Histopathology Laz Overview Very Important Quite Important Worth
- Slides: 49
Histopathology Laz
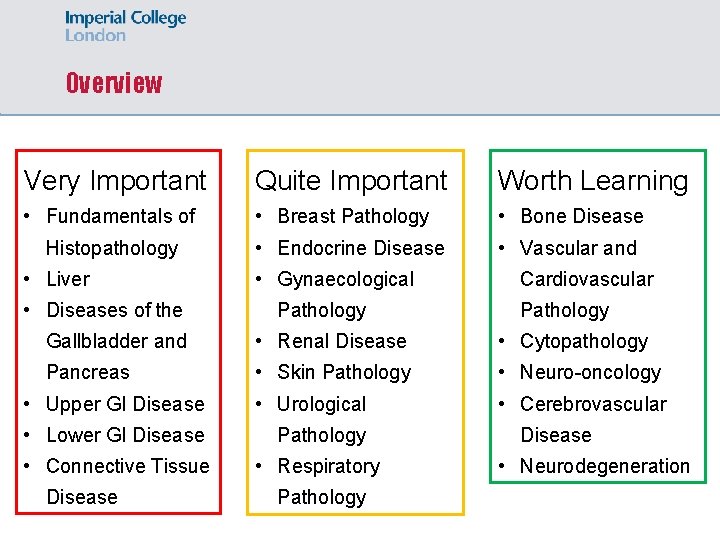
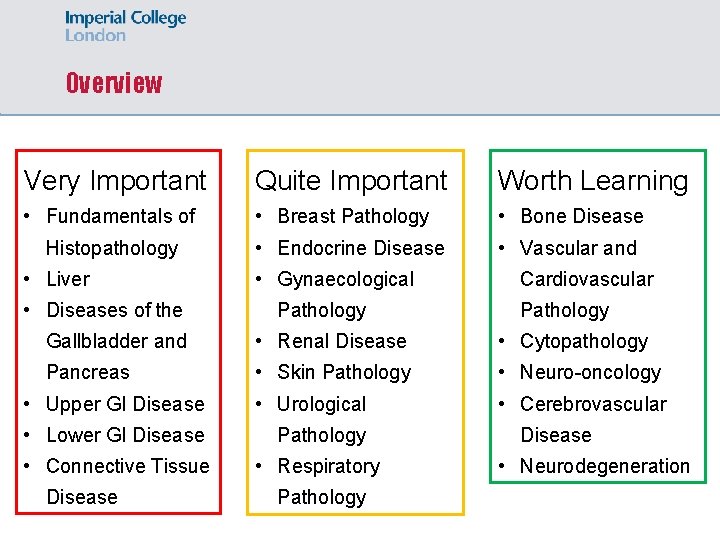
Overview Very Important Quite Important Worth Learning • Fundamentals of • Breast Pathology • Bone Disease • Endocrine Disease • Vascular and Histopathology • Liver • Diseases of the • Gynaecological Pathology Cardiovascular Pathology Gallbladder and • Renal Disease • Cytopathology Pancreas • Skin Pathology • Neuro-oncology • Upper GI Disease • Urological • Cerebrovascular • Lower GI Disease Pathology • Connective Tissue • Respiratory Disease Pathology Disease • Neurodegeneration
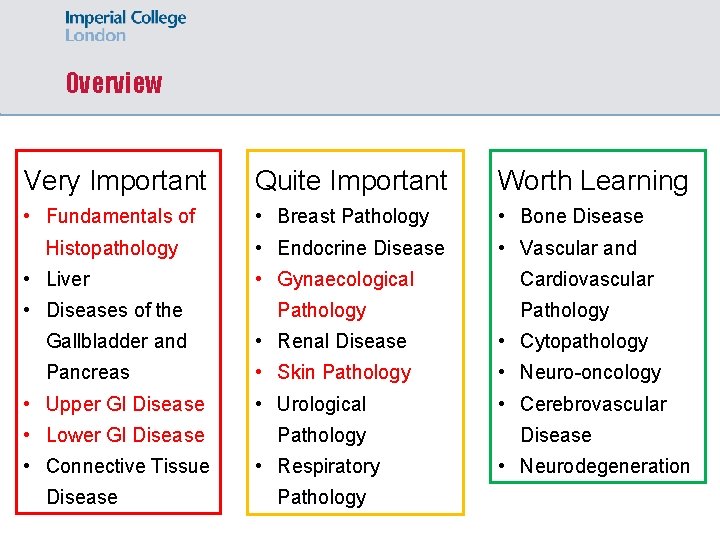
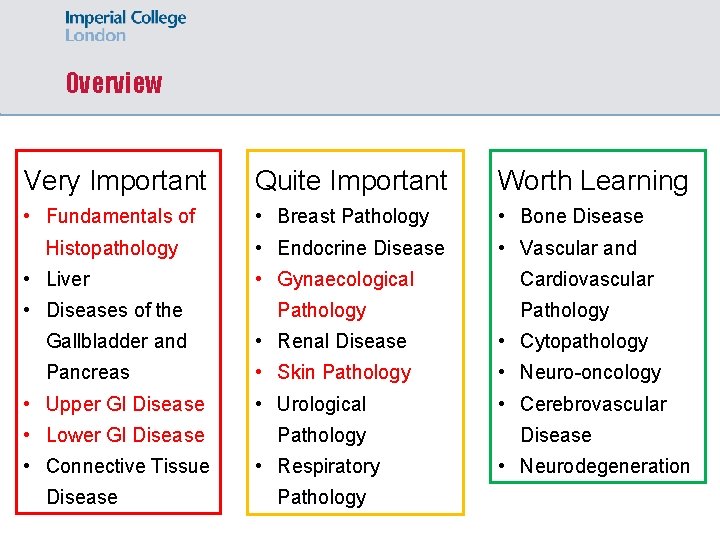
Overview Very Important Quite Important Worth Learning • Fundamentals of • Breast Pathology • Bone Disease • Endocrine Disease • Vascular and Histopathology • Liver • Diseases of the • Gynaecological Pathology Cardiovascular Pathology Gallbladder and • Renal Disease • Cytopathology Pancreas • Skin Pathology • Neuro-oncology • Upper GI Disease • Urological • Cerebrovascular • Lower GI Disease Pathology • Connective Tissue • Respiratory Disease Pathology Disease • Neurodegeneration
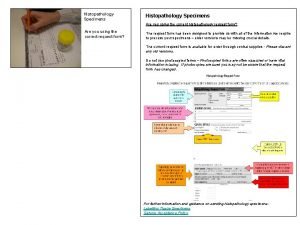
Fundamentals of Histopathology
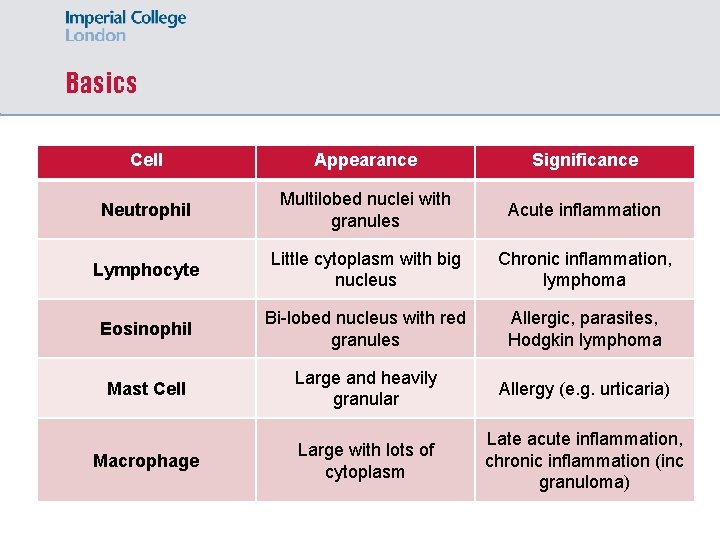
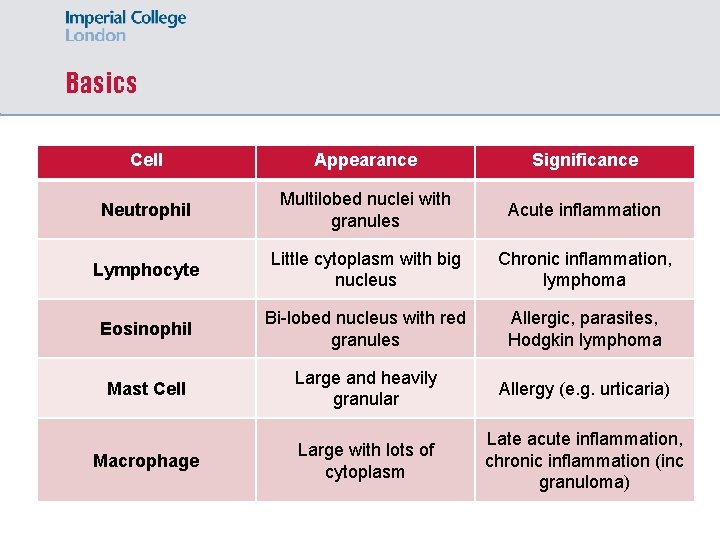
Basics Cell Appearance Significance Neutrophil Multilobed nuclei with granules Acute inflammation Lymphocyte Little cytoplasm with big nucleus Chronic inflammation, lymphoma Eosinophil Bi-lobed nucleus with red granules Allergic, parasites, Hodgkin lymphoma Mast Cell Large and heavily granular Allergy (e. g. urticaria) Macrophage Large with lots of cytoplasm Late acute inflammation, chronic inflammation (inc granuloma)
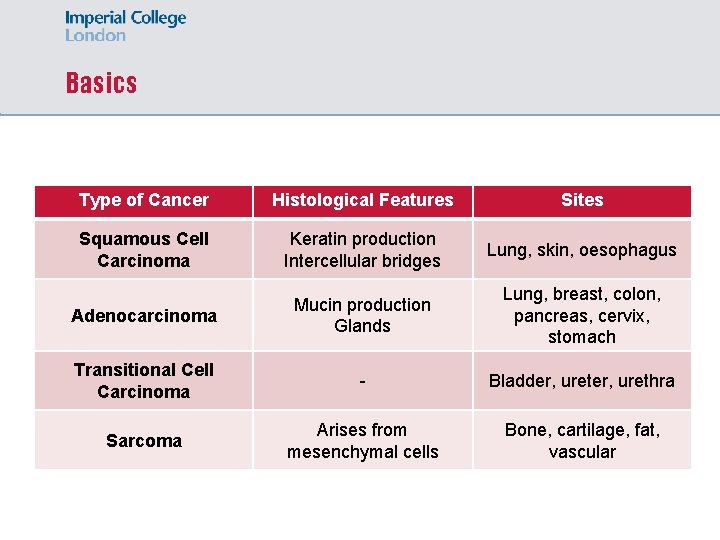
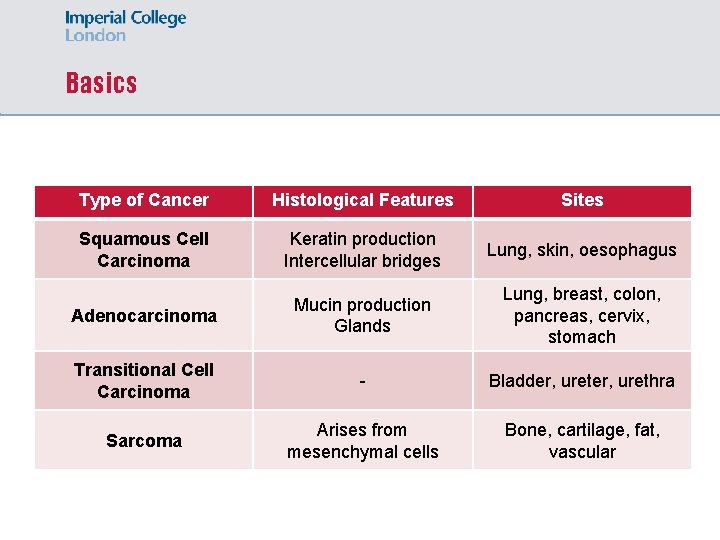
Basics Type of Cancer Histological Features Sites Squamous Cell Carcinoma Keratin production Intercellular bridges Lung, skin, oesophagus Adenocarcinoma Mucin production Glands Lung, breast, colon, pancreas, cervix, stomach Transitional Cell Carcinoma - Bladder, urethra Sarcoma Arises from mesenchymal cells Bone, cartilage, fat, vascular
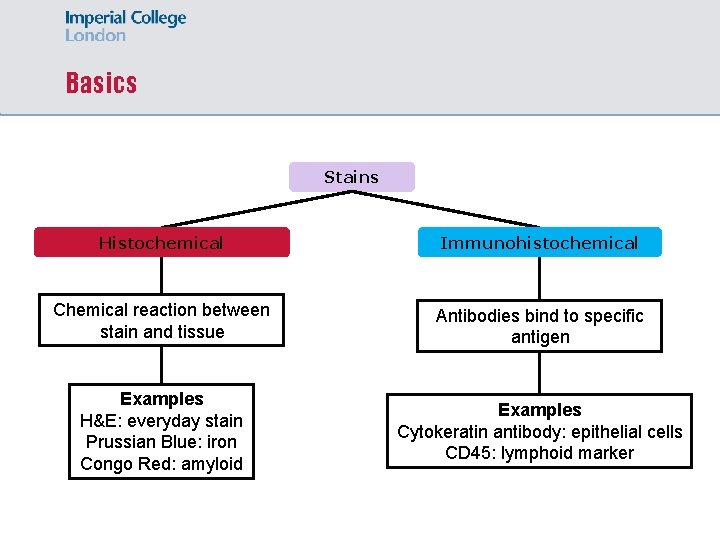
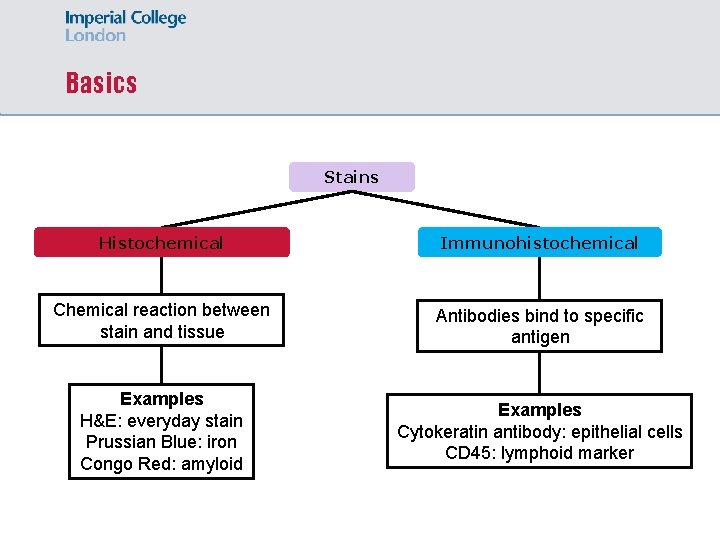
Basics Stains Histochemical Immunohistochemical Chemical reaction between stain and tissue Antibodies bind to specific antigen Examples H&E: everyday stain Prussian Blue: iron Congo Red: amyloid Examples Cytokeratin antibody: epithelial cells CD 45: lymphoid marker
Upper & Lower GI Pathology
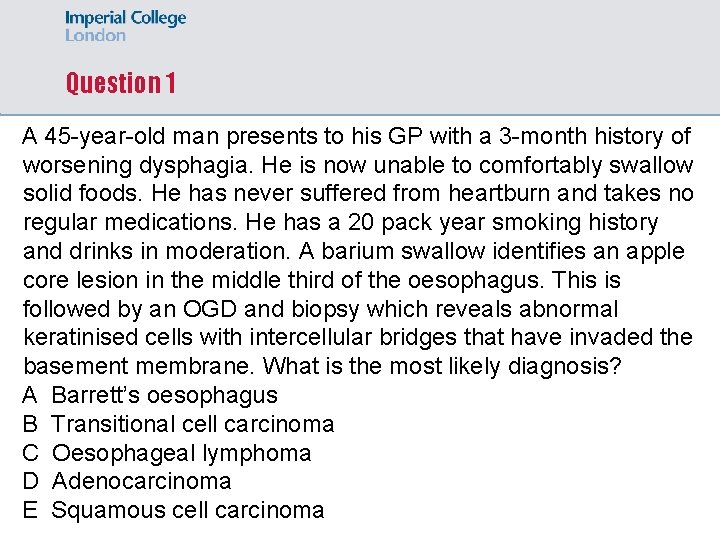
Question 1 A 45 -year-old man presents to his GP with a 3 -month history of worsening dysphagia. He is now unable to comfortably swallow solid foods. He has never suffered from heartburn and takes no regular medications. He has a 20 pack year smoking history and drinks in moderation. A barium swallow identifies an apple core lesion in the middle third of the oesophagus. This is followed by an OGD and biopsy which reveals abnormal keratinised cells with intercellular bridges that have invaded the basement membrane. What is the most likely diagnosis? A Barrett’s oesophagus B Transitional cell carcinoma C Oesophageal lymphoma D Adenocarcinoma E Squamous cell carcinoma
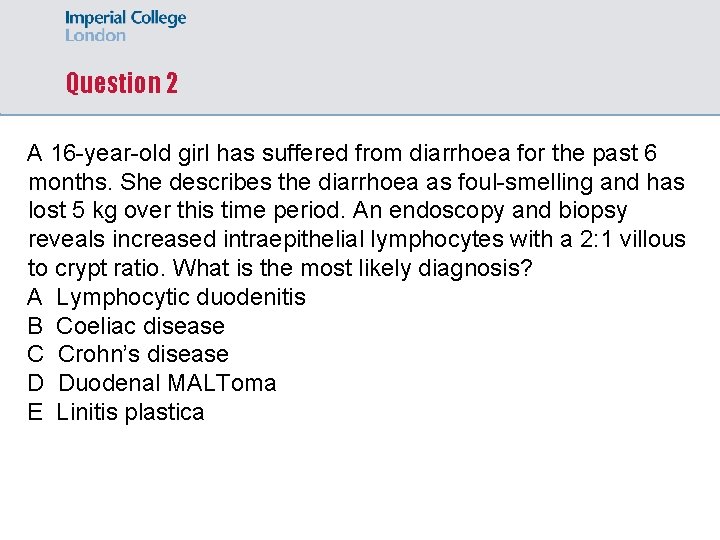
Question 2 A 16 -year-old girl has suffered from diarrhoea for the past 6 months. She describes the diarrhoea as foul-smelling and has lost 5 kg over this time period. An endoscopy and biopsy reveals increased intraepithelial lymphocytes with a 2: 1 villous to crypt ratio. What is the most likely diagnosis? A Lymphocytic duodenitis B Coeliac disease C Crohn’s disease D Duodenal MALToma E Linitis plastica
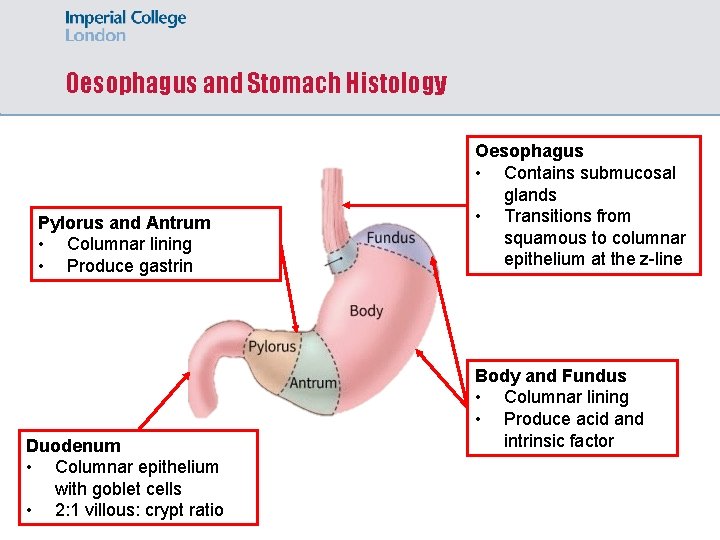
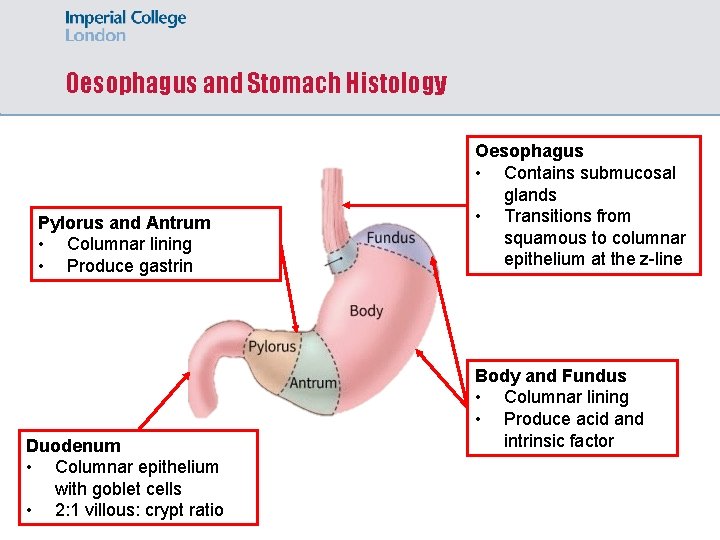
Oesophagus and Stomach Histology Pylorus and Antrum • Columnar lining • Produce gastrin Duodenum • Columnar epithelium with goblet cells • 2: 1 villous: crypt ratio Oesophagus • Contains submucosal glands • Transitions from squamous to columnar epithelium at the z-line Body and Fundus • Columnar lining • Produce acid and intrinsic factor
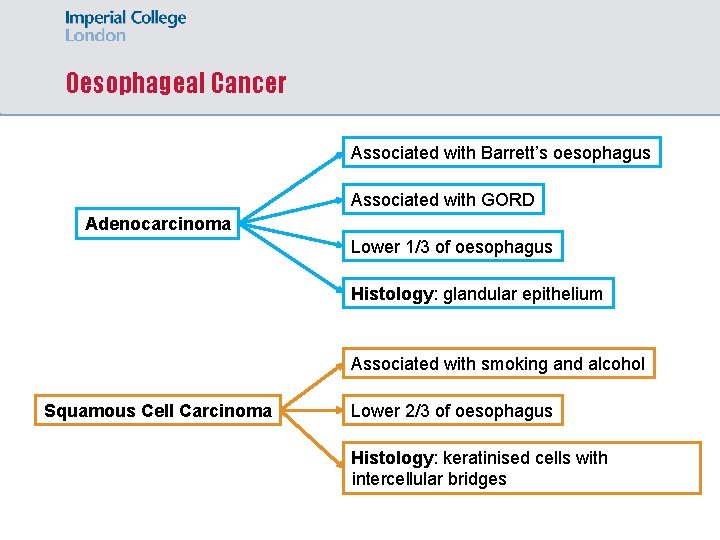
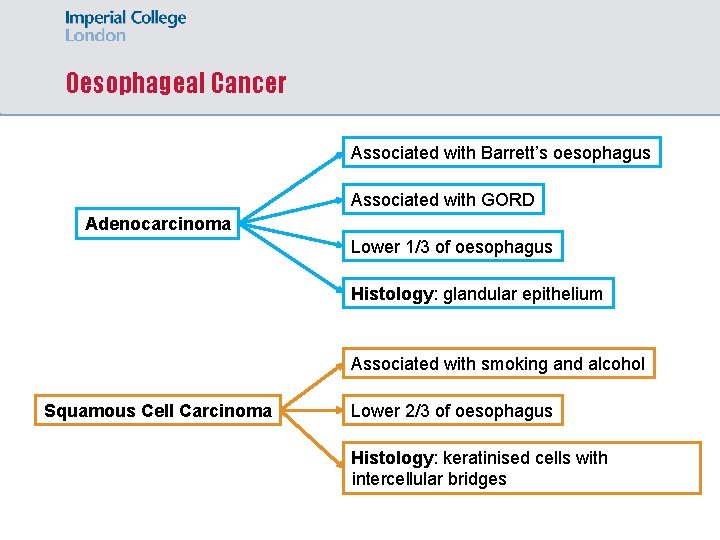
Oesophageal Cancer Associated with Barrett’s oesophagus Associated with GORD Adenocarcinoma Lower 1/3 of oesophagus Histology: glandular epithelium Associated with smoking and alcohol Squamous Cell Carcinoma Lower 2/3 of oesophagus Histology: keratinised cells with intercellular bridges
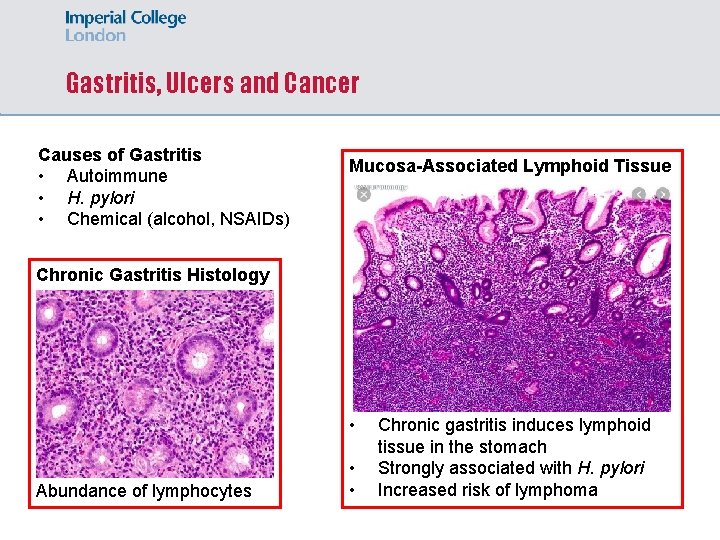
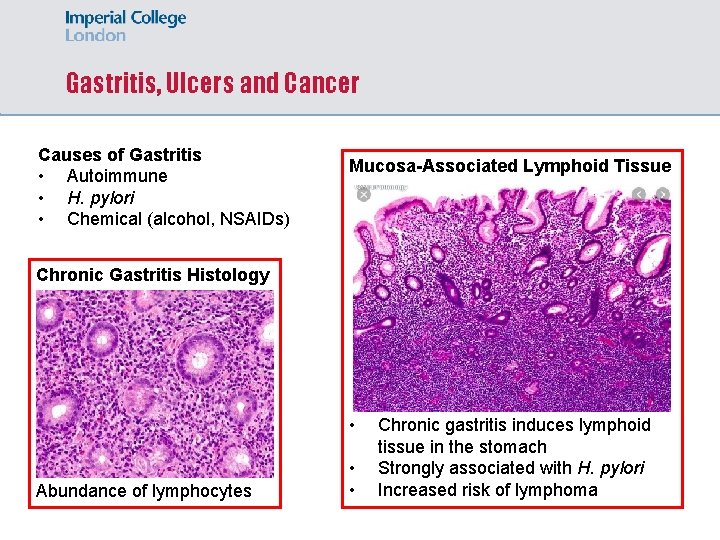
Gastritis, Ulcers and Cancer Causes of Gastritis • Autoimmune • H. pylori • Chemical (alcohol, NSAIDs) Mucosa-Associated Lymphoid Tissue Chronic Gastritis Histology • Abundance of lymphocytes • • Chronic gastritis induces lymphoid tissue in the stomach Strongly associated with H. pylori Increased risk of lymphoma
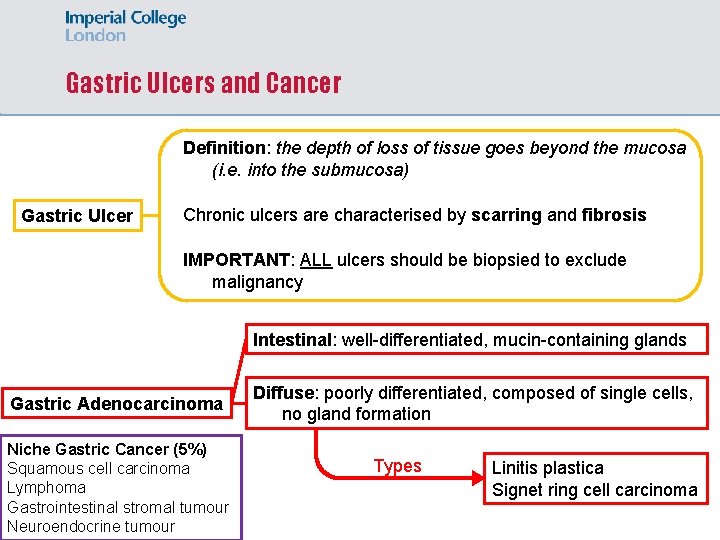
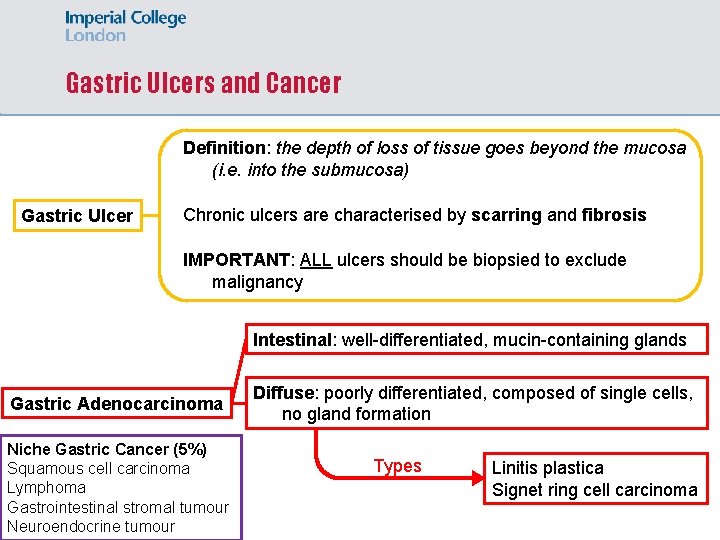
Gastric Ulcers and Cancer Definition: the depth of loss of tissue goes beyond the mucosa (i. e. into the submucosa) Gastric Ulcer Chronic ulcers are characterised by scarring and fibrosis IMPORTANT: ALL ulcers should be biopsied to exclude malignancy Intestinal: well-differentiated, mucin-containing glands Gastric Adenocarcinoma Niche Gastric Cancer (5%) Squamous cell carcinoma Lymphoma Gastrointestinal stromal tumour Neuroendocrine tumour Diffuse: poorly differentiated, composed of single cells, no gland formation Types Linitis plastica Signet ring cell carcinoma
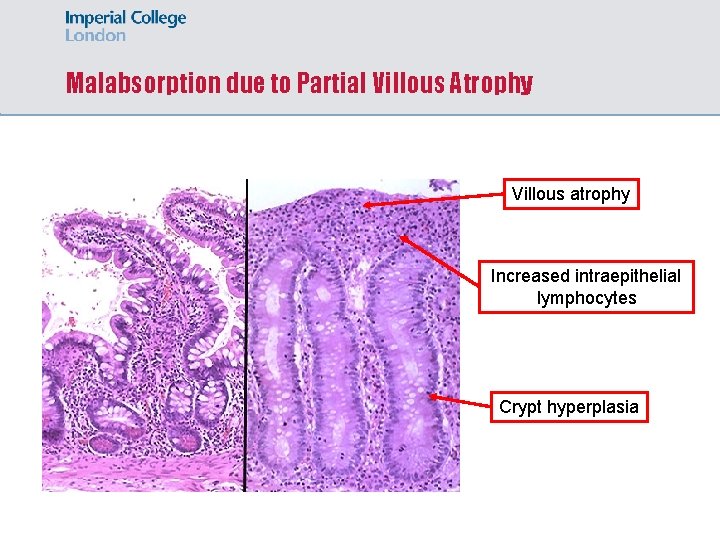
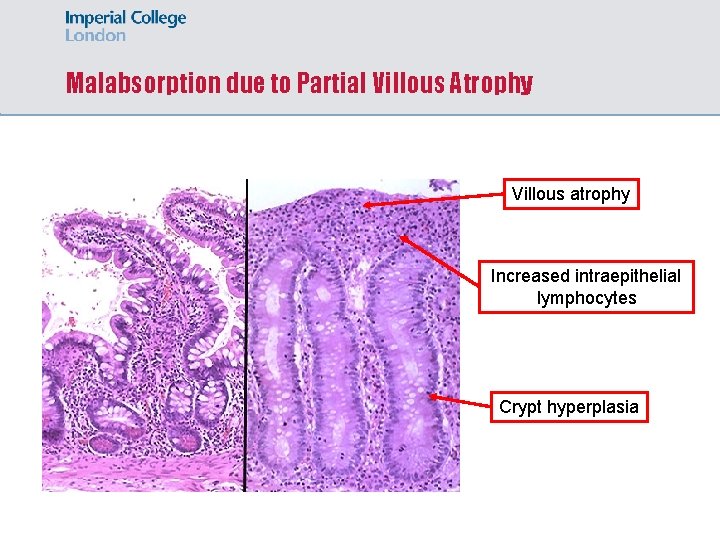
Malabsorption due to Partial Villous Atrophy Villous atrophy Increased intraepithelial lymphocytes Crypt hyperplasia
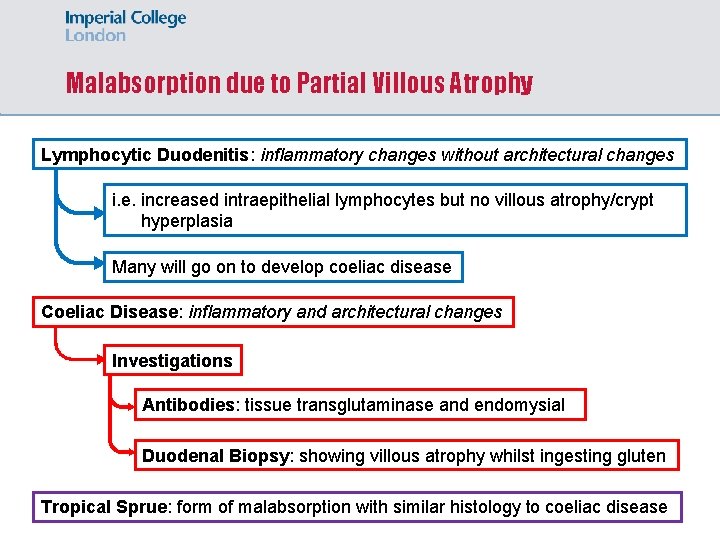
Malabsorption due to Partial Villous Atrophy Lymphocytic Duodenitis: inflammatory changes without architectural changes i. e. increased intraepithelial lymphocytes but no villous atrophy/crypt hyperplasia Many will go on to develop coeliac disease Coeliac Disease: inflammatory and architectural changes Investigations Antibodies: tissue transglutaminase and endomysial Duodenal Biopsy: showing villous atrophy whilst ingesting gluten Tropical Sprue: form of malabsorption with similar histology to coeliac disease
Lower GI Pathology Px: constipation, abdo distension, vomiting Congenital • Hirschsprung Disease absence of myenteric plexus ganglion cells Ix: full thickness rectal biopsy Rx: resection of affected section (anorectal pullthrough) Diverticular Disease Colitis Acute Infection, drugs, chemo/radio Pseudomembranous Chronic Crohn’s, UC and TB • • • Outpouchings Low-fibre diet Complications: pain, diverticulitis, bleeding
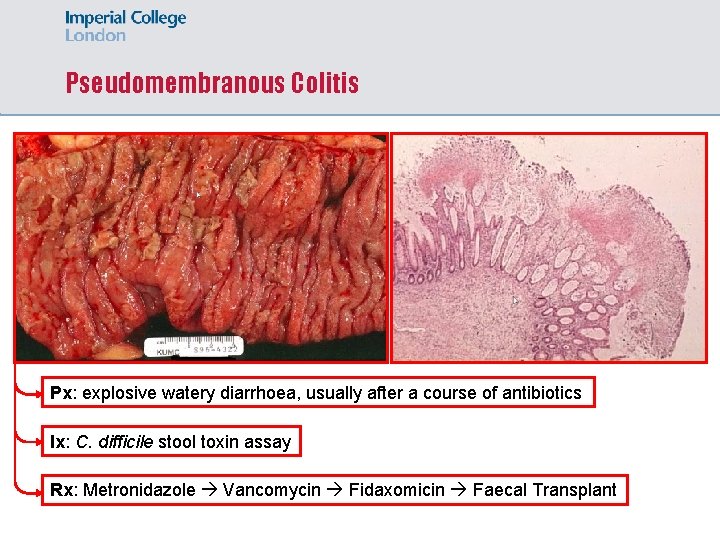
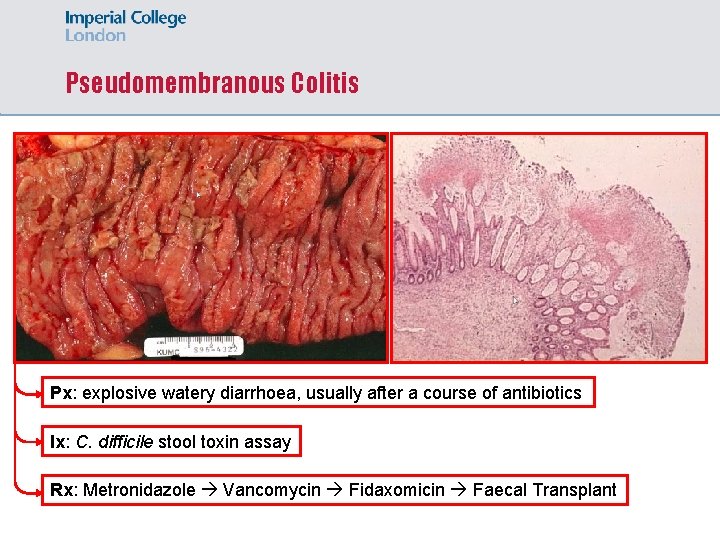
Pseudomembranous Colitis Px: explosive watery diarrhoea, usually after a course of antibiotics Ix: C. difficile stool toxin assay Rx: Metronidazole Vancomycin Fidaxomicin Faecal Transplant
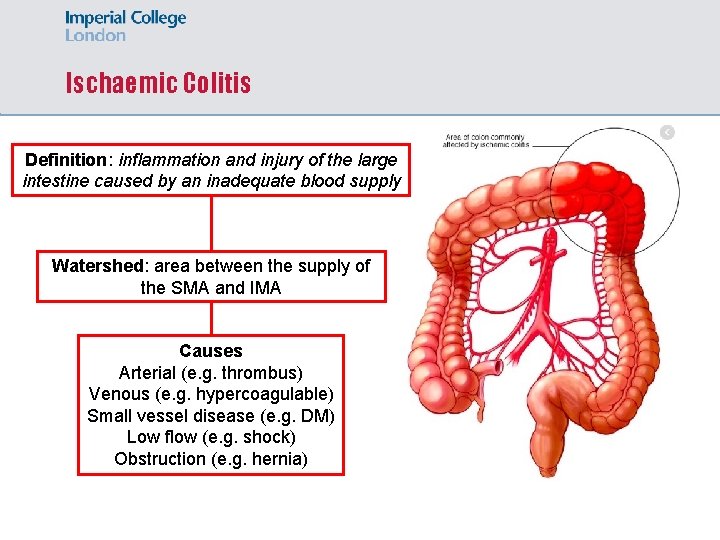
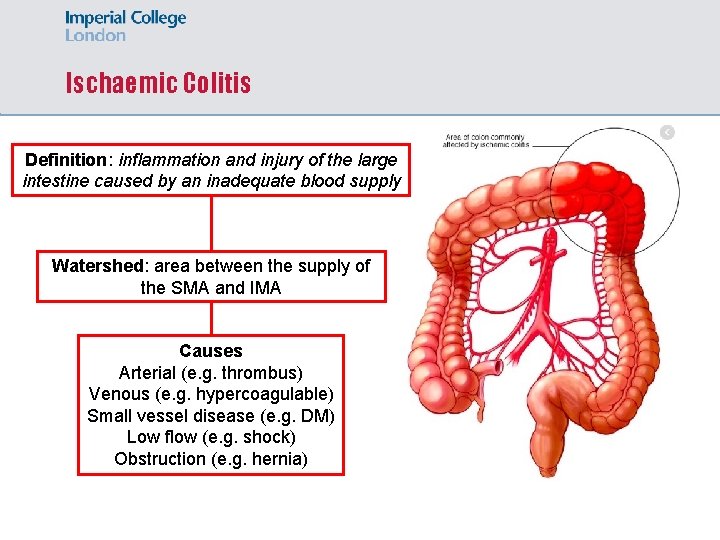
Ischaemic Colitis Definition: inflammation and injury of the large intestine caused by an inadequate blood supply Watershed: area between the supply of the SMA and IMA Causes Arterial (e. g. thrombus) Venous (e. g. hypercoagulable) Small vessel disease (e. g. DM) Low flow (e. g. shock) Obstruction (e. g. hernia)
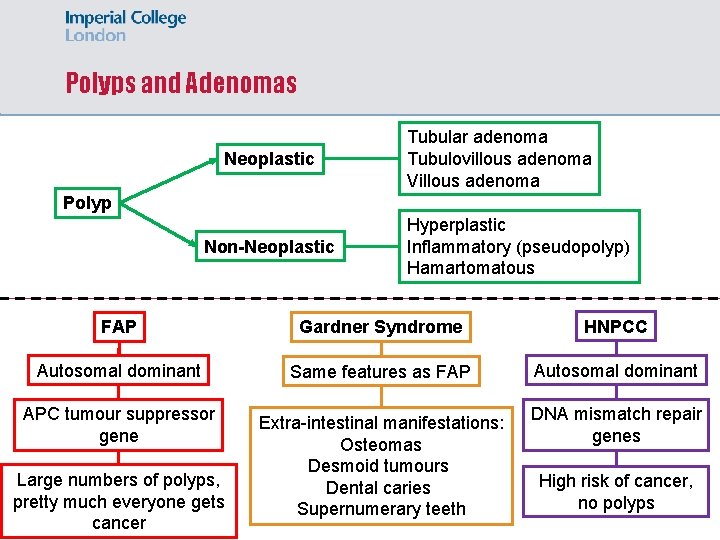
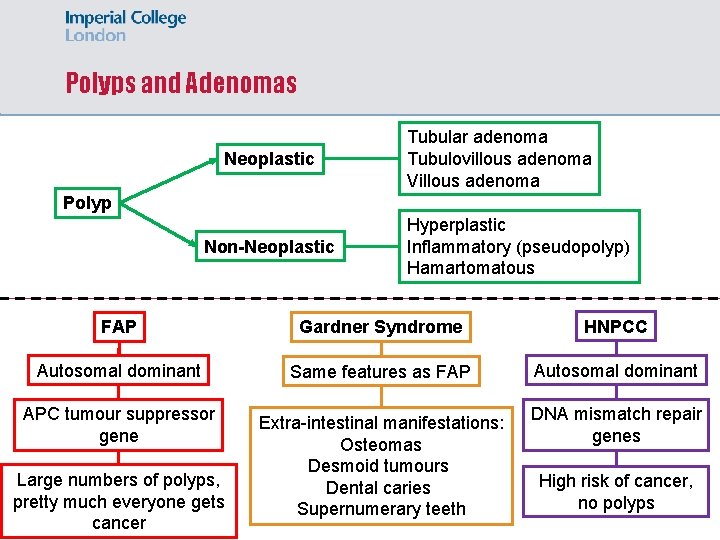
Polyps and Adenomas Neoplastic Tubular adenoma Tubulovillous adenoma Villous adenoma Polyp Non-Neoplastic Hyperplastic Inflammatory (pseudopolyp) Hamartomatous FAP Gardner Syndrome HNPCC Autosomal dominant Same features as FAP Autosomal dominant APC tumour suppressor gene Extra-intestinal manifestations: Osteomas Desmoid tumours Dental caries Supernumerary teeth DNA mismatch repair genes Large numbers of polyps, pretty much everyone gets cancer High risk of cancer, no polyps
Answer 1 A 45 -year-old man presents to his GP with a 3 -month history of worsening dysphagia. He is now unable to comfortably swallow solid foods. He has never suffered from heartburn and takes no regular medications. He has a 20 pack year smoking history and drinks in moderation. A barium swallow identifies an apple core lesion in the middle third of the oesophagus. This is followed by an OGD and biopsy which reveals abnormal keratinised cells with intercellular bridges that have invaded the basement membrane. What is the most likely diagnosis? A Barrett’s oesophagus B Transitional cell carcinoma C Oesophageal lymphoma D Adenocarcinoma E Squamous cell carcinoma
Answer 2 A 16 -year-old girl has suffered from diarrhoea for the past 6 months. She describes the diarrhoea as foul-smelling and has lost 5 kg over this time period. An endoscopy and biopsy reveals increased intraepithelial lymphocytes with a 2: 1 villous to crypt ratio. What is the most likely diagnosis? A Lymphocytic duodenitis B Coeliac disease C Crohn’s disease D Duodenal MALToma E Linitis plastica
Gynaecological Pathology
Question 5 A 36 -year-old woman who was identified as having an abnormal cervical smear, underwent a cervical excision biopsy which reveals cervical glandular intraepithelial neoplasia. Which type of cancer would this have progressed to if left untreated? A Adenocarcinoma B Krukenberg tumour C Squamous cell carcinoma D Transitional cell carcinoma E Serous carcinoma
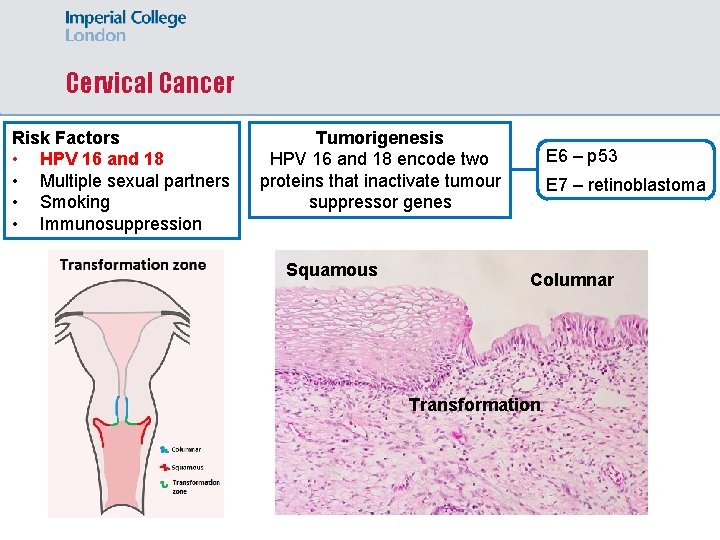
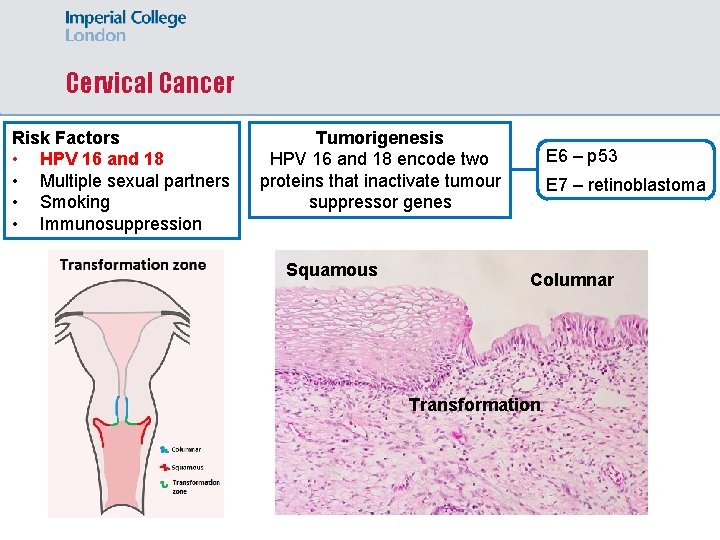
Cervical Cancer Risk Factors • HPV 16 and 18 • Multiple sexual partners • Smoking • Immunosuppression Tumorigenesis HPV 16 and 18 encode two proteins that inactivate tumour suppressor genes Squamous E 6 – p 53 E 7 – retinoblastoma Columnar Transformation
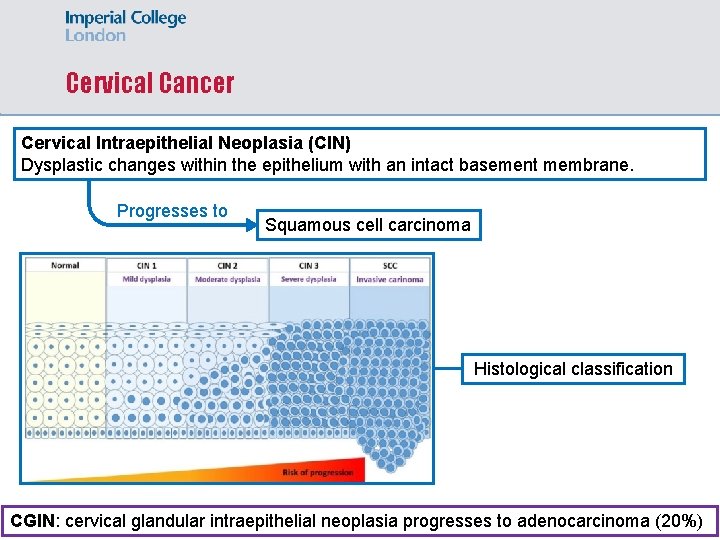
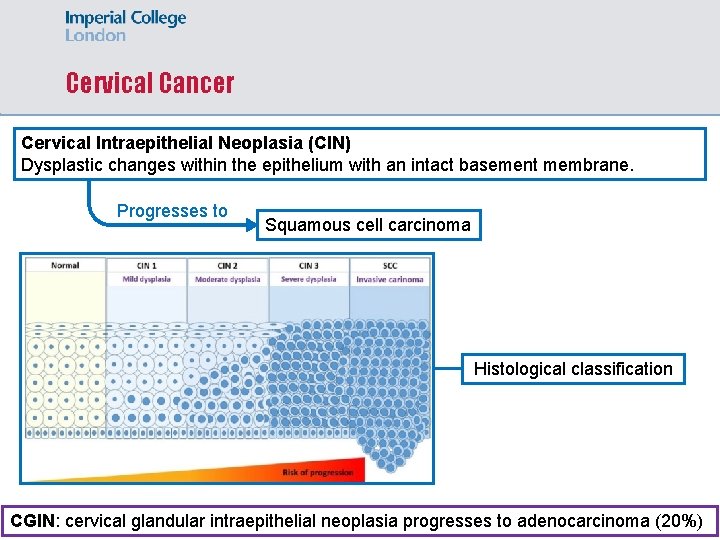
Cervical Cancer Cervical Intraepithelial Neoplasia (CIN) Dysplastic changes within the epithelium with an intact basement membrane. Progresses to Squamous cell carcinoma Histological classification CGIN: cervical glandular intraepithelial neoplasia progresses to adenocarcinoma (20%)
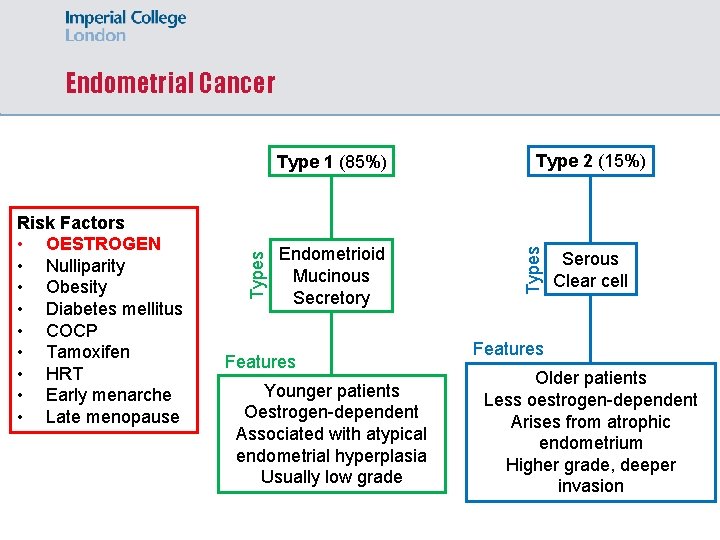
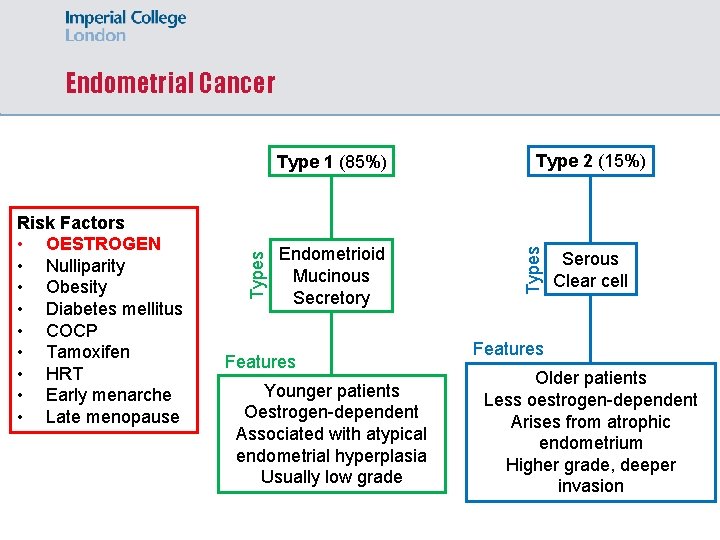
Endometrial Cancer Endometrioid Mucinous Secretory Features Younger patients Oestrogen-dependent Associated with atypical endometrial hyperplasia Usually low grade Type 2 (15%) Types Risk Factors • OESTROGEN • Nulliparity • Obesity • Diabetes mellitus • COCP • Tamoxifen • HRT • Early menarche • Late menopause Types Type 1 (85%) Serous Clear cell Features Older patients Less oestrogen-dependent Arises from atrophic endometrium Higher grade, deeper invasion
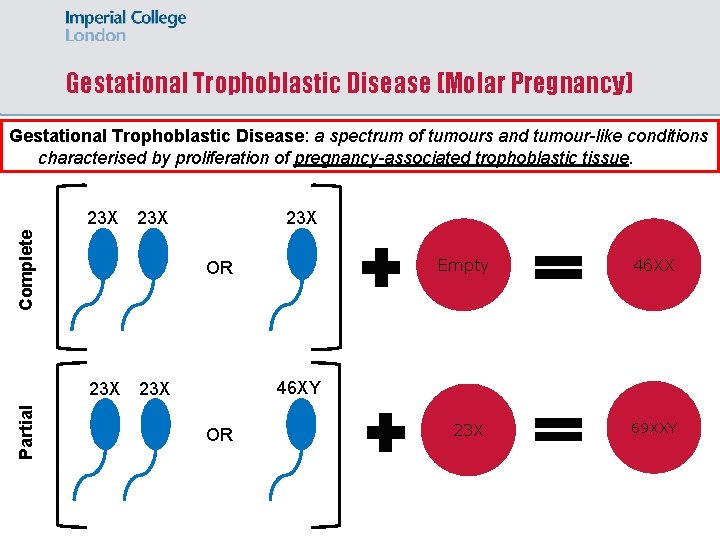
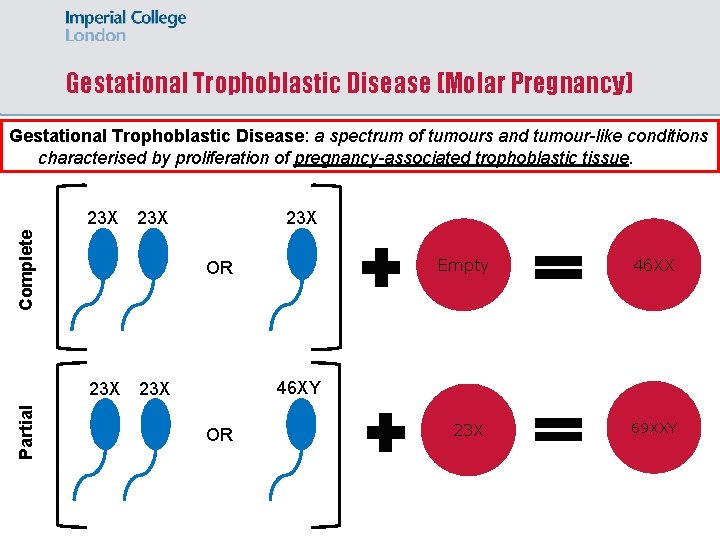
Gestational Trophoblastic Disease (Molar Pregnancy) Gestational Trophoblastic Disease: a spectrum of tumours and tumour-like conditions characterised by proliferation of pregnancy-associated trophoblastic tissue. 23 X Complete 23 X Empty OR 23 X Partial 23 X 46 XY 23 X OR 23 X 69 XXY
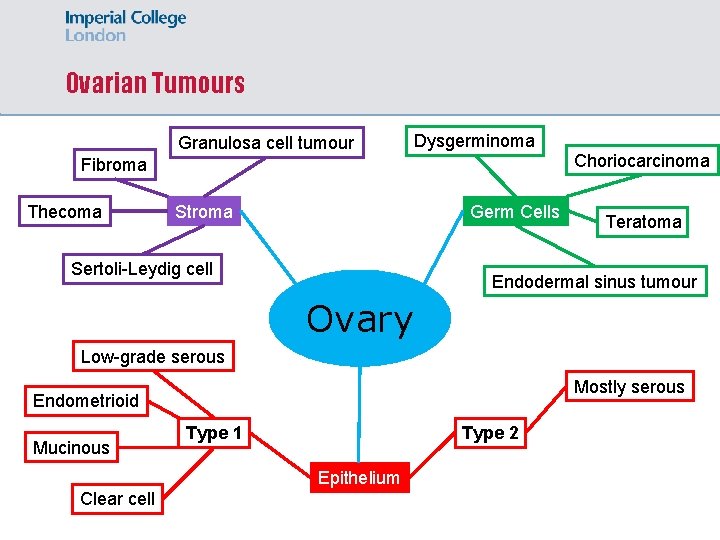
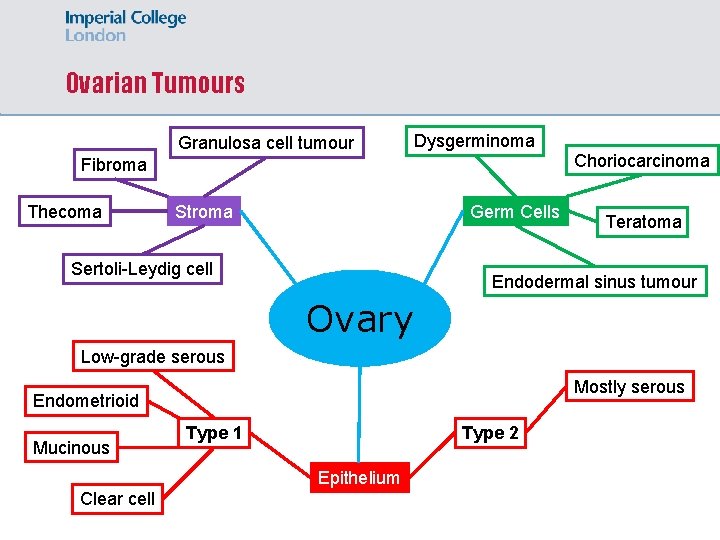
Ovarian Tumours Granulosa cell tumour Dysgerminoma Fibroma Thecoma Germ Cells Stroma Sertoli-Leydig cell Choriocarcinoma Teratoma Endodermal sinus tumour Ovary Low-grade serous Mostly serous Endometrioid Mucinous Type 1 Type 2 Epithelium Clear cell
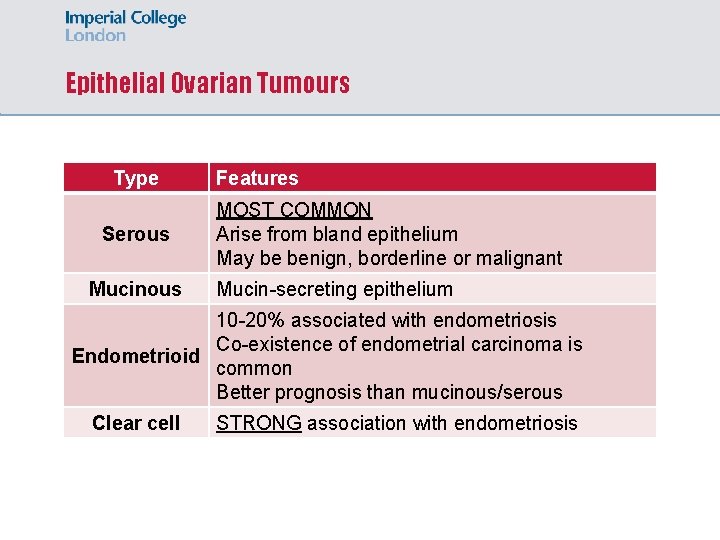
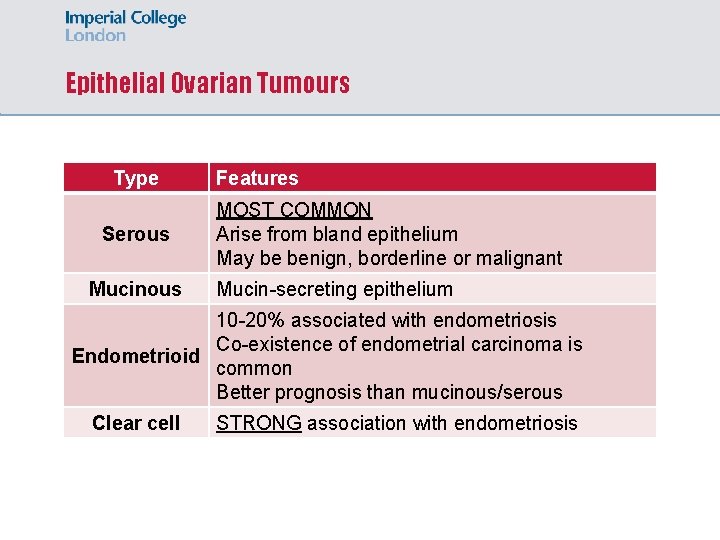
Epithelial Ovarian Tumours Type Serous Mucinous Features MOST COMMON Arise from bland epithelium May be benign, borderline or malignant Mucin-secreting epithelium 10 -20% associated with endometriosis Co-existence of endometrial carcinoma is Endometrioid common Better prognosis than mucinous/serous Clear cell STRONG association with endometriosis
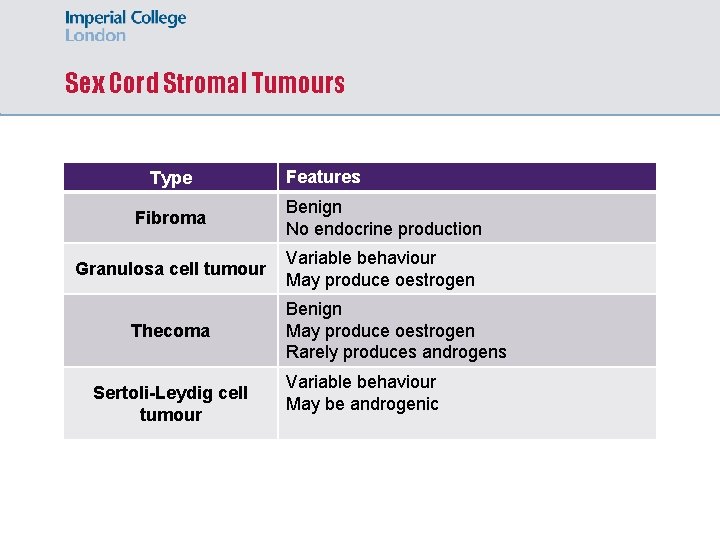
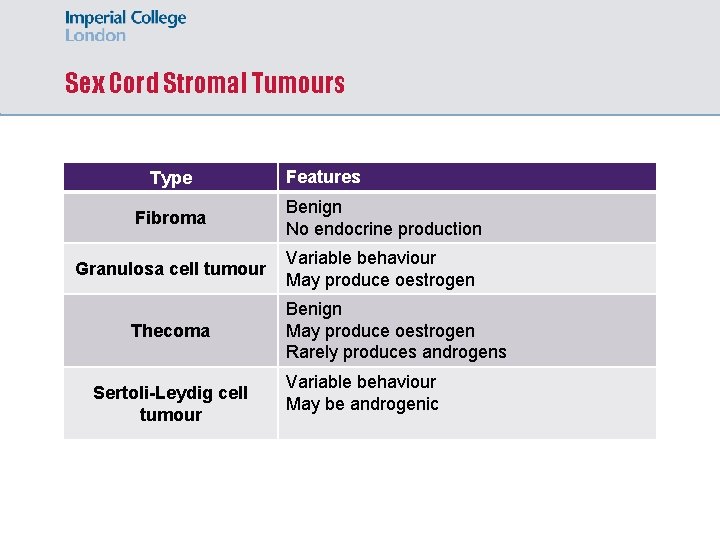
Sex Cord Stromal Tumours Type Features Fibroma Benign No endocrine production Granulosa cell tumour Variable behaviour May produce oestrogen Thecoma Sertoli-Leydig cell tumour Benign May produce oestrogen Rarely produces androgens Variable behaviour May be androgenic
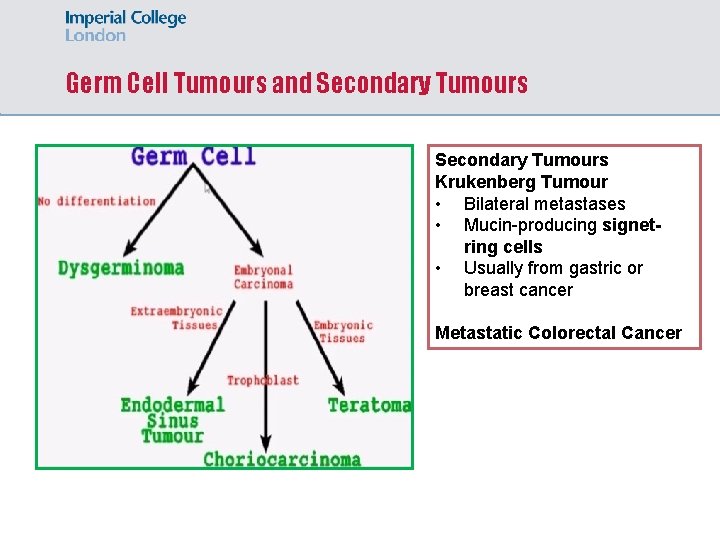
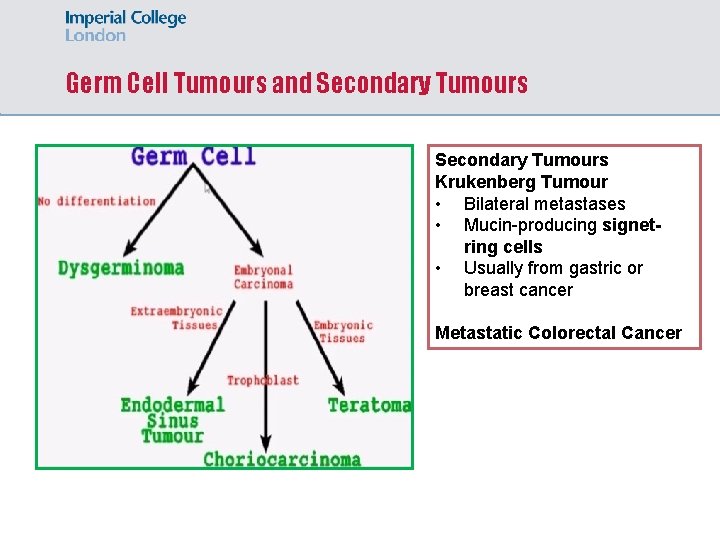
Germ Cell Tumours and Secondary Tumours Krukenberg Tumour • Bilateral metastases • Mucin-producing signetring cells • Usually from gastric or breast cancer Metastatic Colorectal Cancer
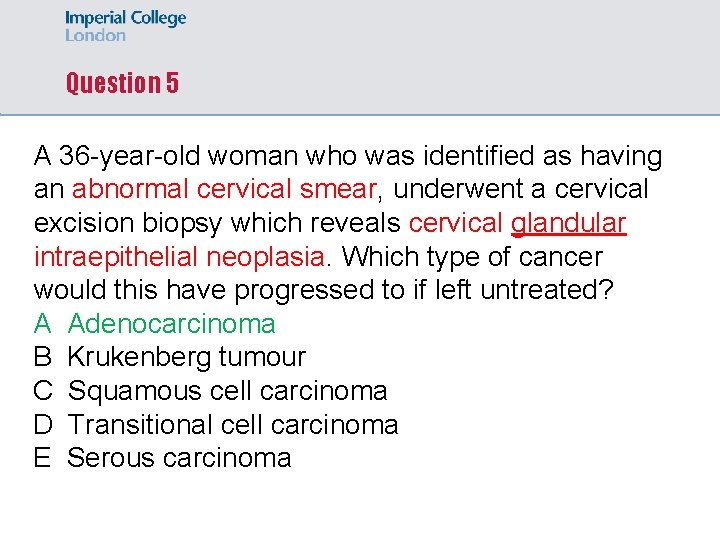
Question 5 A 36 -year-old woman who was identified as having an abnormal cervical smear, underwent a cervical excision biopsy which reveals cervical glandular intraepithelial neoplasia. Which type of cancer would this have progressed to if left untreated? A Adenocarcinoma B Krukenberg tumour C Squamous cell carcinoma D Transitional cell carcinoma E Serous carcinoma
Skin Pathology
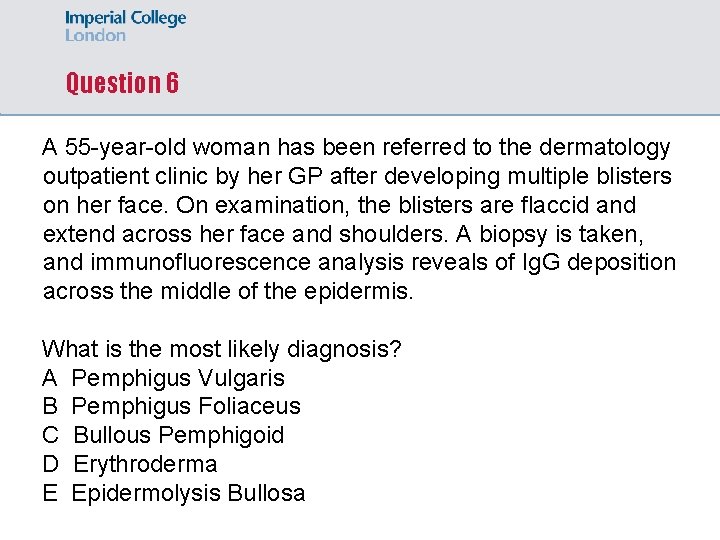
Question 6 A 55 -year-old woman has been referred to the dermatology outpatient clinic by her GP after developing multiple blisters on her face. On examination, the blisters are flaccid and extend across her face and shoulders. A biopsy is taken, and immunofluorescence analysis reveals of Ig. G deposition across the middle of the epidermis. What is the most likely diagnosis? A Pemphigus Vulgaris B Pemphigus Foliaceus C Bullous Pemphigoid D Erythroderma E Epidermolysis Bullosa
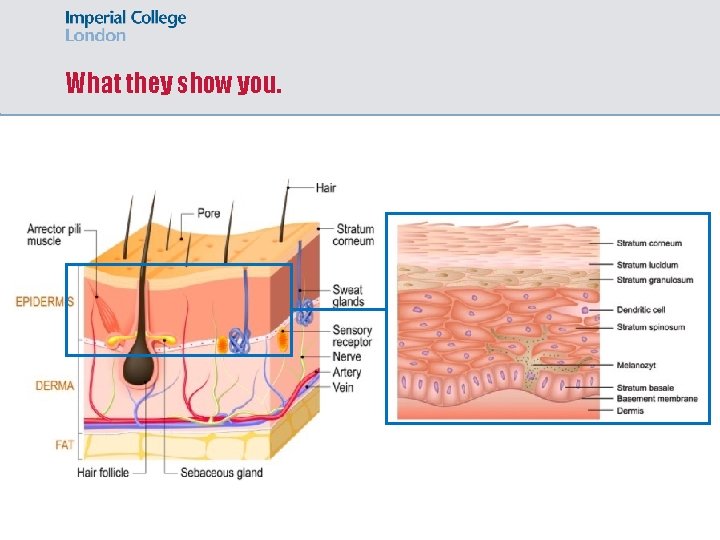
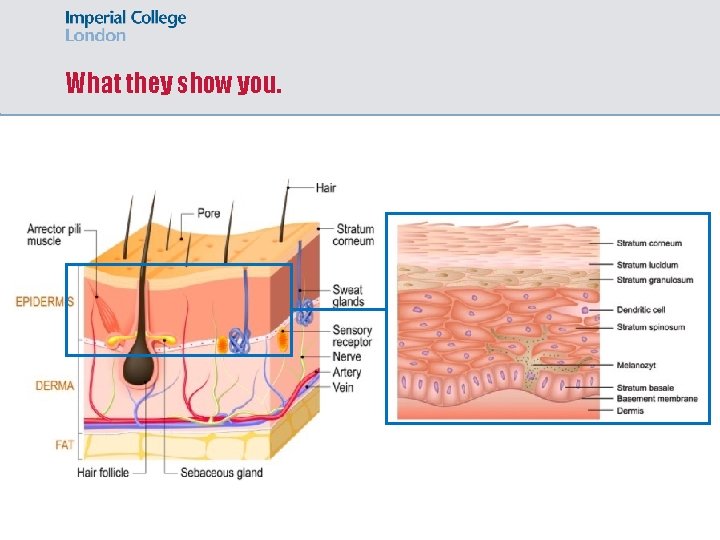
What they show you.
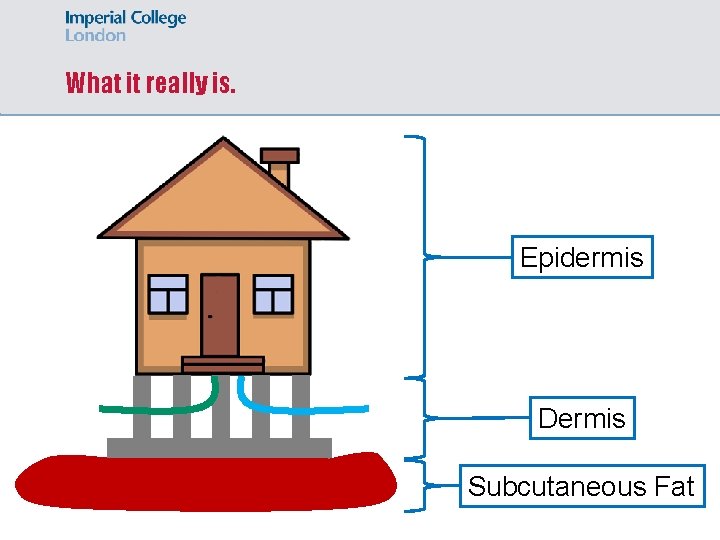
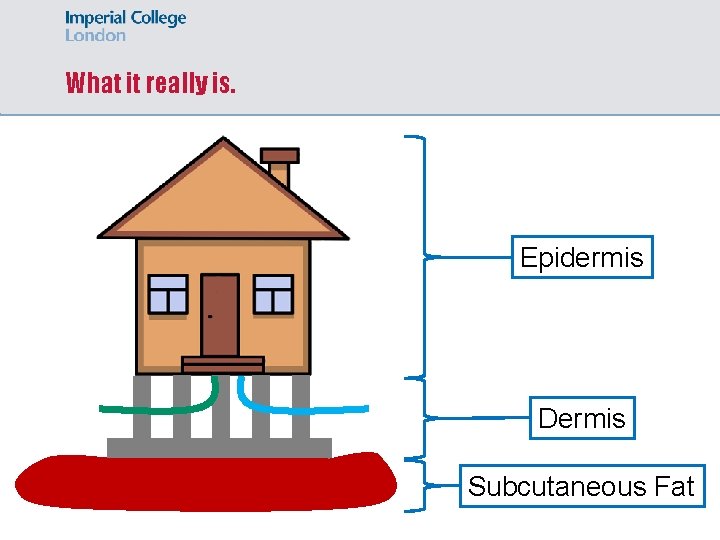
What it really is. Epidermis Dermis Subcutaneous Fat
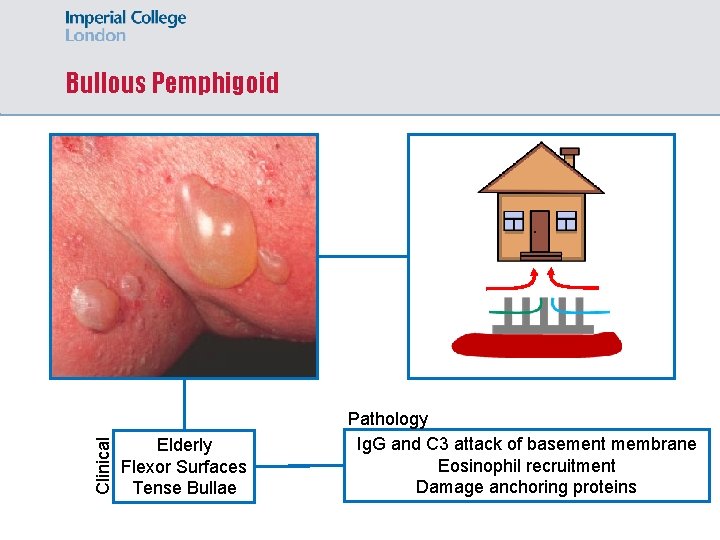
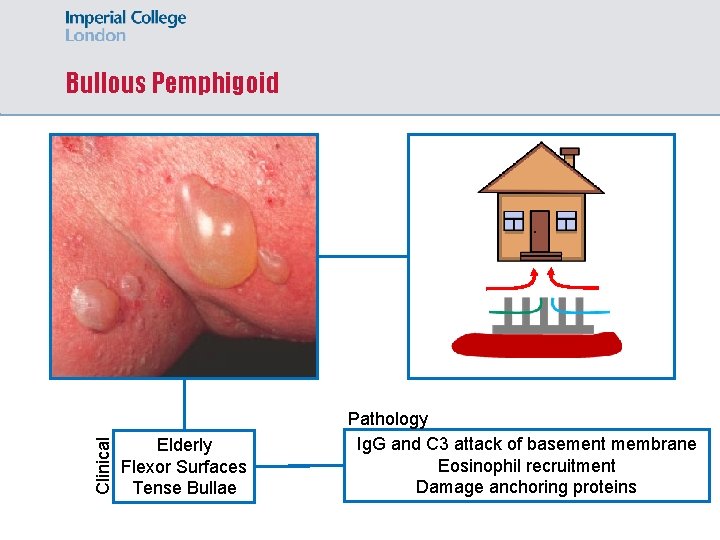
Clinical Bullous Pemphigoid Elderly Flexor Surfaces Tense Bullae Pathology Ig. G and C 3 attack of basement membrane Eosinophil recruitment Damage anchoring proteins
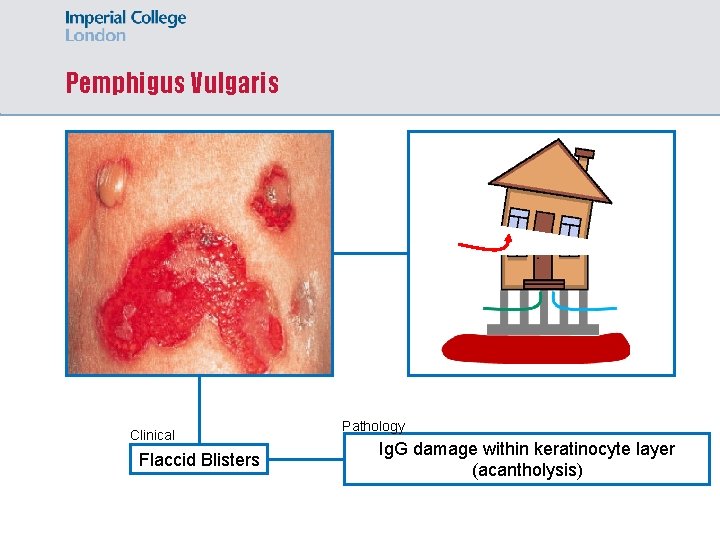
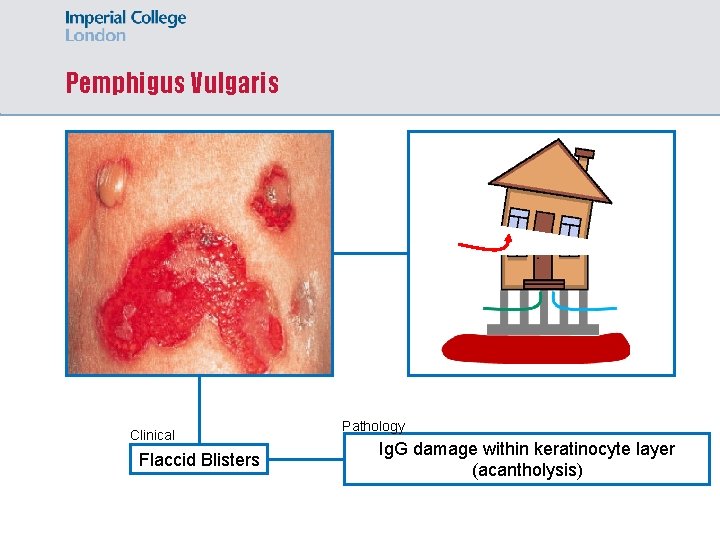
Pemphigus Vulgaris Clinical Flaccid Blisters Pathology Ig. G damage within keratinocyte layer (acantholysis)
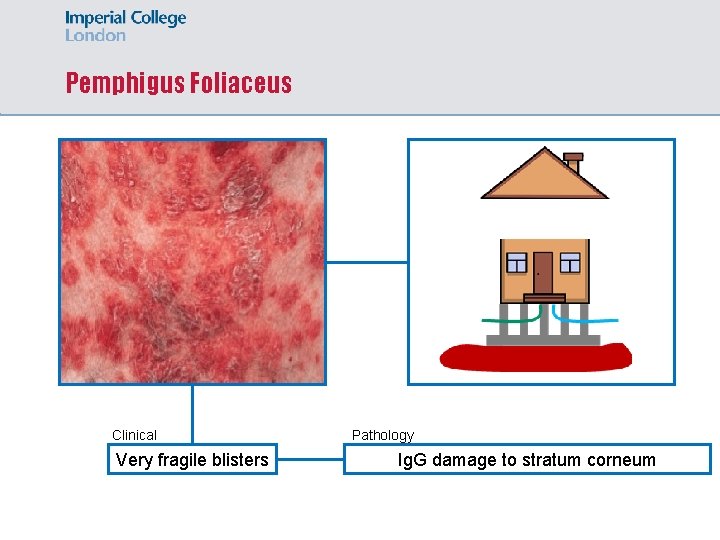
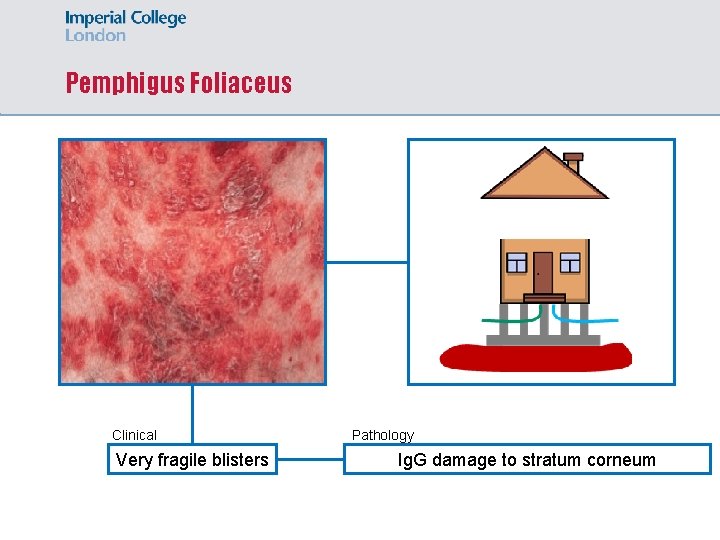
Pemphigus Foliaceus Clinical Very fragile blisters Pathology Ig. G damage to stratum corneum
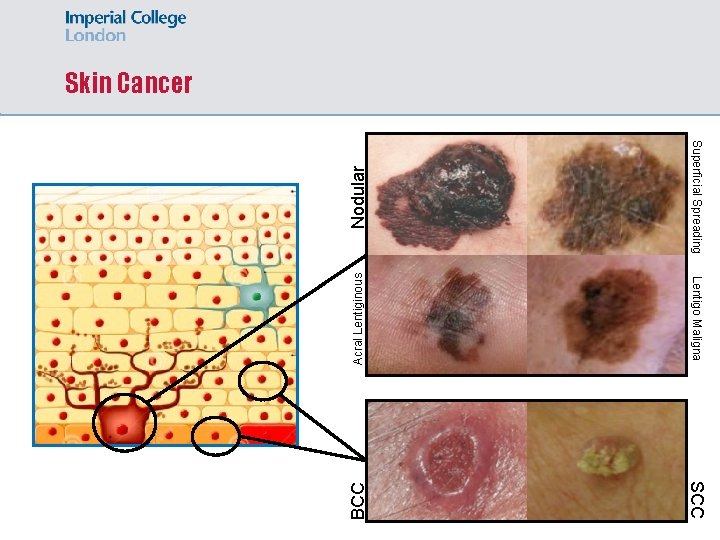
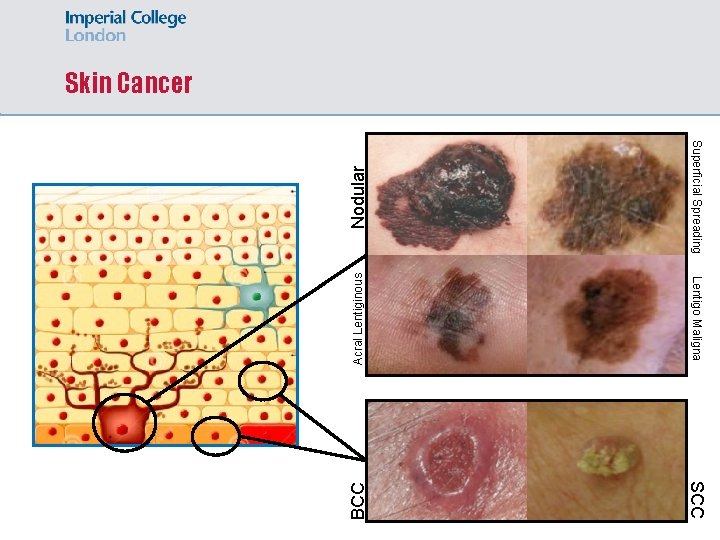
Nodular Superficial Spreading Acral Lentiginous Lentigo Maligna BCC Skin Cancer SCC
Answer 6 A 55 -year-old woman has been referred to the dermatology outpatient clinic by her GP after developing multiple blisters on her face. On examination, the blisters are flaccid and extend across her face and shoulders. A biopsy is taken, and immunofluorescence analysis reveals of Ig. G deposition across the middle of the epidermis. What is the most likely diagnosis? A Pemphigus Vulgaris B Pemphigus Foliaceus C Bullous Pemphigoid D Erythroderma E Epidermolysis Bullosa
Thank You! Questions? Email: lpr 114@ic. ac. uk Feedback:
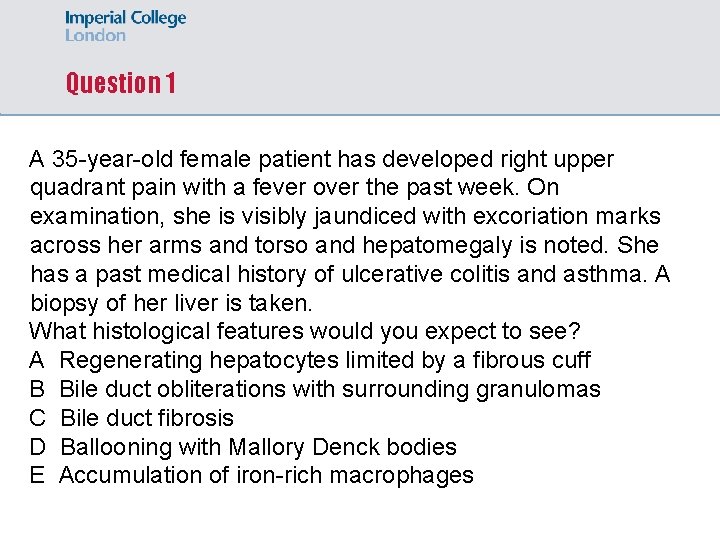
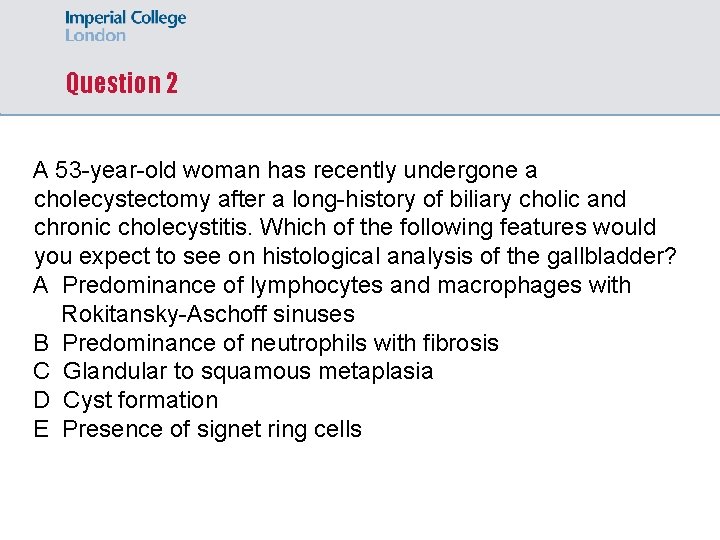
Question 1 A 35 -year-old female patient has developed right upper quadrant pain with a fever over the past week. On examination, she is visibly jaundiced with excoriation marks across her arms and torso and hepatomegaly is noted. She has a past medical history of ulcerative colitis and asthma. A biopsy of her liver is taken. What histological features would you expect to see? A Regenerating hepatocytes limited by a fibrous cuff B Bile duct obliterations with surrounding granulomas C Bile duct fibrosis D Ballooning with Mallory Denck bodies E Accumulation of iron-rich macrophages
Answer 1 A 35 -year-old female patient has developed right upper quadrant pain with a fever over the past week. On examination, she is visibly jaundiced with excoriation marks across her arms and torso and hepatomegaly is noted. She has a past medical history of ulcerative colitis and asthma. A biopsy of her liver is taken. What histological features would you expect to see? A Regenerating hepatocytes limited by a fibrous cuff B Bile duct obliterations with surrounding granulomas C Bile duct fibrosis D Ballooning with Mallory Denck bodies E Accumulation of iron-rich macrophages
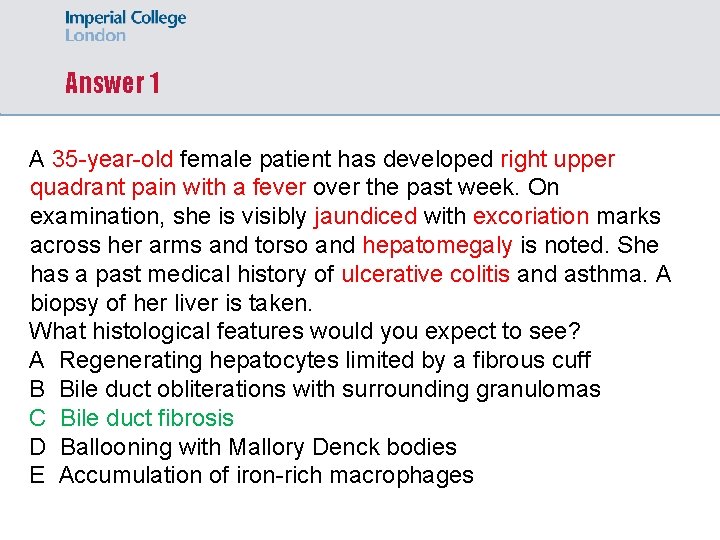
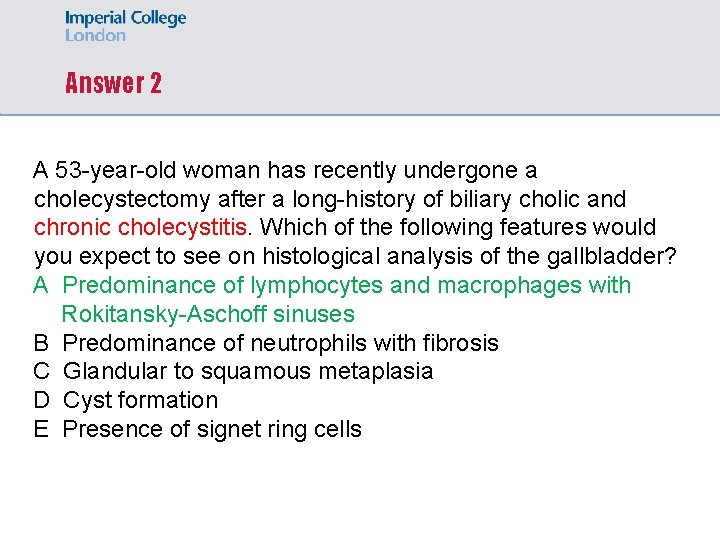
Question 2 A 53 -year-old woman has recently undergone a cholecystectomy after a long-history of biliary cholic and chronic cholecystitis. Which of the following features would you expect to see on histological analysis of the gallbladder? A Predominance of lymphocytes and macrophages with Rokitansky-Aschoff sinuses B Predominance of neutrophils with fibrosis C Glandular to squamous metaplasia D Cyst formation E Presence of signet ring cells
Answer 2 A 53 -year-old woman has recently undergone a cholecystectomy after a long-history of biliary cholic and chronic cholecystitis. Which of the following features would you expect to see on histological analysis of the gallbladder? A Predominance of lymphocytes and macrophages with Rokitansky-Aschoff sinuses B Predominance of neutrophils with fibrosis C Glandular to squamous metaplasia D Cyst formation E Presence of signet ring cells
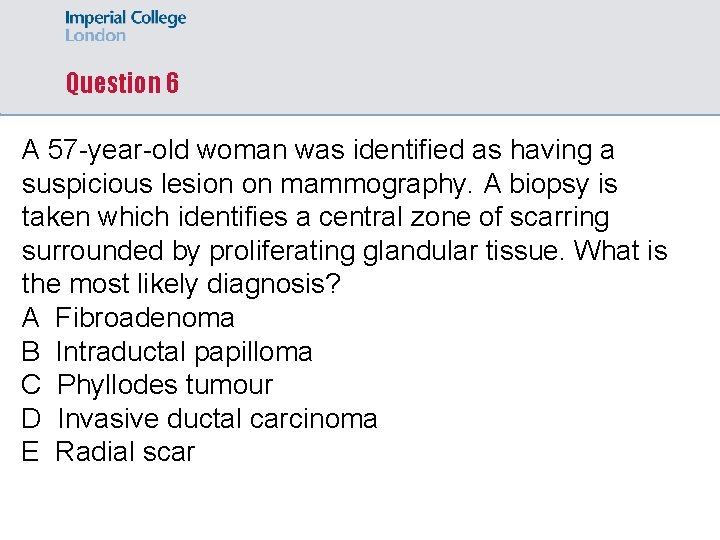
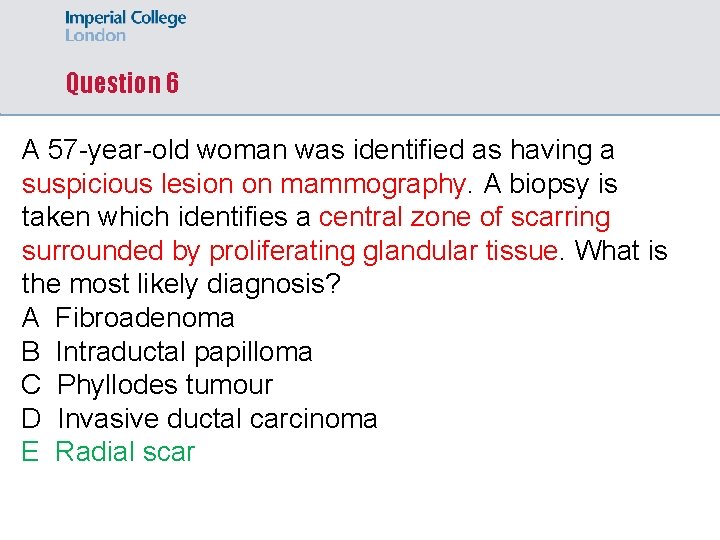
Question 6 A 57 -year-old woman was identified as having a suspicious lesion on mammography. A biopsy is taken which identifies a central zone of scarring surrounded by proliferating glandular tissue. What is the most likely diagnosis? A Fibroadenoma B Intraductal papilloma C Phyllodes tumour D Invasive ductal carcinoma E Radial scar
Question 6 A 57 -year-old woman was identified as having a suspicious lesion on mammography. A biopsy is taken which identifies a central zone of scarring surrounded by proliferating glandular tissue. What is the most likely diagnosis? A Fibroadenoma B Intraductal papilloma C Phyllodes tumour D Invasive ductal carcinoma E Radial scar
 Laz parking kansas city
Laz parking kansas city Annual worth analysis example
Annual worth analysis example Anything worth doing is not necessarily worth doing well
Anything worth doing is not necessarily worth doing well Present worth and annual worth
Present worth and annual worth Acetone fixative
Acetone fixative Tissue processing
Tissue processing Zones of dentinal caries
Zones of dentinal caries Histopathology is a subdiscipline of microscopic anatomy.
Histopathology is a subdiscipline of microscopic anatomy. Fewfew
Fewfew Is a very shallow skillet with very short sloping sides
Is a very shallow skillet with very short sloping sides Figure 10
Figure 10 Quantifiers food exercises
Quantifiers food exercises Multiplication of scientific notation
Multiplication of scientific notation 1 important lesson that is worth sharing about this lesson
1 important lesson that is worth sharing about this lesson Very important words
Very important words Radio telex stations
Radio telex stations School is very important
School is very important Very important place
Very important place Communication plays a very important role in
Communication plays a very important role in Hi im dog
Hi im dog Smile is very important
Smile is very important In cement hardening process instants are very important
In cement hardening process instants are very important Write about your dream school
Write about your dream school Newspaper article format
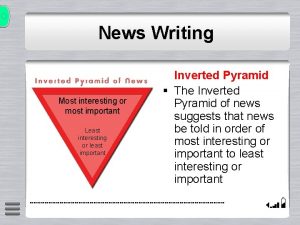
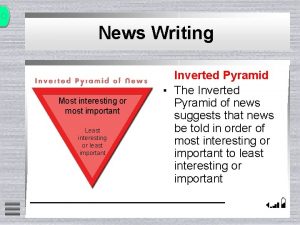
Newspaper article format Inverted pyramid in news writing
Inverted pyramid in news writing Least important to most important
Least important to most important Placet ex officio
Placet ex officio A centipede was happy quite
A centipede was happy quite He has short
He has short Cephalocaudal growth
Cephalocaudal growth You need a passport to cross the
You need a passport to cross the Who is the chief guest at macbeth's celebration feast
Who is the chief guest at macbeth's celebration feast The story was quite interesting
The story was quite interesting Scc bu
Scc bu Sarah rarely misses her basketball shots
Sarah rarely misses her basketball shots Which of the seven deadly sins does mrs birling embody
Which of the seven deadly sins does mrs birling embody Alone is something you'll be quite a lot
Alone is something you'll be quite a lot Desforrada
Desforrada An inspector calls opening stage directions
An inspector calls opening stage directions I can hear you quite well. you not shout
I can hear you quite well. you not shout Use excessive force if things don't quite slip into place
Use excessive force if things don't quite slip into place I wonder by jeannie kirby
I wonder by jeannie kirby Spend quite a bit of time
Spend quite a bit of time Mr conrad's son is becoming quite well known as an artist
Mr conrad's son is becoming quite well known as an artist Mc hammer investments
Mc hammer investments Mike mazzalongo net worth
Mike mazzalongo net worth Franzj net worth
Franzj net worth Els worth bunker
Els worth bunker Capricorn private investments
Capricorn private investments What can be inferred from the graph?
What can be inferred from the graph?