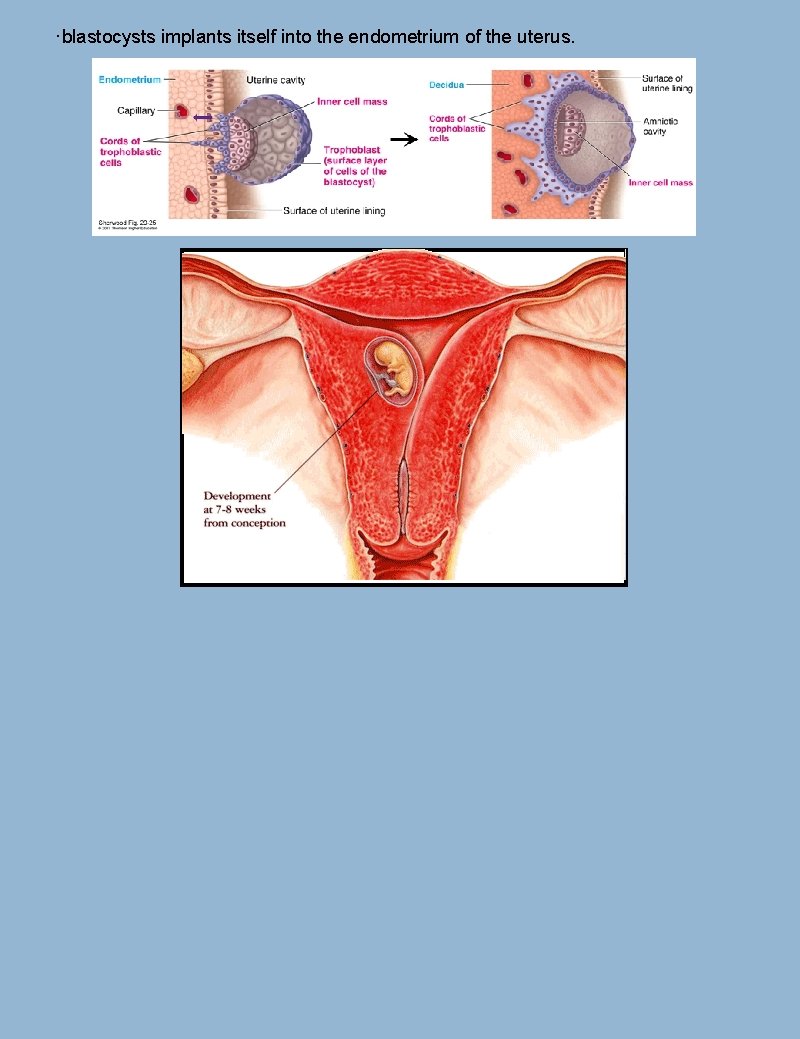
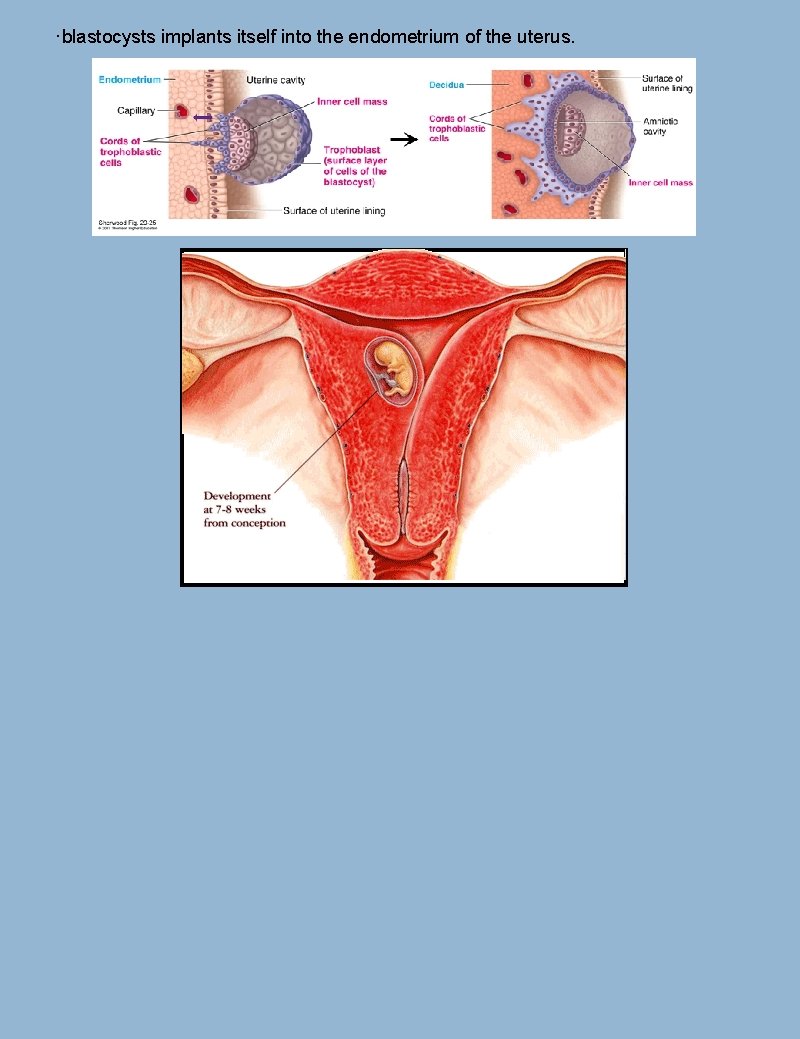
·blastocysts implants itself into the endometrium of the uterus.
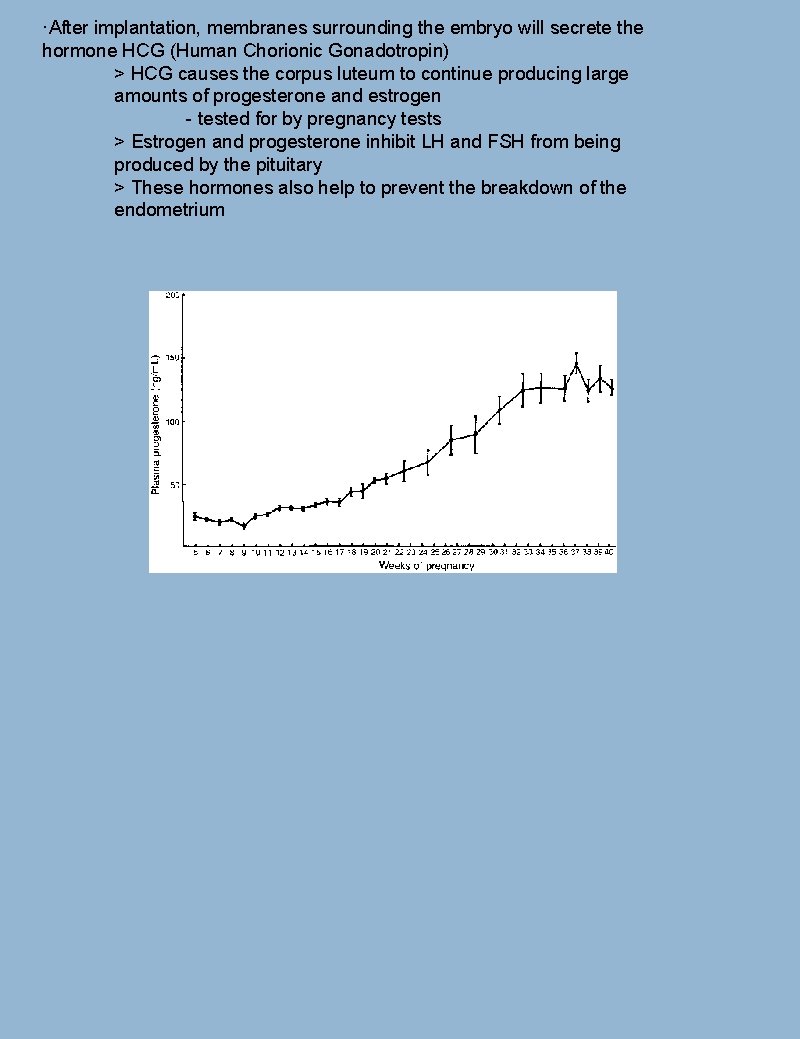
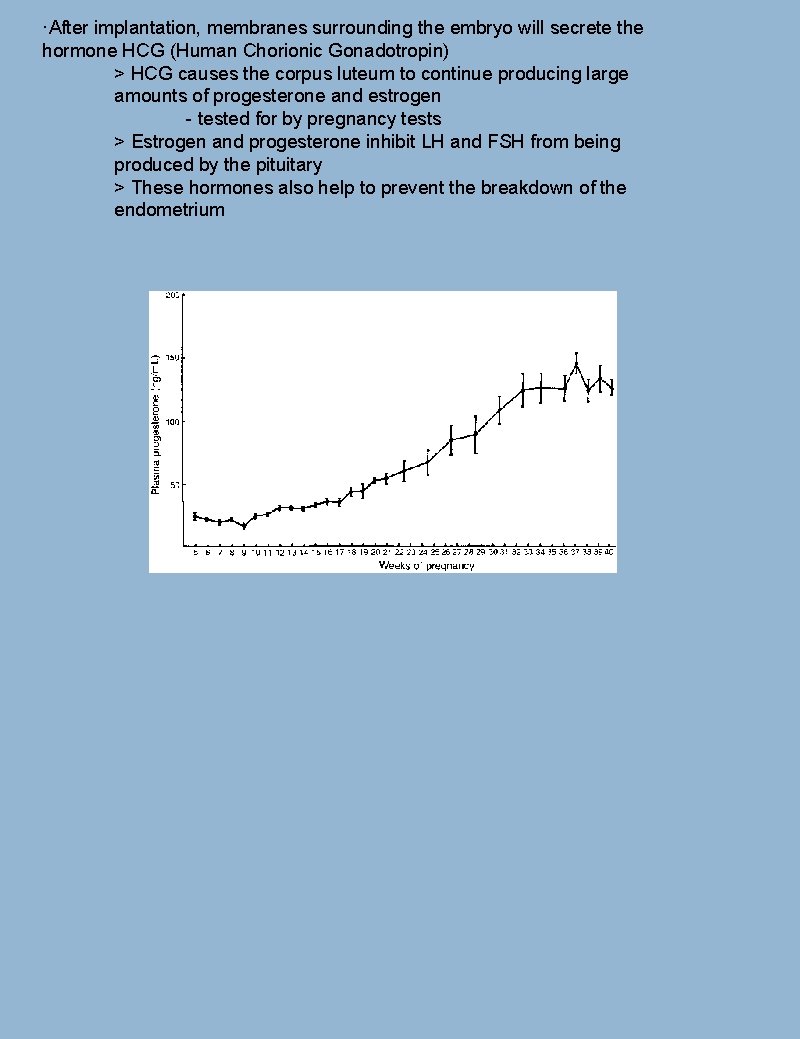
·After implantation, membranes surrounding the embryo will secrete the hormone HCG (Human Chorionic Gonadotropin) > HCG causes the corpus luteum to continue producing large amounts of progesterone and estrogen - tested for by pregnancy tests > Estrogen and progesterone inhibit LH and FSH from being produced by the pituitary > These hormones also help to prevent the breakdown of the endometrium
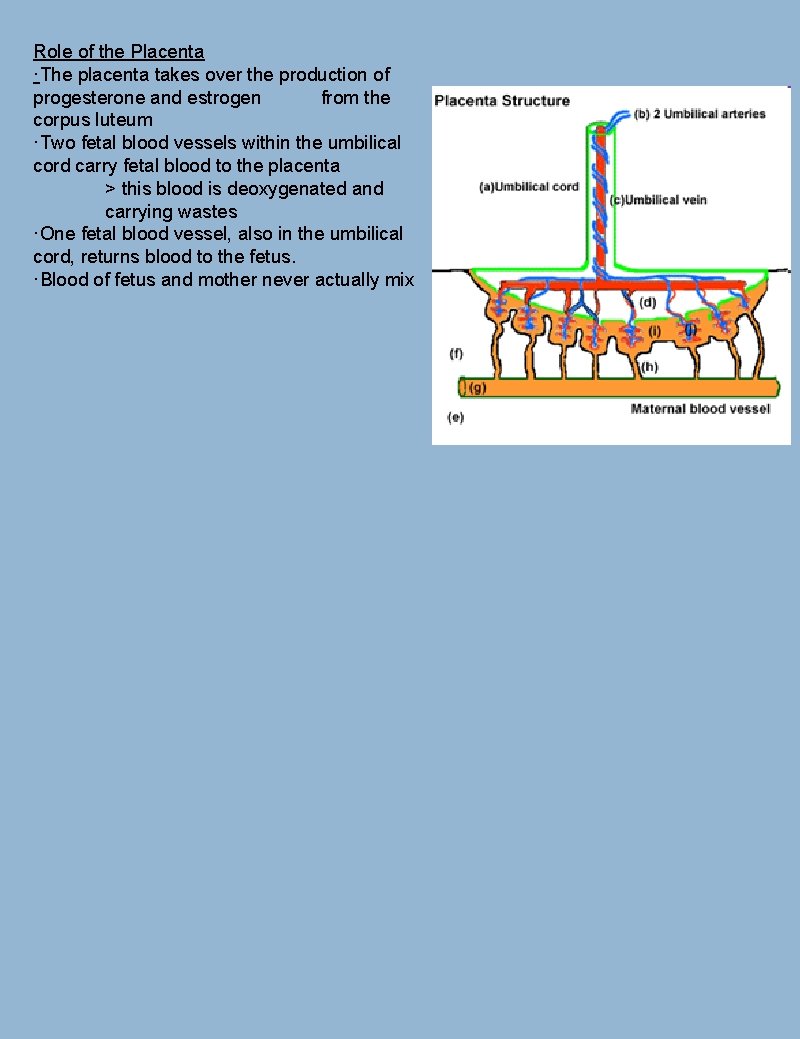
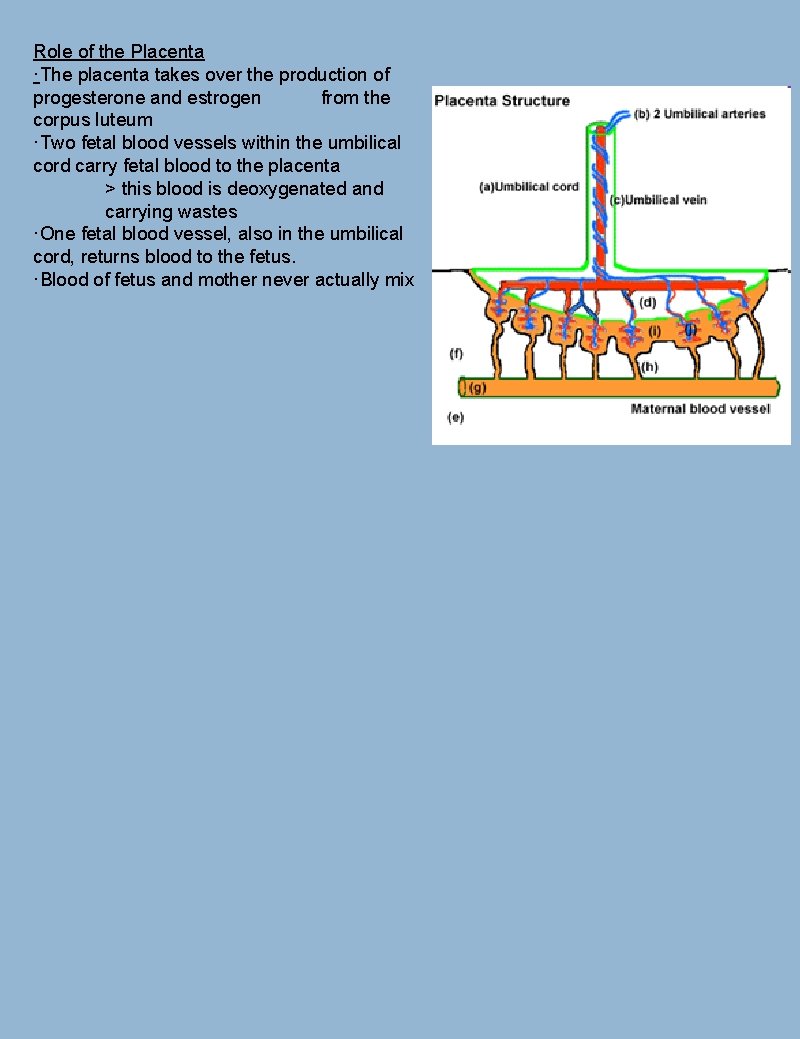
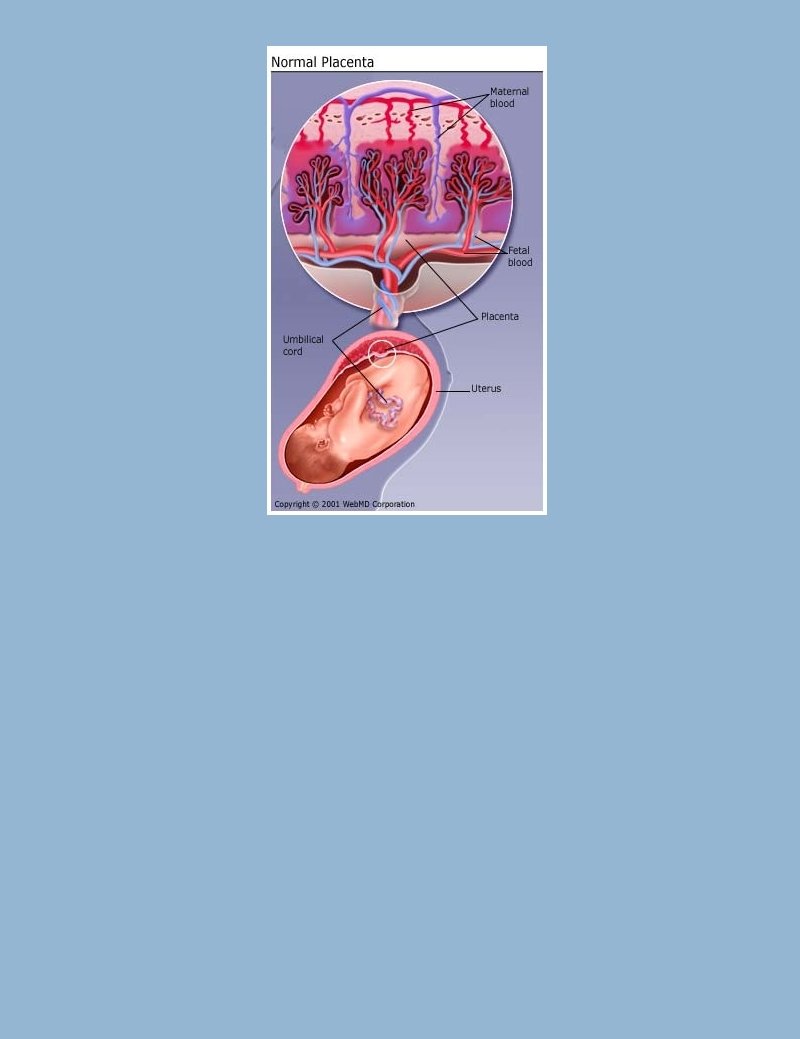
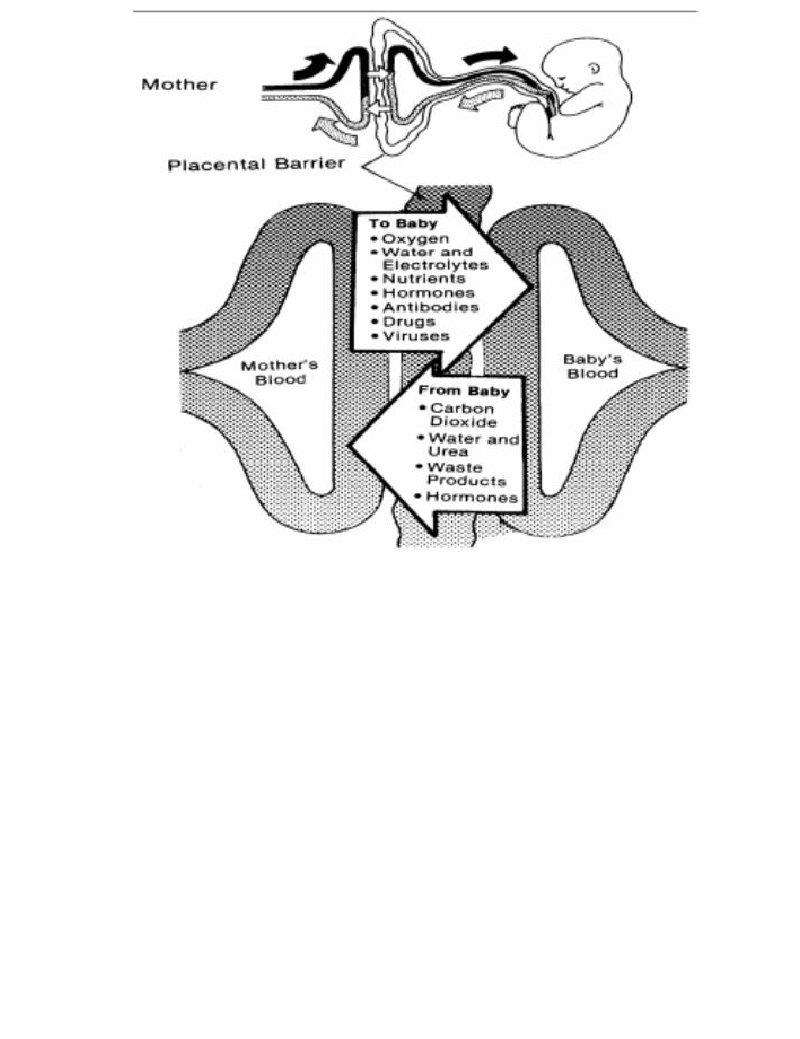
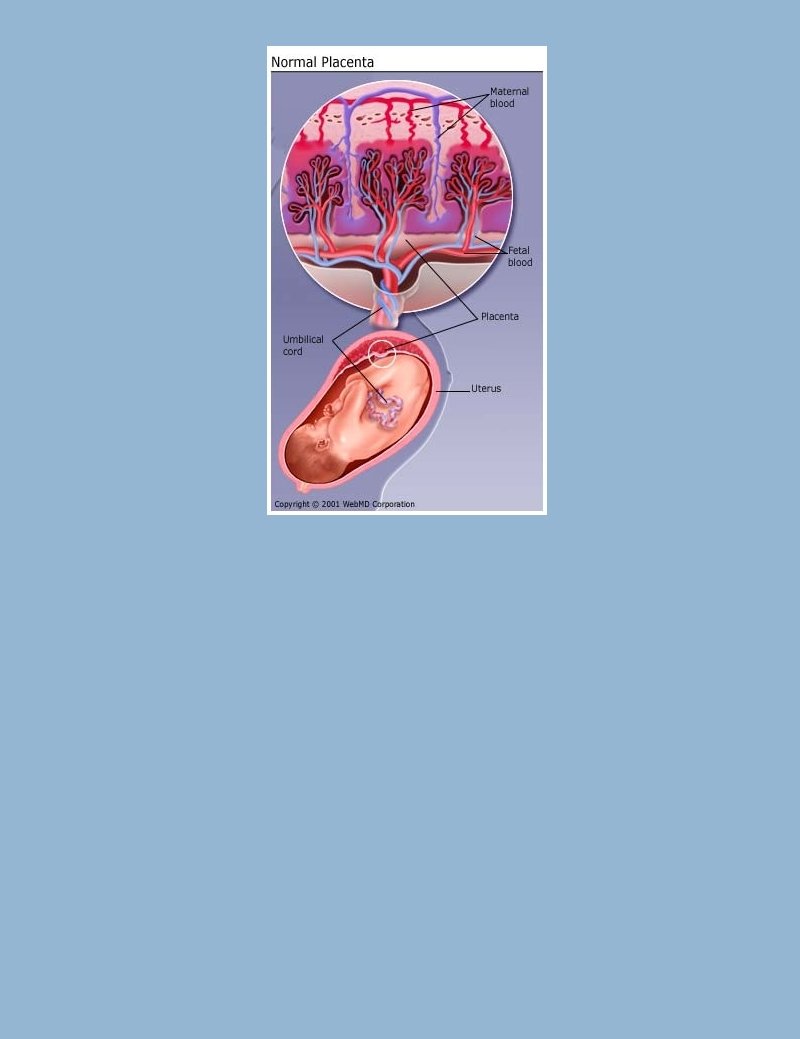
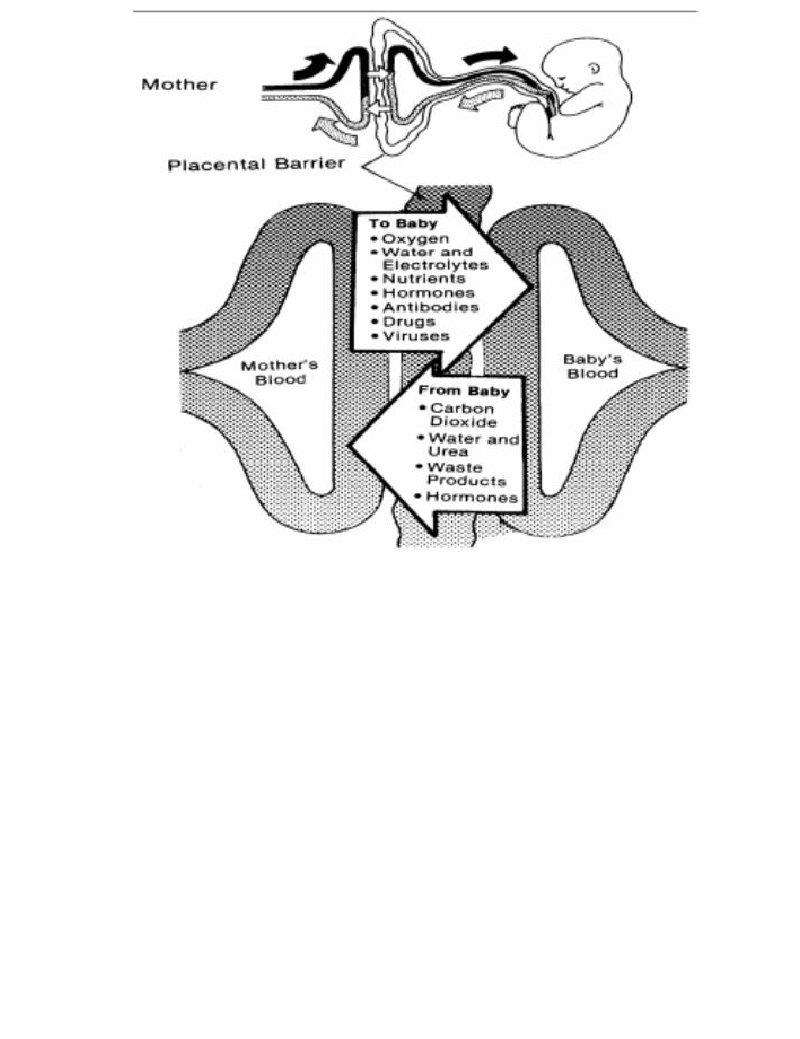
Role of the Placenta ·The placenta takes over the production of progesterone and estrogen from the corpus luteum ·Two fetal blood vessels within the umbilical cord carry fetal blood to the placenta > this blood is deoxygenated and carrying wastes ·One fetal blood vessel, also in the umbilical cord, returns blood to the fetus. ·Blood of fetus and mother never actually mix
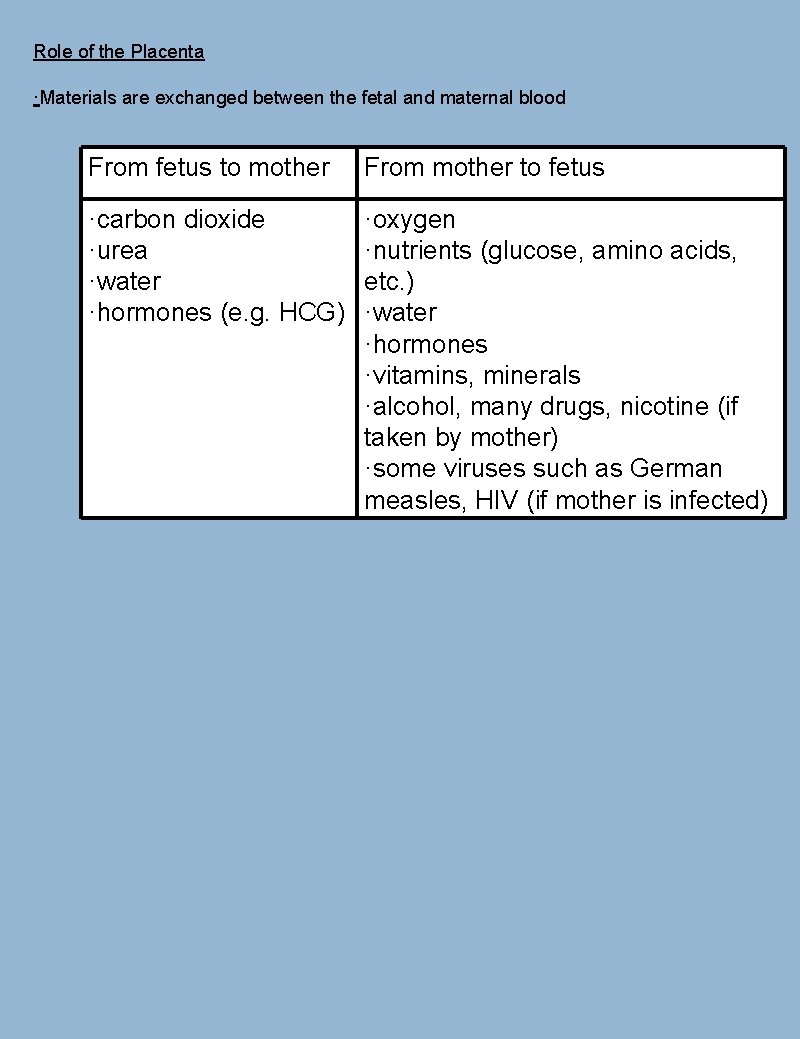
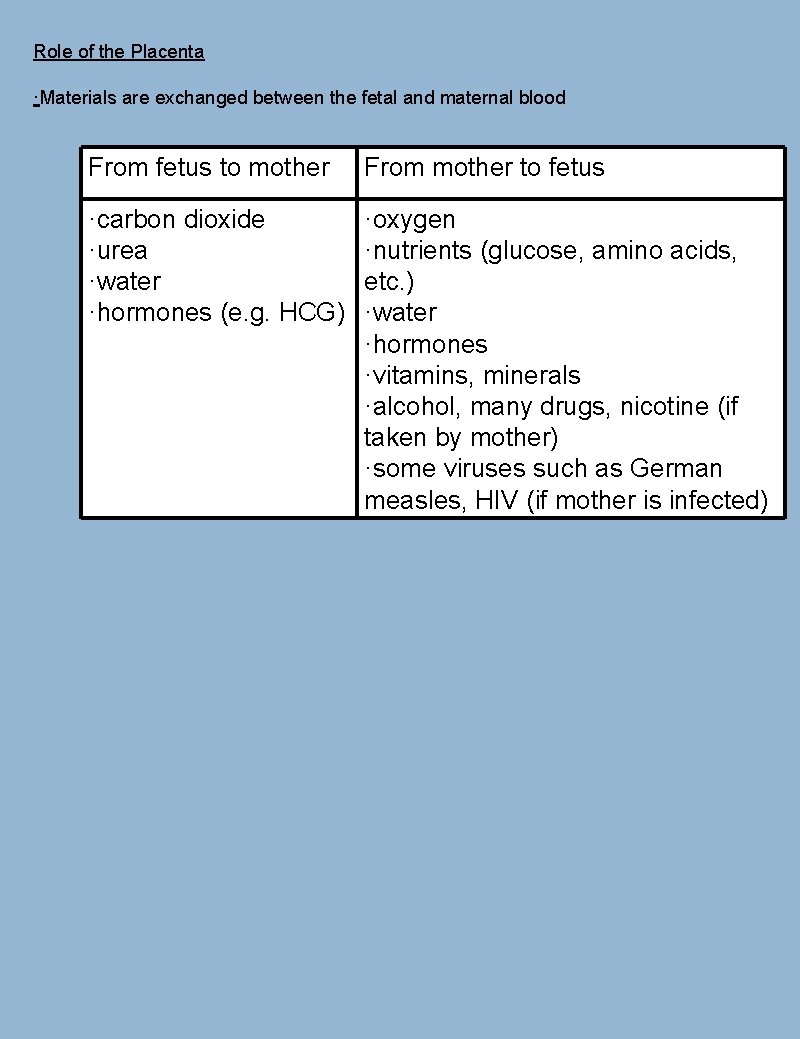
Role of the Placenta ·Materials are exchanged between the fetal and maternal blood From fetus to mother From mother to fetus ·carbon dioxide ·urea ·water ·hormones (e. g. HCG) ·oxygen ·nutrients (glucose, amino acids, etc. ) ·water ·hormones ·vitamins, minerals ·alcohol, many drugs, nicotine (if taken by mother) ·some viruses such as German measles, HIV (if mother is infected)


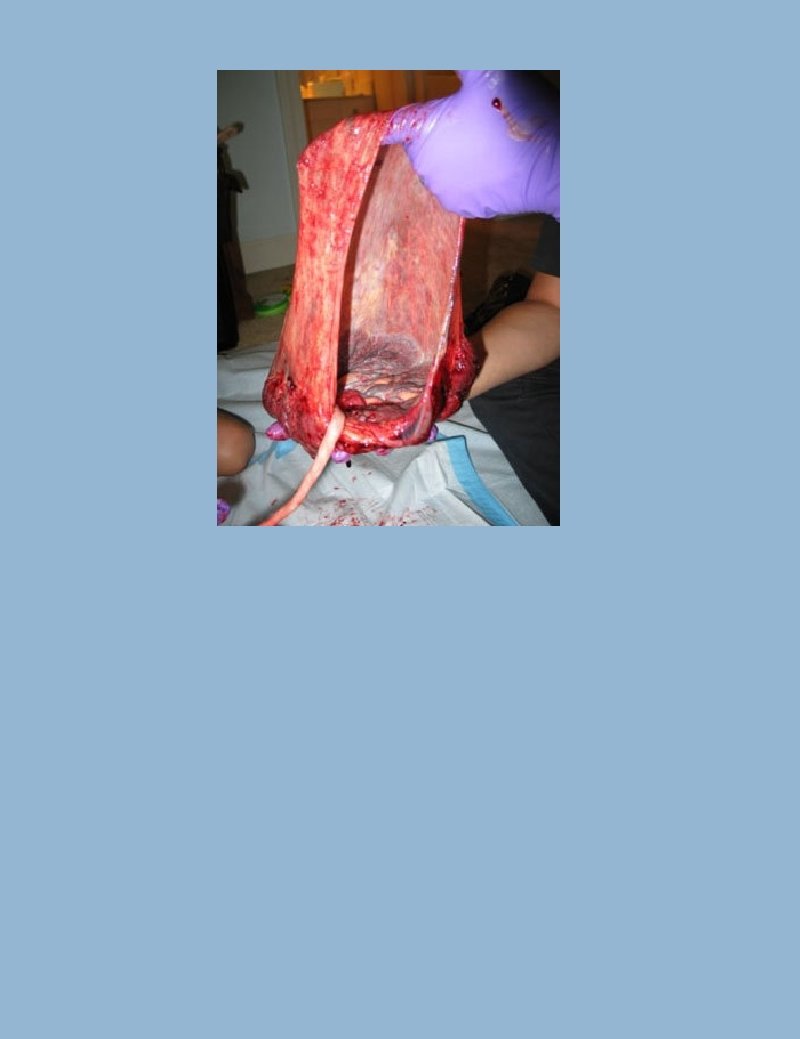
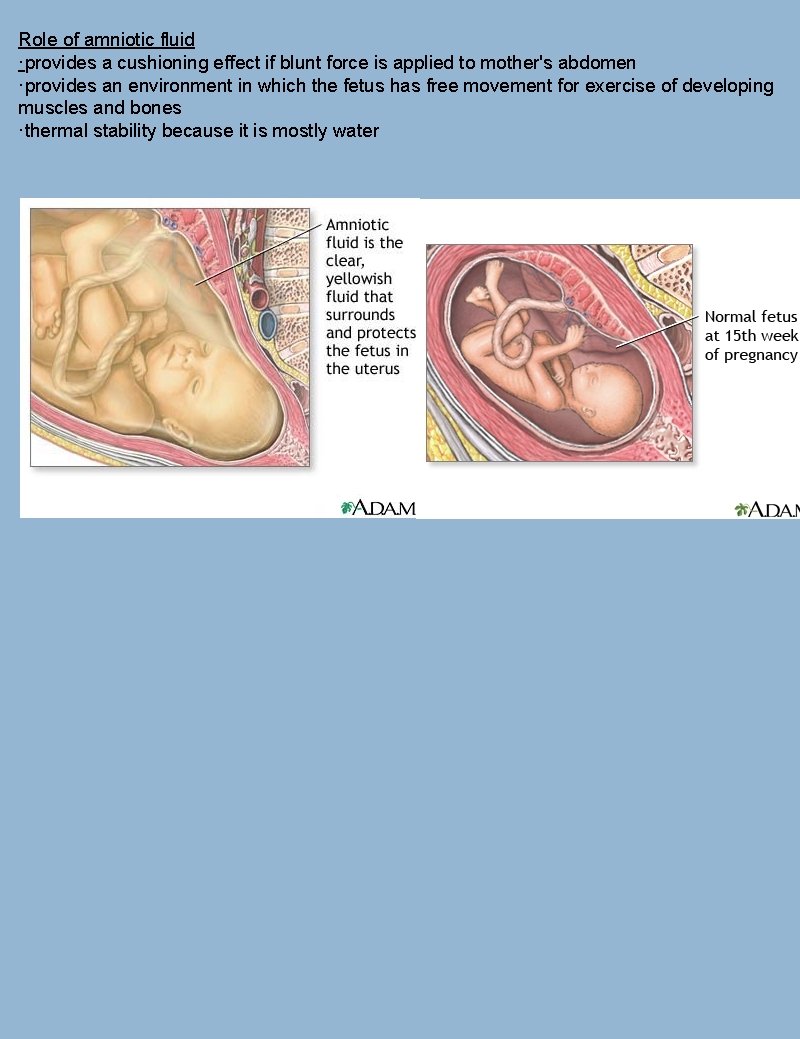
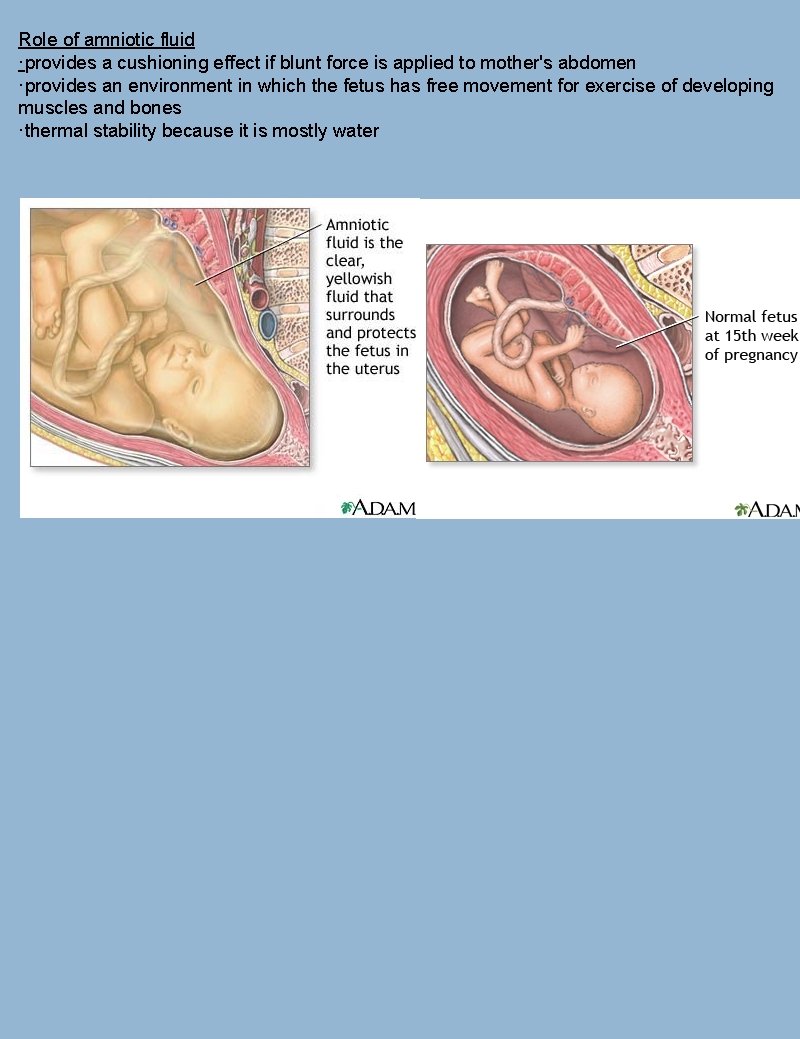
Role of amniotic fluid ·provides a cushioning effect if blunt force is applied to mother's abdomen ·provides an environment in which the fetus has free movement for exercise of developing muscles and bones ·thermal stability because it is mostly water
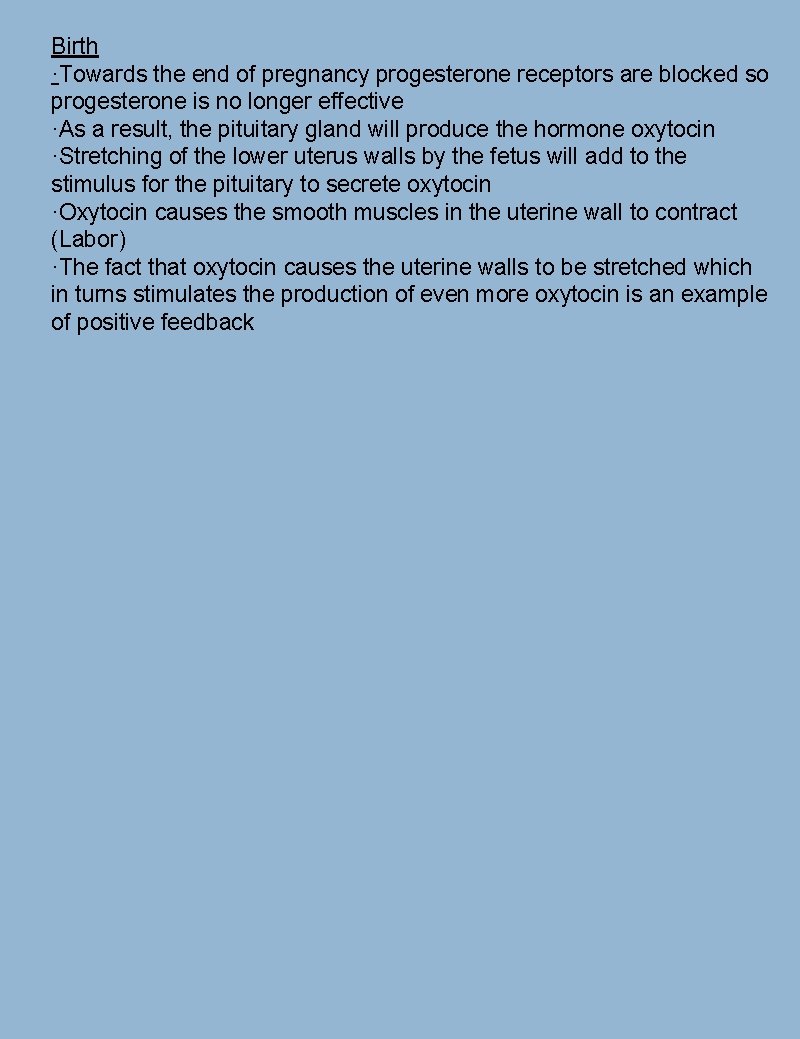
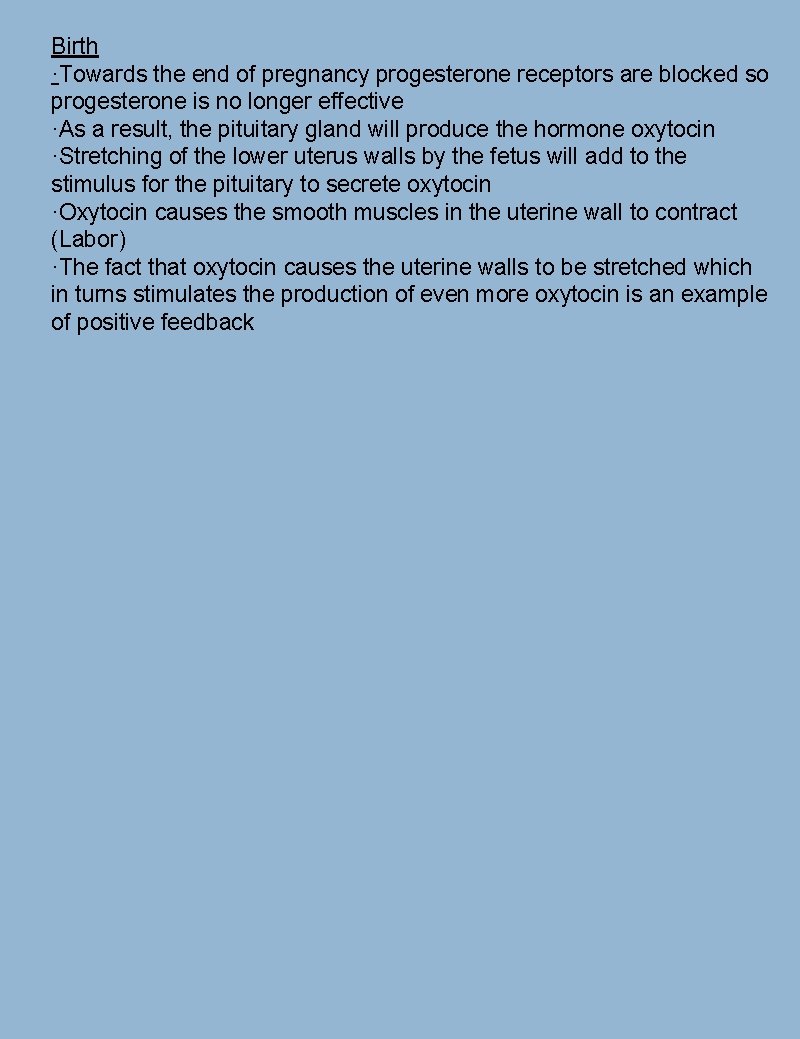
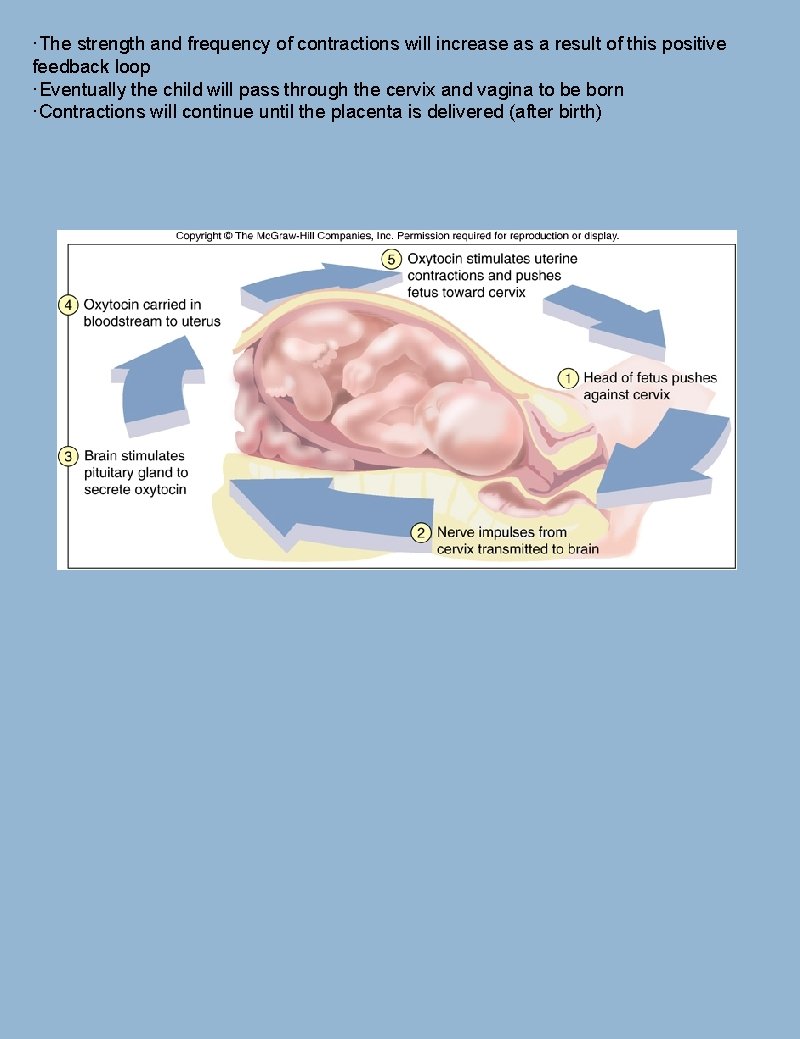
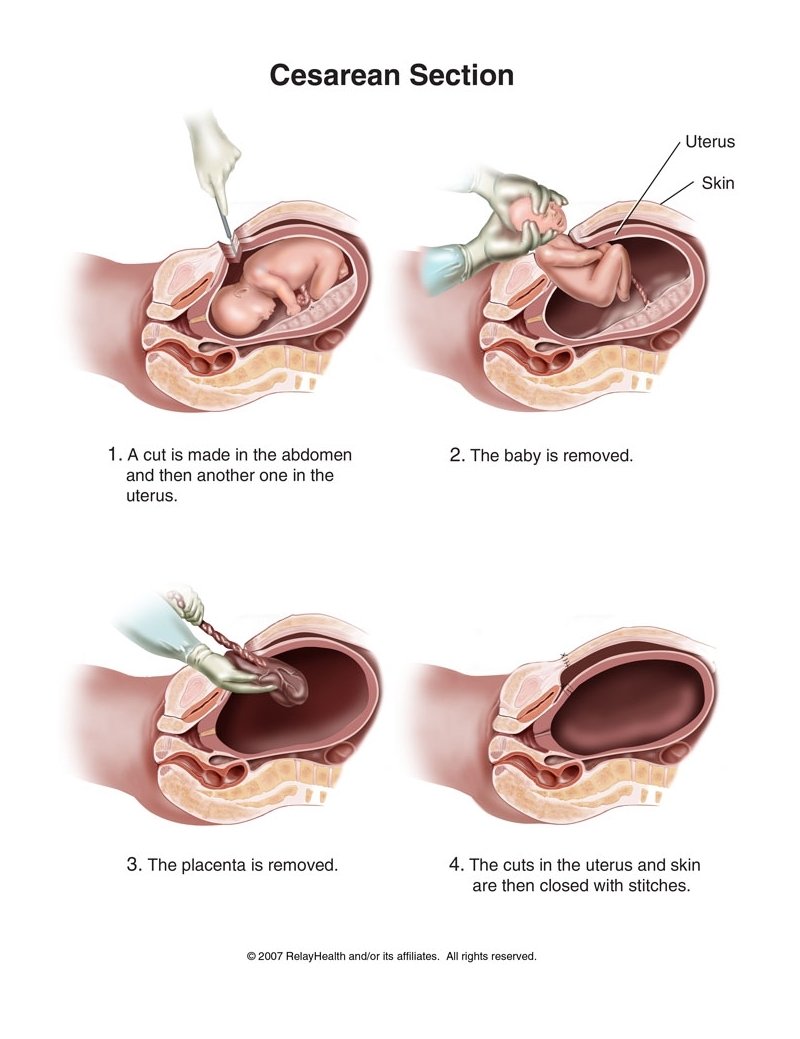
Birth ·Towards the end of pregnancy progesterone receptors are blocked so progesterone is no longer effective ·As a result, the pituitary gland will produce the hormone oxytocin ·Stretching of the lower uterus walls by the fetus will add to the stimulus for the pituitary to secrete oxytocin ·Oxytocin causes the smooth muscles in the uterine wall to contract (Labor) ·The fact that oxytocin causes the uterine walls to be stretched which in turns stimulates the production of even more oxytocin is an example of positive feedback
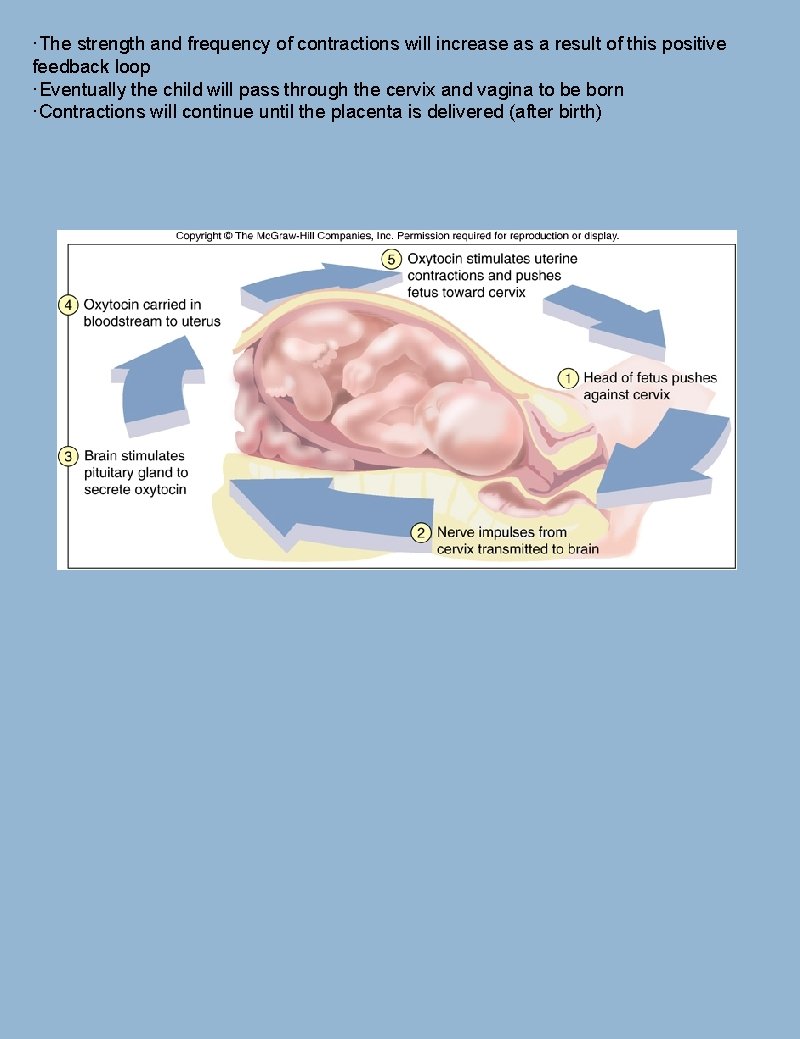
·The strength and frequency of contractions will increase as a result of this positive feedback loop ·Eventually the child will pass through the cervix and vagina to be born ·Contractions will continue until the placenta is delivered (after birth)
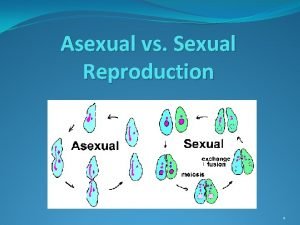
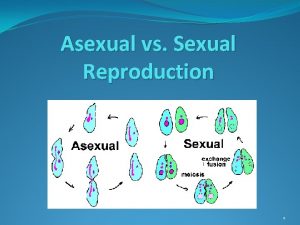
 Asexual reproduction cell division
Asexual reproduction cell division Asexualk
Asexualk Asexual and sexual reproduction venn diagram
Asexual and sexual reproduction venn diagram Concluding sentence
Concluding sentence Narrowed down topic
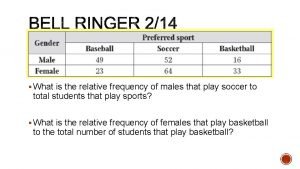
Narrowed down topic What is the relative frequency for males ?
What is the relative frequency for males ? Fritz haarmann childhood
Fritz haarmann childhood Puberache
Puberache Bulbourethral gland
Bulbourethral gland Dos pecados ha cometido mi pueblo
Dos pecados ha cometido mi pueblo Is puberty a physical or chemical change
Is puberty a physical or chemical change What is a pedigree?
What is a pedigree? Meioss
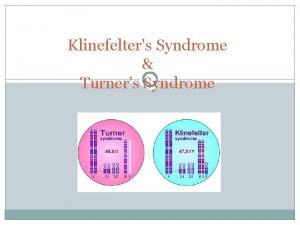
Meioss Down turner and klinefelter syndrome
Down turner and klinefelter syndrome Turner syndrome in males
Turner syndrome in males Jacob's syndrome
Jacob's syndrome Lh and fsh in males
Lh and fsh in males Males with extra y chromosome
Males with extra y chromosome Spermatogenesis vs oogenesis
Spermatogenesis vs oogenesis Mia malemo
Mia malemo Turner syndrome symptoms
Turner syndrome symptoms Hypergonadism in males
Hypergonadism in males Factors affecting spermatogenesis slideshare
Factors affecting spermatogenesis slideshare Spermatogenesis begins in the
Spermatogenesis begins in the Tanner scale
Tanner scale Rsabill
Rsabill Fccla dress code
Fccla dress code Tanner staging
Tanner staging The unequal access of males and females to property
The unequal access of males and females to property Måleenhet for spenning
Måleenhet for spenning In males, fsh prods these organs to produce testosterone.
In males, fsh prods these organs to produce testosterone. The diagram below represents chromosomes in a zygote
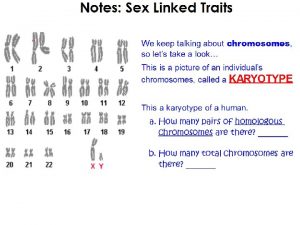
The diagram below represents chromosomes in a zygote Human reproduction webquest
Human reproduction webquest Chapter 21 human reproduction answer key
Chapter 21 human reproduction answer key Human reproduction introduction
Human reproduction introduction Sexual reproduction in human
Sexual reproduction in human A sexual reproduction in humans
A sexual reproduction in humans