HIV SELFTESTING HIVST IN MEN WHO HAVE SEX



- Slides: 24
HIV SELF-TESTING (HIVST) IN MEN WHO HAVE SEX WITH MEN (MSM) Sheri A. Lippman, Ph. D, MPH Center for AIDS Prevention Studies University of California, San Francisco
ROADMAP • Potential of HIV self-testing (HIVST) • What have we learned? • What remains unclear? • How will we get answers?
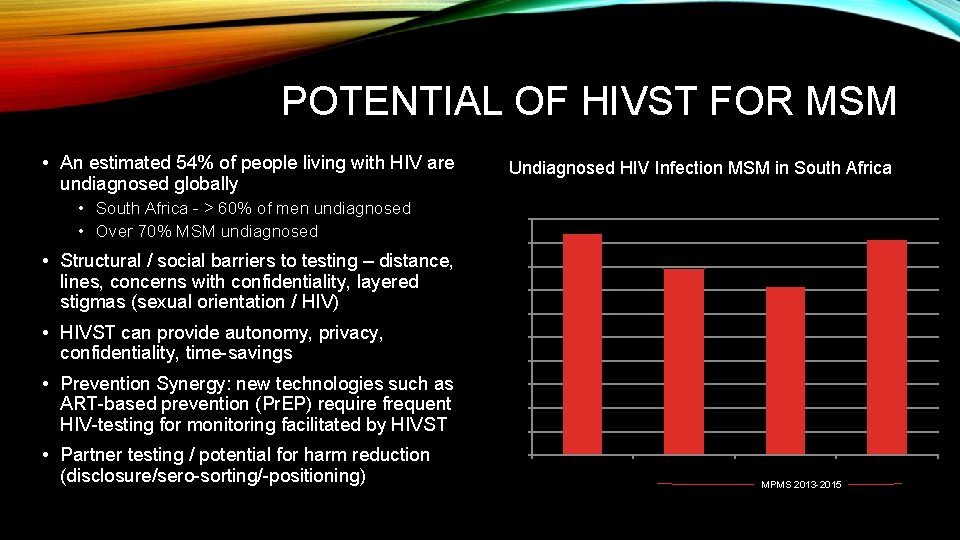
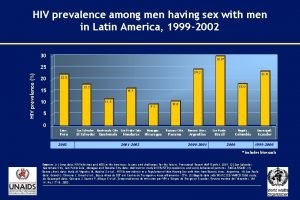
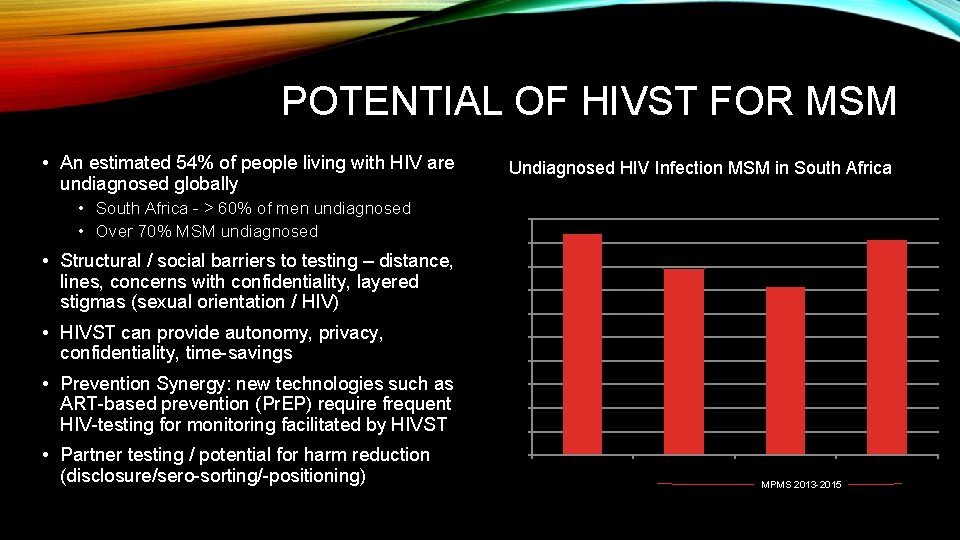
POTENTIAL OF HIVST FOR MSM • An estimated 54% of people living with HIV are undiagnosed globally • South Africa - > 60% of men undiagnosed • Over 70% MSM undiagnosed • Structural / social barriers to testing – distance, lines, concerns with confidentiality, layered stigmas (sexual orientation / HIV) • HIVST can provide autonomy, privacy, confidentiality, time-savings • Prevention Synergy: new technologies such as ART-based prevention (Pr. EP) require frequent HIV-testing for monitoring facilitated by HIVST • Partner testing / potential for harm reduction (disclosure/sero-sorting/-positioning) Undiagnosed HIV Infection MSM in South Africa 100% 94. 00% 91. 6% 90% 79. 1% 80% 71. 6% 70% 60% 50% 40% 30% 20% 10% 0% Baral 2009 Lane (Baseline) Lane (1 st Follow-Up) Lane (2 nd Follow-Up) MPMS 2013 -2015
POTENTIAL DRAWBACKS • Harms – coercion / violence / adverse emotional reactions • Lost opportunity for STI screening and counseling • Test performance (sensitivity/long window period w/out counseling) • Unprotected intercourse following negative test (issue of window period and increased STI transmission) • Cost

CURRENT AVAILABILITY • The US and UK have licensed oral and blood products, respectively • EU, France, Australia, Hong Kong, China, and Kenya have made HIVST legal • Supportive regulations in discussions in a number of countries • Informally sold kits in 5+ countries and on internet Johannesburg airport pharmacy, 2014
WHAT HAVE WE LEARNED ABOUT HIV SELF-TESTING AMONG MSM?
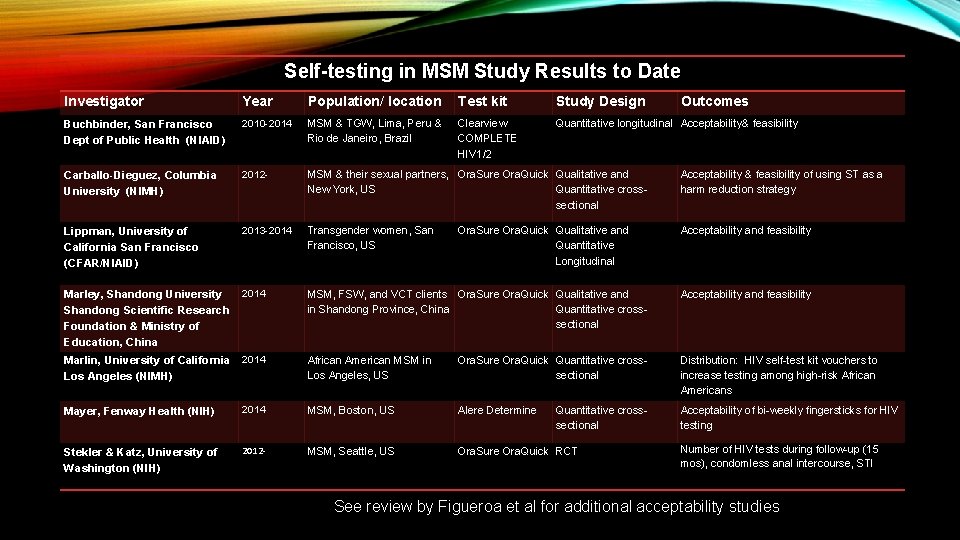
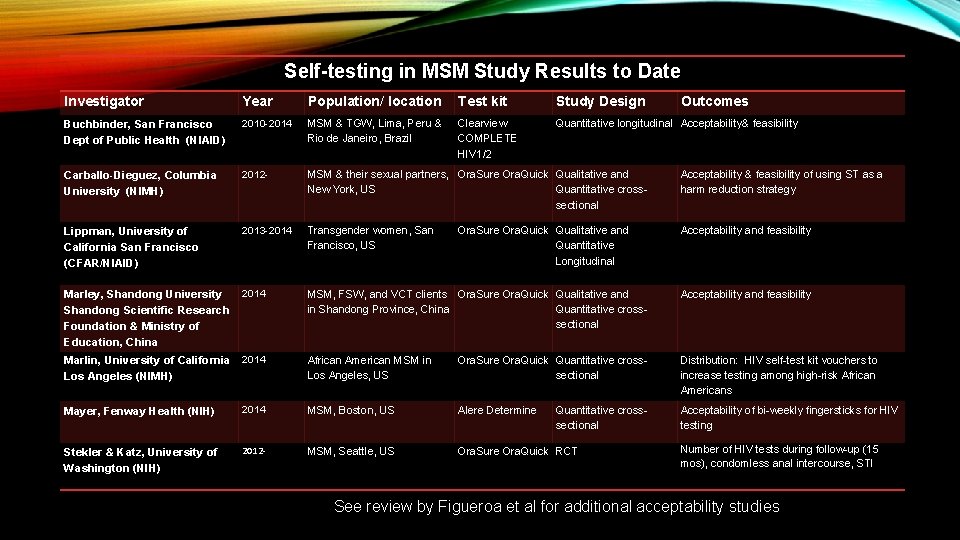
Self-testing in MSM Study Results to Date Investigator Year Population/ location Test kit Study Design Buchbinder, San Francisco Dept of Public Health (NIAID) 2010 -2014 MSM & TGW, Lima, Peru & Rio de Janeiro, Brazil Clearview COMPLETE HIV 1/2 Quantitative longitudinal Acceptability& feasibility Carballo-Dieguez, Columbia University (NIMH) 2012 - MSM & their sexual partners, Ora. Sure Ora. Quick Qualitative and New York, US Quantitative crosssectional Acceptability & feasibility of using ST as a harm reduction strategy Lippman, University of California San Francisco (CFAR/NIAID) 2013 -2014 Transgender women, San Francisco, US Acceptability and feasibility Marley, Shandong University Shandong Scientific Research Foundation & Ministry of Education, China 2014 MSM, FSW, and VCT clients Ora. Sure Ora. Quick Qualitative and in Shandong Province, China Quantitative crosssectional Acceptability and feasibility African American MSM in Los Angeles, US Ora. Sure Ora. Quick Quantitative crosssectional Distribution: HIV self-test kit vouchers to increase testing among high-risk African Americans Acceptability of bi-weekly fingersticks for HIV testing Marlin, University of California 2014 Los Angeles (NIMH) Ora. Sure Ora. Quick Qualitative and Quantitative Longitudinal Mayer, Fenway Health (NIH) 2014 MSM, Boston, US Alere Determine Stekler & Katz, University of Washington (NIH) 2012 - MSM, Seattle, US Ora. Sure Ora. Quick RCT Quantitative crosssectional Outcomes Number of HIV tests during follow-up (15 mos), condomless anal intercourse, STI See review by Figueroa et al for additional acceptability studies
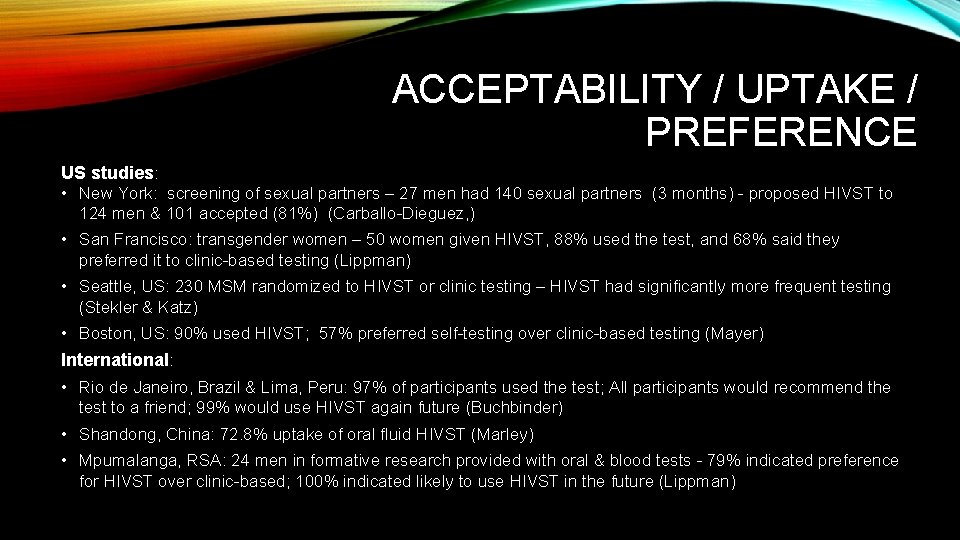
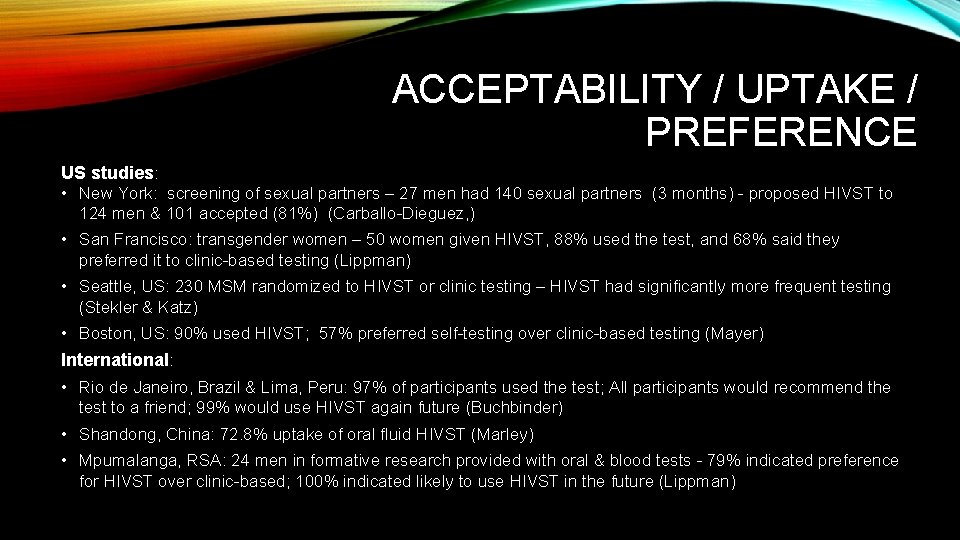
ACCEPTABILITY / UPTAKE / PREFERENCE US studies: • New York: screening of sexual partners – 27 men had 140 sexual partners (3 months) - proposed HIVST to 124 men & 101 accepted (81%) (Carballo-Dieguez, ) • San Francisco: transgender women – 50 women given HIVST, 88% used the test, and 68% said they preferred it to clinic-based testing (Lippman) • Seattle, US: 230 MSM randomized to HIVST or clinic testing – HIVST had significantly more frequent testing (Stekler & Katz) • Boston, US: 90% used HIVST; 57% preferred self-testing over clinic-based testing (Mayer) International: • Rio de Janeiro, Brazil & Lima, Peru: 97% of participants used the test; All participants would recommend the test to a friend; 99% would use HIVST again future (Buchbinder) • Shandong, China: 72. 8% uptake of oral fluid HIVST (Marley) • Mpumalanga, RSA: 24 men in formative research provided with oral & blood tests - 79% indicated preference for HIVST over clinic-based; 100% indicated likely to use HIVST in the future (Lippman)
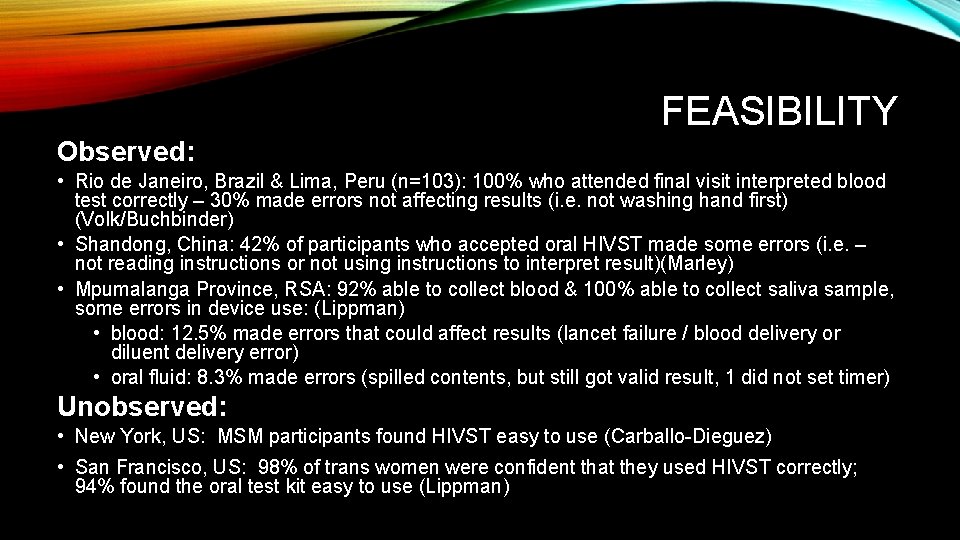
FEASIBILITY Observed: • Rio de Janeiro, Brazil & Lima, Peru (n=103): 100% who attended final visit interpreted blood test correctly – 30% made errors not affecting results (i. e. not washing hand first) (Volk/Buchbinder) • Shandong, China: 42% of participants who accepted oral HIVST made some errors (i. e. – not reading instructions or not using instructions to interpret result)(Marley) • Mpumalanga Province, RSA: 92% able to collect blood & 100% able to collect saliva sample, some errors in device use: (Lippman) • blood: 12. 5% made errors that could affect results (lancet failure / blood delivery or diluent delivery error) • oral fluid: 8. 3% made errors (spilled contents, but still got valid result, 1 did not set timer) Unobserved: • New York, US: MSM participants found HIVST easy to use (Carballo-Dieguez) • San Francisco, US: 98% of trans women were confident that they used HIVST correctly; 94% found the oral test kit easy to use (Lippman)
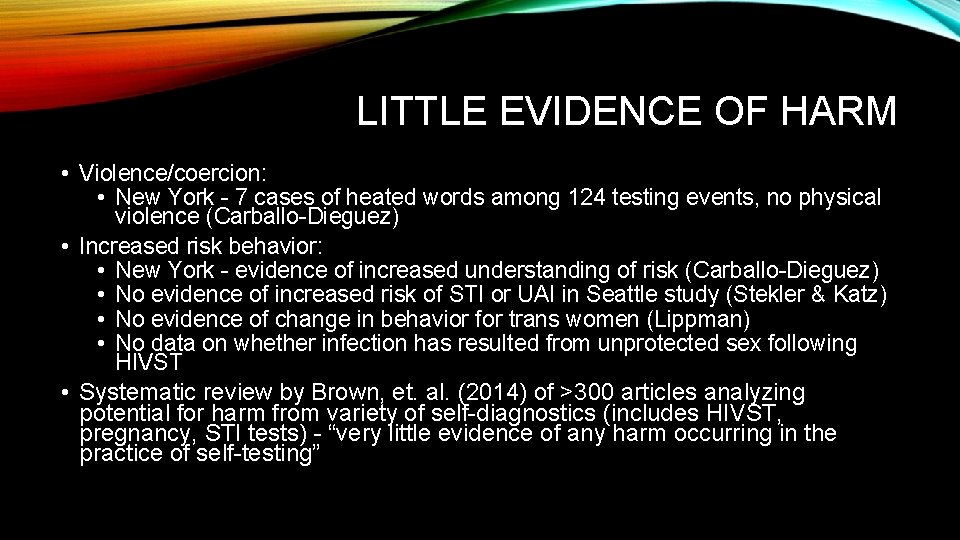
LITTLE EVIDENCE OF HARM • Violence/coercion: • New York - 7 cases of heated words among 124 testing events, no physical violence (Carballo-Dieguez) • Increased risk behavior: • New York - evidence of increased understanding of risk (Carballo-Dieguez) • No evidence of increased risk of STI or UAI in Seattle study (Stekler & Katz) • No evidence of change in behavior for trans women (Lippman) • No data on whether infection has resulted from unprotected sex following HIVST • Systematic review by Brown, et. al. (2014) of >300 articles analyzing potential for harm from variety of self-diagnostics (includes HIVST, pregnancy, STI tests) - “very little evidence of any harm occurring in the practice of self-testing”
WHAT REMAINS UNCLEAR? PART 1 – HUMAN BEHAVIOR • Will MSM test more frequently with HIVST? • Linkage to care using HIVST • Potential for harm / coercion • How HIVST will influence sexual behavior and risk of HIV and STI infection
INCREASE TESTING FREQUENCY & EARLY DETECTION? To date: • Seattle, US: 230 MSM randomized to HIVST or clinic testing – HIVST had significantly more frequent testing (Stekler & Katz) • Various studies found HIVST uptake among previous non-testers • Volk/Buchbinder – 16% never tested in Rio/Lima • Woods/Lippman – 7% never tested –SF bathhouse • Medline/Klausner – 11% never tested – LA Grindr Additional evidence to come: • Lightfoot, YMSMOC in Alameda, US – proportion new testers vs. county data • Sullivan, MSM, high prevalence US cities – testing frequency vs. comparison group (internet sample) • Buchbinder, YMSMOC in San Francisco and Alameda, US – testing frequency with HIVST vs. comparison condition (current SOC) • Lippman, MSM, South Africa – testing frequency with HIVST compared to past testing (cohort) • Merchant, YBMSM, multiple cities, US – uptake in HIVST group vs. comparison (clinic-based) • Guy, Australia - testing frequency and early detection vs. comparison group
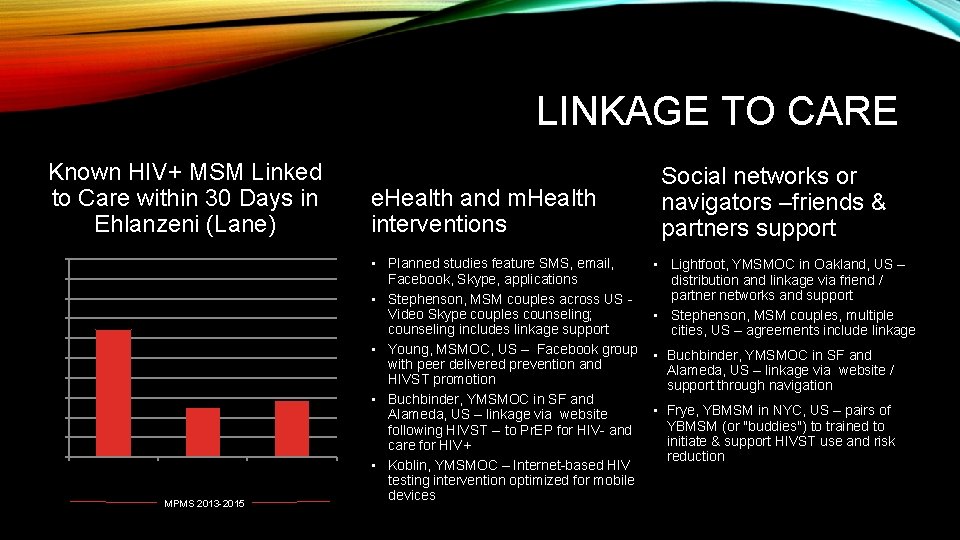
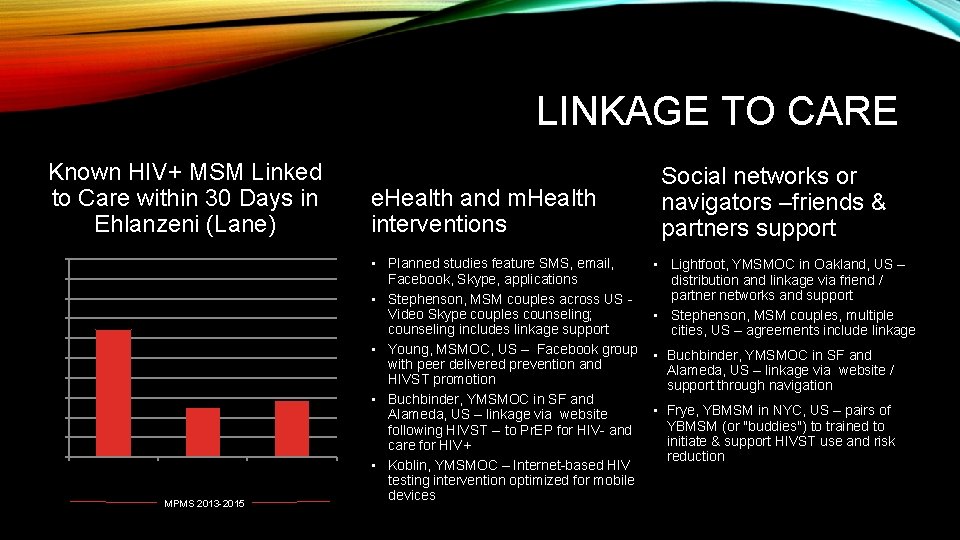
LINKAGE TO CARE Known HIV+ MSM Linked to Care within 30 Days in Ehlanzeni (Lane) 100% 90% 80% 70% 64. 29% 60% 50% 40% 25. 00% 30% 28. 57% 20% 10% 0% Baseline (n=14) 1 st Follow Up (n=36) MPMS 2013 -2015 2 nd Follow Up (n=14) e. Health and m. Health interventions • Planned studies feature SMS, email, Facebook, Skype, applications • Stephenson, MSM couples across US - Video Skype couples counseling; counseling includes linkage support • Young, MSMOC, US – Facebook group with peer delivered prevention and HIVST promotion • Buchbinder, YMSMOC in SF and Alameda, US – linkage via website following HIVST -- to Pr. EP for HIV- and care for HIV+ • Koblin, YMSMOC – Internet-based HIV testing intervention optimized for mobile devices Social networks or navigators –friends & partners support • Lightfoot, YMSMOC in Oakland, US – distribution and linkage via friend / partner networks and support • Stephenson, MSM couples, multiple cities, US – agreements include linkage • Buchbinder, YMSMOC in SF and Alameda, US – linkage via website / support through navigation • Frye, YBMSM in NYC, US – pairs of YBMSM (or "buddies") to trained to initiate & support HIVST use and risk reduction
SOCIAL HARM / ADVERSE EVENTS • Has been primary concern of community entry discussions • Monitoring and support within research setting / less obvious how this would be monitored with real-world roll-out Strategies to date: • 24 -hour helplines (toll-free) • Referral “coupons” • Counseling prior to test distribution Current research: • Stephenson (US) – couples Skype counseling • Frye (New York, US) – online “buddy system” and personalized e-testing plan • Lightfoot (Oakland, US) – peer-based distribution & support • Young (Los Angeles, US) – Facebook Group • Grinsztejn (Curitiba, Brazil) - Mobile services – online support
INCREASED RISKY SEXUAL BEHAVIOR Will this improve safety (harm reduction) or put people at risk? • In research settings – there is counseling around the window period • Carballo-Dieguez – MSM in NYC, US – no unprotected following a positive test • Katz / Stekler – no increases in unprotected anal intercourse Strategies to date: • Counseling about early infection / window period Current research: • Lippman - MSM in Mpumalanga Province, RSA – monitoring changes in sexual behavior and whether HIVST had direct influence • Stephenson – US couples HIVST (control) vs. couples HIVST + video Skype with a counselor – monitoring sexual risk taking and adherence agreements – sero concordant neg and discordant couples • Carballo-Dieguez – US MSM/TGW, NYC and San Juan – monitoring whether access to HIVST alters sexual risk among sex partners
WHAT REMAINS UNCLEAR? PART 2 – STRUCTURAL QUESTIONS • Regulations • Cost-effectiveness • Improvements to sensitivity and specificity? • How to distribute/deliver • Utilization / resource needs – effective instructions • Optimal packaging and labeling
HIV SELF-TEST PERFORMANCE • Can we reduce the window period? • In high risk populations – window period is particularly worrisome • Same in clinic settings in most of the world, but loss of counseling to educate about window period • Determine Rapid p 24 antigen / antibody combo recently approved by the FDA for healthcare settings, detects HIV in blood ~9 days earlier than antibody-only tests • Ideal to improve sensitivity • Ora. Sure Ora. Quick is most widely used HIVST - lower sensitivity (92%) than blood test, but easier to use, less invasive. (new tests may improve sensitivity) • Poor predictive value in low prevalence populations (low background prev) • Better predictive value among high-risk MSM • Sullivan, Chavez, Mac. Gowan US: will assess Ora. Quick, Sure. Check vs. DBS lab diagnosis • Mathematical modeling by Katz, et. al. suggested widespread use of oral tests could increase prevalence, due to long window period and false sense of security of negative results leading to greater sexual risk-taking

DISTRIBUTION FOR MSM • Will MSM purchase test kits? Target price? • Transwomen SF - $20 or less (or free) • MSM in Seattle – most said $20 or less • MSM in China – willing to pay around $10 via internet • Clinic distribution – nested in current HCT programming • Provides opportunity for in-person counseling, linkage to care • But undermines privacy, confidentiality that motivates HIVST use among MSM • Alternative distribution points preferred? • MSM respondents in South Africa expressed preference for obtaining through local NGOs (could provide counseling)
DISTRIBUTION FOR MSM, CONT’D Recent studies have looked at novel distribution methods: • Klausner / Young, Los Angeles • Outreach via Grindr, a gay dating app – 67% requested HIVST via mail; 30% vouchers for Walgreens; 3% choose code for use at vending machine. - ongoing due to popularity • Vouchers distributed through CBOs redeemable at Walgreens, by mail, or vending machines • Lippman and Woods, San Francisco – distribution at gay bathhouse (place-based distribution) • Tao, Beijing • Test ordered through the internet & sent in the mail • Sabharwal, New York City Health Department • Assessed HIVST uptake in MSM using partner testing (following HIV + index patient) Upcoming research utilizing novel distribution • Grinsztejn, Curitiba, Brazil – “e-test” ordered on the internet, delivered through mail, pick-up, or mobile testing • Lightfoot, Oakland, US – through social and sexual networks • Merchant, US – distribution through internet and social networking sites
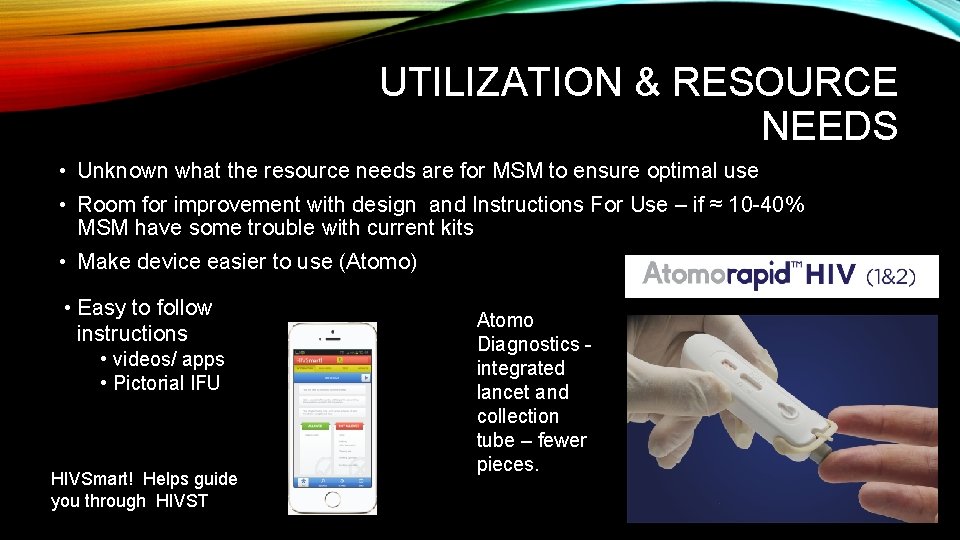
UTILIZATION & RESOURCE NEEDS • Unknown what the resource needs are for MSM to ensure optimal use • Room for improvement with design and Instructions For Use – if ≈ 10 -40% MSM have some trouble with current kits • Make device easier to use (Atomo) • Easy to follow instructions • videos/ apps • Pictorial IFU HIVSmart! Helps guide you through HIVST Atomo Diagnostics - integrated lancet and collection tube – fewer pieces.
MESSAGING & INSTRUCTIONS • Instructions for use (IFU) for low literacy • Fewer steps • More pictures • Clear follow-up guidance (e. g. if negative, re-test in 3 months, if positive, go to clinic) • Upcoming/ongoing studies: • Mavedzenge, general pop Zimbabwe – instructional videos • Not MSM – specific

DESIGN & PACKAGING • Discrete packaging? – hard for a stigmatized group to purchase / be seen with a large package with HIV test clearly displayed • Must appeal to MSM / target populations • Market research to target MSM? • Package in pairs? • Facilitates partner testing or repeat testing following window period • Partner uptake seems high (no studies to test uptake in single pack vs. double) Frog Designs /i. TEACH self-test packaging, Kwa. Zulu-Natal, RSA
CONCLUSIONS • Making progress – but much more research needed to document: • Uptake in different settings • Approaches for distribution • Facilitating linkage to care • Resource needs – for instructions and user support • Packaging and distribution target to MSM • Cost-effectiveness in high prevalence settings? • Potential adverse events/ harms
ACKNOWLEDGEMENTS • Hailey Gilmore and Alexander Marr • HIVST study collaborators in South Africa and the US: • • MSM Mpumalanga: Tim Lane, James Mc. Intyre, Oscar Radebe MSM Alameda County, US: Marguerita Lightfoot, Nick Moss Trans women, San Francisco: Jae Sevelius, Susan Buchbinder Young women Mpumalanga: Kathleen Kahn, Audrey Pettifor • Authors of the cited literature / planned research who provided information about their studies – Buchbinder/Scott, Carballo-Dieguez/Balan, Frye, Grinsztejn, Guy, Katz/Stekler, Koblin, Mayer, Stephenson, Young • Funding the above work: NIH, CDC, CHRP, CFAR/NIH
 Sex sex sex
Sex sex sex Kurt bumby
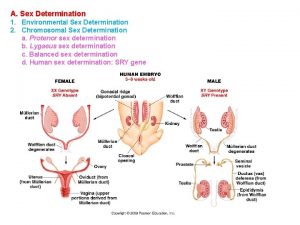
Kurt bumby Secondary sexual characters
Secondary sexual characters Sex in the greenhouse
Sex in the greenhouse Xxtesticles
Xxtesticles Sex determination and sex linkage
Sex determination and sex linkage Once a sex offender always a sex offender
Once a sex offender always a sex offender Sex
Sex What is sex linkage in biology
What is sex linkage in biology White men are saving brown women from brown men
White men are saving brown women from brown men It has 6 rectangular faces 12 edges and 6 vertices
It has 6 rectangular faces 12 edges and 6 vertices Do asexuals have sex
Do asexuals have sex How often do female dogs go into heat
How often do female dogs go into heat Can a dog get pregnant when not in heat
Can a dog get pregnant when not in heat Yu1u
Yu1u Vidas hiv duo ultra package insert
Vidas hiv duo ultra package insert Hiv virus
Hiv virus What does hiv diarrhea look like
What does hiv diarrhea look like Stadium hiv
Stadium hiv Basic hiv course
Basic hiv course Abcde hiv
Abcde hiv Triệu chứng nhiễm hiv
Triệu chứng nhiễm hiv Phagocytosis ap bio
Phagocytosis ap bio Syptoms of hiv
Syptoms of hiv Dot
Dot