Growth and Development University of Maryland School of


- Slides: 30
Growth and Development University of Maryland School of Dentistry Department of Orthodontics
UNIT A 4 Theories of Craniofacial Growth
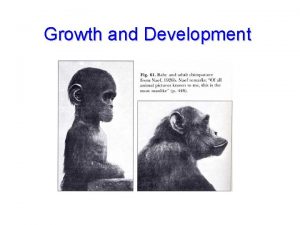
Introduction • • • Growth is influenced by genetics, environment, nutrition, physical activity, health, illness and similar factors. Since much of orthodontic treatment is created by disproportionate growth of the jaws, and to understand the etiologic processes of malocclusion and dentofacial deformity, it is vital to learn how facial growth is influenced and controlled. Three major theories in recent years have attempted to explain the determinants of craniofacial growth: 1. Bone as primary determinant of its own growth genetic control in bone 2. Cartilage is primary determinant of skeletal growth, while bone responds secondarily and passively genetic control in cartilage, and bone indirectly controlled epigenetically 3. Soft tissue matrix in which the skeletal elements are embedded is primary determinant of growth, and both bone and cartilage are secondary followers genetic control mediated largely outside skeletal system, and both bone and cartilage controlled epigenetically • First view has been discarded. Today truth found in second and third view.
Theories of Craniofacial Growth • Remodeling Theory (1930 s) • Suture Theory (1940 s) • Nasal Septum Theory (1950 s) • Functional Matrix Theory (1960 s)
Remodeling Theory • 1930 s • Research by Brash provided the foundation for the development of the first theory of craniofacial growth • The principles of theory were – Bone grows appositionally at its surfaces – Grow of the jaws occurs by apposition of bone in the posterior surfaces of the maxilla and mandible – Bone of the cranial base occurs by deposition on the external surface and resorption on the internal surface • All growth occurred by bone remodeling – selective apposition and resorption. • Sutures and cartilages have no role in growth of the craniofacial skeleton
Suture Theory • 1940’s • Weinmann and Sicher prominent anatomists worked on the suture theory • This theory proposes that the growth of the craniofacial bone is driven by intrinsic property inside the suture • The connective tissue and cartilagenous joints of the craniofacial skeleton are the primary sites were growth takes place and it’s genetically regulated • The suture is the driving force for bone growth
Suture Theory • The cranial vault grows by an intrinsic pattern of proliferative growth at the suture connective tissue • The maxilla grows downward and forward by proliferation of sutural connective tissue in the suture system surrounding the maxilla • The mandible was thought as a long bone that was bent. • The condylar cartilage was the equivalent to the epiphyseal plates of long bones and grow the mandible downward and forward away from the cranial base
Suture Theory • The suture theory explained two factors that the remodeling theory could not explain – The periosteal remodeling of bone is influenced strongly by environmental factors which made it unlikely to be under intrinsic hereditary control – The sutural theory was consistent with the importance of the cartilagenous structures and skeletal joints in the development and postnatal growth of bones • Growth of the face and jaws was unchallengeable and the sutures were the locations of centers of bone growth.
• 1950 s • Proposed by Irish anatomist James H. Scott. • Several experiments involving dies and surgical manipulation of the cranial sutures demostrated that the sutures were major sites of craniofacial growth but did not play a determining role in that growth • This theory contradicts the sutural theory in that it does not believe in the intrinsic factor (hereditary) inside the suture. • There is no direct role of suture to control growth. The suture are compensatory and may contribute secondarily • Scott proposed an alternative explanation the Nasal Septum Theory as a single theory of craniofacial growth
Nasal Septum Theory • Scott proposed that growth of the Nasal Septal Cartilage is the major driving force for the growth of midface to forward and downward direction. • Scott concluded that the nasal septum is the most active for craniofacial skeletal growth late prenatally and early postnatally through 3 to 4 years of age in humans • The growth of the cartilage which is supported at the cranial base posteriorly pushes the midface downward and forward • The cranial base synchondroses also have a lasting effect of craniofacial growth • Also the cartilage of the condyle determines the growth of the mandible downward and forward
Nasal Septum Theory • Numerous experiments were conducted in the 1950 s and 1960 s to address the sutural and nasal septum theories • It became clear that the sutures are secondary sites and very responsive to expansion of the contents of the cranial vault (i. e hydrocephaly) • Also the sutures were responsive to orthopedic manipulation of the growing maxillary complex • Other studies performed experiments that confirmed that normal growth of the nasal septum is very important for the growth of the maxillary complex • These experiments involved excision or disruption of the nasal septal cartilage in animals. – The results reported detrimental effects in the growth of the midface – However the surgeries were relatively crude so there was a criticism regarding the cause of the midface deficiency. – Was it the lack of the nasal septum of it was scar tissue from the surgery?
Paradigm Shift • Growth Centers vs Growth Sites – Areas of the growing skeleton with tissue separating capabilities which included craniofacial cartilages that are under control of heredity were called Growth Centers – Areas were growth occurs as a secondary, compensatory activity were called Growth Sites – Growth Sites lack direct genetic influence and are influenced by the environment
Functional Matrix Theory • 1960 s • Proposed by Melvin Moss dentist-anatomist • He theorizes that growth of the face occurs as a response to functional needs an neurotropic influences and is mediated by the soft tissue in which the jaws are embedded. In this conceptual view, the soft tissue grow, and both bone and cartilage react. • An example of the so-called functional matrix is the brain which is believed to contribute to growth of skull. Pressure exerted by the growing brain separates the cranial bones at the sutures, and new bone passively fills in at these sites so that the brain case fits the brain. Moss theorizes that the major determinant of growth of the maxilla and mandible is the enlargement of the nasal and oral cavities, which grow in response to functional needs. • • The functional matrix concept was developed primarily for bone growth; the biologic principles involved can be extended to soft tissue too.
Functional Matrix Theory • Functional Cranial Components – Functional Matrix • All soft tissues and spaces that perform a given function – Skeletal Unit • Bony structures that support the functional matrix and are necessary for that function • Skeletal units are not individual bones but a group of bones that support a certain function
Functional Matrix Theory • Functional Matrices – Periosteal Matrix • Corresponds to the immediate local environment • Muscles, blood vessels and nerves – Capsular Matrix • Organs and spaces that occupy a broader anatomical complex • Brain, eyes, and spaces such as nasopharynx and oropharynx
• Skeletal Units – Microskeletal Units • Variations in the periosteal matrix because of muscular activity (i. e. tuberosities or ridges for muscle attachment) • Size and shape of microskeletal units is associated with transformation of embryonic cell to osteoblast to osteocyte (periosteal deposition) – Macroskeletal Units • Neurocranium and maxillomandibular complex • Expansion of capsular matrices and translational growth of associated skeletal structures – The craniofacial skeleton does not grow in primary fashion to permit expansion of soft tissues, organs and spaces. – Translation of skeletal units occurs secondarily and in compensation to the growth of the functional matrix, and expansion growth related to the capsular matrices.
Functional Matrix Theory • There was a lot of debate in the 1960 s and 1970 s about the functional matrix theory because it was a new way to see craniofacial growth – The theory was criticized because of to simplistic view about “function” – There was a very extreme position on the role of the cartilages regarding growth of the craniofacial skeleton.
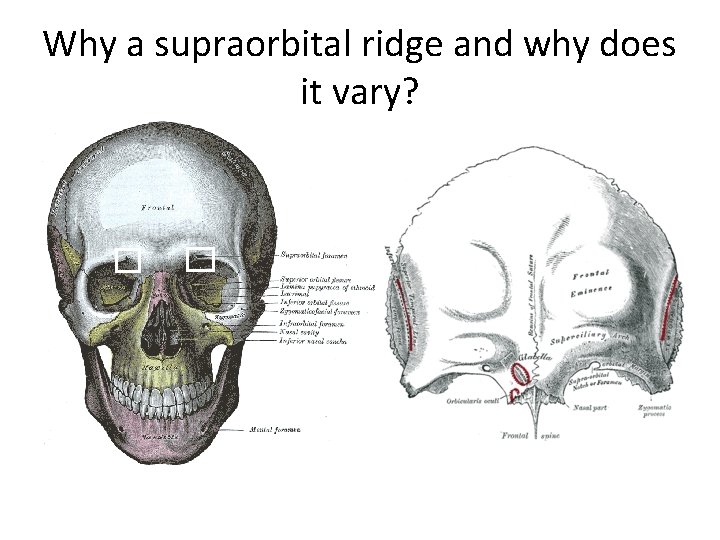
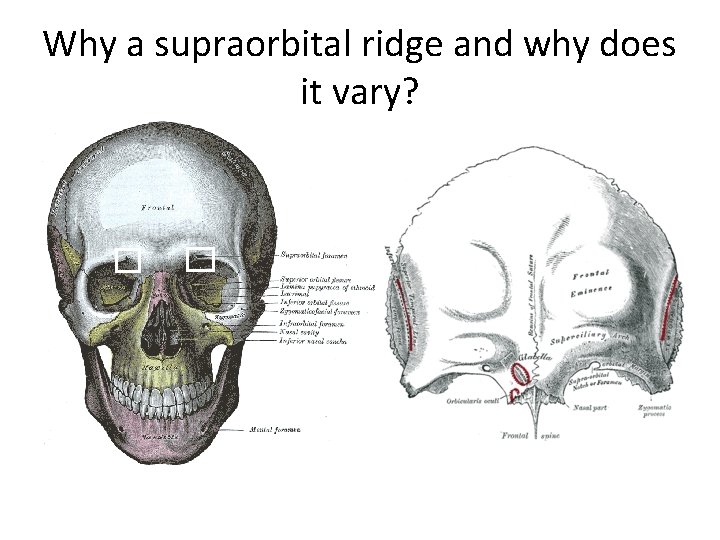
Why a supraorbital ridge and why does it vary?
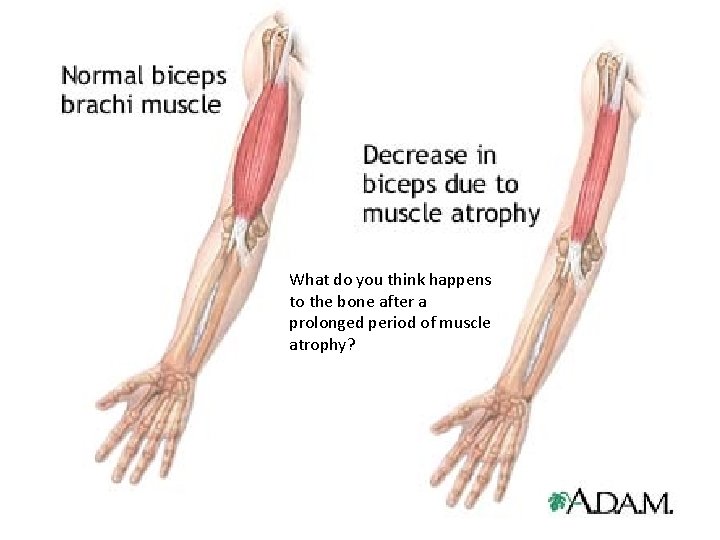
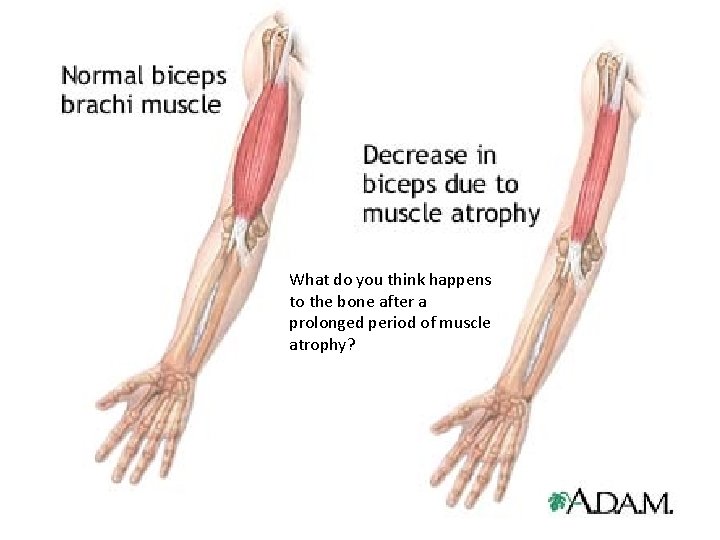
What do you think happens to the bone after a prolonged period of muscle atrophy?
• A new study by researchers at San Francisco VA Medical Center (SFVAMC) moves in on the physiological basis for the bone density loss experienced by people subjected to prolonged periods of bed rest and by astronauts who fly lengthy missions under the weightless conditions of space.
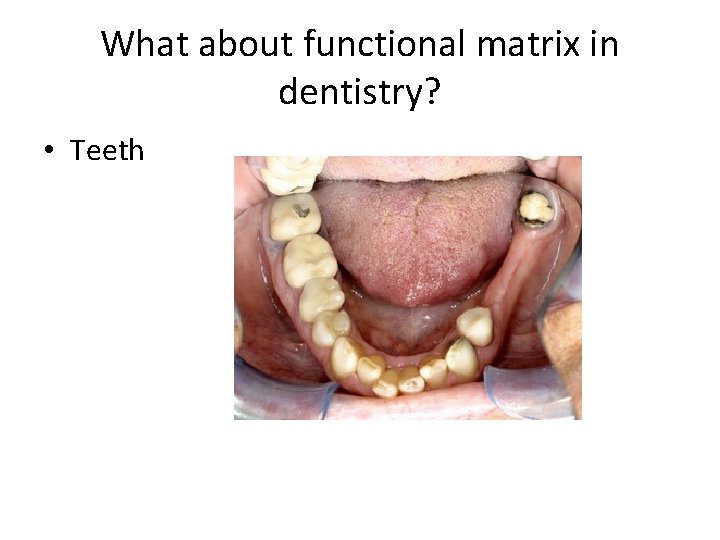
What about functional matrix in dentistry? • Teeth
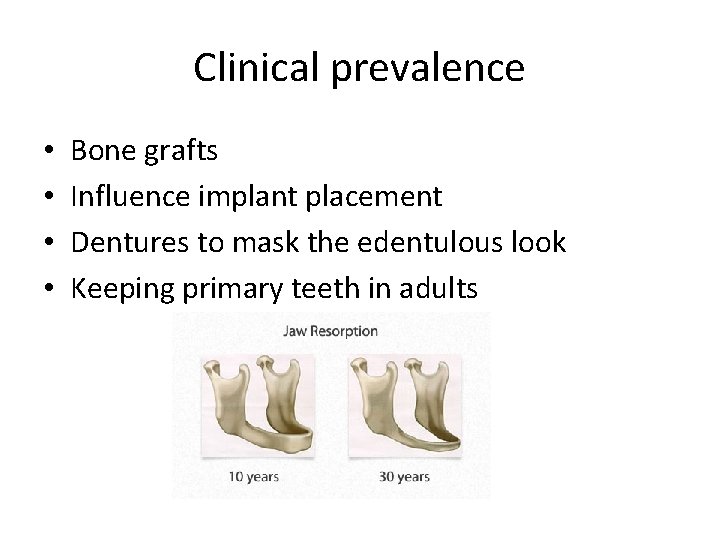
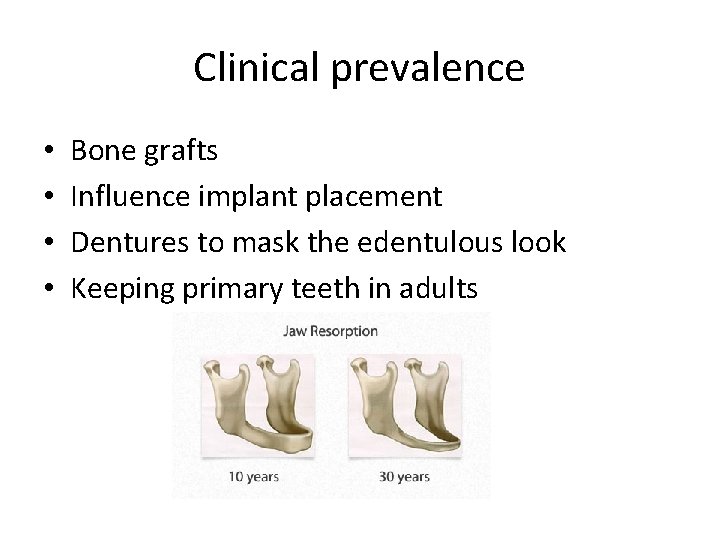
Clinical prevalence • • Bone grafts Influence implant placement Dentures to mask the edentulous look Keeping primary teeth in adults

Why this open bite?
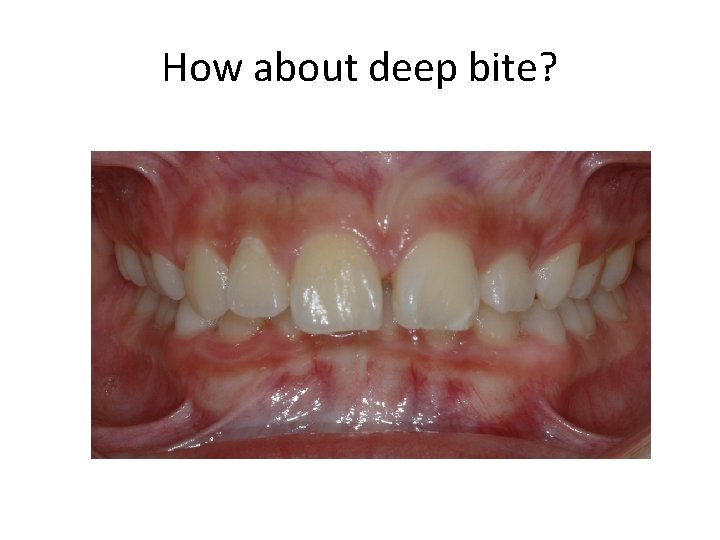
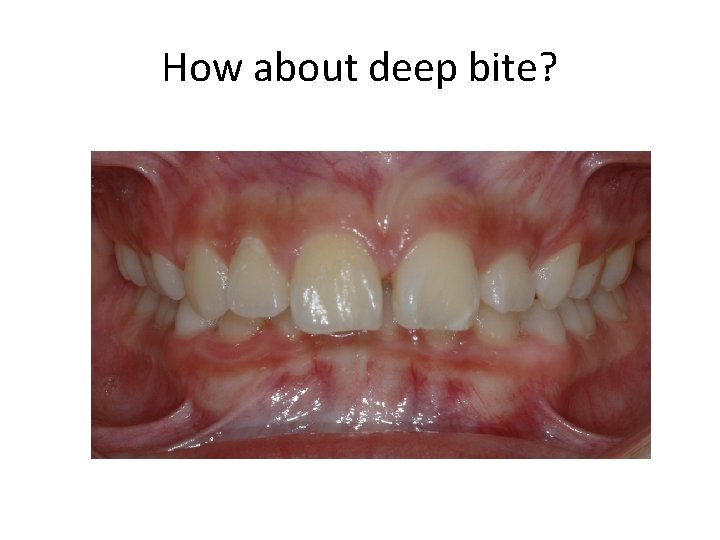
How about deep bite?
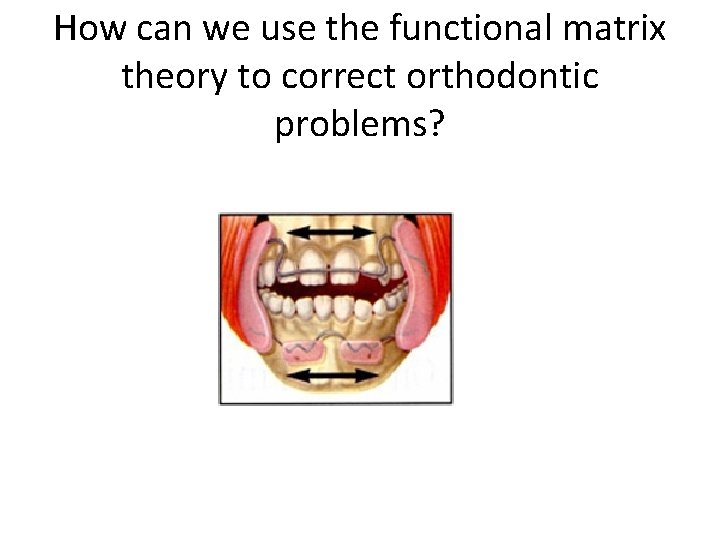
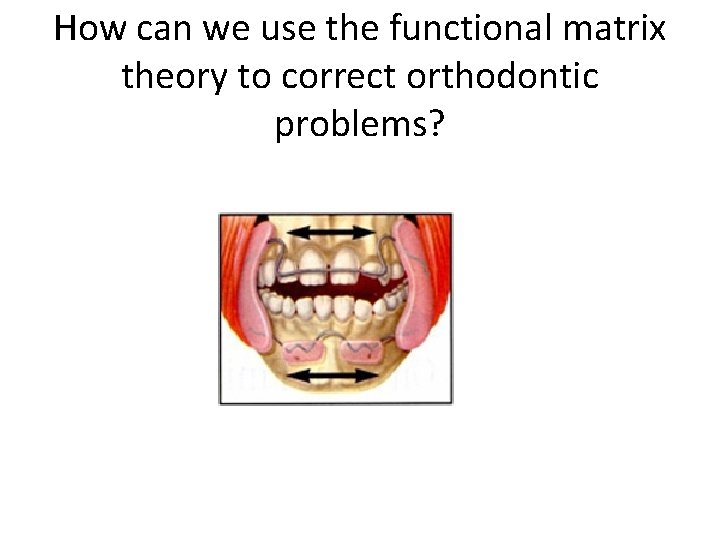
How can we use the functional matrix theory to correct orthodontic problems?
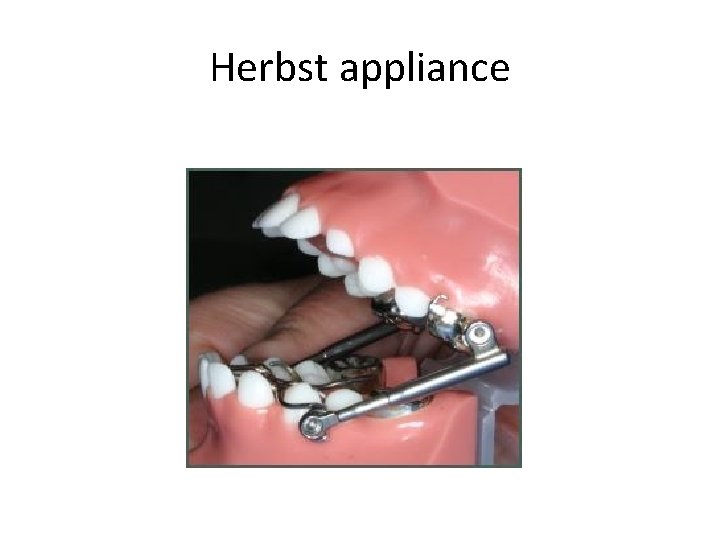
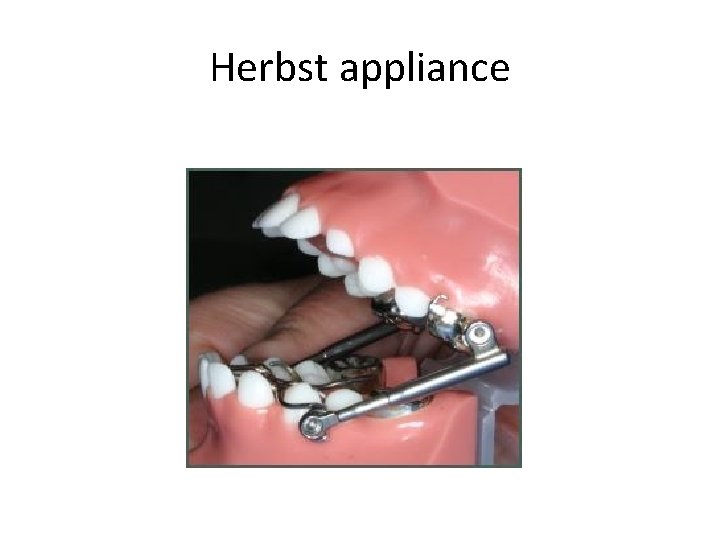
Herbst appliance
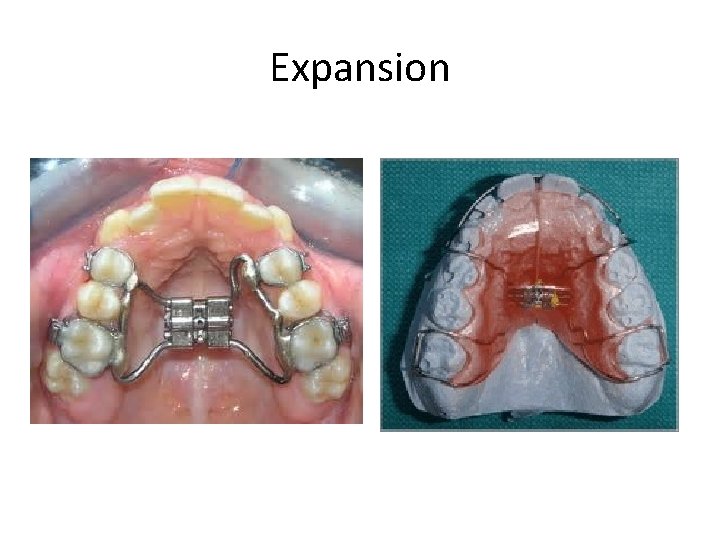
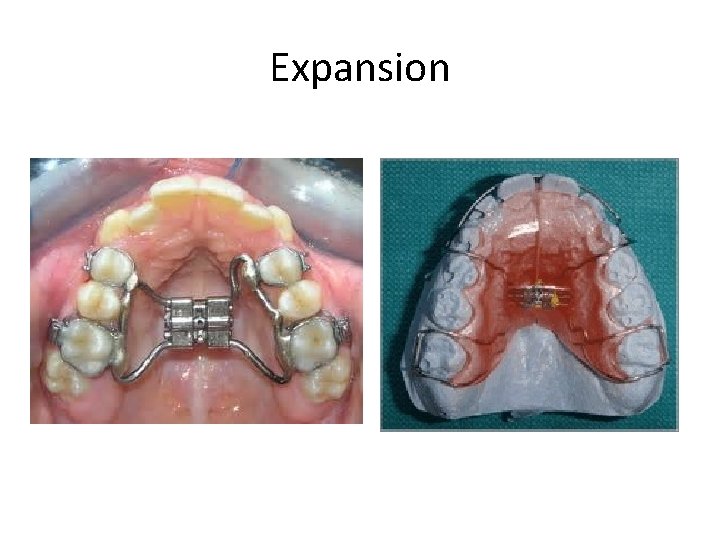
Expansion
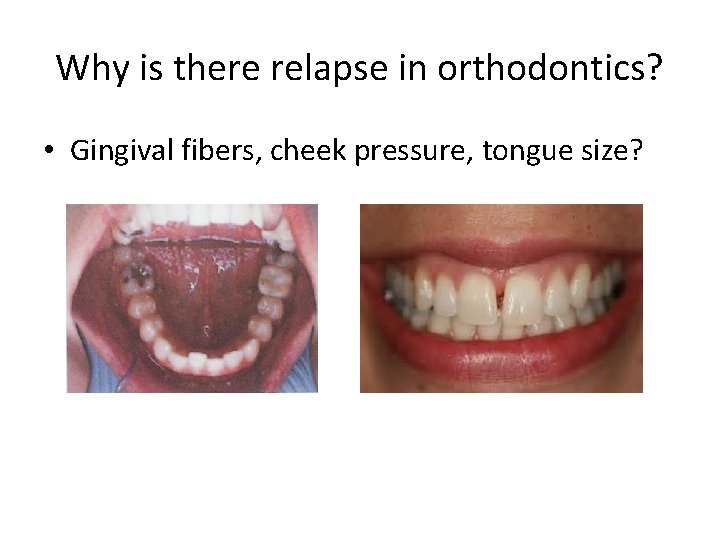
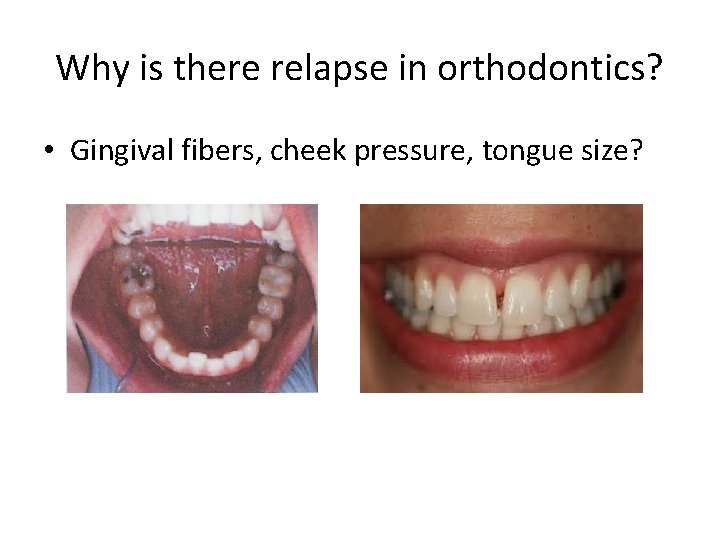
Why is there relapse in orthodontics? • Gingival fibers, cheek pressure, tongue size?
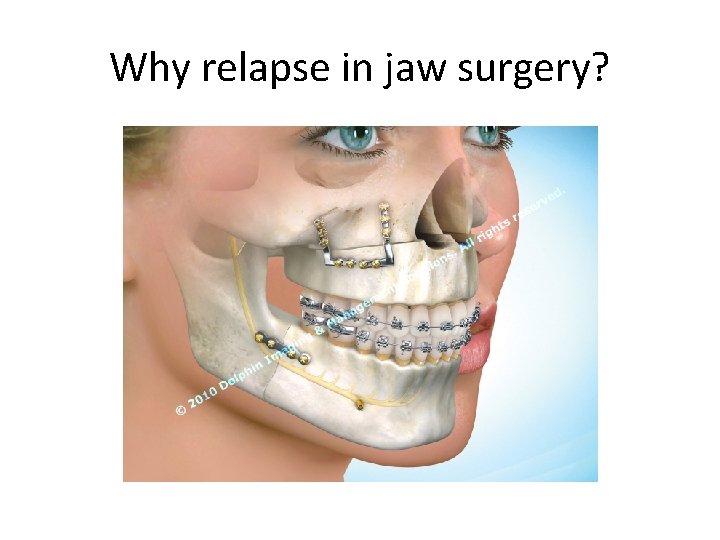
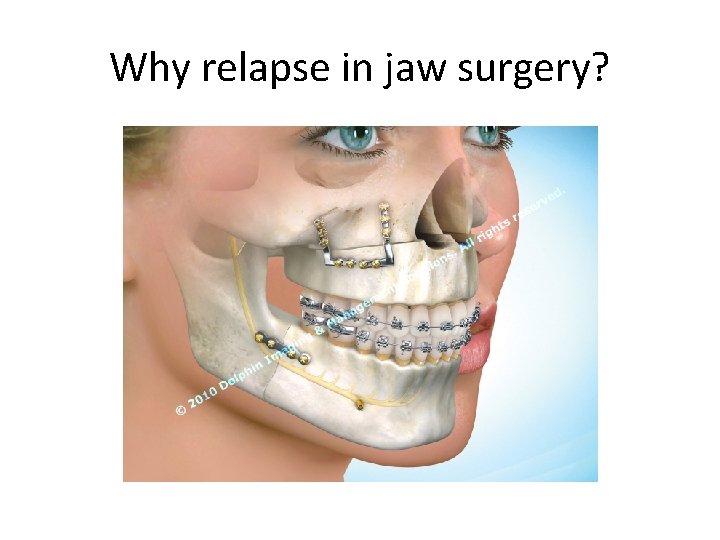
Why relapse in jaw surgery?

Form follows function
 詹景裕
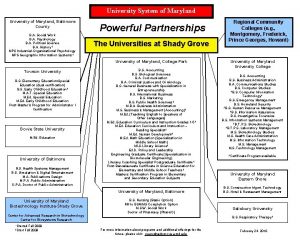
詹景裕 University of maryland observatory
University of maryland observatory University of maryland capital region health medical group
University of maryland capital region health medical group University of maryland hci
University of maryland hci University of maryland
University of maryland University of maryland
University of maryland University of maryland observatory
University of maryland observatory Insideloyola
Insideloyola Juliet aiken university of maryland
Juliet aiken university of maryland Medscope university of maryland
Medscope university of maryland Relative growth rate equation
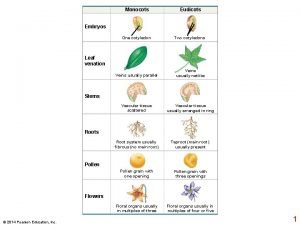
Relative growth rate equation Monocot vs eudicot
Monocot vs eudicot Primary growth and secondary growth in plants
Primary growth and secondary growth in plants Primary growth and secondary growth in plants
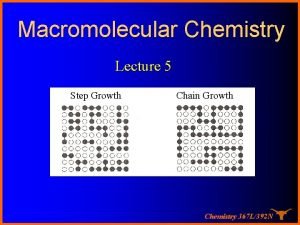
Primary growth and secondary growth in plants Growthchain
Growthchain Geometric vs exponential growth
Geometric vs exponential growth Neoclassical growth theory vs. endogenous growth theory
Neoclassical growth theory vs. endogenous growth theory Organic growth vs inorganic growth
Organic growth vs inorganic growth Stages of human growth and development pictures
Stages of human growth and development pictures What are the theories of growth and development
What are the theories of growth and development Human growth and development
Human growth and development Emotional changes in childhood
Emotional changes in childhood Pretest growth development and sexuality
Pretest growth development and sexuality Maturation development
Maturation development Stages of developmetn
Stages of developmetn Stages of growth and development from infancy to adulthood
Stages of growth and development from infancy to adulthood Growth and development conclusion
Growth and development conclusion Domain 7 personal growth and professional development
Domain 7 personal growth and professional development Growth and development pictures
Growth and development pictures Middle childhood growth and development
Middle childhood growth and development Distinguish between growth and development
Distinguish between growth and development