For internal use only Overview This Training Sheet
- Slides: 10
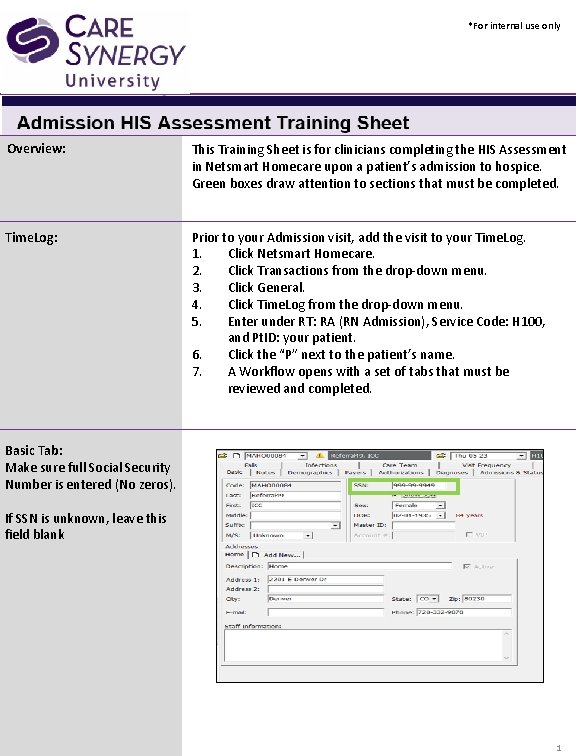
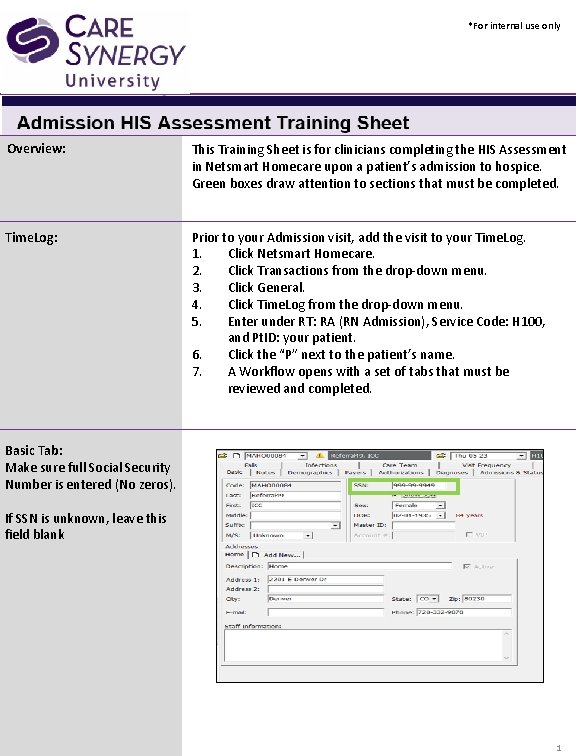
*For internal use only Overview: This Training Sheet is for clinicians completing the HIS Assessment in Netsmart Homecare upon a patient’s admission to hospice. Green boxes draw attention to sections that must be completed. Time. Log: Prior to your Admission visit, add the visit to your Time. Log. 1. Click Netsmart Homecare. 2. Click Transactions from the drop-down menu. 3. Click General. 4. Click Time. Log from the drop-down menu. 5. Enter under RT: RA (RN Admission), Service Code: H 100, and Pt. ID: your patient. 6. Click the “P” next to the patient’s name. 7. A Workflow opens with a set of tabs that must be reviewed and completed. Basic Tab: Make sure full Social Security Number is entered (No zeros). If SSN is unknown, leave this field blank 1
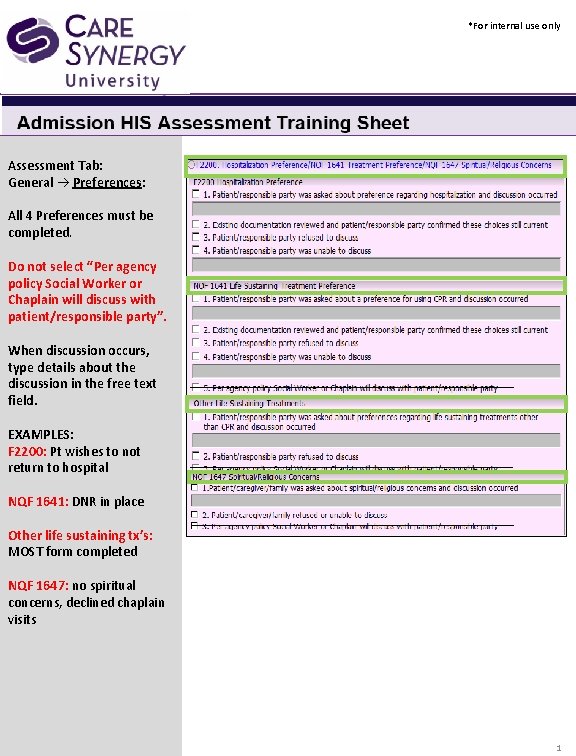
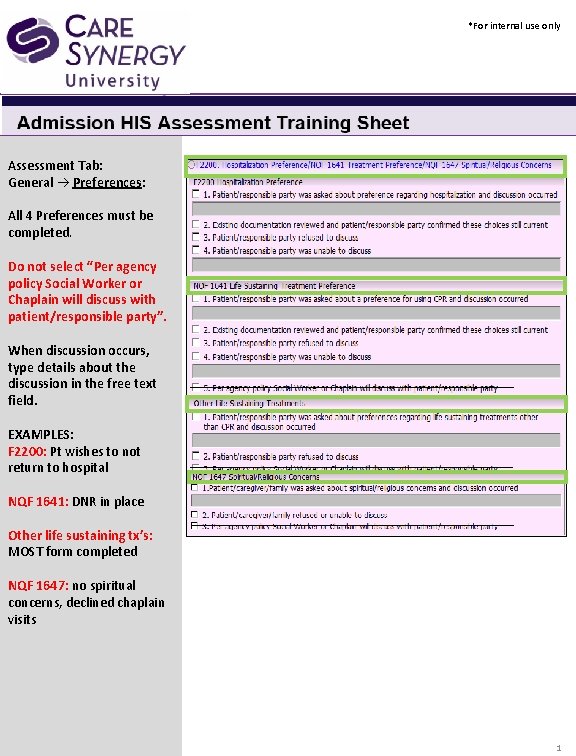
*For internal use only Assessment Tab: General Preferences: All 4 Preferences must be completed. Do not select “Per agency policy Social Worker or Chaplain will discuss with patient/responsible party”. When discussion occurs, type details about the discussion in the free text field. EXAMPLES: F 2200: Pt wishes to not return to hospital NQF 1641: DNR in place Other life sustaining tx’s: MOST form completed NQF 1647: no spiritual concerns, declined chaplain visits 1
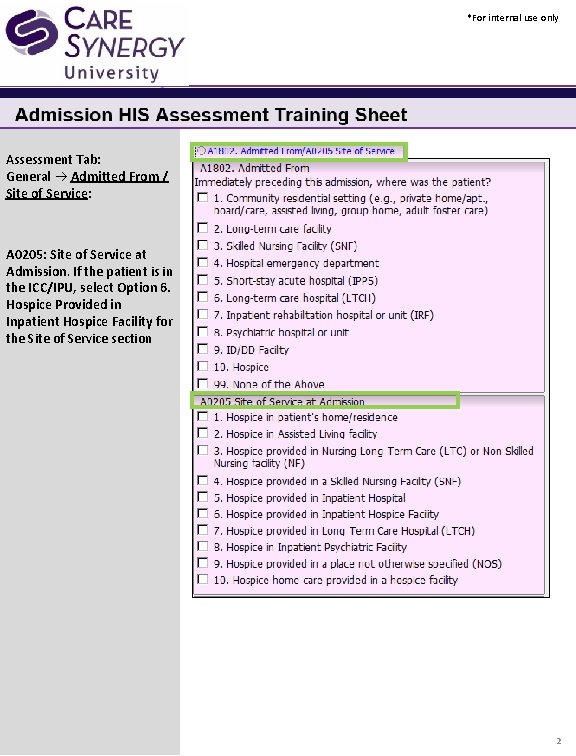
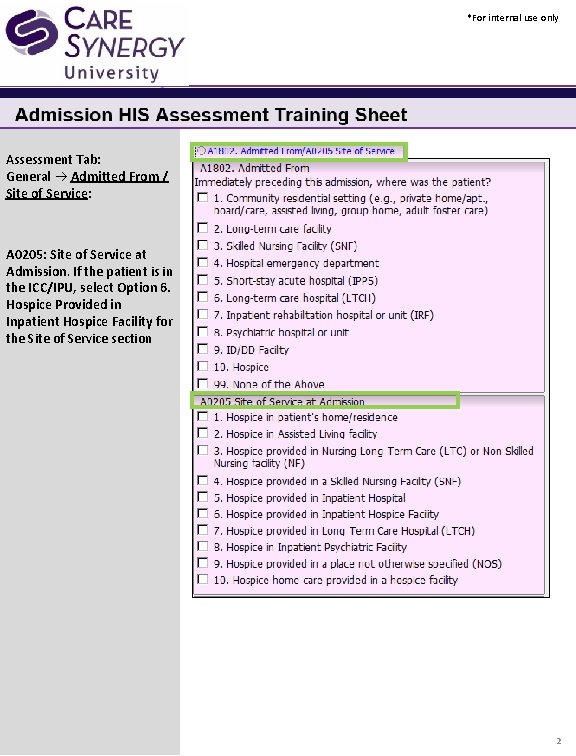
*For internal use only Assessment Tab: General Admitted From / Site of Service: A 0205: Site of Service at Admission. If the patient is in the ICC/IPU, select Option 6. Hospice Provided in Inpatient Hospice Facility for the Site of Service section 2
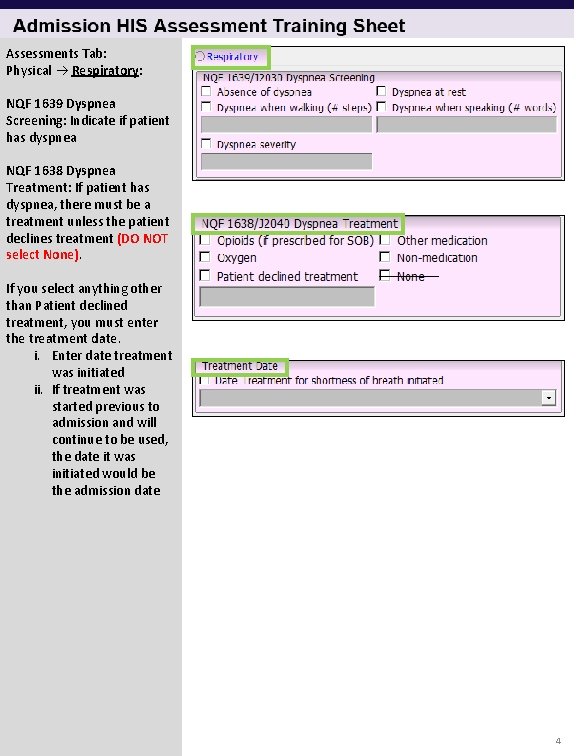
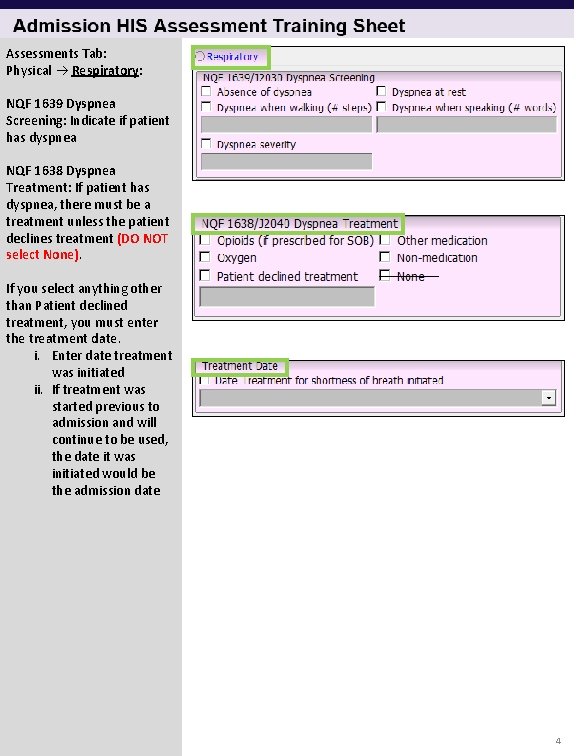
Assessments Tab: Physical Respiratory: NQF 1639 Dyspnea Screening: Indicate if patient has dyspnea NQF 1638 Dyspnea Treatment: If patient has dyspnea, there must be a treatment unless the patient declines treatment (DO NOT select None). If you select anything other than Patient declined treatment, you must enter the treatment date. i. Enter date treatment was initiated ii. If treatment was started previous to admission and will continue to be used, the date it was initiated would be the admission date 4
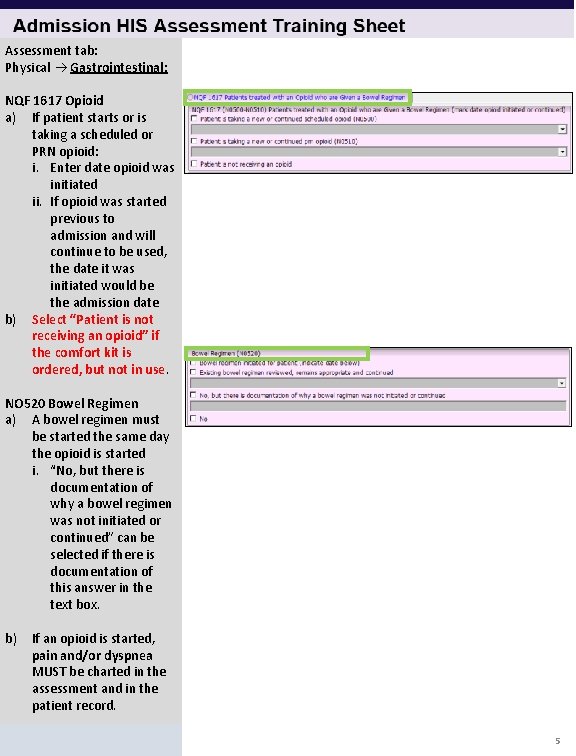
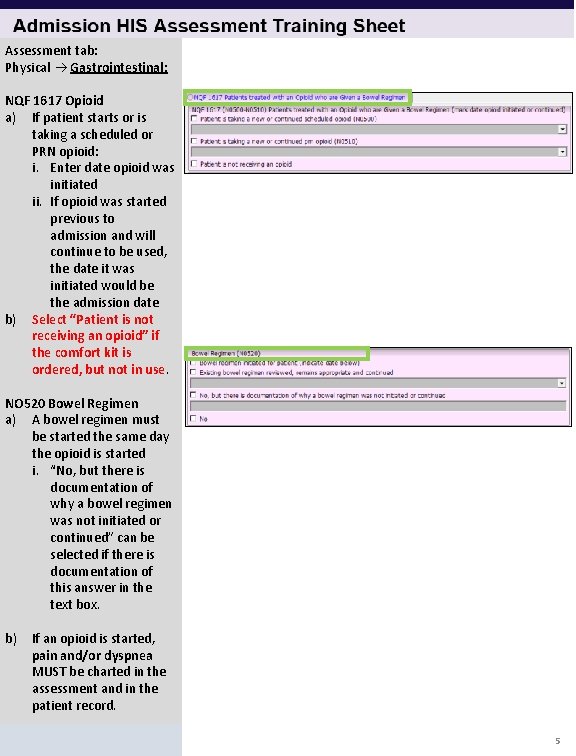
Assessment tab: Physical Gastrointestinal: NQF 1617 Opioid a) If patient starts or is taking a scheduled or PRN opioid: i. Enter date opioid was initiated ii. If opioid was started previous to admission and will continue to be used, the date it was initiated would be the admission date b) Select “Patient is not receiving an opioid” if the comfort kit is ordered, but not in use. NO 520 Bowel Regimen a) A bowel regimen must be started the same day the opioid is started i. “No, but there is documentation of why a bowel regimen was not initiated or continued” can be selected if there is documentation of this answer in the text box. b) If an opioid is started, pain and/or dyspnea MUST be charted in the assessment and in the patient record. 5
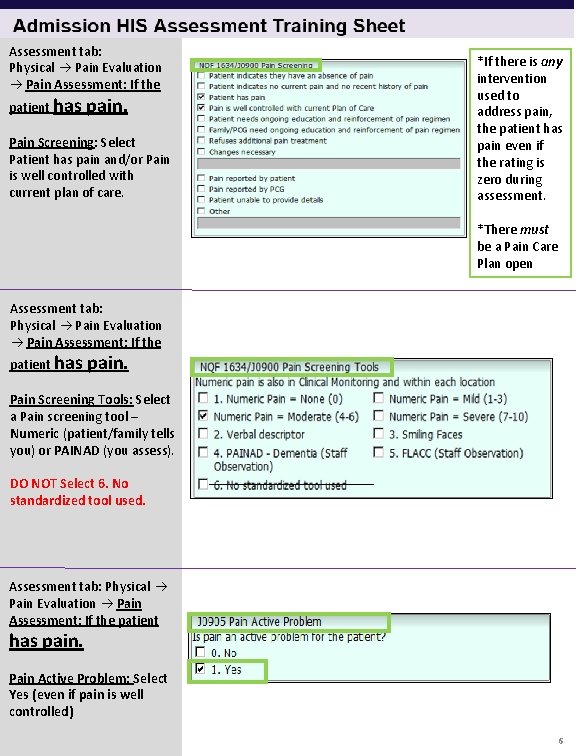
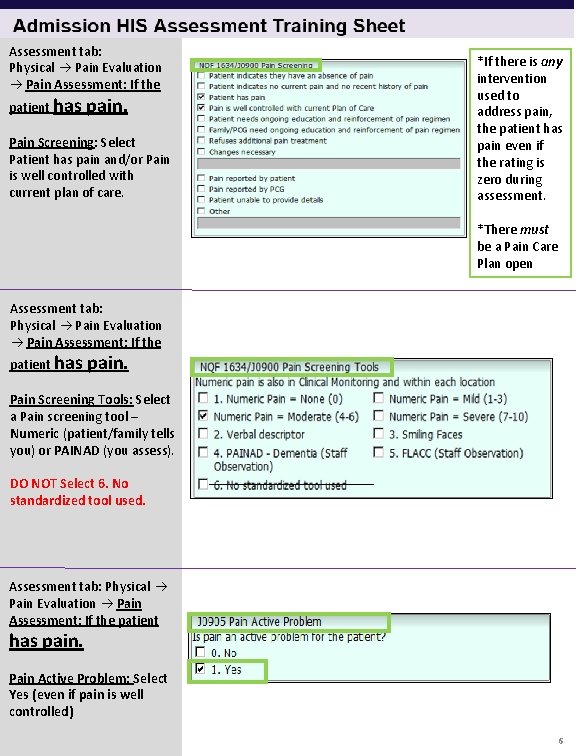
Assessment tab: Physical Pain Evaluation Pain Assessment: If the patient has pain. Pain Screening: Select Patient has pain and/or Pain is well controlled with current plan of care. *If there is any intervention used to address pain, the patient has pain even if the rating is zero during assessment. *There must be a Pain Care Plan open Assessment tab: Physical Pain Evaluation Pain Assessment: If the patient has pain. Pain Screening Tools: Select a Pain screening tool – Numeric (patient/family tells you) or PAINAD (you assess). DO NOT Select 6. No standardized tool used. Assessment tab: Physical Pain Evaluation Pain Assessment: If the patient has pain. Pain Active Problem: Select Yes (even if pain is well controlled) 6
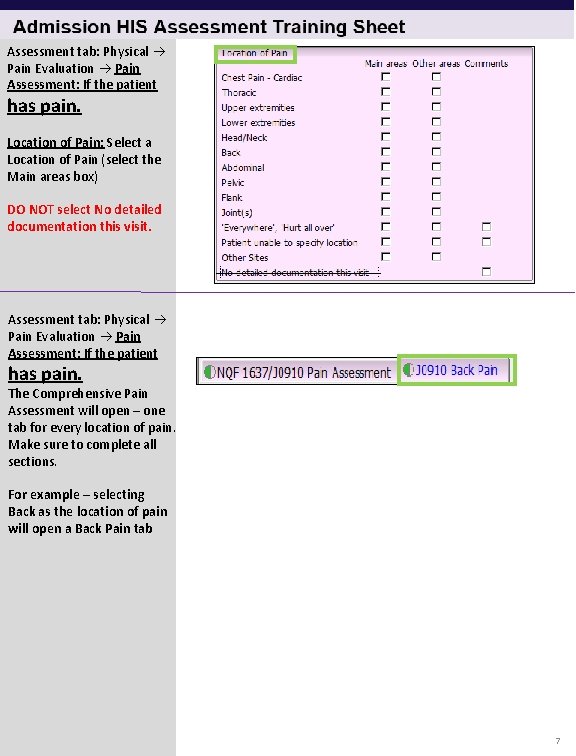
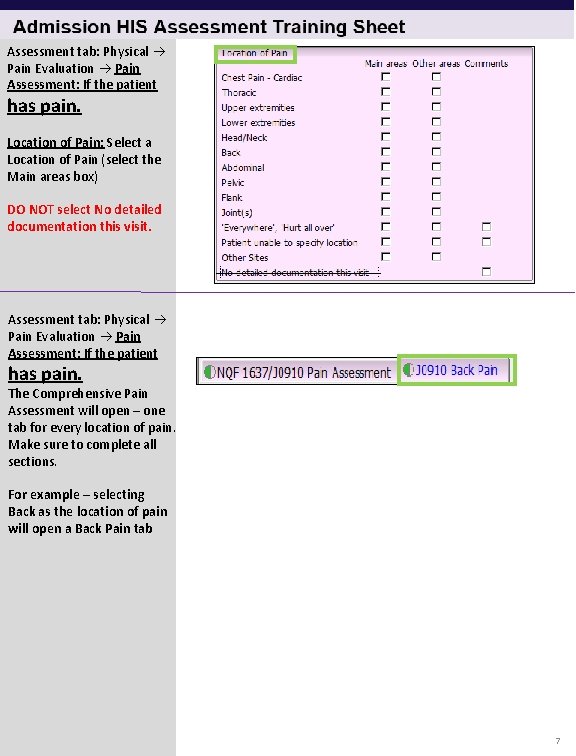
Assessment tab: Physical Pain Evaluation Pain Assessment: If the patient has pain. Location of Pain: Select a Location of Pain (select the Main areas box) DO NOT select No detailed documentation this visit. Assessment tab: Physical Pain Evaluation Pain Assessment: If the patient has pain. The Comprehensive Pain Assessment will open – one tab for every location of pain. Make sure to complete all sections. For example – selecting Back as the location of pain will open a Back Pain tab 7
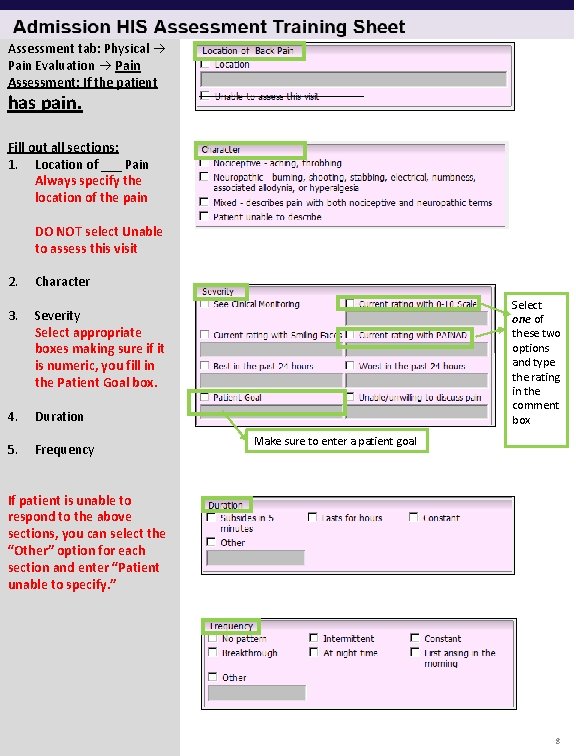
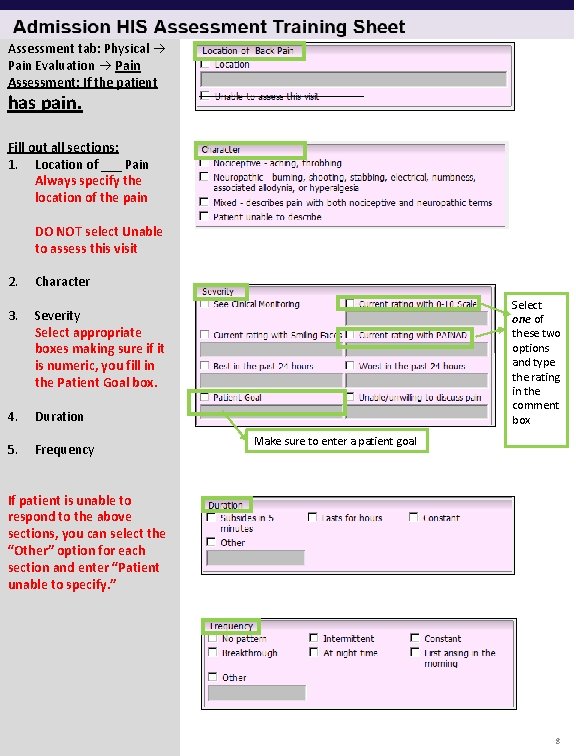
Assessment tab: Physical Pain Evaluation Pain Assessment: If the patient has pain. Fill out all sections: 1. Location of ___ Pain Always specify the location of the pain DO NOT select Unable to assess this visit 2. Character 3. Severity Select appropriate boxes making sure if it is numeric, you fill in the Patient Goal box. 4. Duration 5. Frequency Select one of these two options and type the rating in the comment box Make sure to enter a patient goal If patient is unable to respond to the above sections, you can select the “Other” option for each section and enter “Patient unable to specify. ” 8
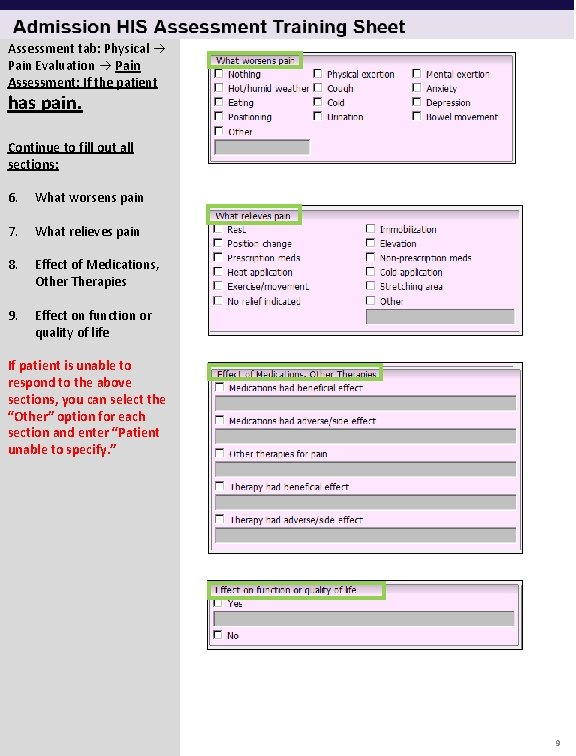
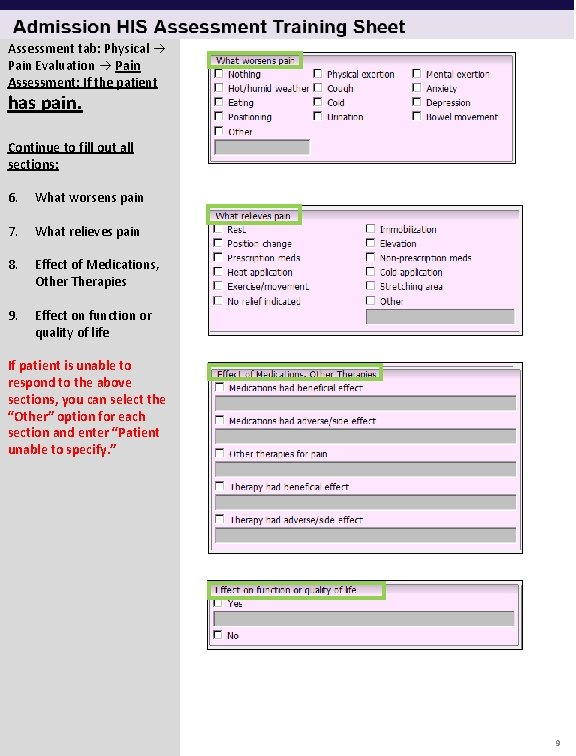
Assessment tab: Physical Pain Evaluation Pain Assessment: If the patient has pain. Continue to fill out all sections: 6. What worsens pain 7. What relieves pain 8. Effect of Medications, Other Therapies 9. Effect on function or quality of life If patient is unable to respond to the above sections, you can select the “Other” option for each section and enter “Patient unable to specify. ” 9
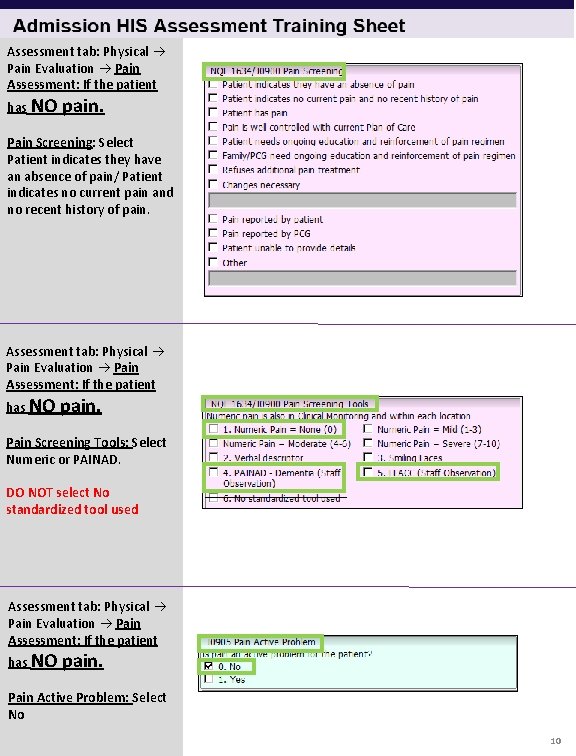
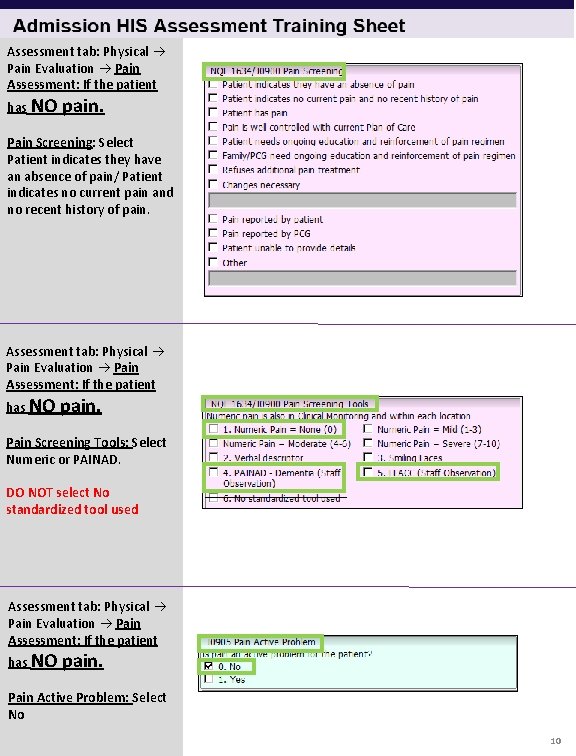
Assessment tab: Physical Pain Evaluation Pain Assessment: If the patient has NO pain. Pain Screening: Select Patient indicates they have an absence of pain/ Patient indicates no current pain and no recent history of pain. Assessment tab: Physical Pain Evaluation Pain Assessment: If the patient has NO pain. Pain Screening Tools: Select Numeric or PAINAD. DO NOT select No standardized tool used Assessment tab: Physical Pain Evaluation Pain Assessment: If the patient has NO pain. Pain Active Problem: Select No 10