Health system components to support UHC Thai experience

- Slides: 31
Health system components to support UHC: Thai experience on pre-requisites for UHC Phusit Prakongsai, M. D. Ph. D. International Health Policy Program (IHPP) Ministry of Public Health, Thailand Presentation to the Exchange and Study Program on UHC Monitoring and Evaluation VIC 3 Bangkok Hotel 9 September 2013
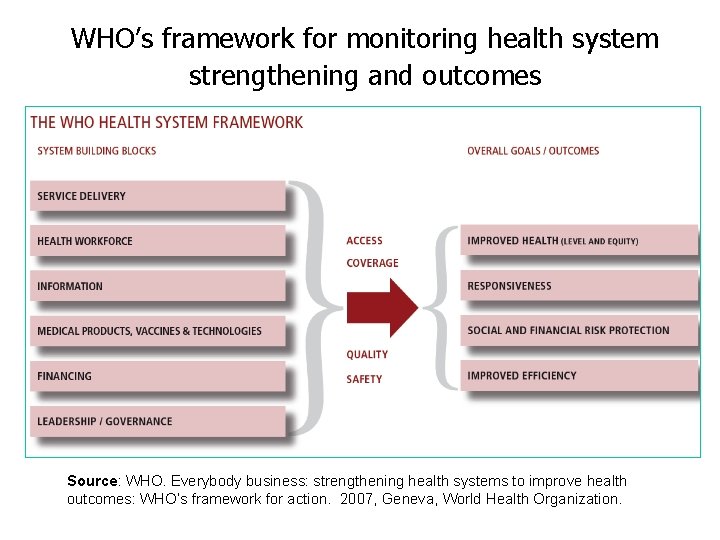
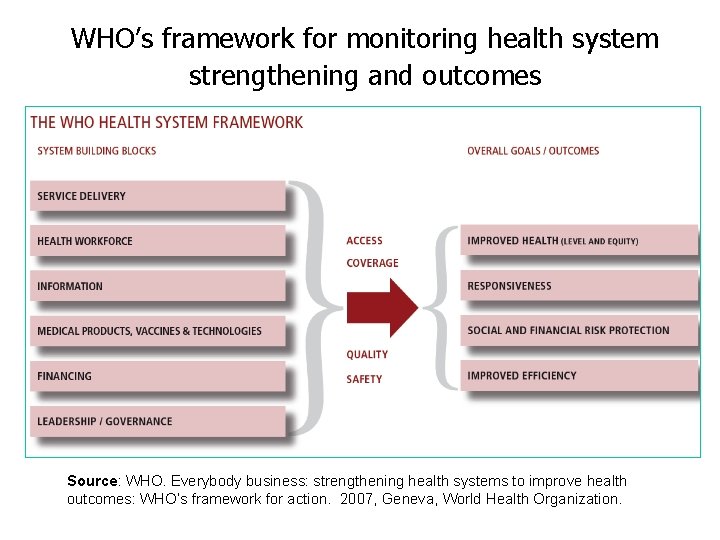
WHO’s framework for monitoring health system strengthening and outcomes Source: WHO. Everybody business: strengthening health systems to improve health outcomes: WHO’s framework for action. 2007, Geneva, World Health Organization.
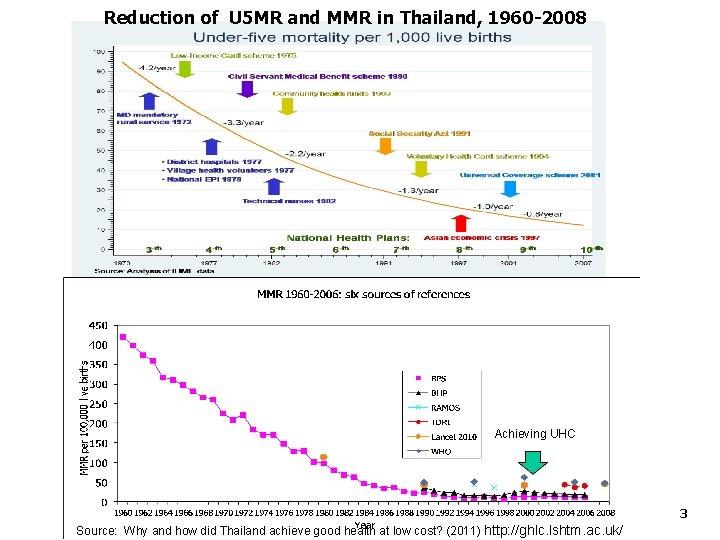
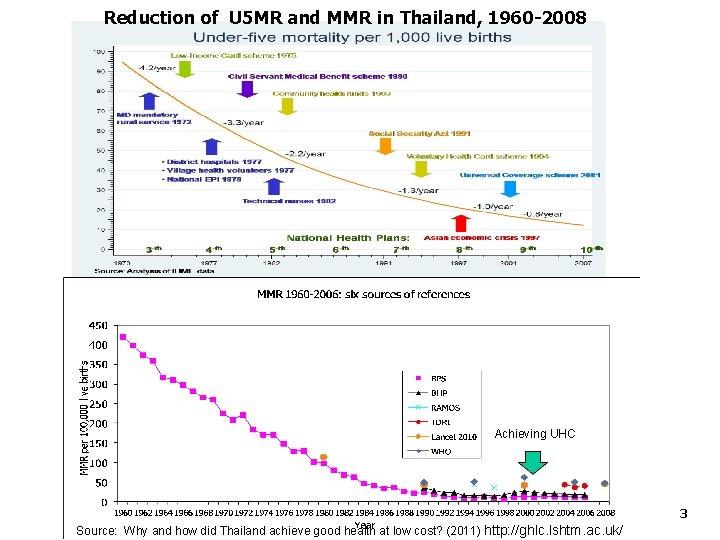
Reduction of U 5 MR and MMR in Thailand, 1960 -2008 Achieving UHC 3 Source: Why and how did Thailand achieve good health at low cost? (2011) http: //ghlc. lshtm. ac. uk/
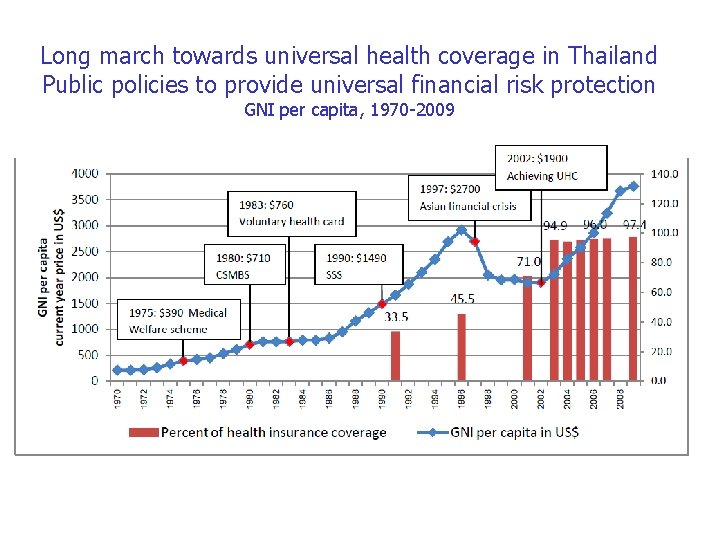
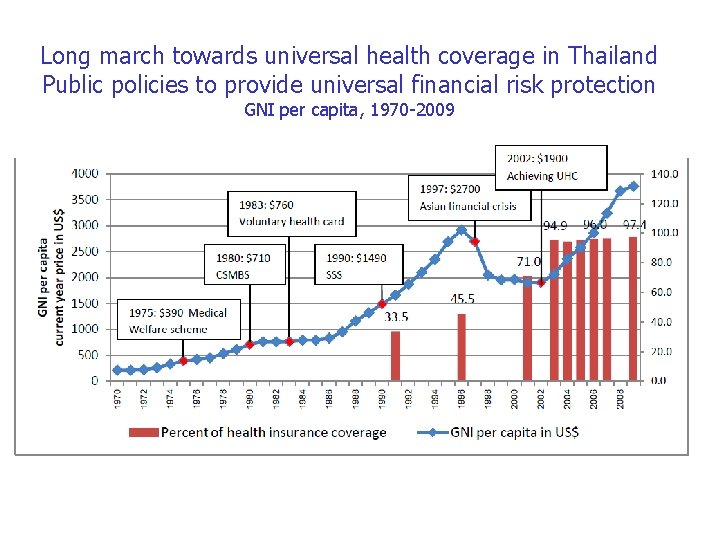
Long march towards universal health coverage in Thailand Public policies to provide universal financial risk protection GNI per capita, 1970 -2009
UHC policy objectives • Improving health of all Thais by providing equitable access to quality health services in accordance with health need of the population, • Preventing Thai households from being financially catastrophic when facing with high cost care, 5
Health care financing strategies of the UHC policy • Removal of financial barriers to health services; • Risk sharing expand the UHC scheme to cover uninsured and merge LIC and voluntary health card scheme, • Shift of the main source of HCF from OOPs to general tax; • Sustainable systems: – Policy sustainability Law – Financial sustainability – Institutional sustainability • Participatory process • Protect people right 6
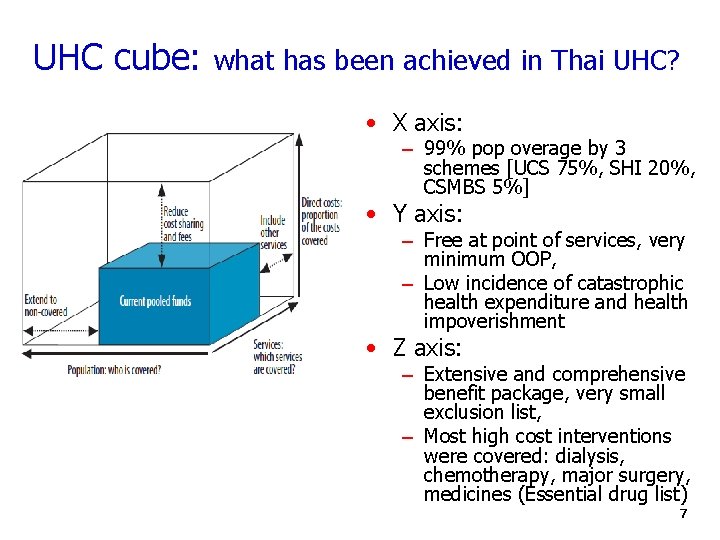
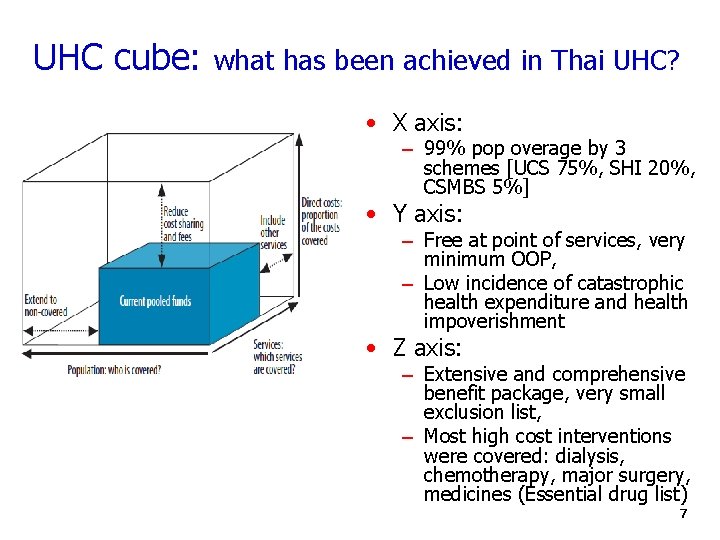
UHC cube: what has been achieved in Thai UHC? • X axis: – 99% pop overage by 3 schemes [UCS 75%, SHI 20%, CSMBS 5%] • Y axis: – Free at point of services, very minimum OOP, – Low incidence of catastrophic health expenditure and health impoverishment • Z axis: – Extensive and comprehensive benefit package, very small exclusion list, – Most high cost interventions were covered: dialysis, chemotherapy, major surgery, medicines (Essential drug list) 7
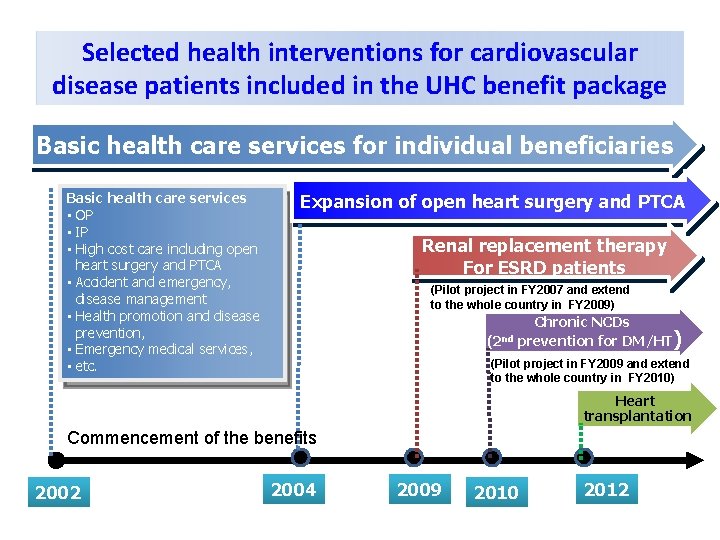
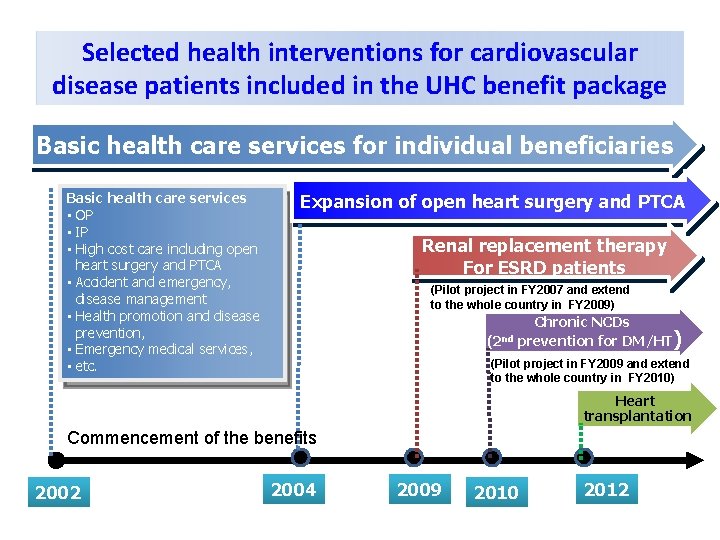
Selected health interventions for cardiovascular disease patients included in the UHC benefit package Basic health care services for individual beneficiaries Basic health care services • OP • IP • High cost care including open heart surgery and PTCA • Accident and emergency, disease management • Health promotion and disease prevention, • Emergency medical services, • etc. Expansion of open heart surgery and PTCA Renal replacement therapy For ESRD patients (Pilot project in FY 2007 and extend to the whole country in FY 2009) Chronic NCDs (2 nd prevention for DM/HT) (Pilot project in FY 2009 and extend to the whole country in FY 2010) Heart transplantation Commencement of the benefits 2002 2004 2009 2010 2012
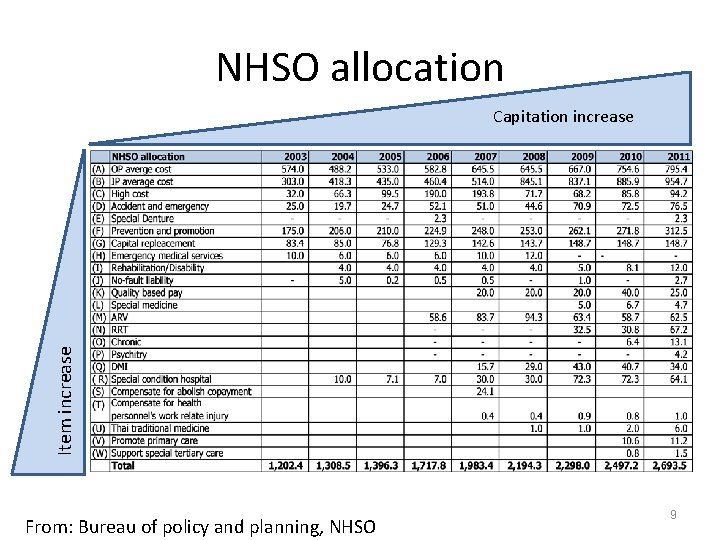
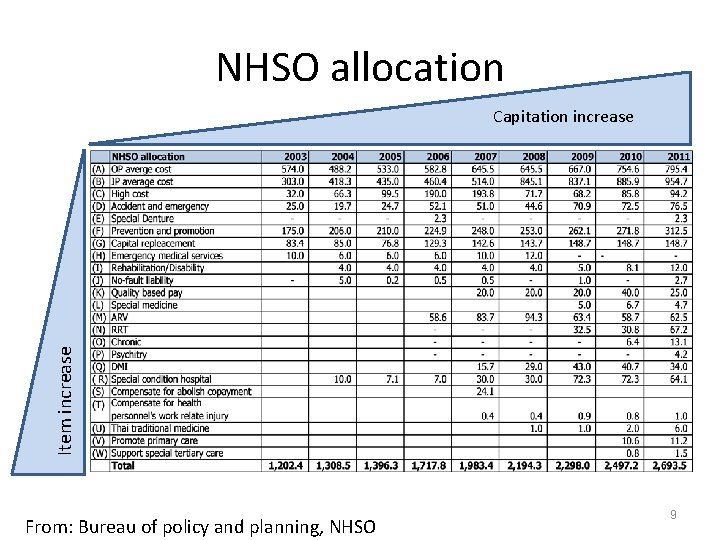
NHSO allocation Item increase Capitation increase From: Bureau of policy and planning, NHSO 9
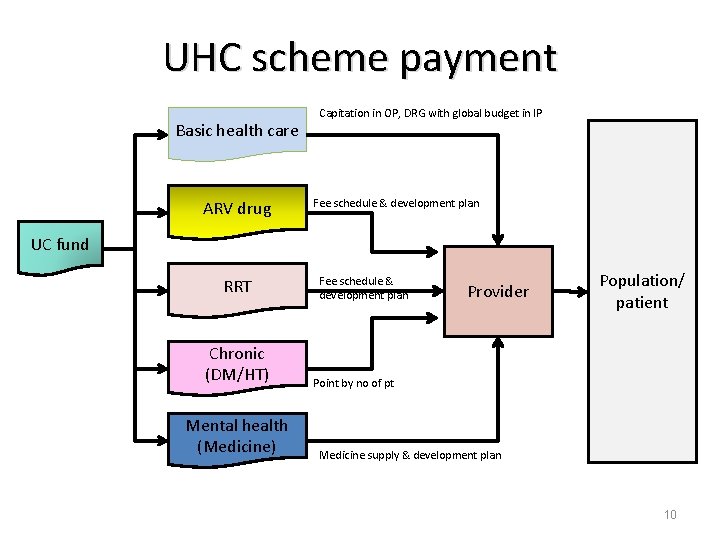
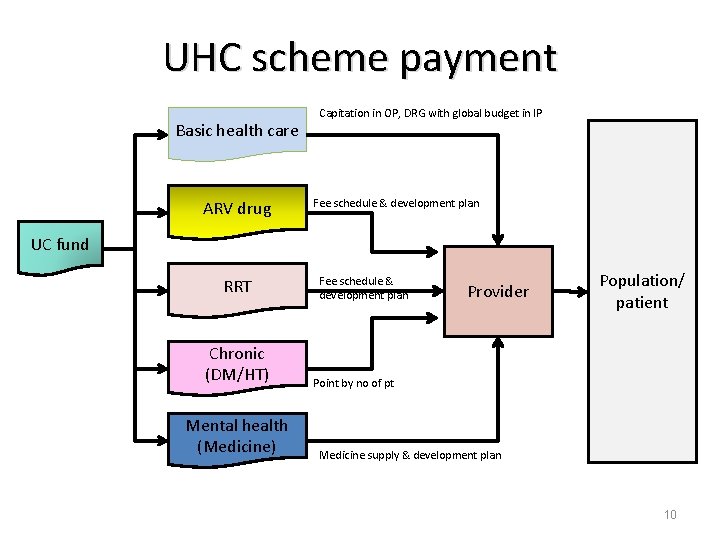
UHC scheme payment Basic health care ARV drug Capitation in OP, DRG with global budget in IP Fee schedule & development plan UC fund RRT Chronic (DM/HT) Mental health (Medicine) Fee schedule & development plan Provider Population/ patient Point by no of pt Medicine supply & development plan 10
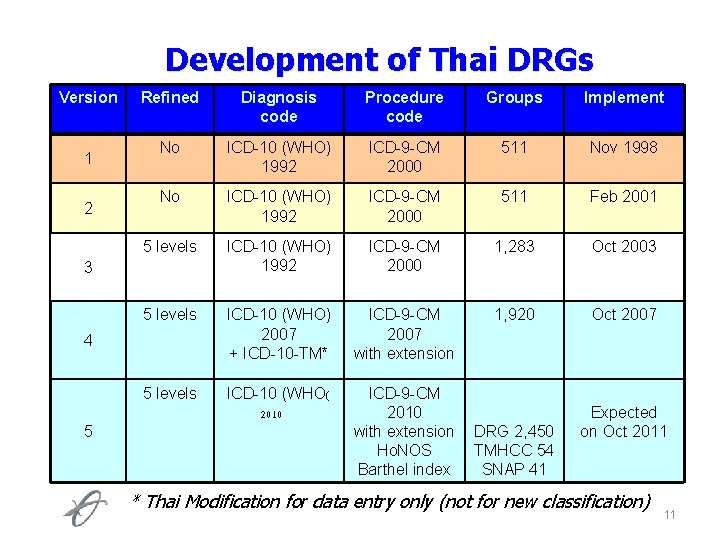
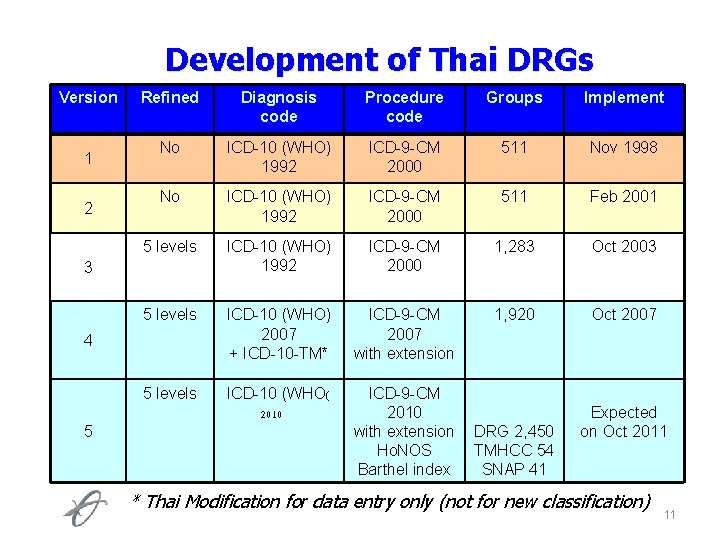
Development of Thai DRGs Version 1 2 Refined Diagnosis code Procedure code Groups Implement No ICD-10 (WHO) 1992 ICD-9 -CM 2000 511 Nov 1998 No ICD-10 (WHO) 1992 ICD-9 -CM 2000 511 Feb 2001 5 levels ICD-10 (WHO) 1992 ICD-9 -CM 2000 1, 283 Oct 2003 5 levels ICD-10 (WHO) 2007 + ICD-10 -TM* ICD-9 -CM 2007 with extension 1, 920 Oct 2007 5 levels ICD-10 (WHO( 2010 ICD-9 -CM 2010 with extension Ho. NOS Barthel index 3 4 5 DRG 2, 450 TMHCC 54 SNAP 41 Expected on Oct 2011 * Thai Modification for data entry only (not for new classification) 11
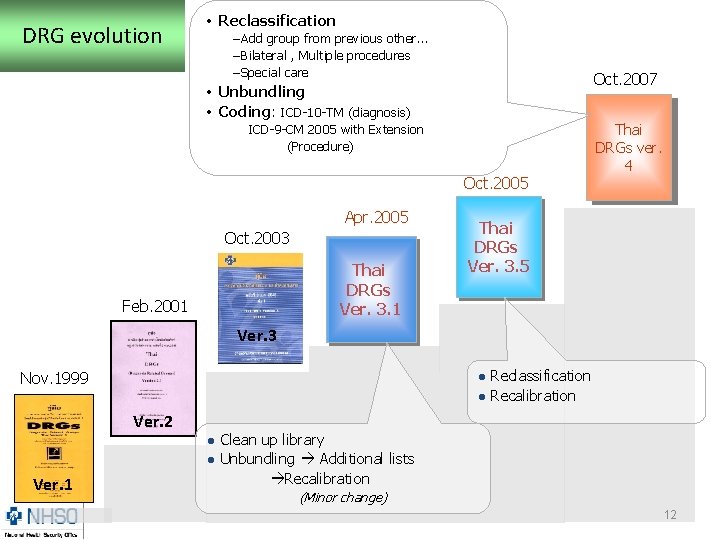
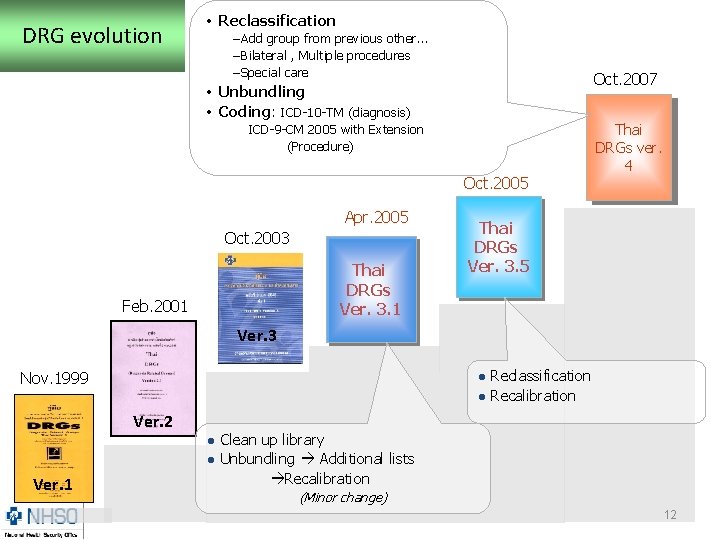
DRG evolution • Reclassification –Add group from previous other… –Bilateral , Multiple procedures –Special care Oct. 2007 • Unbundling • Coding: ICD-10 -TM (diagnosis) ICD-9 -CM 2005 with Extension (Procedure) Oct. 2005 Apr. 2005 Oct. 2003 Thai DRGs Ver. 3. 1 Feb. 2001 Thai DRGs ver. 4 Thai DRGs Ver. 3. 5 Ver. 3 Nov. 1999 l l Ver. 2 l l Ver. 1 Reclassification Recalibration Clean up library Unbundling Additional lists Recalibration (Minor change) 12
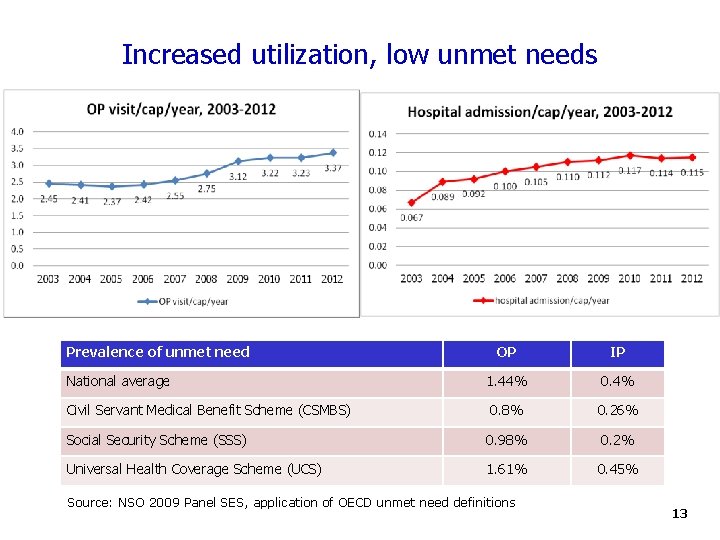
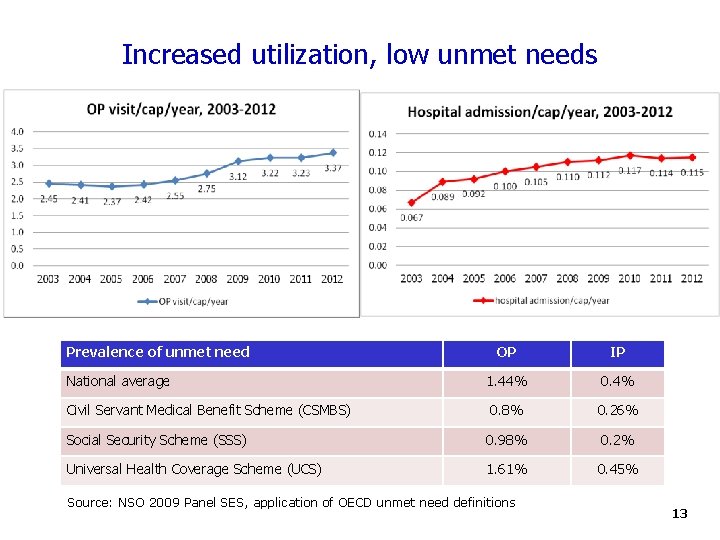
Increased utilization, low unmet needs Prevalence of unmet need OP IP National average 1. 44% 0. 4% Civil Servant Medical Benefit Scheme (CSMBS) 0. 8% 0. 26% Social Security Scheme (SSS) 0. 98% 0. 2% Universal Health Coverage Scheme (UCS) 1. 61% 0. 45% Source: NSO 2009 Panel SES, application of OECD unmet need definitions 13
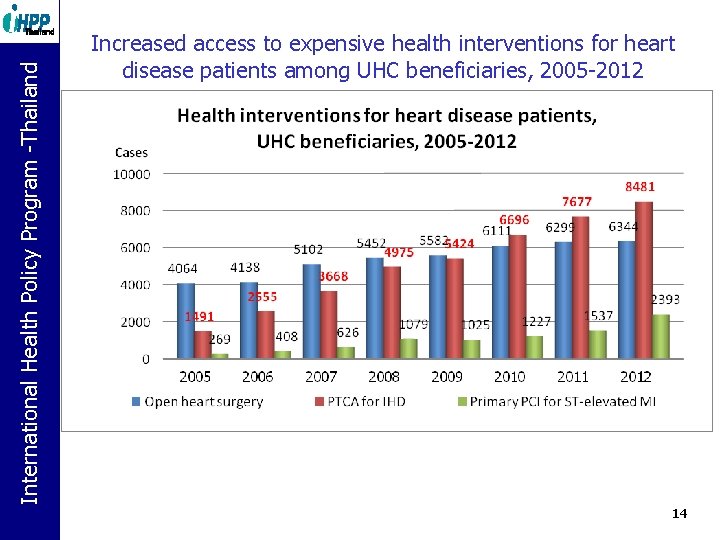
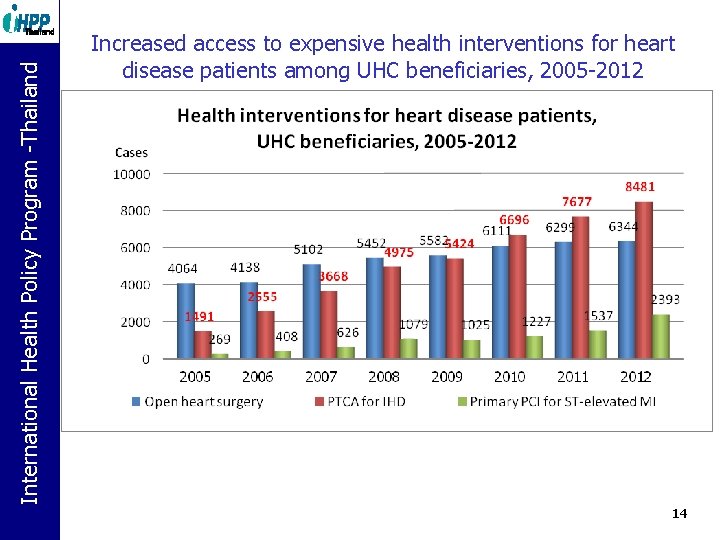
International Health Policy Program. Policy -Thailand Program -Thailand Increased access to expensive health interventions for heart disease patients among UHC beneficiaries, 2005 -2012 14
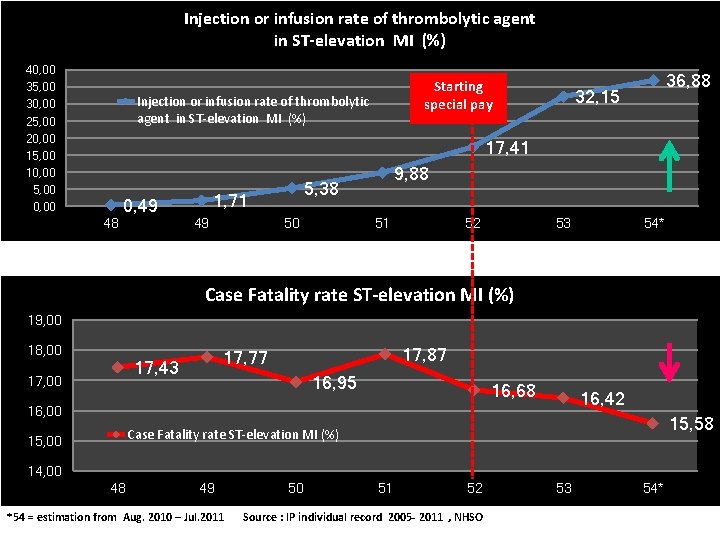
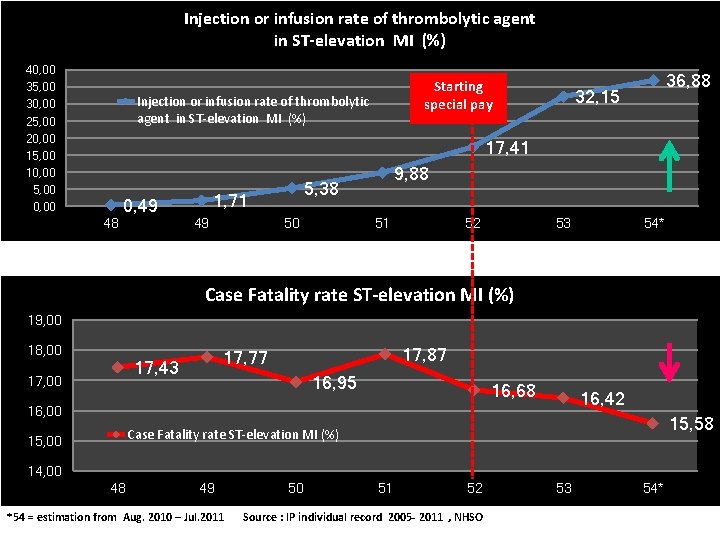
Injection or infusion rate of thrombolytic agent in ST-elevation MI (%) 40, 00 35, 00 30, 00 25, 00 20, 00 15, 00 10, 00 5, 00 0, 00 Starting special pay Injection or infusion rate of thrombolytic agent in ST-elevation MI (%) 36, 88 32, 15 17, 41 48 0, 49 5, 38 1, 71 49 9, 88 50 51 52 53 54* Case Fatality rate ST-elevation MI (%) 19, 00 18, 00 17, 87 17, 77 17, 43 16, 95 16, 68 16, 42 16, 00 15, 58 Case Fatality rate ST-elevation MI (%) 15, 00 14, 00 48 49 *54 = estimation from Aug. 2010 – Jul. 2011 50 51 52 Source : IP individual record 2005 - 2011 , NHSO 53 54*
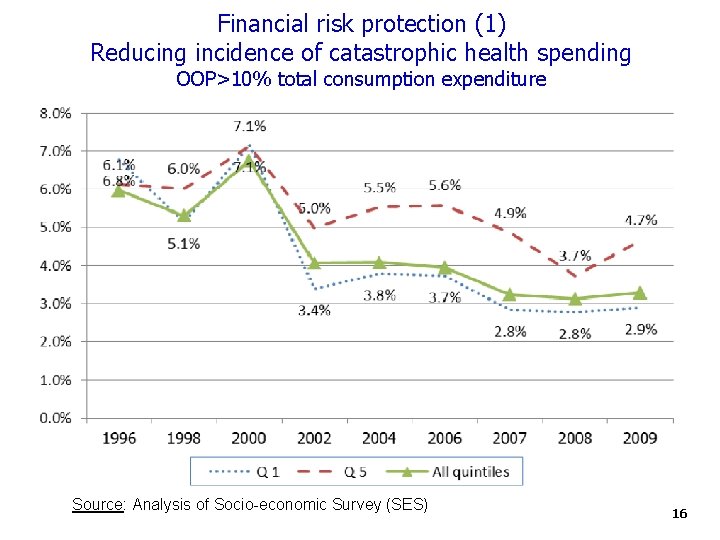
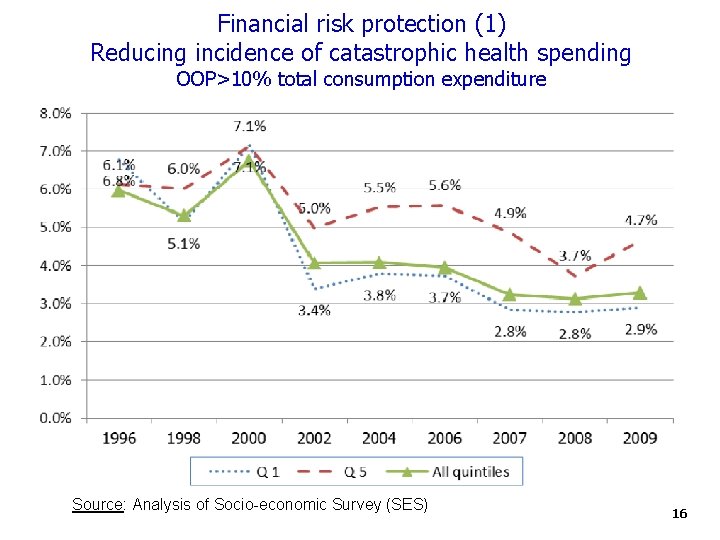
Financial risk protection (1) Reducing incidence of catastrophic health spending OOP>10% total consumption expenditure Source: Analysis of Socio-economic Survey (SES) 16
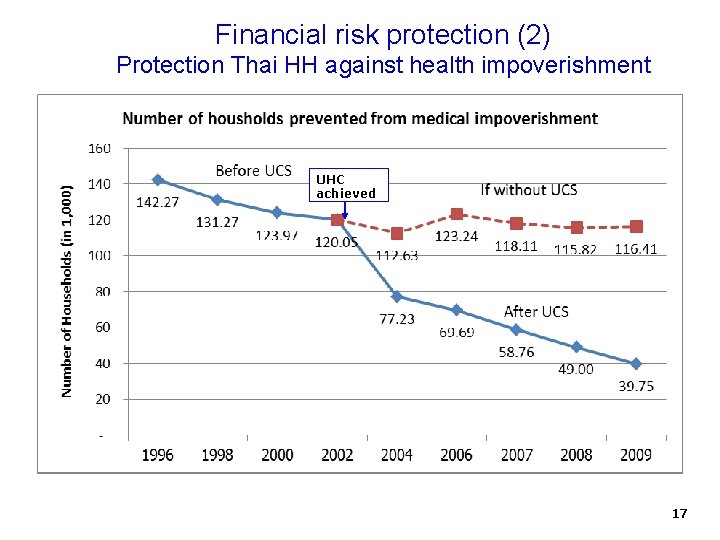
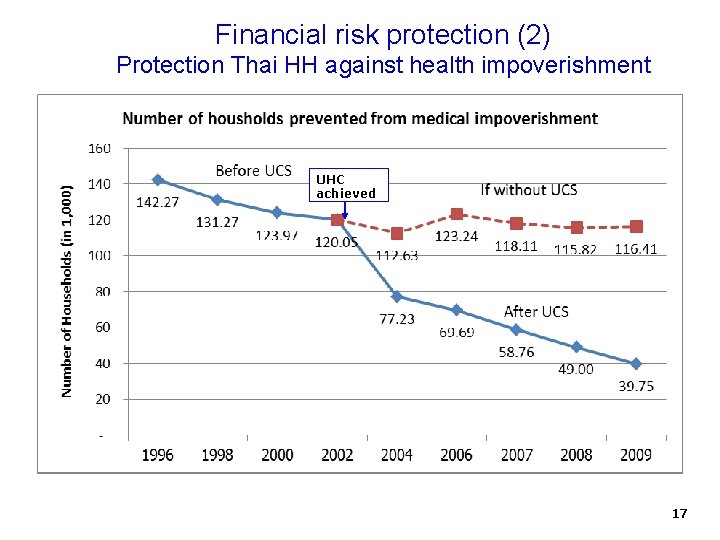
Financial risk protection (2) Protection Thai HH against health impoverishment UHC achieved 17
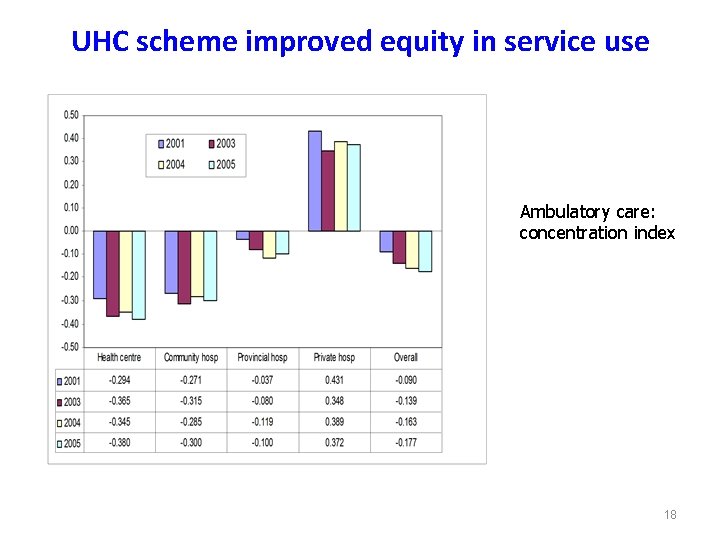
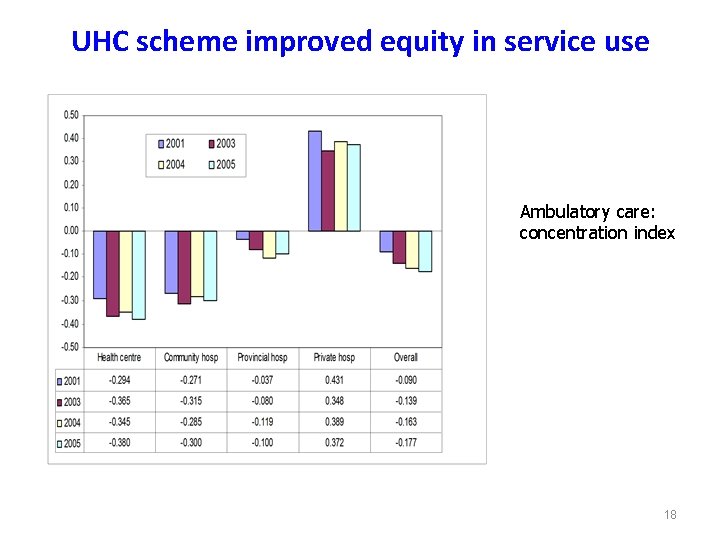
UHC scheme improved equity in service use Ambulatory care: concentration index 18
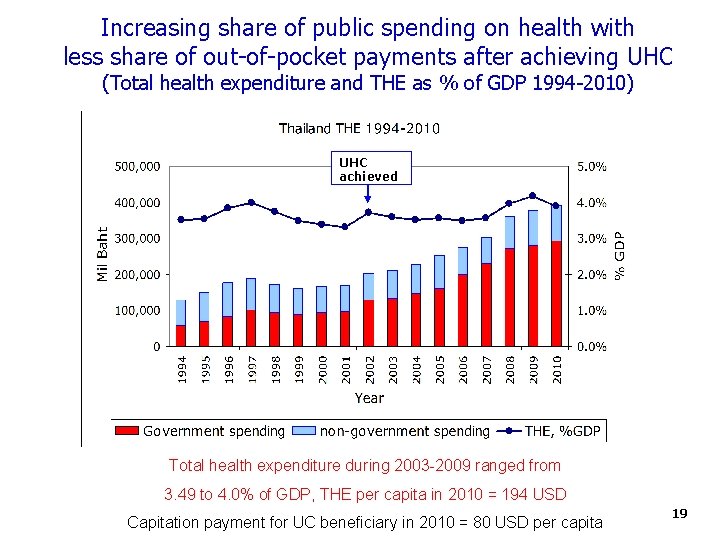
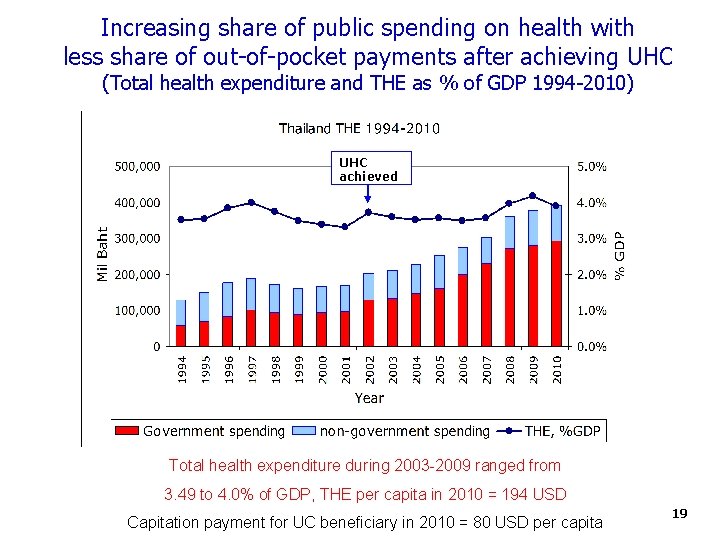
Increasing share of public spending on health with less share of out-of-pocket payments after achieving UHC (Total health expenditure and THE as % of GDP 1994 -2010) UHC achieved Total health expenditure during 2003 -2009 ranged from 3. 49 to 4. 0% of GDP, THE per capita in 2010 = 194 USD Capitation payment for UC beneficiary in 2010 = 80 USD per capita 19
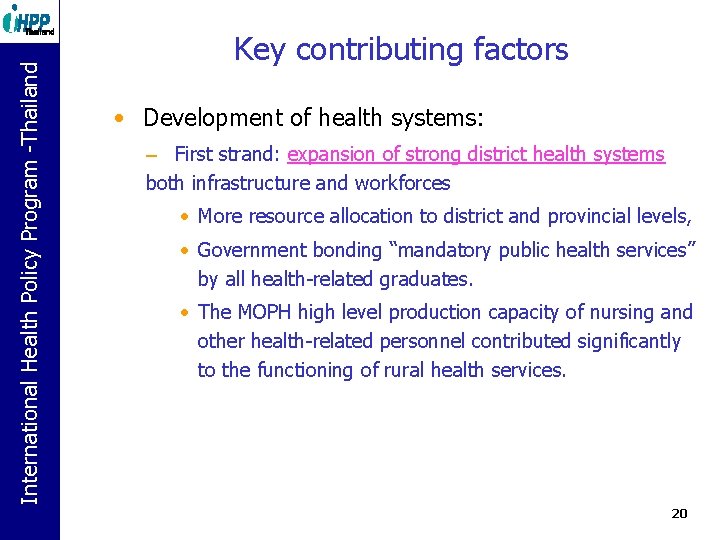
International Health Policy Program. Policy -Thailand Program -Thailand Key contributing factors • Development of health systems: – First strand: expansion of strong district health systems both infrastructure and workforces • More resource allocation to district and provincial levels, • Government bonding “mandatory public health services” by all health-related graduates. • The MOPH high level production capacity of nursing and other health-related personnel contributed significantly to the functioning of rural health services. 20
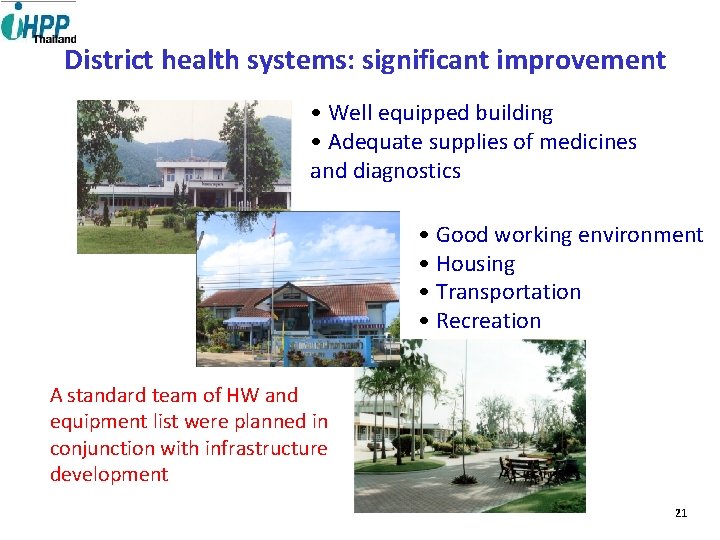
District health systems: significant improvement • Well equipped building • Adequate supplies of medicines and diagnostics • Good working environment • Housing • Transportation • Recreation A standard team of HW and equipment list were planned in conjunction with infrastructure development 21
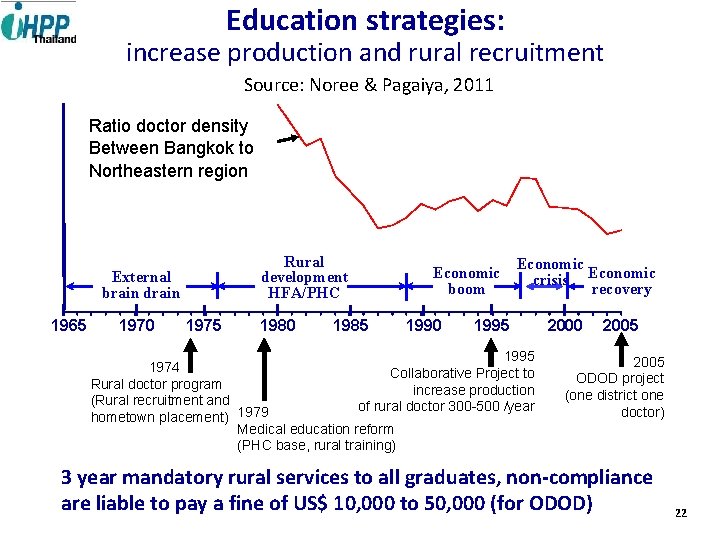
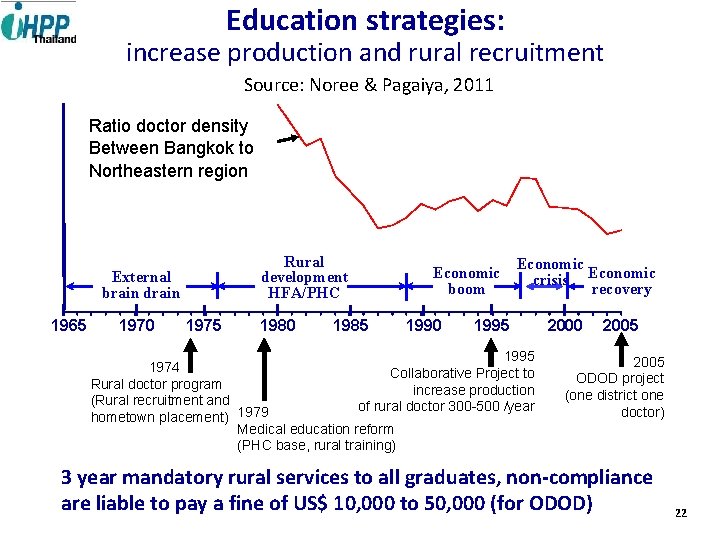
Education strategies: increase production and rural recruitment Source: Noree & Pagaiya, 2011 Ratio doctor density Between Bangkok to Northeastern region Rural development HFA/PHC External brain drain 1965 1970 1975 1980 1985 Economic boom 1990 Economic crisis Economic recovery 1995 1974 Collaborative Project to Rural doctor program increase production (Rural recruitment and of rural doctor 300 -500 /year hometown placement) 1979 Medical education reform (PHC base, rural training) 2000 2005 ODOD project (one district one doctor) 3 year mandatory rural services to all graduates, non-compliance are liable to pay a fine of US$ 10, 000 to 50, 000 (for ODOD) 22
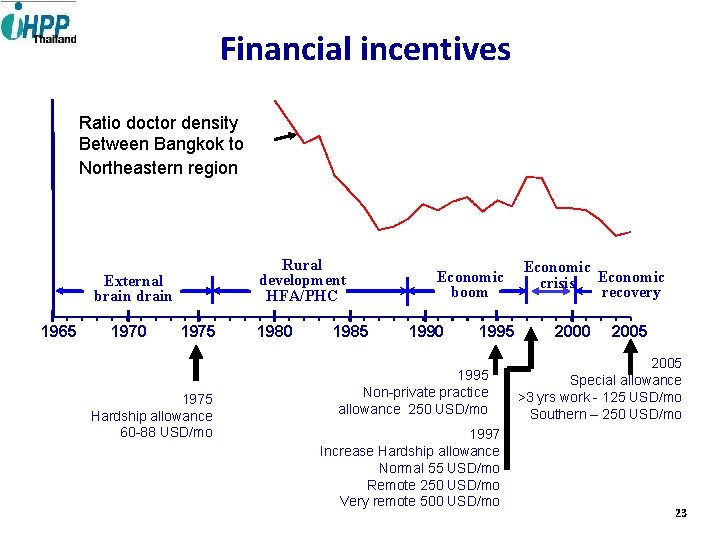
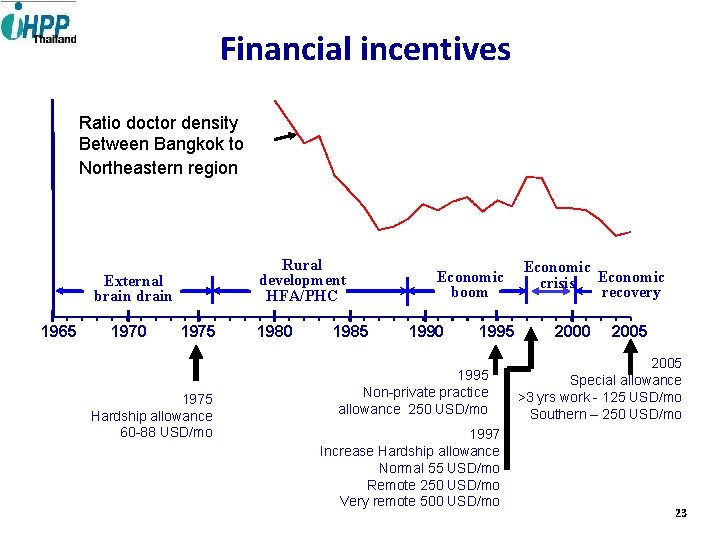
Financial incentives Ratio doctor density Between Bangkok to Northeastern region Rural development HFA/PHC External brain drain 1965 1970 1975 Hardship allowance 60 -88 USD/mo 1980 1985 Economic boom 1990 1995 Non-private practice allowance 250 USD/mo 1997 Increase Hardship allowance Normal 55 USD/mo Remote 250 USD/mo Very remote 500 USD/mo Economic crisis Economic recovery 2000 2005 Special allowance >3 yrs work - 125 USD/mo Southern – 250 USD/mo 23
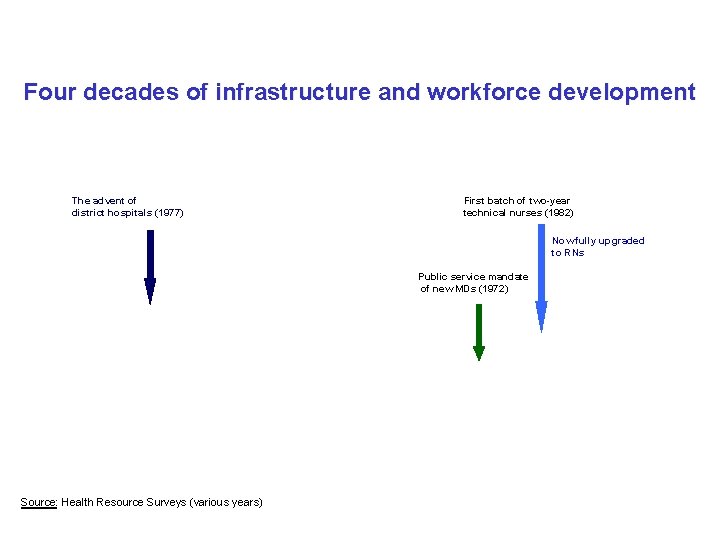
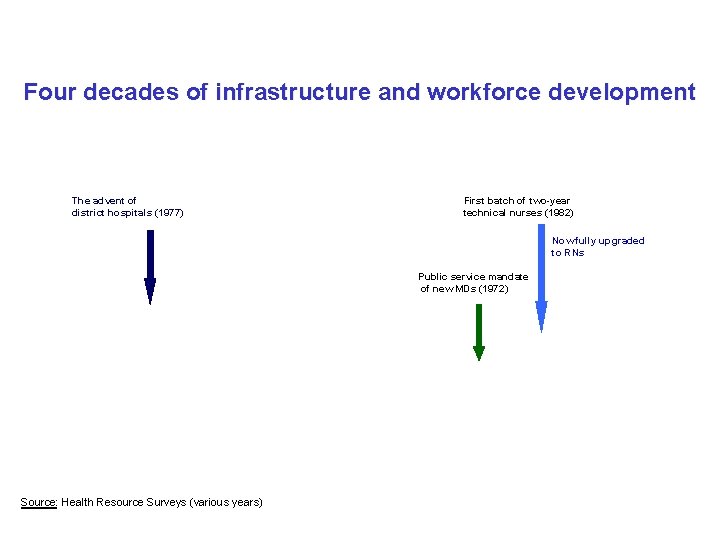
Four decades of infrastructure and workforce development The advent of district hospitals (1977) First batch of two-year technical nurses (1982) Now fully upgraded to RNs Public service mandate of new MDs (1972) Source: Health Resource Surveys (various years)
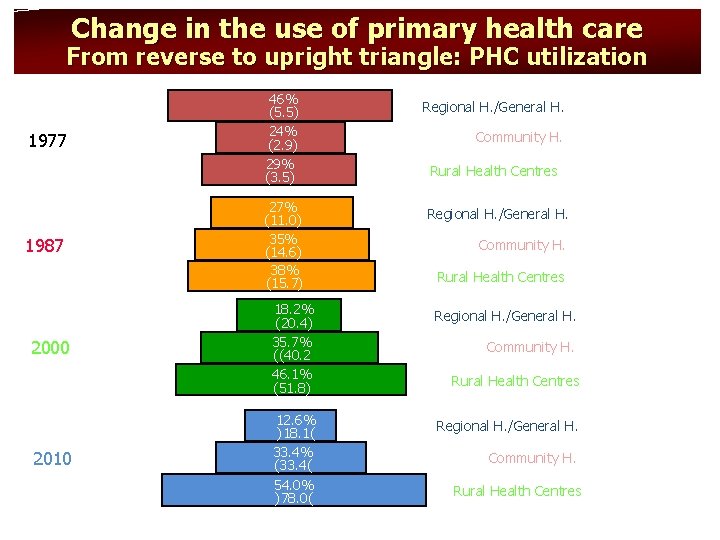
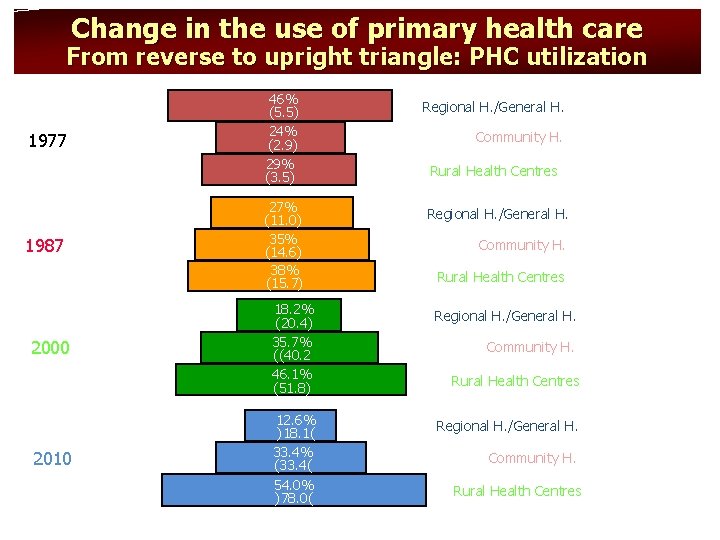
Change in the use of primary health care From reverse to upright triangle: PHC utilization 1977 1987 2000 2010 46% (5. 5) 24% (2. 9) 29% (3. 5) 27% (11. 0) 35% (14. 6) 38% (15. 7) Regional H. /General H. Community H. Rural Health Centres 18. 2% (20. 4) 35. 7% ((40. 2 46. 1% (51. 8) Regional H. /General H. 12. 6% )18. 1( 33. 4% (33. 4( 54. 0% )78. 0( Regional H. /General H. Community H. Rural Health Centres
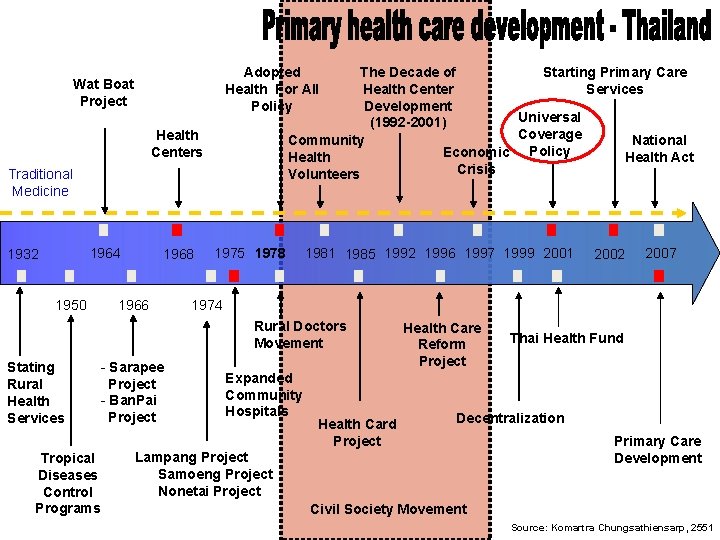
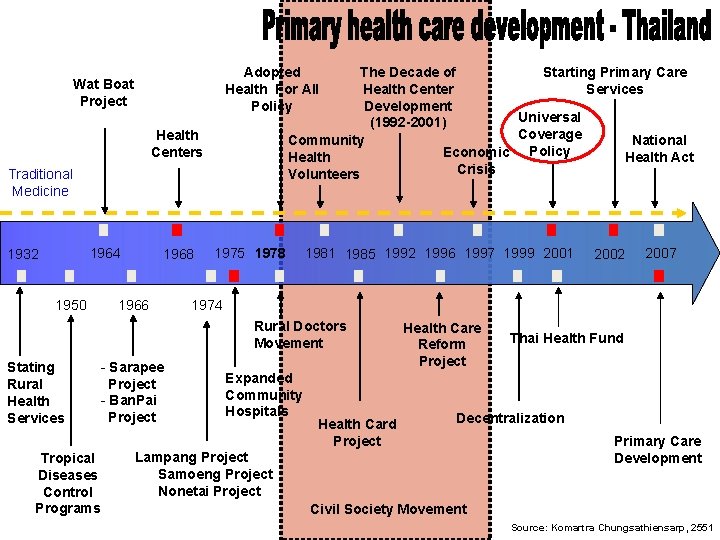
The Decade of Starting Primary Care Health Center Services Development Universal (1992 -2001) Coverage Community National Policy Economic Health Act Crisis Volunteers Adopted Health For All Policy Wat Boat Project Health Centers Traditional Medicine 1964 1932 1950 1968 1966 1975 1978 1981 1985 1992 1996 1997 1999 2001 Tropical Diseases Control Programs - Sarapee Project - Ban. Pai Project 2007 1974 Rural Doctors Movement Stating Rural Health Services 2002 Expanded Community Hospitals Health Card Project Health Care Reform Project Thai Health Fund Decentralization Lampang Project Samoeng Project Nonetai Project Primary Care Development Civil Society Movement Source: Komartra Chungsathiensarp, 2551
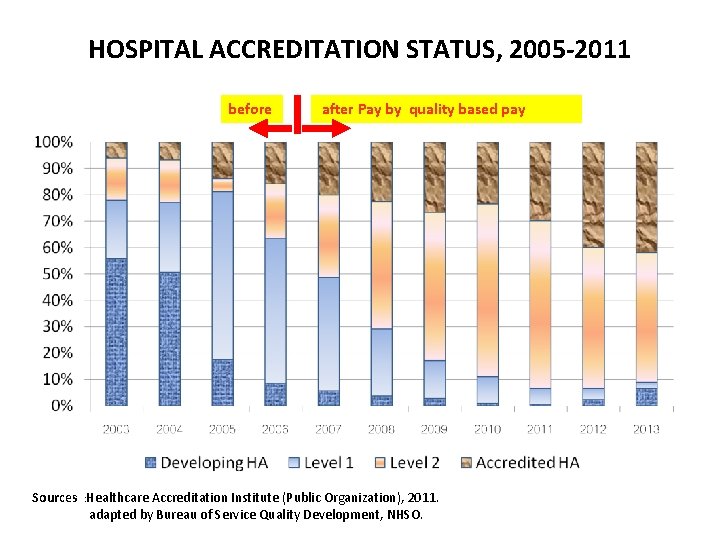
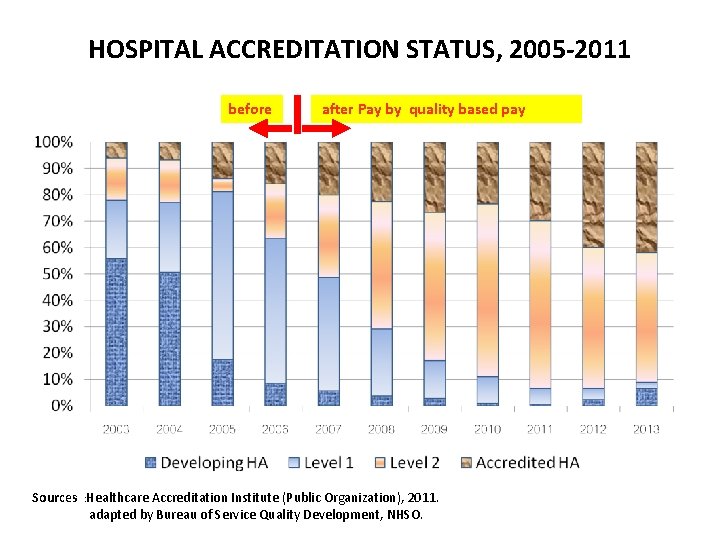
HOSPITAL ACCREDITATION STATUS, 2005 -2011 before after Pay by quality based pay Sources : Healthcare Accreditation Institute (Public Organization), 2011. adapted by Bureau of Service Quality Development, NHSO. หมายเหต ป 2554 เปนขอมล ณ ไตรมาส 2
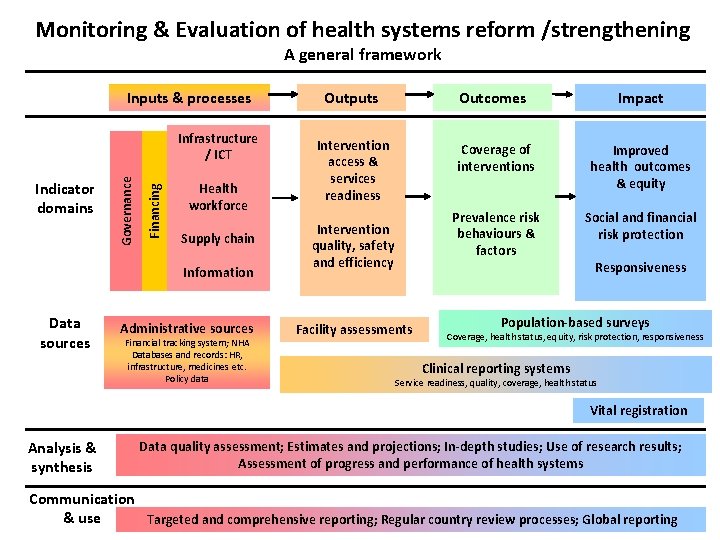
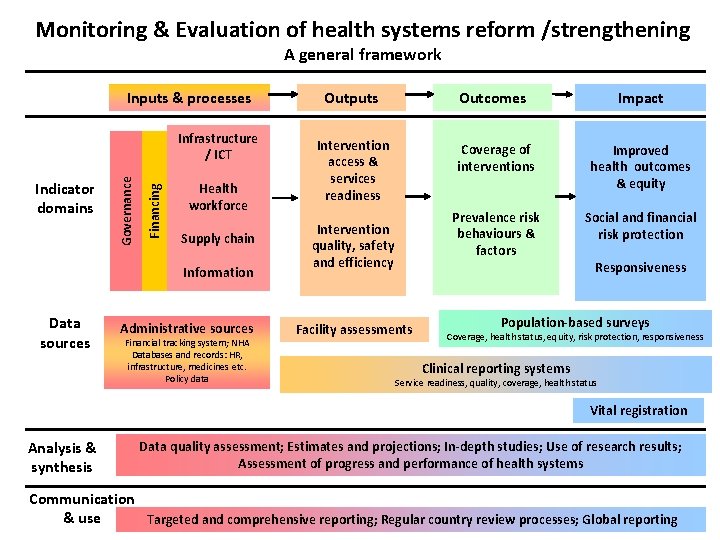
Monitoring & Evaluation of health systems reform /strengthening A general framework Inputs & processes Financing Indicator domains Governance Infrastructure / ICT Health workforce Supply chain Information Data sources Administrative sources Financial tracking system; NHA Databases and records: HR, infrastructure, medicines etc. Policy data Outputs Outcomes Impact Intervention access & services readiness Coverage of interventions Improved health outcomes & equity Prevalence risk behaviours & factors Social and financial risk protection Intervention quality, safety and efficiency Facility assessments Responsiveness Population-based surveys Coverage, health status, equity, risk protection, responsiveness Clinical reporting systems Service readiness, quality, coverage, health status Vital registration Analysis & synthesis Data quality assessment; Estimates and projections; In-depth studies; Use of research results; Assessment of progress and performance of health systems Communication & use Targeted and comprehensive reporting; Regular country review processes; Global reporting
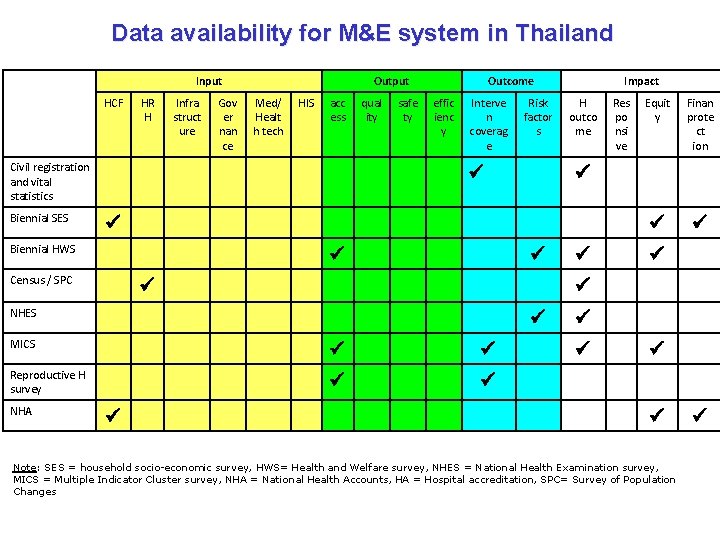
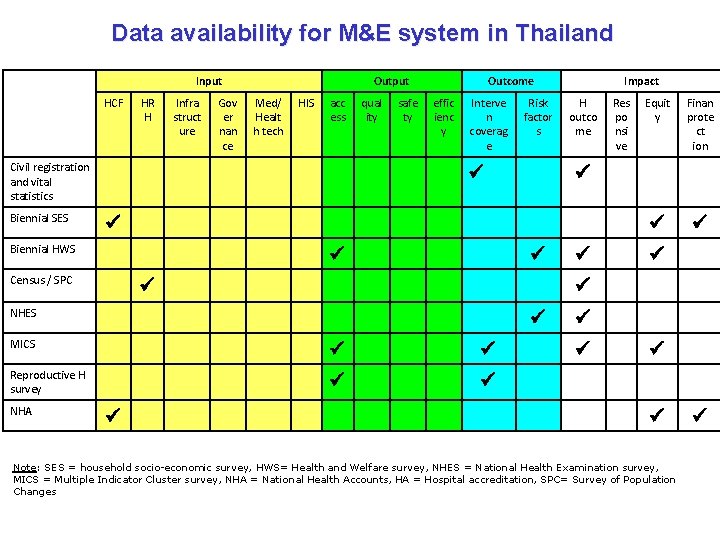
Data availability for M&E system in Thailand Input HCF HR H Infra struct ure Gov er nan ce Output Med/ Healt h tech HIS acc ess Civil registration and vital statistics Biennial SES qual ity safe ty Outcome effic ienc y Interve n coverag e H outco me Census / SPC Equit y Finan prote ct ion NHES MICS Reproductive H survey Res po nsi ve Biennial HWS NHA Risk factor s Impact Note: SES = household socio-economic survey, HWS= Health and Welfare survey, NHES = National Health Examination survey, MICS = Multiple Indicator Cluster survey, NHA = National Health Accounts, HA = Hospital accreditation, SPC= Survey of Population Changes
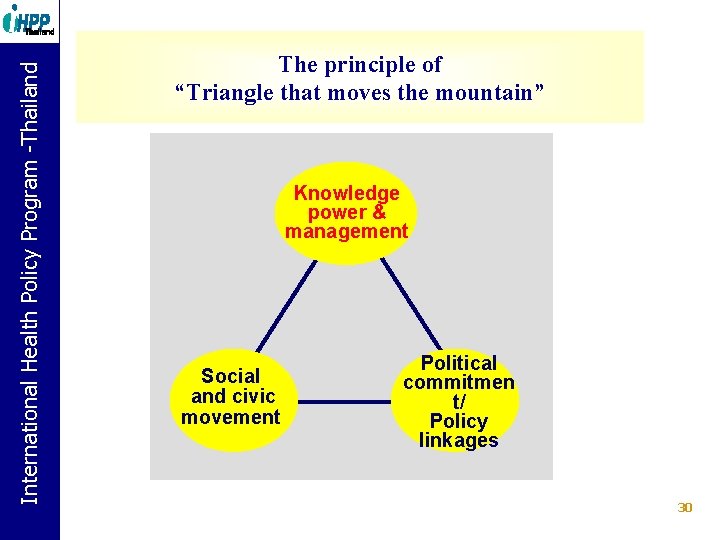
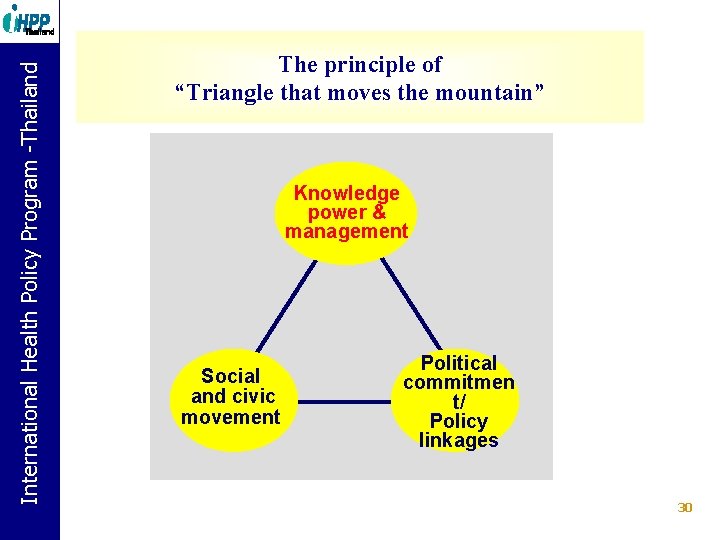
International Health Policy Program. Policy -Thailand Program -Thailand The principle of “Triangle that moves the mountain” Knowledge power & management Social and civic movement Political commitmen t/ Policy linkages 30

International Health Policy Program. Policy -Thailand Program -Thailand Acknowledgements • • • Ministry of Public Health (MOPH) of Thailand, National Statistical Office (NSO) of Thailand, National Health Security Office (NHSO) of Thailand, Health Systems Research Institute (HSRI), World Health Organization (WHO) 31