Family living conditions maternal employment conditions and health




- Slides: 18
Family living conditions, maternal employment conditions, and health care access experiences: Are these factors associated with childhood vaccination coverage? Karen G. Wooten MA Immunization Services Division, NCIRD
Background • Persistent racial disparity and poverty disparity in childhood vaccination • Racial disparity can be controlled by factors associated with household income • Socioeconomic Status Module (SES) was added to the NIS in January- June 2008.

Methods • 2008 National Immunization Survey (NIS)– List-Assisted Random Digit Dialed (RDD) Telephone Survey – Children between 19 and 35 months of age – Includes a mailed survey to children’s vaccination providers – Weighted to account for non-telephone households and provider non-response – Response rate: 63. 2% – Children born January 2005 – June 2007
Methods (analytic) • Analyses conducted using SUDAAN Software Package – Survey analysis tool for complex sample survey data • Tests of Significance – Wald Chi Square test (logistic regression): • Significance levels p<0. 10 and p<0. 05 – Modeling… • Identify factors associated with childhood vaccination • Evaluate effects of predictive variables among race/ethnic groups and poverty groups. • 4: 3: 1: 3: 3: 1 vaccine series • Sample size= 7, 159 children

Results
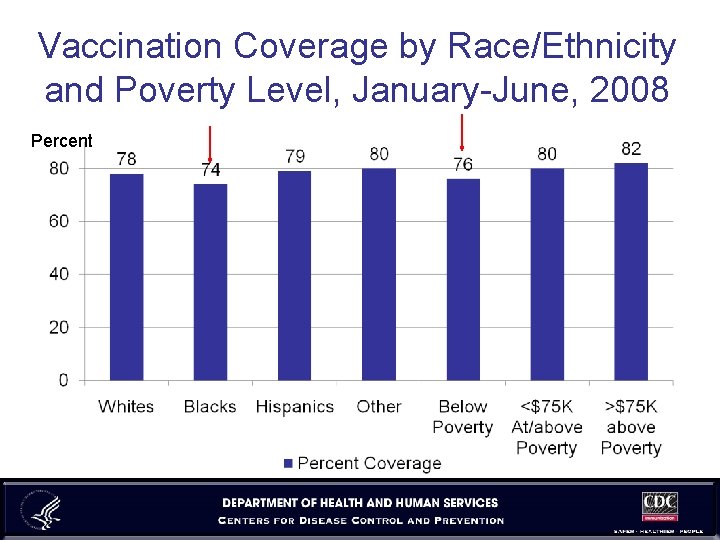
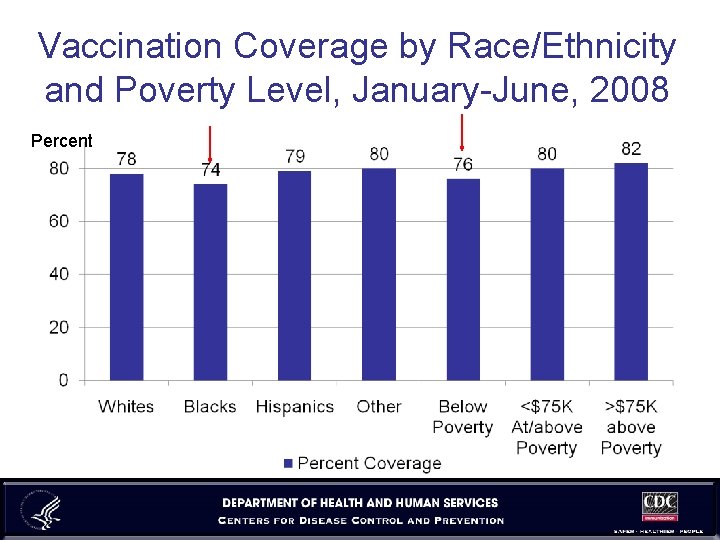
Vaccination Coverage by Race/Ethnicity and Poverty Level, January-June, 2008 Percent
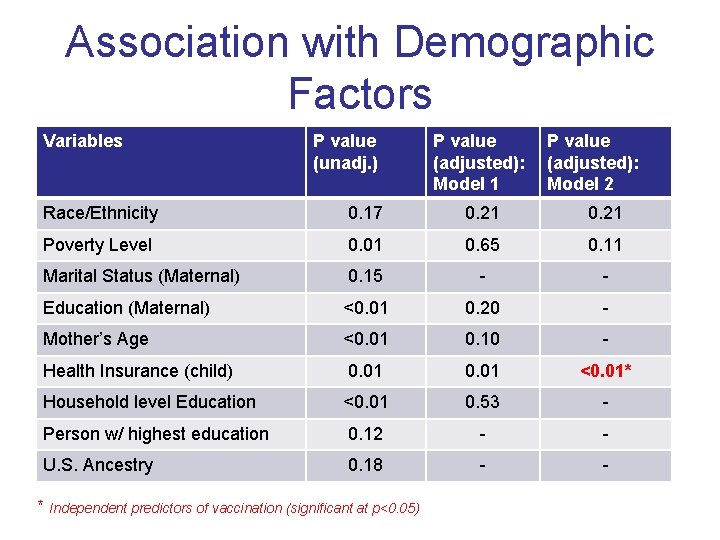
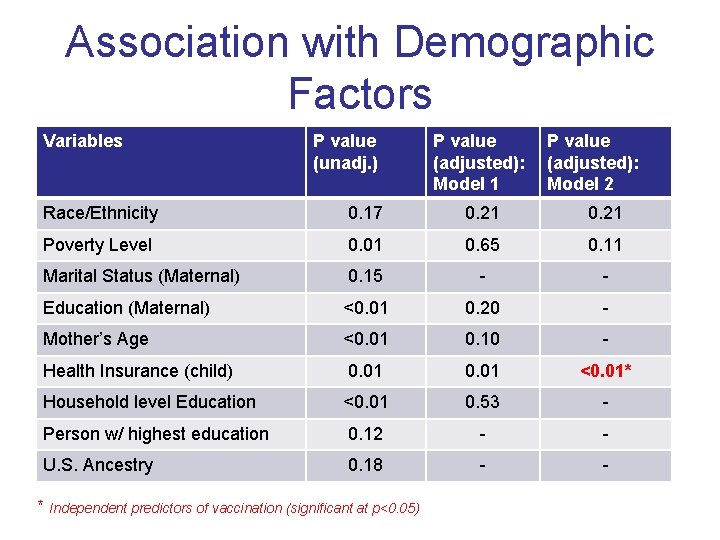
Association with Demographic Factors Variables P value (unadj. ) P value (adjusted): Model 1 P value (adjusted): Model 2 Race/Ethnicity 0. 17 0. 21 Poverty Level 0. 01 0. 65 0. 11 Marital Status (Maternal) 0. 15 - - Education (Maternal) <0. 01 0. 20 - Mother’s Age <0. 01 0. 10 - Health Insurance (child) 0. 01 <0. 01* Household level Education <0. 01 0. 53 - Person w/ highest education 0. 12 - - U. S. Ancestry 0. 18 - - * Independent predictors of vaccination (significant at p<0. 05)
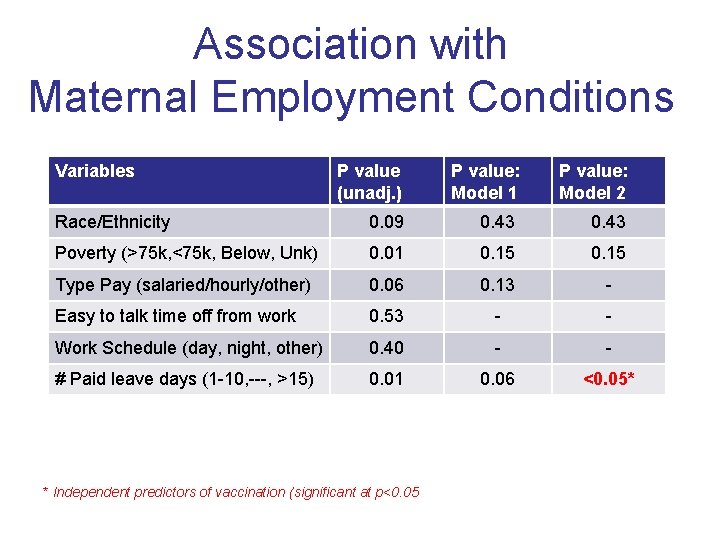
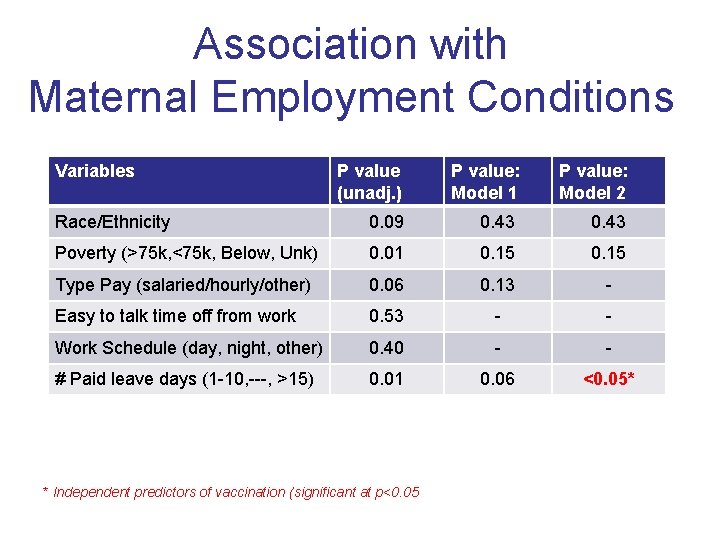
Association with Maternal Employment Conditions Variables P value (unadj. ) P value: Model 1 P value: Model 2 Race/Ethnicity 0. 09 0. 43 Poverty (>75 k, <75 k, Below, Unk) 0. 01 0. 15 Type Pay (salaried/hourly/other) 0. 06 0. 13 - Easy to talk time off from work 0. 53 - - Work Schedule (day, night, other) 0. 40 - - # Paid leave days (1 -10, ---, >15) 0. 01 0. 06 <0. 05* * Independent predictors of vaccination (significant at p<0. 05
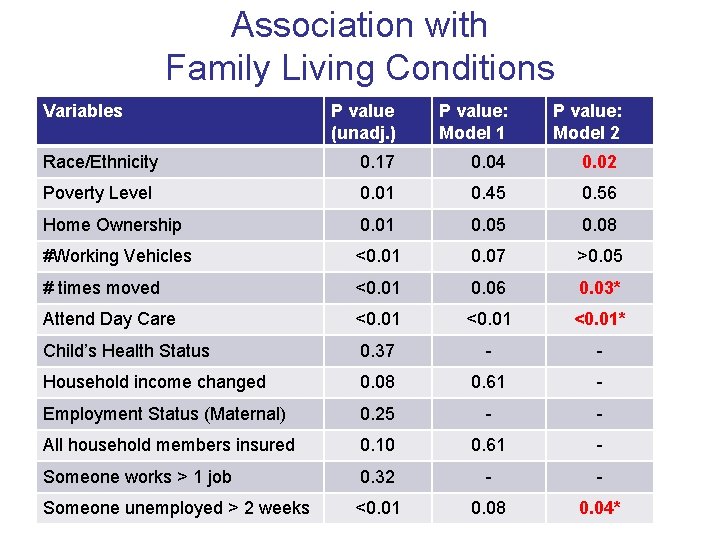
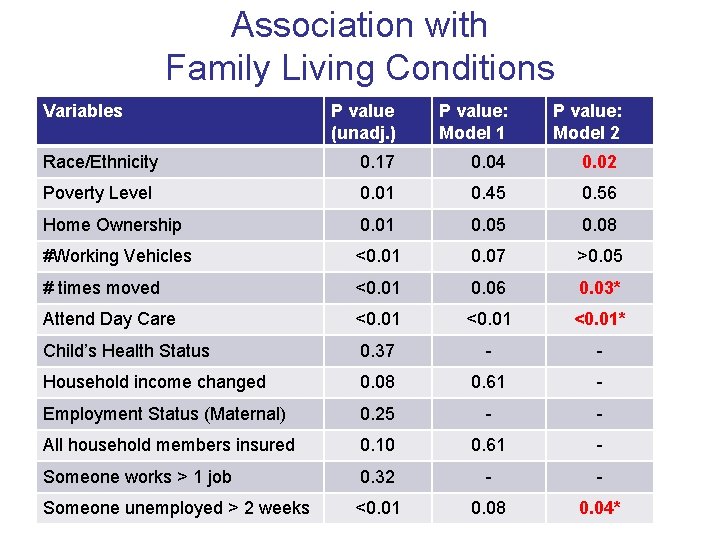
Association with Family Living Conditions Variables P value (unadj. ) P value: Model 1 P value: Model 2 Race/Ethnicity 0. 17 0. 04 0. 02 Poverty Level 0. 01 0. 45 0. 56 Home Ownership 0. 01 0. 05 0. 08 #Working Vehicles <0. 01 0. 07 >0. 05 # times moved <0. 01 0. 06 0. 03* Attend Day Care <0. 01* Child’s Health Status 0. 37 - - Household income changed 0. 08 0. 61 - Employment Status (Maternal) 0. 25 - - All household members insured 0. 10 0. 61 - Someone works > 1 job 0. 32 - - Someone unemployed > 2 weeks <0. 01 0. 08 0. 04*

Association with Access to Immunization Services Variables P value (unadj. ) P value (adj. **) Race/Ethnicity 0. 17 0. 03 0. 02 Poverty Level 0. 01 0. 26 0. 22 All household members insured 0. 10 0. 99 - Has regular/routine doctor <0. 01 - - Travel time to doctor’s office 0. 67 - - Has had to cancel child’s dr. appt. <0. 01* Able to get dr. appt. when needed <0. 01 0. 06 Doctor spends enough time w/ child 0. 26 - - Doctor explains things clearly 0. 03 0. 07 Wait time in exam room <0. 01 0. 04* Ever vaccinated at P. H. clinic <0. 01 0. 09 Ever refused/delayed a vaccine <0. 01*
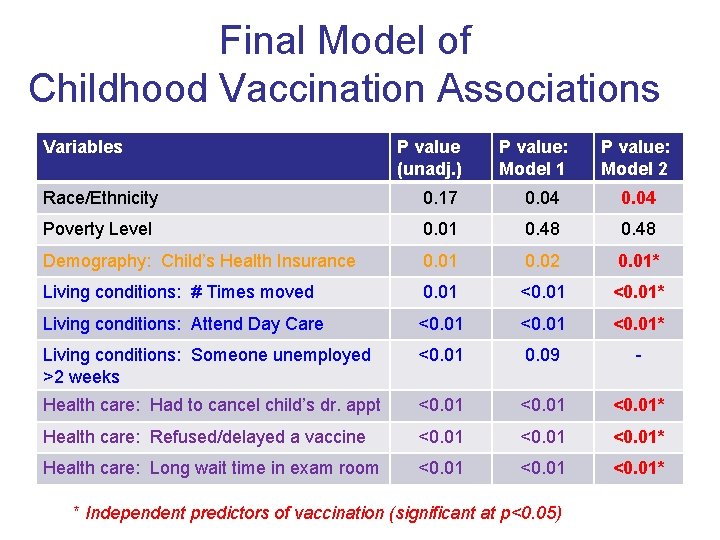
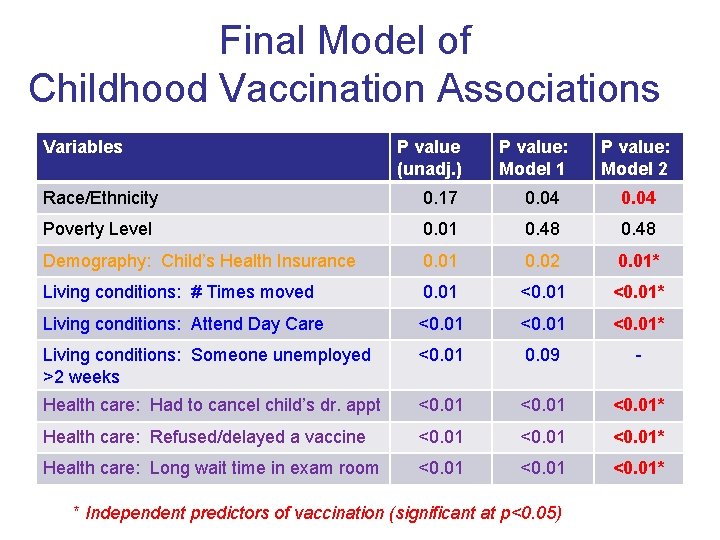
Final Model of Childhood Vaccination Associations Variables P value (unadj. ) P value: Model 1 P value: Model 2 Race/Ethnicity 0. 17 0. 04 Poverty Level 0. 01 0. 48 Demography: Child’s Health Insurance 0. 01 0. 02 0. 01* Living conditions: # Times moved 0. 01 <0. 01* Living conditions: Attend Day Care <0. 01* Living conditions: Someone unemployed >2 weeks <0. 01 0. 09 - Health care: Had to cancel child’s dr. appt <0. 01* Health care: Refused/delayed a vaccine <0. 01* Health care: Long wait time in exam room <0. 01* * Independent predictors of vaccination (significant at p<0. 05)

Children of working mothers: Childhood Vaccination Associations Variables P value (unadj. ) P value: Model 1 P value: Model 2 Race/Ethnicity 0. 17 0. 50 0. 71 Poverty Level 0. 01 0. 90 0. 76 Demography: Child’s health insurance 0. 01 0. 50 - Maternal employment: Paid Leave 0. 01 0. 03 Living conditions: # Times moved 0. 01 0. 02 <0. 01* Living conditions: Attend Day Care <0. 01 0. 08 - Living conditions: Someone unemployed >2 weeks <0. 01 0. 11 - Health care: Had to cancel child’s dr. appt <0. 01 0. 12 - Health care: Refused/delayed a vaccine <0. 01 <0. 05 0. 03* Health care: Long wait time in exam room <0. 01 0. 30 -
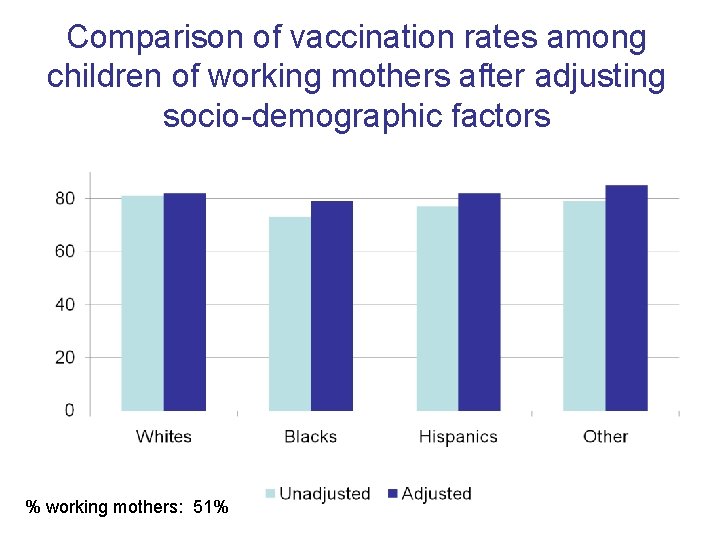
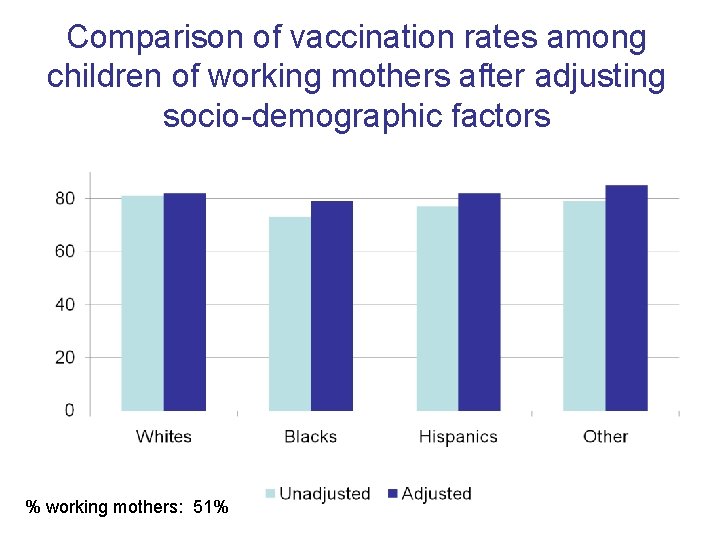
Comparison of vaccination rates among children of working mothers after adjusting socio-demographic factors % working mothers: 51%
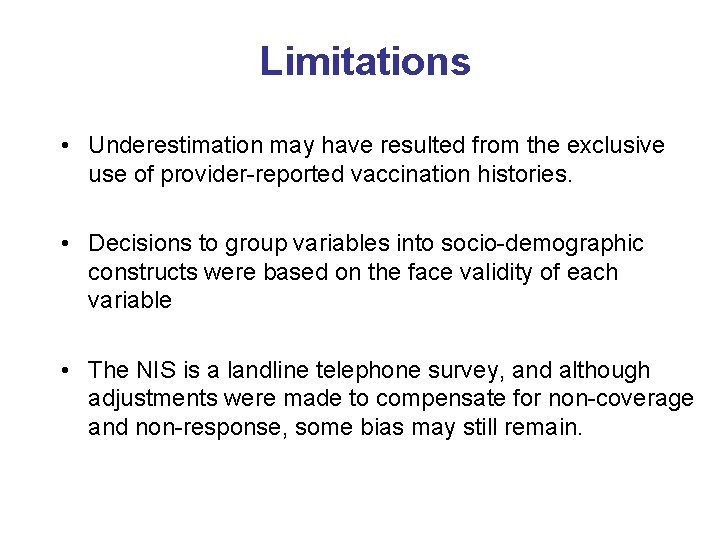
Limitations • Underestimation may have resulted from the exclusive use of provider-reported vaccination histories. • Decisions to group variables into socio-demographic constructs were based on the face validity of each variable • The NIS is a landline telephone survey, and although adjustments were made to compensate for non-coverage and non-response, some bias may still remain.
Conclusions (1) • Among demographic factors, health insurance may be the single most important factor in eliminating racial and poverty disparities in childhood vaccination. • Other factors that may be important predictors of vaccination coverage include family living conditions and experiences in accessing to childhood immunization services: – – – Day care attendance Movement since child’s birth Need to cancel a child’s doctor appointment Delaying or refusing a recommended vaccine Experiencing long waits in the examination room
Conclusions (2) • The likelihood of vaccination increases among children of working mothers if mothers … – Had access to paid leave – Are able to stay in the same home where child was first born – Do not have to delay or refuse one of the recommended vaccines • There is no ‘silver bullet’ to eliminating racial and poverty disparities in vaccination coverage. • It’s complicated… – These data confirm that there are many factors to consider to increase vaccination coverage among all children. – More efforts are needed to make it easier for families to carry out their decisions to vaccinate their children.
Acknowledgements • SES working group members (2004 -2005): – – – • • Lawrence Barker, Ph. D (NCCDPHP) Susan Chu, Ph. D (NCCDPHP) Marcie Cynamon, MS, (NCHS) Maureen Kolasa, MPH (NCIRD) Elizabeth Luman, Ph. D (NCIRD) Marilyn Meltzer, MPH (NCCDPHP) Mark Messonnier, Ph. D (NCIRD) Jeannie Santoli, MD (NCIRD) Phil Smith, Ph. D (NCIRD) John Stevenson, MA (NCIRD) Shannon Stokley, MPH (NCIRD) Karen Wooten, MA (NCIRD) NIS operations working group (includes NORC management team) Qian Li, BS (data analyses assistance)
Contact Information Karen Wooten, MA Health Scientist Kwooten@cdc. gov 404 639 -8343 National Centers for Disease Control and Prevention National Center for Immunization and Respiratory Diseases Immunization Services Division 1600 Clifton Road E 62 Atlanta, GA 30329
 Mitochondria non examples
Mitochondria non examples Extranuclear inheritance
Extranuclear inheritance History of maternal and child health
History of maternal and child health Mch indicators full form
Mch indicators full form Jama 2017
Jama 2017 Factors influencing maternal health
Factors influencing maternal health What is maternal health
What is maternal health Blue things
Blue things Living and working conditions in australia 1900
Living and working conditions in australia 1900 Is moss living or non-living
Is moss living or non-living Living non living dead
Living non living dead Smallest living unit of life
Smallest living unit of life National programs
National programs Prophase
Prophase Maternal and child malnutrition
Maternal and child malnutrition Chapter 15 maternal and fetal nutrition
Chapter 15 maternal and fetal nutrition Maternal pelvis and fetal skull
Maternal pelvis and fetal skull Asynclitic
Asynclitic Normal labour
Normal labour