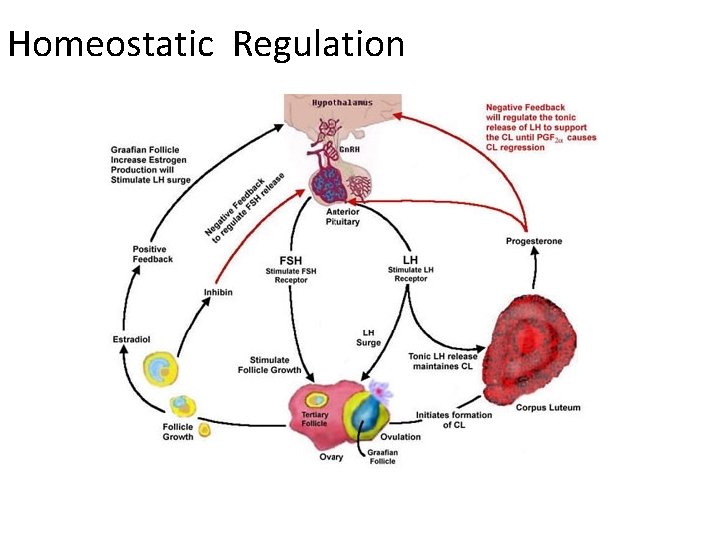
Homeostatic Regulation The Outline q Homeostatic loops q




- Slides: 39
Homeostatic Regulation

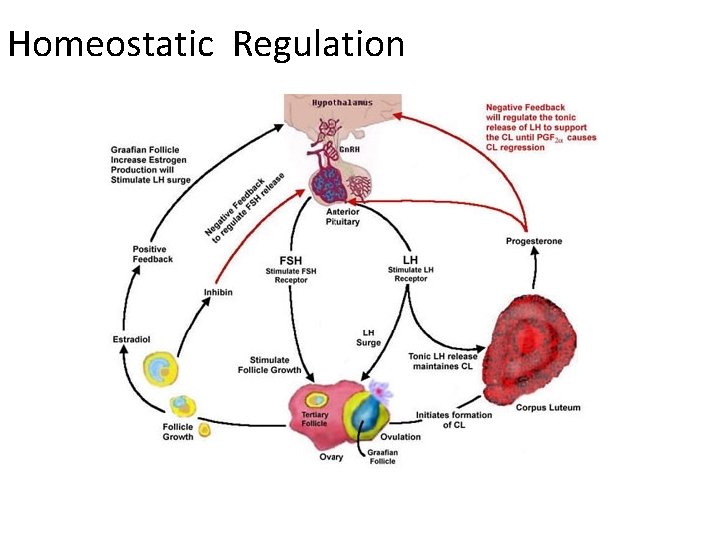
The Outline q. Homeostatic loops q. Introduction to hormones q. Negative feed back in the human body Examples of homeostatic systems • The Stress Response • Water Regulation • Blood Sugar Regulation
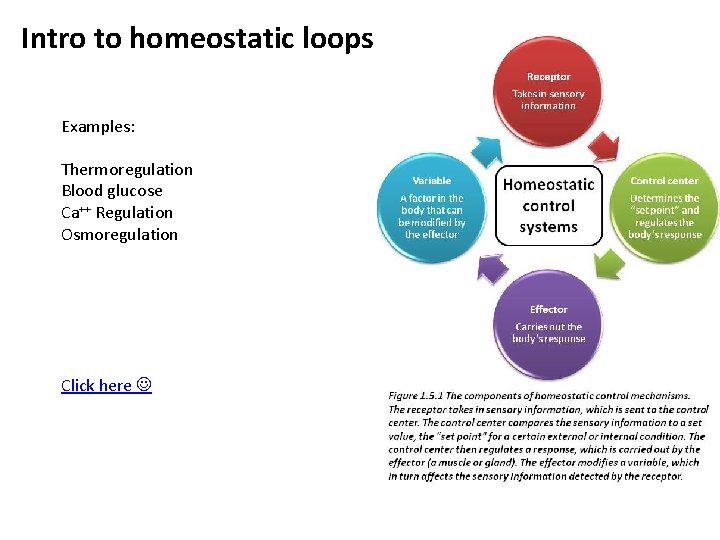
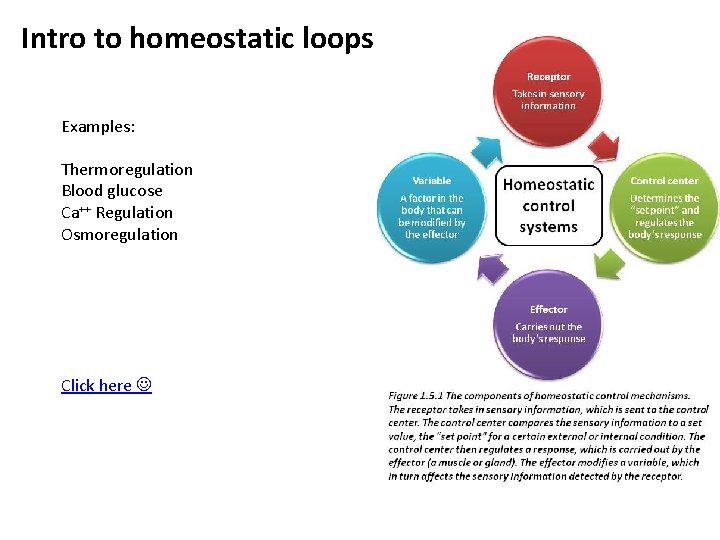
Intro to homeostatic loops Examples: Thermoregulation Blood glucose Ca++ Regulation Osmoregulation Click here
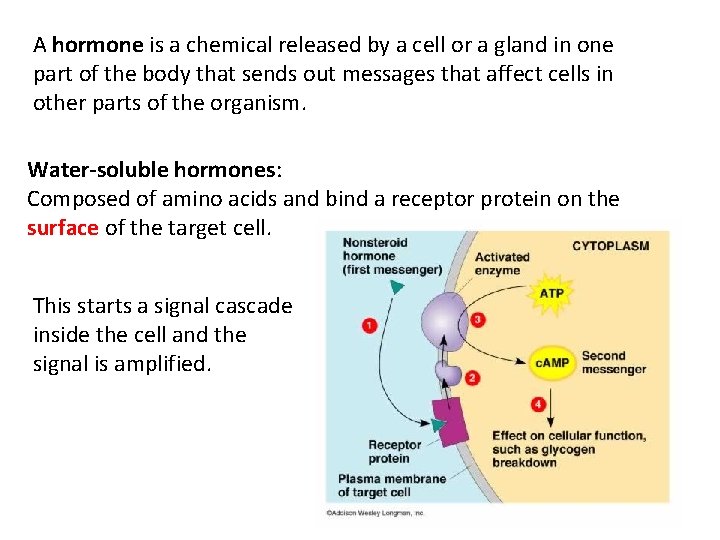
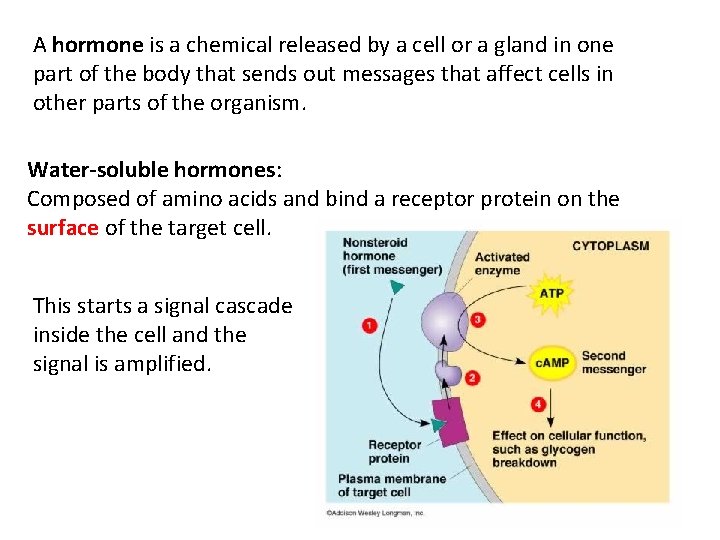
A hormone is a chemical released by a cell or a gland in one part of the body that sends out messages that affect cells in other parts of the organism. Water-soluble hormones: Composed of amino acids and bind a receptor protein on the surface of the target cell. This starts a signal cascade inside the cell and the signal is amplified.
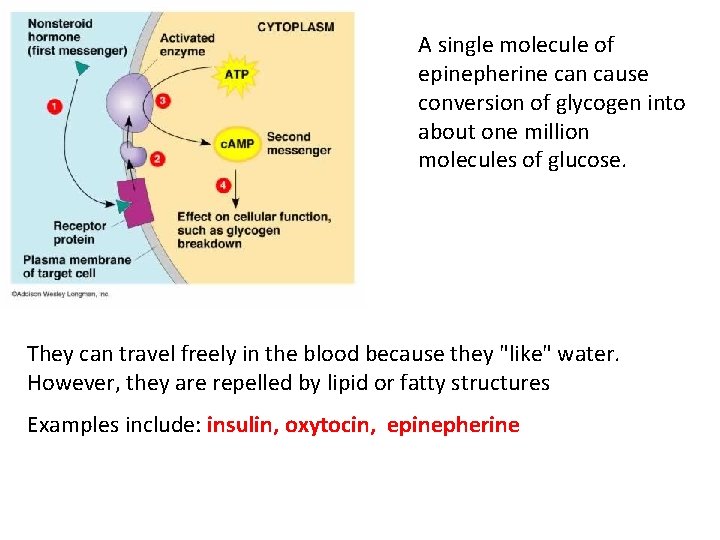
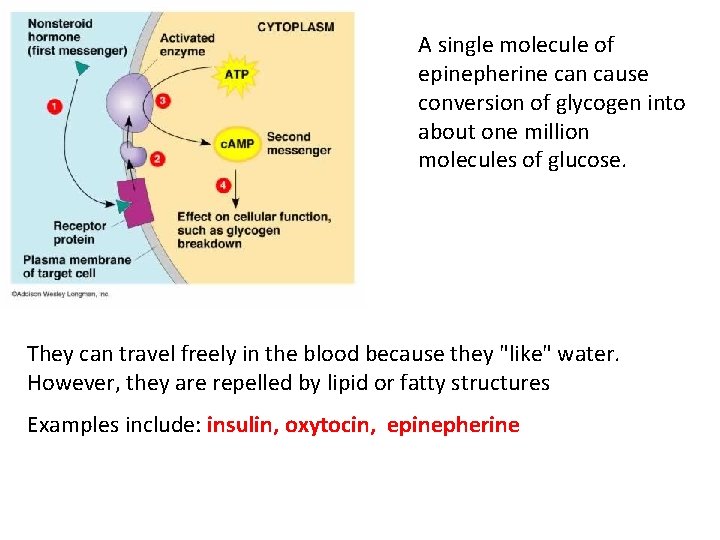
A single molecule of epinepherine can cause conversion of glycogen into about one million molecules of glucose. They can travel freely in the blood because they "like" water. However, they are repelled by lipid or fatty structures Examples include: insulin, oxytocin, epinepherine
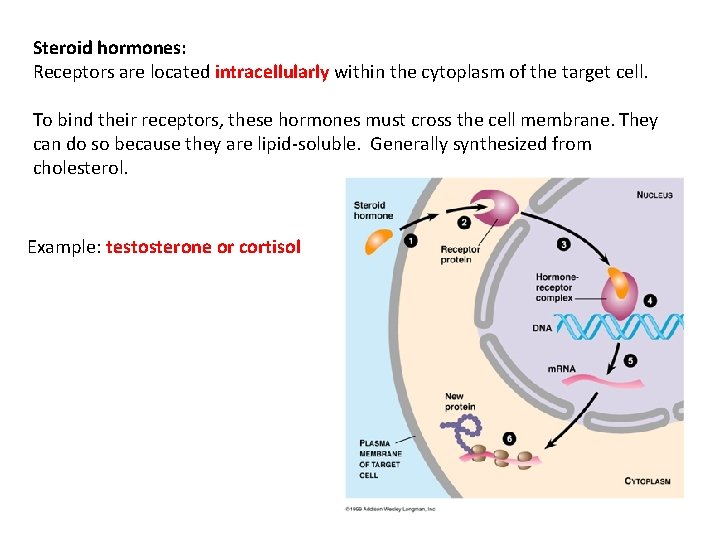
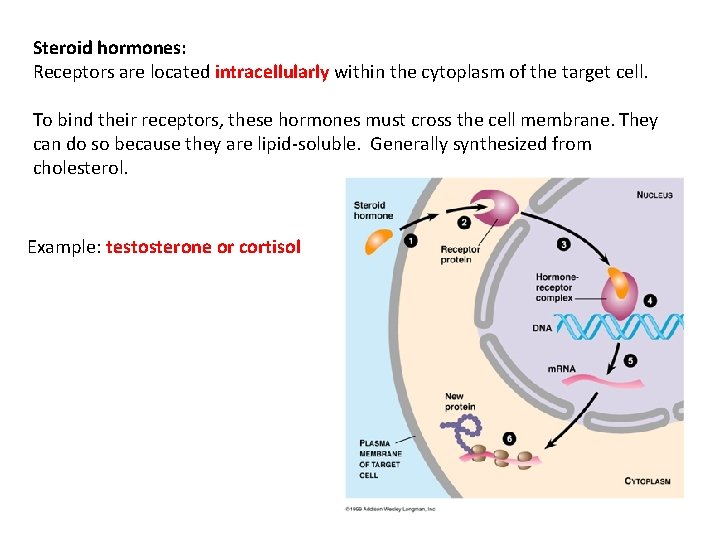
Steroid hormones: Receptors are located intracellularly within the cytoplasm of the target cell. To bind their receptors, these hormones must cross the cell membrane. They can do so because they are lipid-soluble. Generally synthesized from cholesterol. Example: testosterone or cortisol
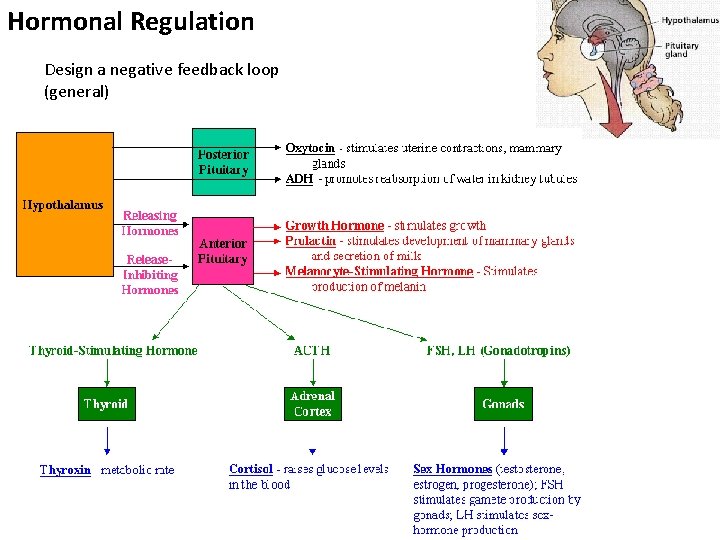
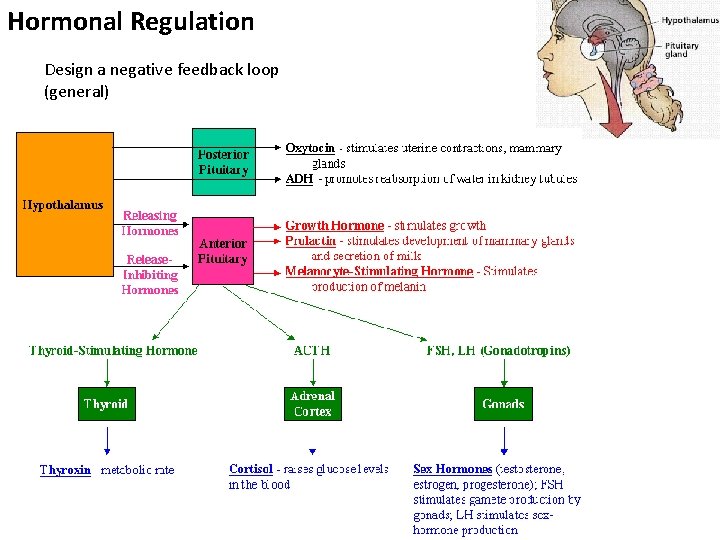
Hormonal Regulation Design a negative feedback loop (general)
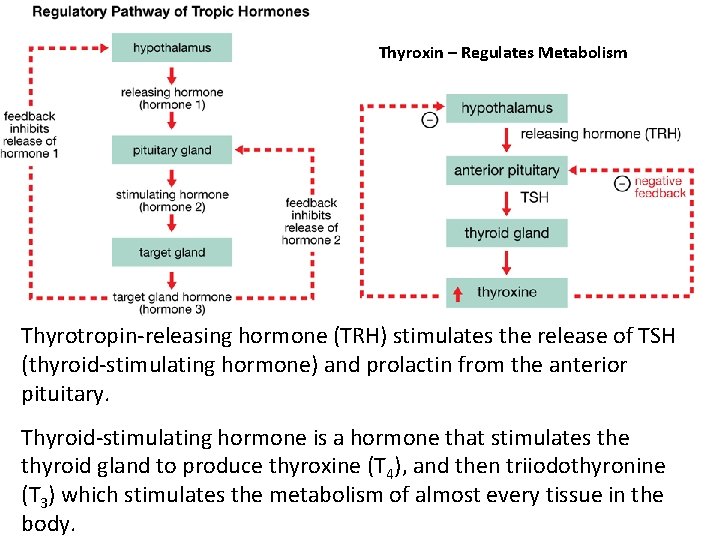
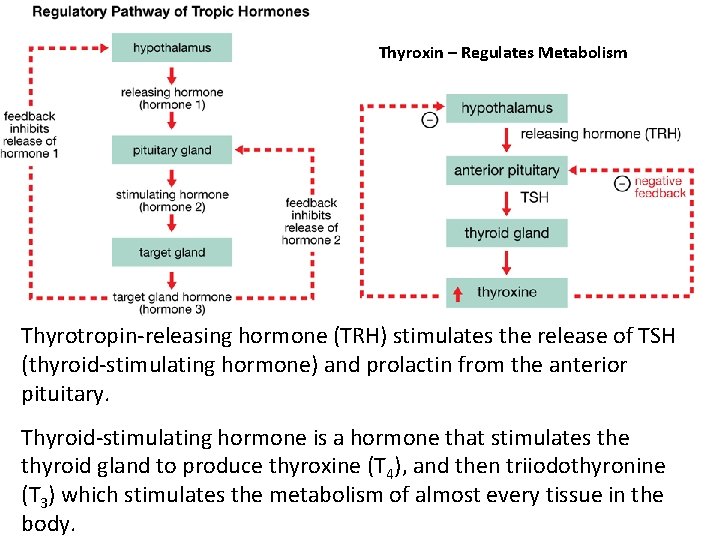
Thyroxin – Regulates Metabolism Thyrotropin-releasing hormone (TRH) stimulates the release of TSH (thyroid-stimulating hormone) and prolactin from the anterior pituitary. Thyroid-stimulating hormone is a hormone that stimulates the thyroid gland to produce thyroxine (T 4), and then triiodothyronine (T 3) which stimulates the metabolism of almost every tissue in the body.
The Stress Response
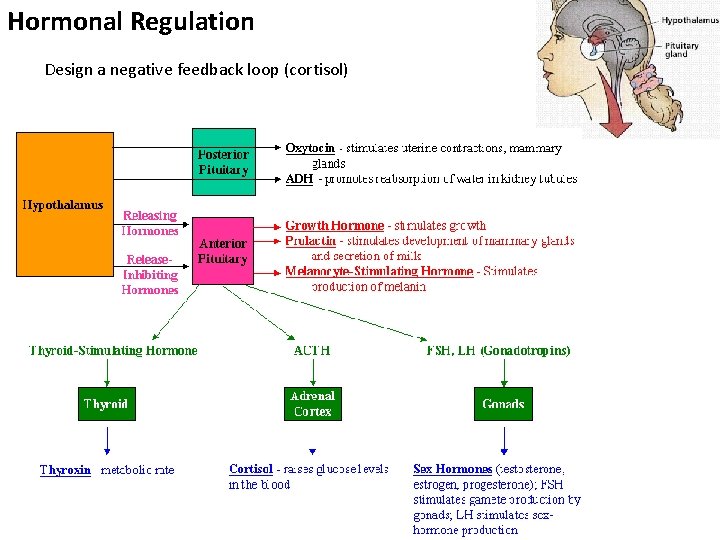
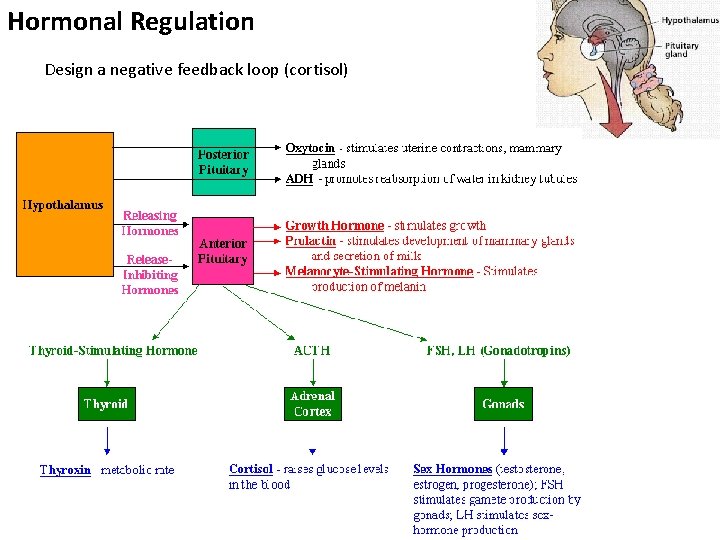
Hormonal Regulation Design a negative feedback loop (cortisol)

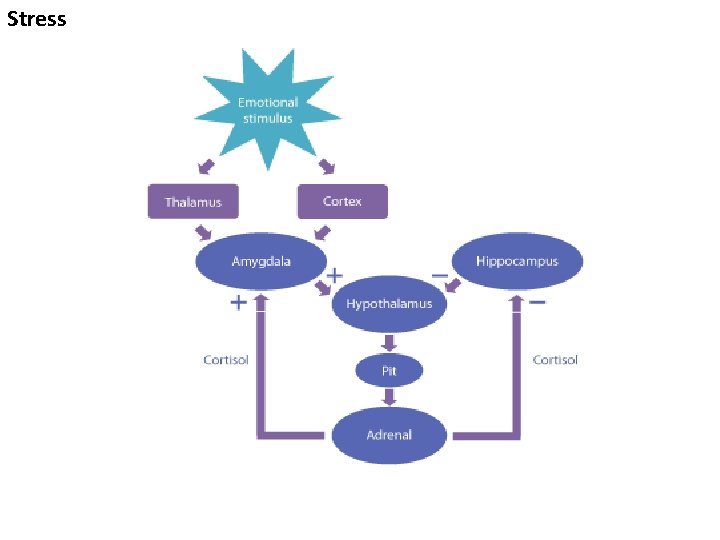
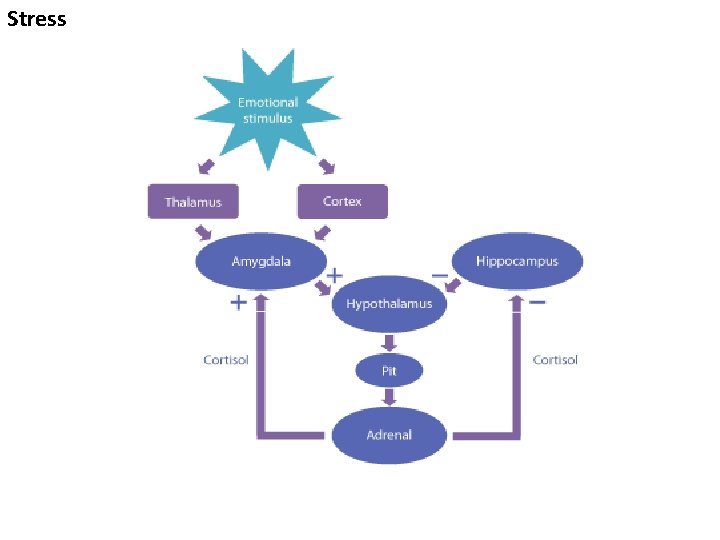
Stress
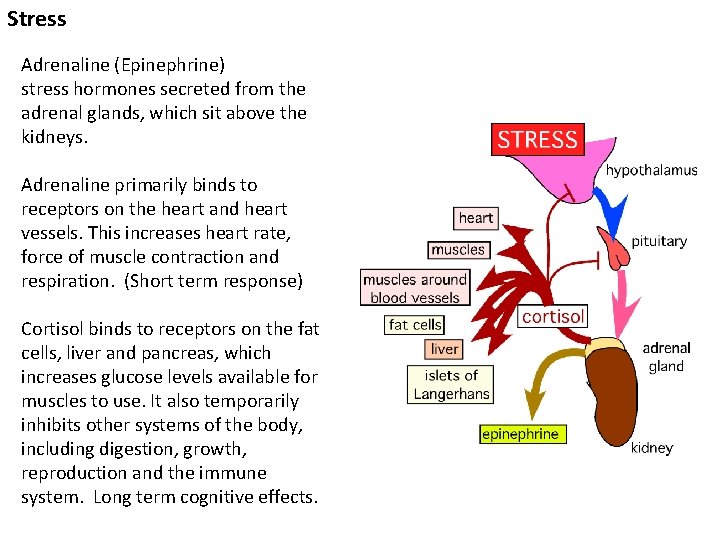
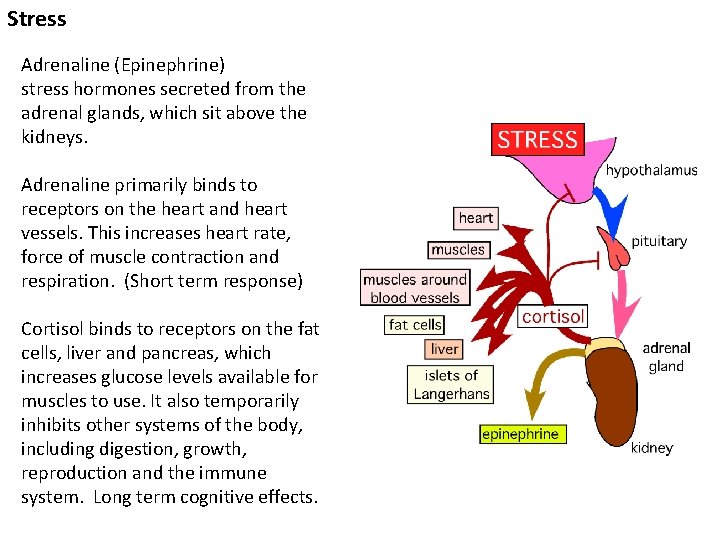
Stress Adrenaline (Epinephrine) stress hormones secreted from the adrenal glands, which sit above the kidneys. Adrenaline primarily binds to receptors on the heart and heart vessels. This increases heart rate, force of muscle contraction and respiration. (Short term response) Cortisol binds to receptors on the fat cells, liver and pancreas, which increases glucose levels available for muscles to use. It also temporarily inhibits other systems of the body, including digestion, growth, reproduction and the immune system. Long term cognitive effects.

http: //vimeo. com/42572194
Water Regulation
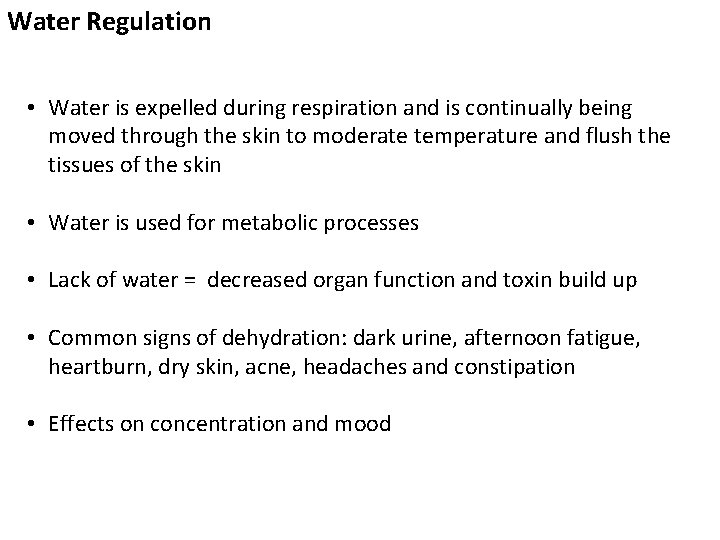
Water Regulation • Water is expelled during respiration and is continually being moved through the skin to moderate temperature and flush the tissues of the skin • Water is used for metabolic processes • Lack of water = decreased organ function and toxin build up • Common signs of dehydration: dark urine, afternoon fatigue, heartburn, dry skin, acne, headaches and constipation • Effects on concentration and mood
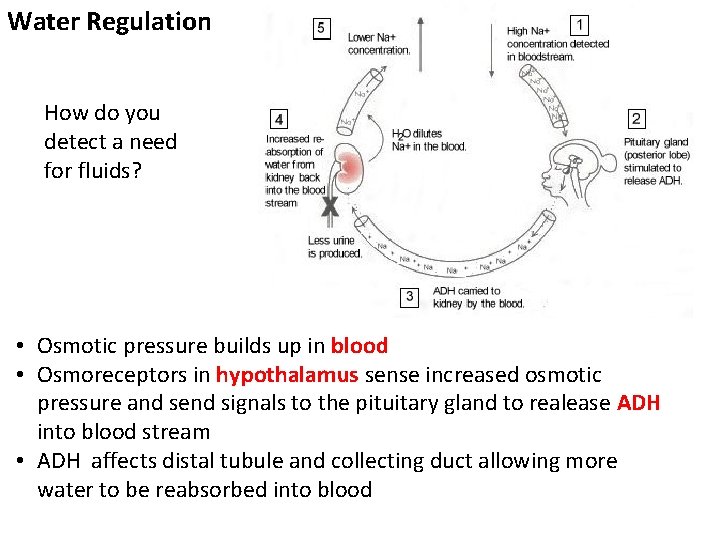
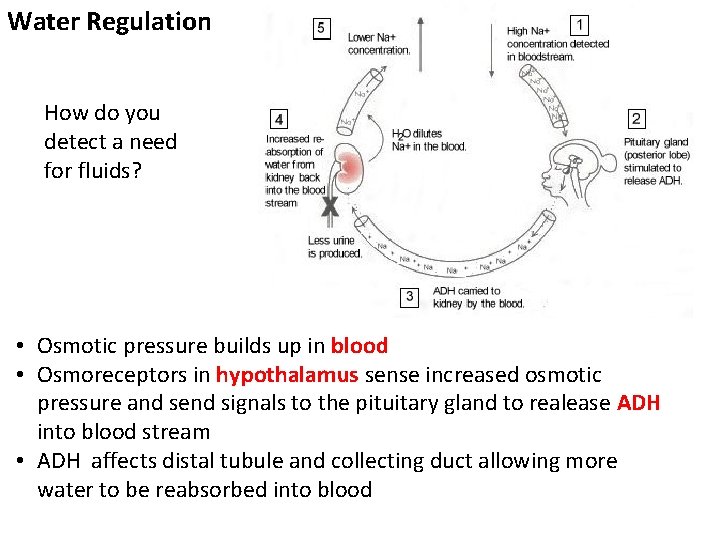
Water Regulation How do you detect a need for fluids? • Osmotic pressure builds up in blood • Osmoreceptors in hypothalamus sense increased osmotic pressure and send signals to the pituitary gland to realease ADH into blood stream • ADH affects distal tubule and collecting duct allowing more water to be reabsorbed into blood
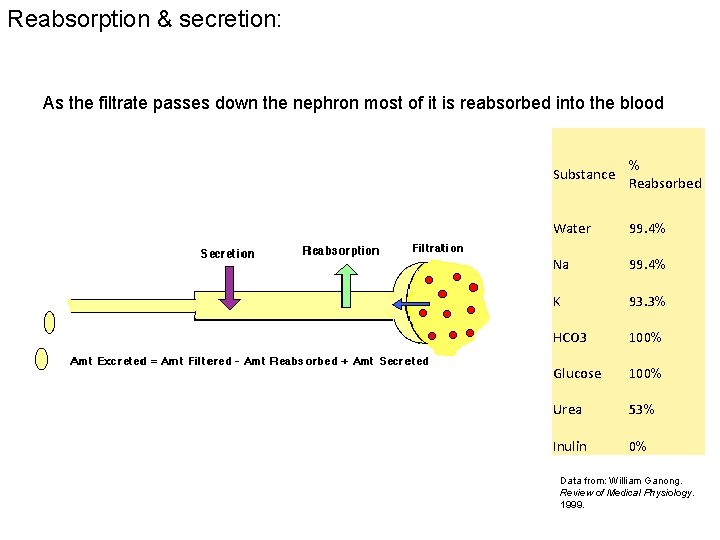
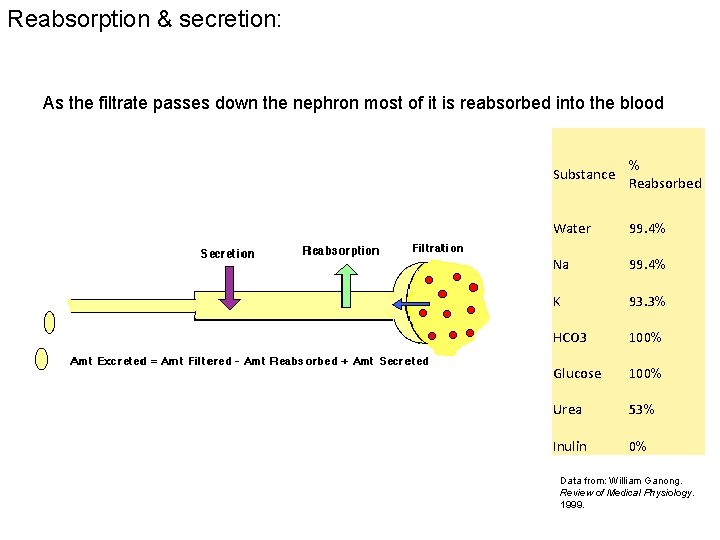
Reabsorption & secretion: As the filtrate passes down the nephron most of it is reabsorbed into the blood Substance % Reabsorbed Water 99. 4% Na 99. 4% K 93. 3% HCO 3 100% Glucose 100% Urea 53% Inulin 0% Data from: William Ganong. Review of Medical Physiology. 1999.
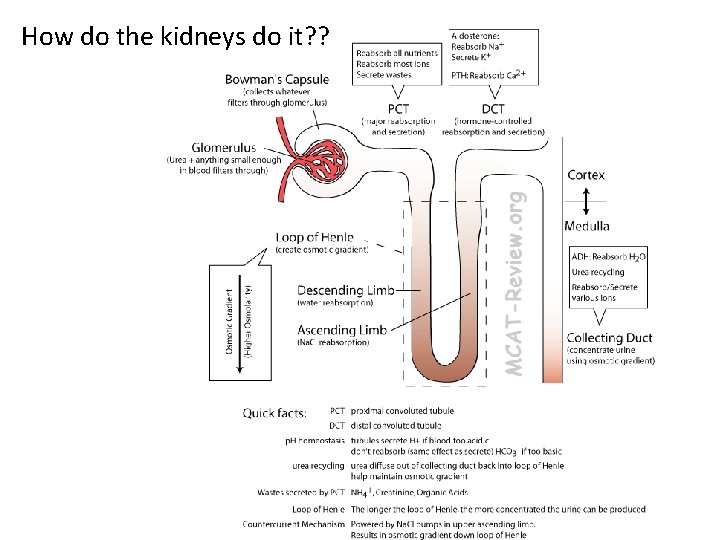
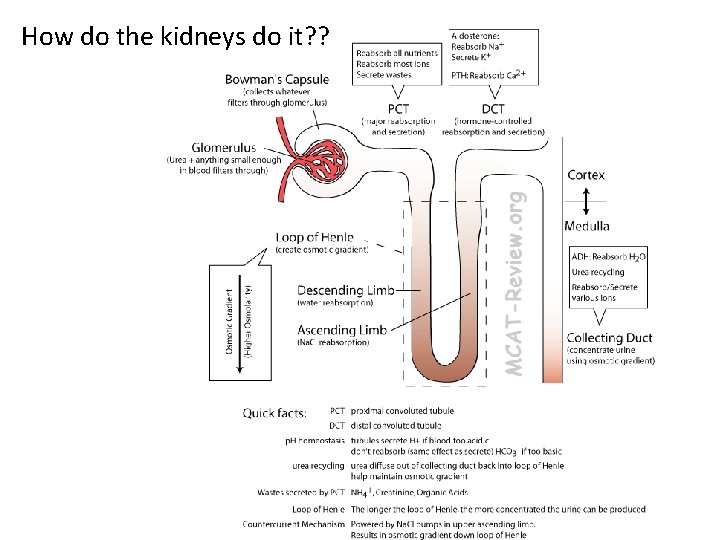
How do the kidneys do it? ?
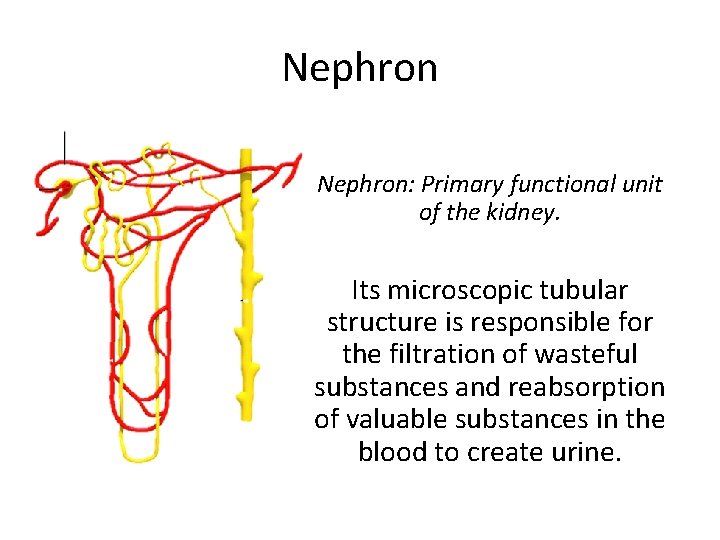
Nephron: Primary functional unit of the kidney. Its microscopic tubular structure is responsible for the filtration of wasteful substances and reabsorption of valuable substances in the blood to create urine.
Steps necessary to create URINE 1. Glomerular Filtration 2. Tubular reabsorption 3. Tubular secretion 4. Water reabsorption
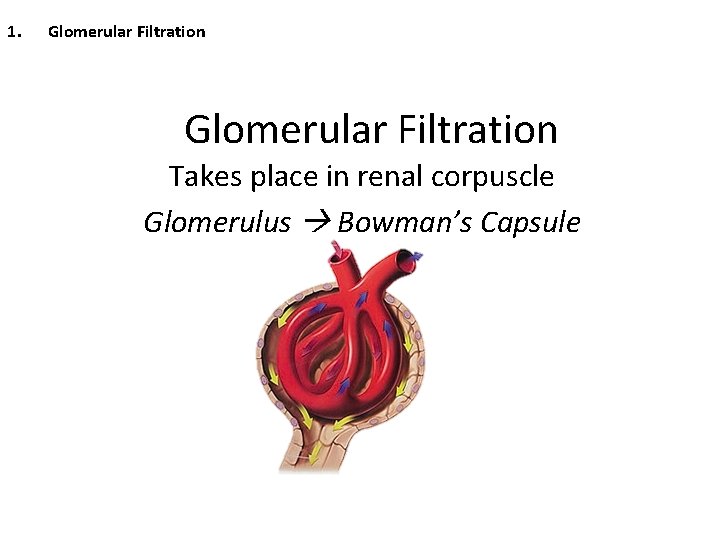
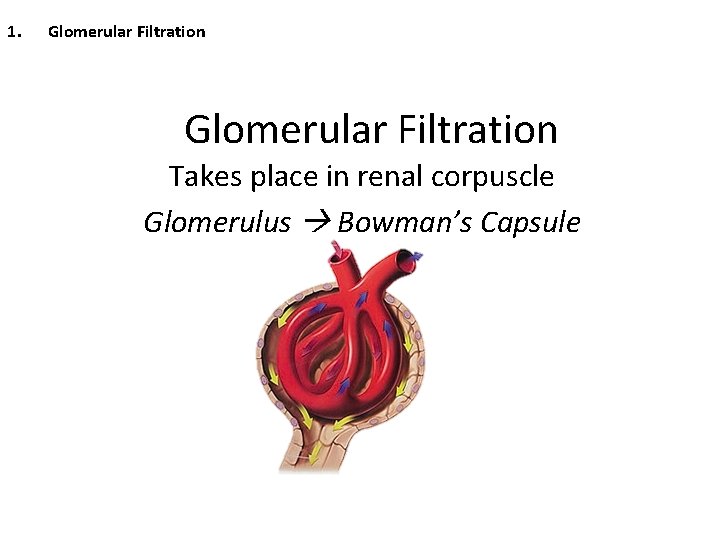
1. Glomerular Filtration Takes place in renal corpuscle Glomerulus Bowman’s Capsule
1. Glomerular Filtration • Glomerulus: Bundle of fine capillaries in which blood first enters the kidneys – Water and other small substances are forced into the Bowman’s Capsule • • Water Salts/ions (Na+ & K+) Glucose Waste product: Urea Glomerular Filtrate – Formed to rid of the toxic ammonia – byproduct of metabolic process of liver from amino acids
1. Glomerular Filtration Factors affecting Glomerular Filtration ① Permeability of glomerulus ② Blood Pressure – 4 times higher blood pressure than any other capillary • Source of the force used for filtration.
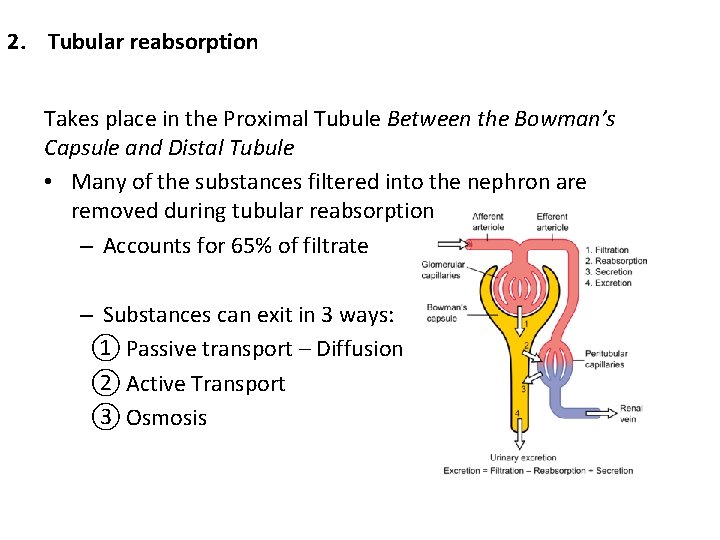
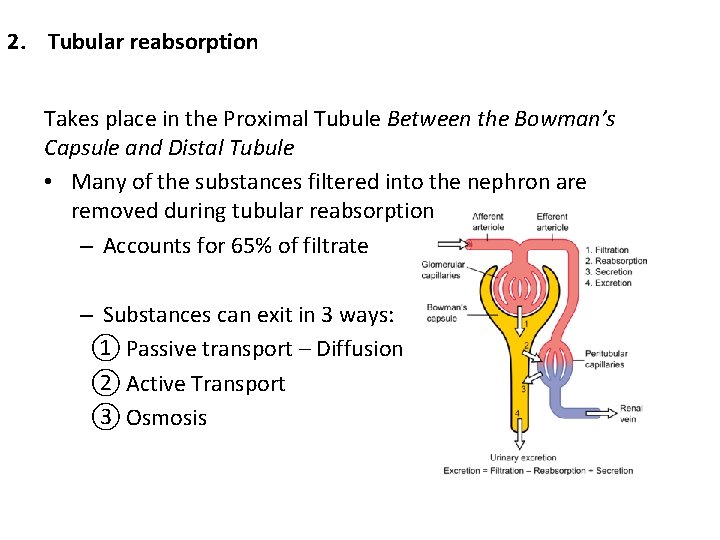
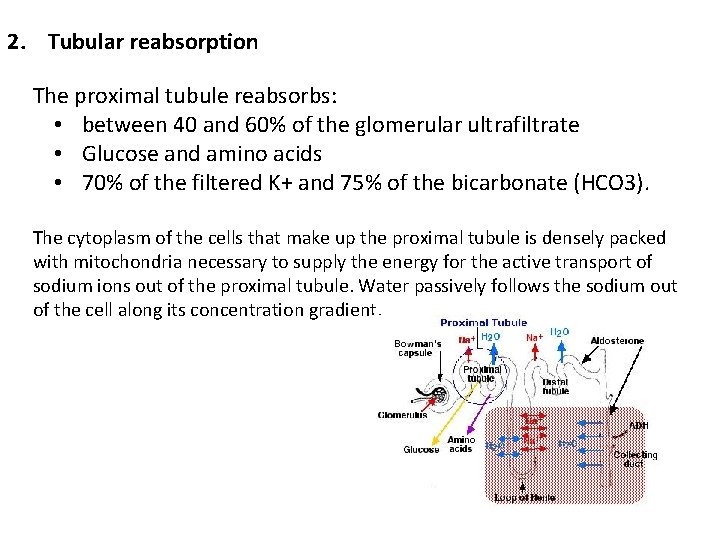
2. Tubular reabsorption Takes place in the Proximal Tubule Between the Bowman’s Capsule and Distal Tubule • Many of the substances filtered into the nephron are removed during tubular reabsorption – Accounts for 65% of filtrate – Substances can exit in 3 ways: ① Passive transport – Diffusion ② Active Transport ③ Osmosis
2. Tubular reabsorption Reabsorption in Proximal Tubule • Active transport – Salts (Na+ & K+) – Glucose – Amino acids • Passive Transport – Negatively charged ions (Cl- & HCO 3 -) a. Electrical attraction with cations • Osmosis – Water is reabsorbed
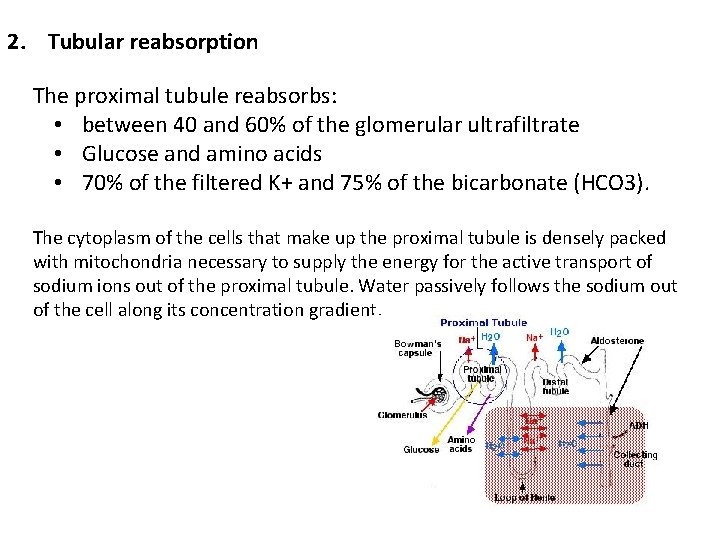
2. Tubular reabsorption The proximal tubule reabsorbs: • between 40 and 60% of the glomerular ultrafiltrate • Glucose and amino acids • 70% of the filtered K+ and 75% of the bicarbonate (HCO 3). The cytoplasm of the cells that make up the proximal tubule is densely packed with mitochondria necessary to supply the energy for the active transport of sodium ions out of the proximal tubule. Water passively follows the sodium out of the cell along its concentration gradient.
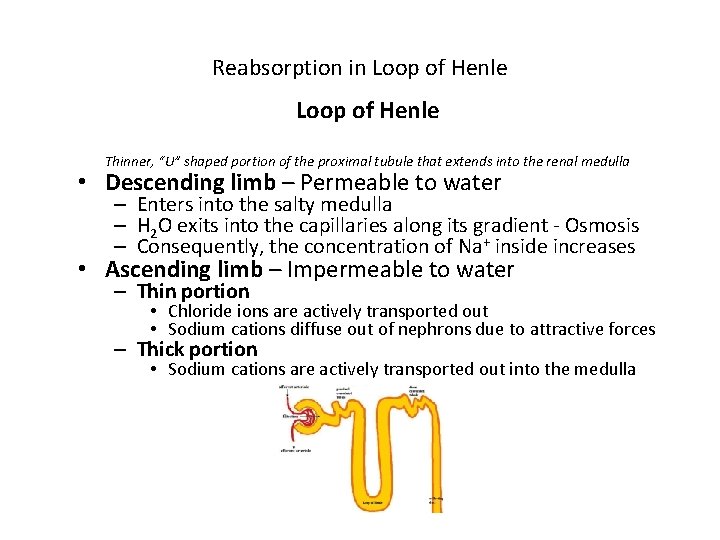
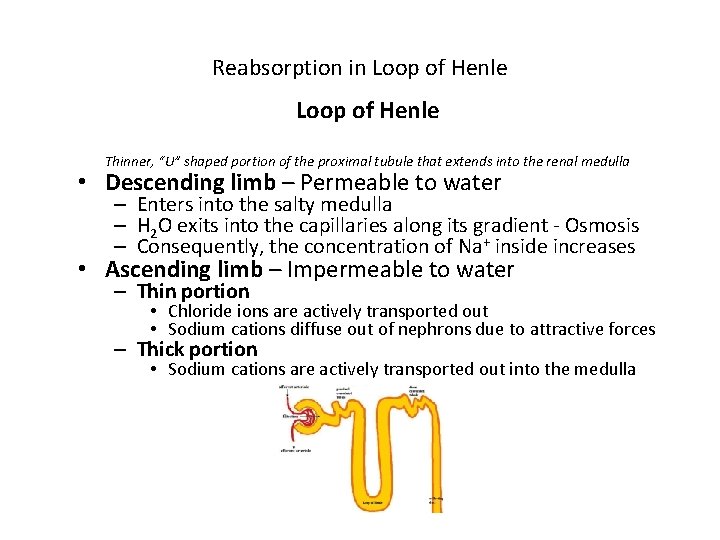
Reabsorption in Loop of Henle Thinner, “U” shaped portion of the proximal tubule that extends into the renal medulla • Descending limb – Permeable to water – Enters into the salty medulla – H 2 O exits into the capillaries along its gradient - Osmosis – Consequently, the concentration of Na+ inside increases • Ascending limb – Impermeable to water – Thin portion • Chloride ions are actively transported out • Sodium cations diffuse out of nephrons due to attractive forces – Thick portion • Sodium cations are actively transported out into the medulla
Importance of Na+ removal from Nephrons ① Replenishes the salty environment of medulla ② Makes filtrate less concentrated than surrounding tissues and blood No sodium ions ever enter the capillaries during tubular reabsorption
3. Tubular Secretion Takes place in the Distal Tubule Immediately prior to collecting duct • Two primary secretions: ①Potassium ions (K+) ②Hydrogen ions (H+) – Regulate blood p. H by the removal of H+
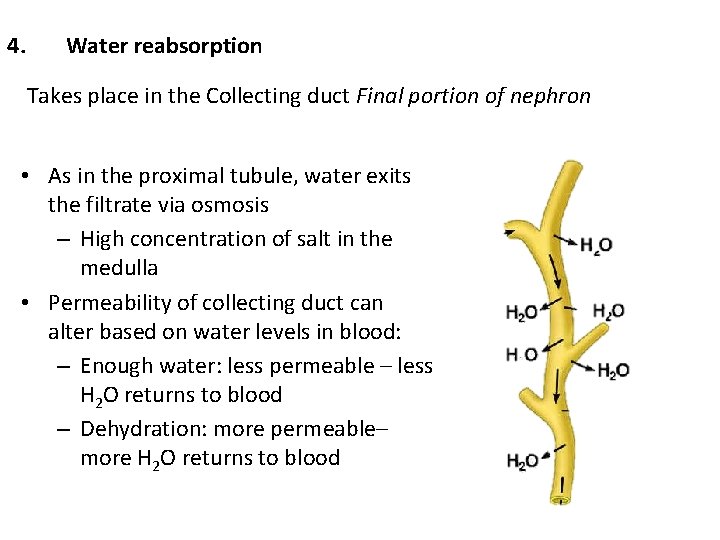
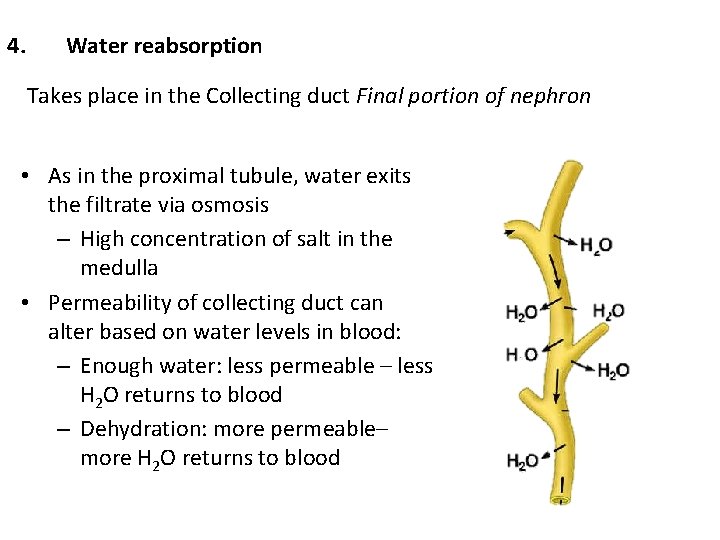
4. Water reabsorption Takes place in the Collecting duct Final portion of nephron • As in the proximal tubule, water exits the filtrate via osmosis – High concentration of salt in the medulla • Permeability of collecting duct can alter based on water levels in blood: – Enough water: less permeable – less H 2 O returns to blood – Dehydration: more permeable– more H 2 O returns to blood
Urine has been created! … but what is it? • Only 1% of the initial distillate from glomerulus – 99% is re-absorbed by blood • Total of 180 Liters of distillate enter the nephrons per day – 178. 2 L return to blood – 1. 8 L is removed via urine
Reabsorption & secretion: • A few substances are secreted from the blood to the nephron • Reabsorption and secretion are energy intensive- the kidney is one of the most metabolically active organs in the body • Filtering substances into the tubules and then reabsorbing nearly 100% of them, using energy, may seem to be a very wastefull process, but it allows the body to quickly remove many toxic substances from the blood (they are usually not reabsorbed) Net Process: Amt in Urine = Amt Filtered - Amt Reabsorbed + Amt Secreted Glomerular Filtration is Easy to Measure From Inulin or Creatinine Clearance

Functions of the Excretory System 1. Excretion of Metabolic Wastes -Mainly nitrogen containing wastes. 2. Maintenance of Water- Salt Balance -Indirectly regulates blood volumes. 3. Maintenance of Acid – Base Balance -Carbonic acid buffer system. 4. Secretion of Hormones -Calcitriol (calcium absorption) + erythropoietin (production of red blood cells).
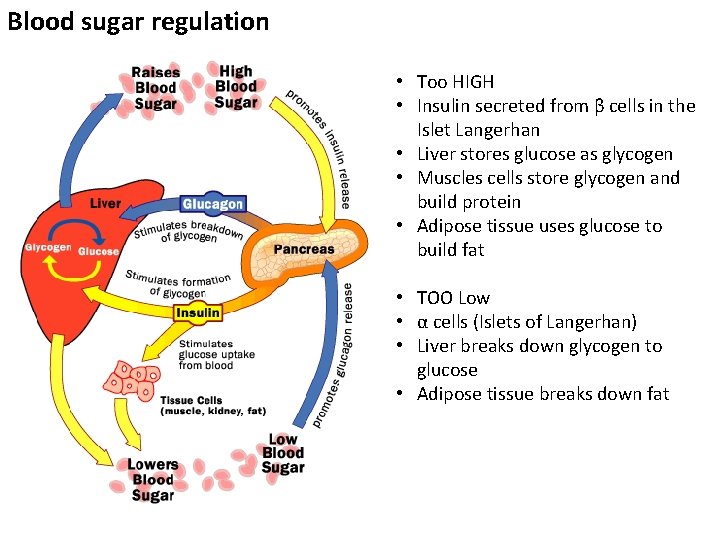
Blood Sugar Regulation
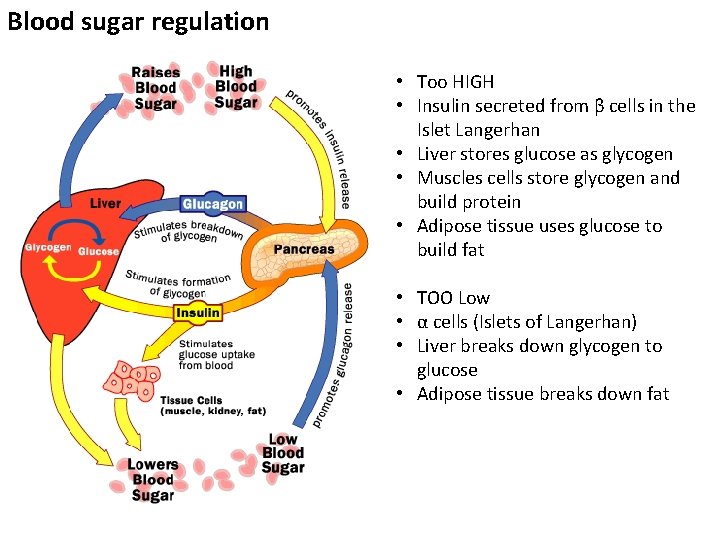
Blood sugar regulation • Too HIGH • Insulin secreted from β cells in the Islet Langerhan • Liver stores glucose as glycogen • Muscles cells store glycogen and build protein • Adipose tissue uses glucose to build fat • TOO Low • α cells (Islets of Langerhan) • Liver breaks down glycogen to glucose • Adipose tissue breaks down fat
Figures to know and love: Figures: 9. 13, 9. 16, 9. 18, 9. 20, 10. 4, 10. 6, 10. 11, 10. 12 Table 10. 3
 Homeostatic regulation usually involves
Homeostatic regulation usually involves Negative feedback loop
Negative feedback loop Keystone acidosis
Keystone acidosis Carbonic acid buffer system
Carbonic acid buffer system Homeostatic imbalances of the skeletal system
Homeostatic imbalances of the skeletal system Skin homeostatic imbalances
Skin homeostatic imbalances Example of topic outline and sentence outline
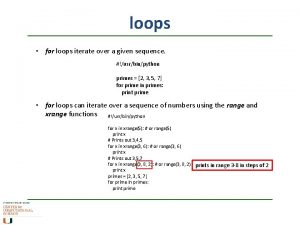
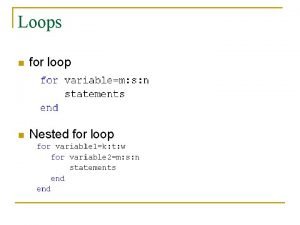
Example of topic outline and sentence outline Nested loops java
Nested loops java Flush shared pool
Flush shared pool Virtual loops
Virtual loops Lesson 13 bee nested loops
Lesson 13 bee nested loops Looping bersarang
Looping bersarang Loops in sequence diagram
Loops in sequence diagram Featureless loops of wangensteen meaning
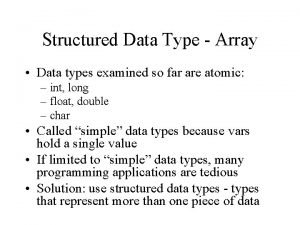
Featureless loops of wangensteen meaning Is array a structured data type
Is array a structured data type Nested loop pseudocode
Nested loop pseudocode Dynamic obstruction intestine
Dynamic obstruction intestine Sun means
Sun means Loops o repeticiones
Loops o repeticiones While loop in matlab
While loop in matlab Non touching loop example
Non touching loop example Broadcasts packets, but creates loops in the systems.
Broadcasts packets, but creates loops in the systems. Nested loops storytelling
Nested loops storytelling Nested loops python
Nested loops python Nested loop complexity
Nested loop complexity Hirschsprung disease
Hirschsprung disease Relation between loop branch and node is given by
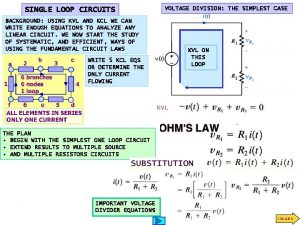
Relation between loop branch and node is given by Lesson 7 sticker art with loops
Lesson 7 sticker art with loops N nested for loops
N nested for loops Non touching loops in control system
Non touching loops in control system Matlab break
Matlab break Be8255 lecture notes ppt
Be8255 lecture notes ppt Python sentinel loop
Python sentinel loop Matlab for loop example problems
Matlab for loop example problems Kvl loop
Kvl loop Its platinum loops shrink to a wedding-ring
Its platinum loops shrink to a wedding-ring Loops in pascal
Loops in pascal Geothermal loops design
Geothermal loops design Loops controlled by an accumulator
Loops controlled by an accumulator Turtle small basic
Turtle small basic