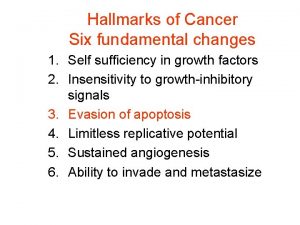
Hallmarks of malignancy 5 Development of Sustained Angiogenesis











- Slides: 28

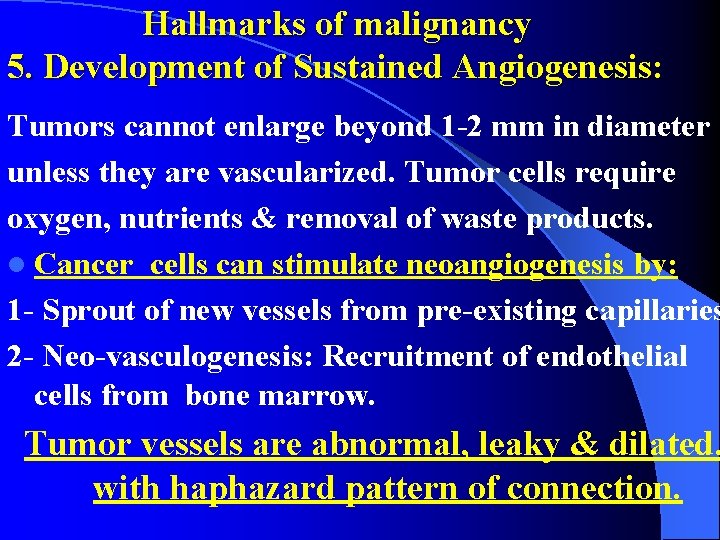
Hallmarks of malignancy 5. Development of Sustained Angiogenesis: Tumors cannot enlarge beyond 1 -2 mm in diameter unless they are vascularized. Tumor cells require oxygen, nutrients & removal of waste products. l Cancer cells can stimulate neoangiogenesis by: 1 - Sprout of new vessels from pre-existing capillaries 2 - Neo-vasculogenesis: Recruitment of endothelial cells from bone marrow. Tumor vessels are abnormal, leaky & dilated, with haphazard pattern of connection.

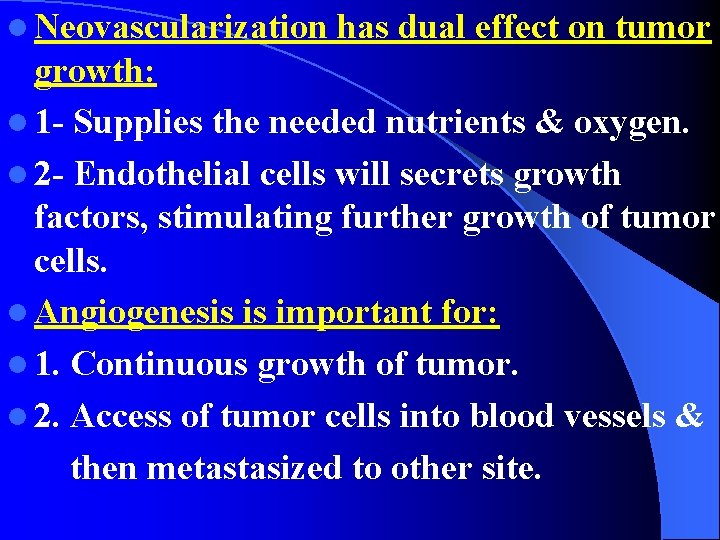
l Neovascularization has dual effect on tumor growth: l 1 - Supplies the needed nutrients & oxygen. l 2 - Endothelial cells will secrets growth factors, stimulating further growth of tumor cells. l Angiogenesis is important for: l 1. Continuous growth of tumor. l 2. Access of tumor cells into blood vessels & then metastasized to other site.

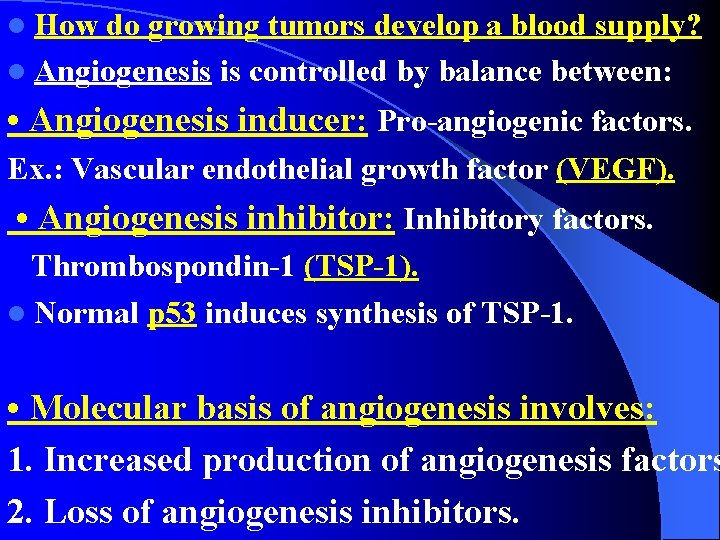
l How do growing tumors develop a blood supply? l Angiogenesis is controlled by balance between: • Angiogenesis inducer: Pro-angiogenic factors. Ex. : Vascular endothelial growth factor (VEGF). • Angiogenesis inhibitor: Inhibitory factors. Thrombospondin-1 (TSP-1). l Normal p 53 induces synthesis of TSP-1. • Molecular basis of angiogenesis involves: 1. Increased production of angiogenesis factors 2. Loss of angiogenesis inhibitors.
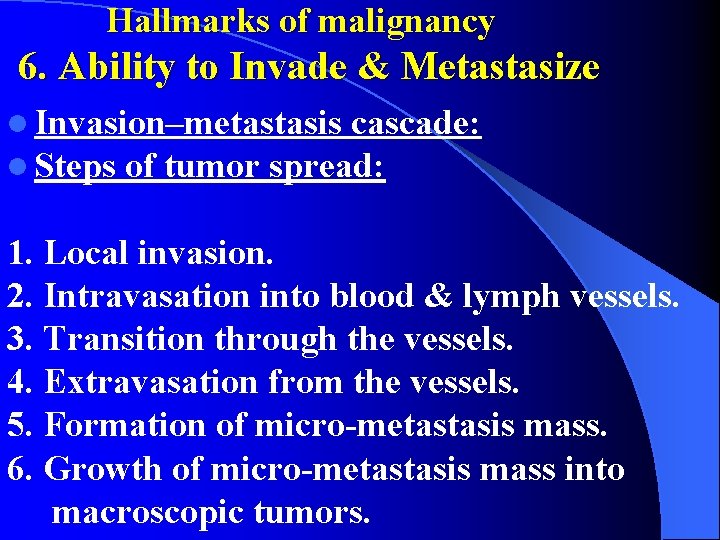
Hallmarks of malignancy 6. Ability to Invade & Metastasize l Invasion–metastasis cascade: l Steps of tumor spread: 1. Local invasion. 2. Intravasation into blood & lymph vessels. 3. Transition through the vessels. 4. Extravasation from the vessels. 5. Formation of micro-metastasis mass. 6. Growth of micro-metastasis mass into macroscopic tumors.

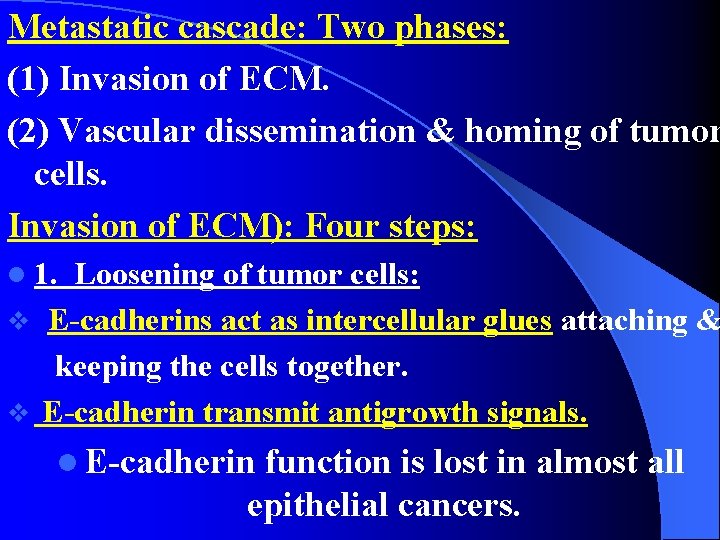
Metastatic cascade: Two phases: (1) Invasion of ECM. (2) Vascular dissemination & homing of tumor cells. Invasion of ECM): Four steps: l 1. Loosening of tumor cells: v E-cadherins act as intercellular glues attaching & keeping the cells together. v E-cadherin transmit antigrowth signals. l E-cadherin function is lost in almost all epithelial cancers.

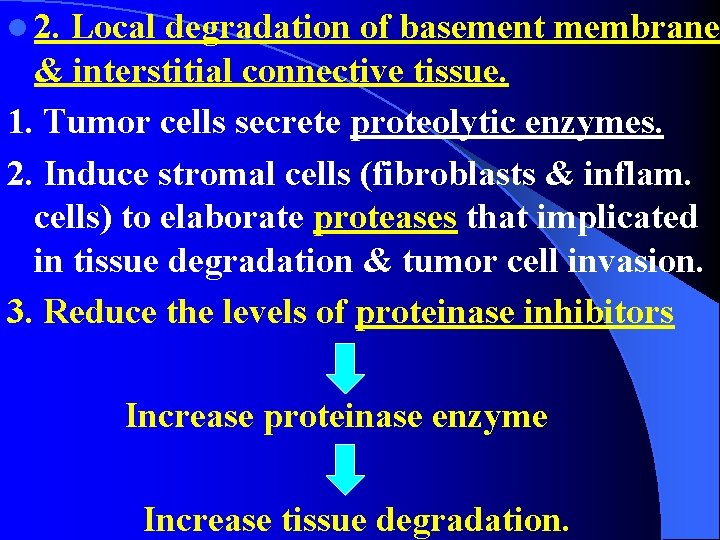
l 2. Local degradation of basement membrane & interstitial connective tissue. 1. Tumor cells secrete proteolytic enzymes. 2. Induce stromal cells (fibroblasts & inflam. cells) to elaborate proteases that implicated in tissue degradation & tumor cell invasion. 3. Reduce the levels of proteinase inhibitors Increase proteinase enzyme Increase tissue degradation.

l 3. Attachment: l Normal epithelial cells have receptors help to maintain cells in resting differentiated state. l Ex. : Integrins receptor for laminin & collagens of the basement membrane are present at their basal surface. l In tumor: There are changes in the attachment of tumor cells to ECM proteins. l Loss of adhesion in normal cells leads to induction of apoptosis. l Tumor cells are resistant to apoptosis.

l • 4. Migration: l Locomotion of tumor cells through the degraded basement membranes & matrix. l Involves many receptors & signaling proteins that impinge on actin cytoskeleton. l Such movement is potentiated & directed by: l 1. Tumor cell–derived cytokines such as: l Autocrine motility factors. l 2. Cleavage products of ECM (collagen, laminin). l 3. Chemotactic activity of some growth factors for tumor cells.

Vascular Dissemination & Homing of Tumor Cells: l Most tumor cells circulate as single cells. l Some tumor cells form emboli by aggregating & adhering to platelets so protected from immune cells. l Extravasation of free tumor cells or tumor emboli involves: l 1. Adhesion to vascular endothelium. l 2. Go out through basement membrane to the parenchyma by mechanisms similar to those involved in invasion.

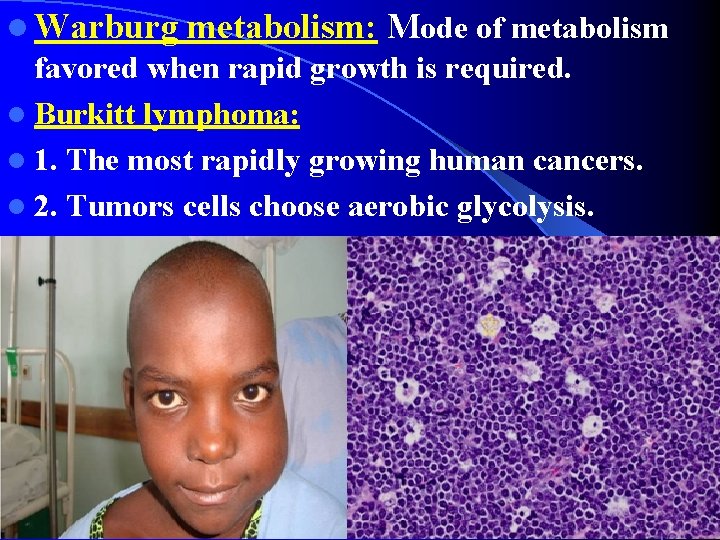
Hallmarks of malignancy 7. Reprogramming of Energy Metabolism: l Cancer cells shift their glucose metabolism into aerobic glycolysis, called: Warburg effect: l Produce 2 molecules of ATP / molecule of glucose. l It is less efficient than mitochondrial oxidative phosphorylation (produce 36 molecule of ATP). l Cancer cells produce less ATP but its production is hundred times faster than normal cells. l So there is increase in glucose uptake, a major feature distinguish tumor cells from normal cells.
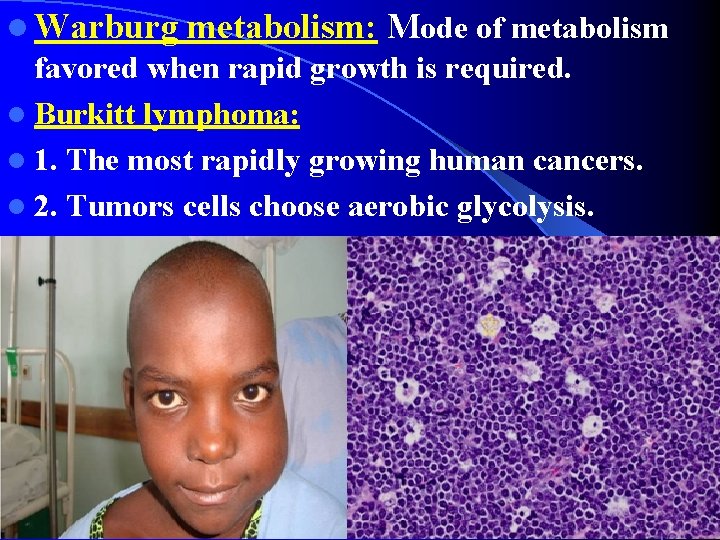
l Warburg metabolism: Mode of metabolism favored when rapid growth is required. l Burkitt lymphoma: l 1. The most rapidly growing human cancers. l 2. Tumors cells choose aerobic glycolysis.
Hallmarks of malignancy 8. Evasion of the Immune System: q Tumors cells have ability to avoide destruction by the immune system. q Most tumors arise in immuno-competent hosts. q Tumor cells can trick the immune system so they are not recognized or eliminated. l What l are the nature of tumor antigens and how they might be recognized? Tumor immunity
Hallmarks of malignancy 9. Genomic Instability as Enabler of cancer: l The preceding eight features of malignancy occurs due to genetic alterations or mutation. l How do these mutations arise? l Mutagenic environmental agents: Chemicals, radiation, sunlight DNA damage l They rarely cause cancers due to ability of normal cells to repair any DNA damage occurred. l Defects in the genes encode proteins that repair the damaged DNA Cancer. Ex. : 1. Hereditary Nonpolyposis Colon Cancer Syndrome 2. Xeroderma Pigmentosum.
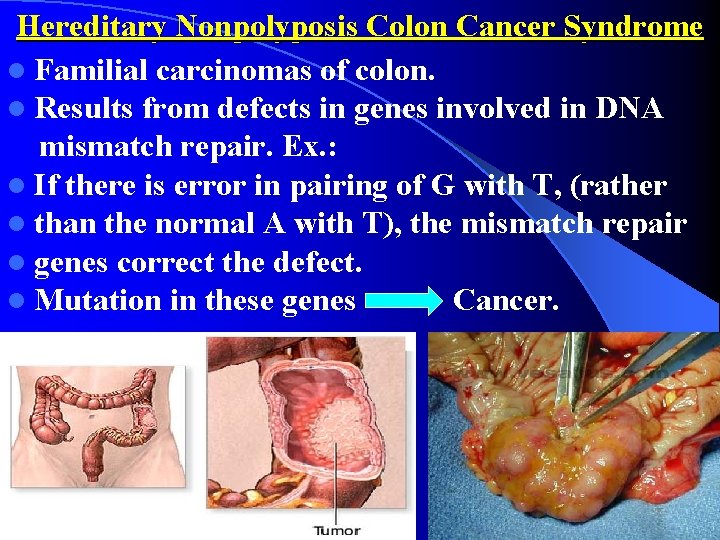
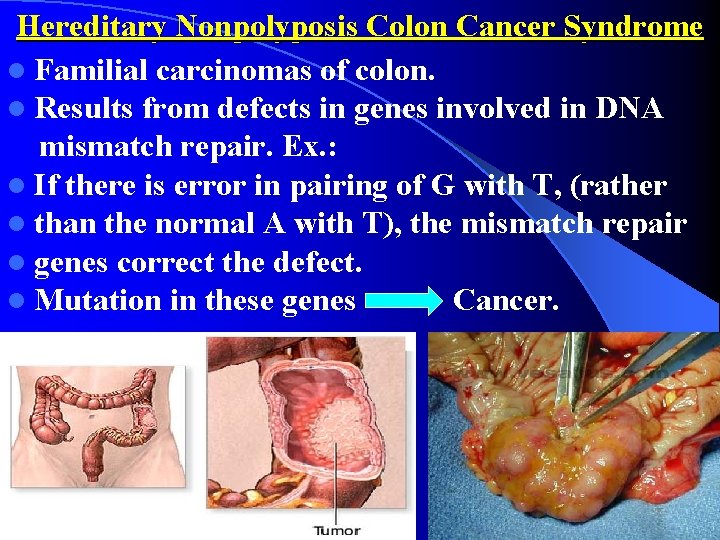
Hereditary Nonpolyposis Colon Cancer Syndrome l Familial carcinomas of colon. l Results from defects in genes involved in DNA mismatch repair. Ex. : l If there is error in pairing of G with T, (rather l than the normal A with T), the mismatch repair l genes correct the defect. l Mutation in these genes Cancer.

Xeroderma Pigmentosum l Inherited disorder. l Cancers in the sun-exposed skin. l There is defective DNA repair.
Hallmarks of malignancy 10. Tumor-Promoting Inflammation as Enabler of cancer: l Inflammation is protective response against tumor l Can enable malignancy in two ways: l • 1 - Persistent chronic inflammation: l Ex. : Microbial infections or autoimmune reaction. l Increased risk of cancer. l Ex. : Chronic inflammatory diseases of GIT: l Barrett esophagus, ulcerative colitis, H. pylori gastritis, hepatitis B & C & chronic pancreatitis. l
l In chronic tissue injury: l A: Regenerative process as a compensatory proliferation of cells to repair damage, aided by growth factors, cytokines, chemokines produced by immune cells at the site. l Persistent cell replication & reduced apoptosis: Increase risk of genetic mutations. B: Reactive oxygen species formed by inflammatory cells Additional DNA damage in the rapidly dividing cells Carcinogenesis.
l The second way: l • 2 - When inflammation occur in response to tumors. l Many tumors are infiltrated by inflammatory cells (Leukocytes), producing growth factors: l Exert tumor-promoting activity. l Causes additional DNA damage.

 Neoplasia
Neoplasia Most common malignancy in hiv
Most common malignancy in hiv Rmi risk of malignancy index
Rmi risk of malignancy index Tumor angiogenesis
Tumor angiogenesis Ibidi free sample
Ibidi free sample Sprouting and intussusceptive angiogenesis
Sprouting and intussusceptive angiogenesis Hallmarks of benedictine education
Hallmarks of benedictine education Bagaimana peran metode ilmiah dalam penelitian
Bagaimana peran metode ilmiah dalam penelitian Firm resources and sustained competitive advantage barney
Firm resources and sustained competitive advantage barney Dealing with synoynm
Dealing with synoynm Extended release vs sustained release
Extended release vs sustained release Sustained release
Sustained release Sustained movement in dance
Sustained movement in dance Metaphor examples
Metaphor examples Divided attention examples
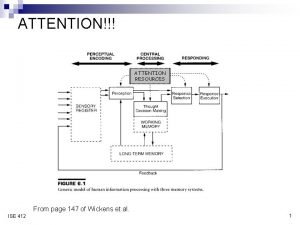
Divided attention examples Immediate release dosage form
Immediate release dosage form Benefits of hpw
Benefits of hpw Joint play assessment grades
Joint play assessment grades Sustained silent reading rules
Sustained silent reading rules Silent reading adalah
Silent reading adalah What flexibility assessment requires a partner
What flexibility assessment requires a partner Ocusert definition
Ocusert definition Example of sustained attention
Example of sustained attention How are local cultures sustained
How are local cultures sustained Evolution of community development
Evolution of community development Development that ended much development crossword
Development that ended much development crossword Surface development of a truncated cylinder
Surface development of a truncated cylinder Coop swot
Coop swot Processing development environment
Processing development environment