FAME 2 Trial Results and Lessons Learned William
- Slides: 37
FAME 2 Trial: Results and Lessons Learned William F. Fearon, MD Associate Professor of Medicine Director, Interventional Cardiology Stanford University Medical Center
William Fearon, MD Grant Support: St. Jude Medical, Inc.
FAME 2 n The trial and results…
FAME 2: Design n Hypothesis: q Optimal medical therapy plus FFR-guided PCI improves outcomes compared to optimal medical therapy alone in patients with stable coronary artery disease. De Bruyne, et al. New Engl J Med 2012; 367: 991 -1001
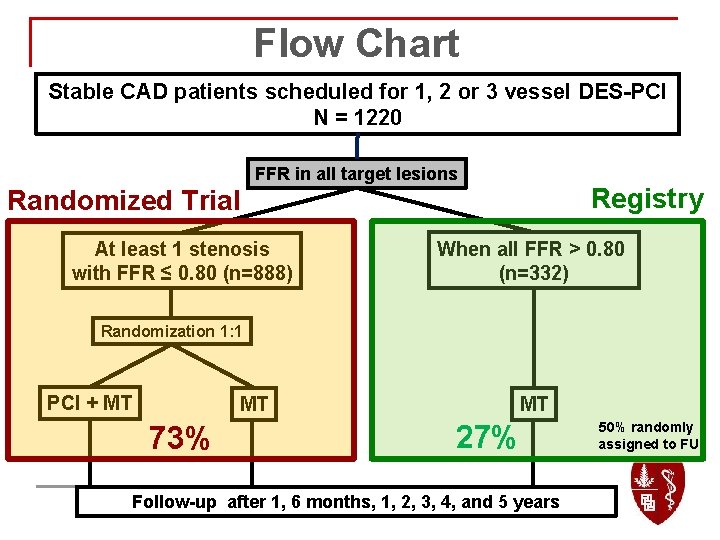
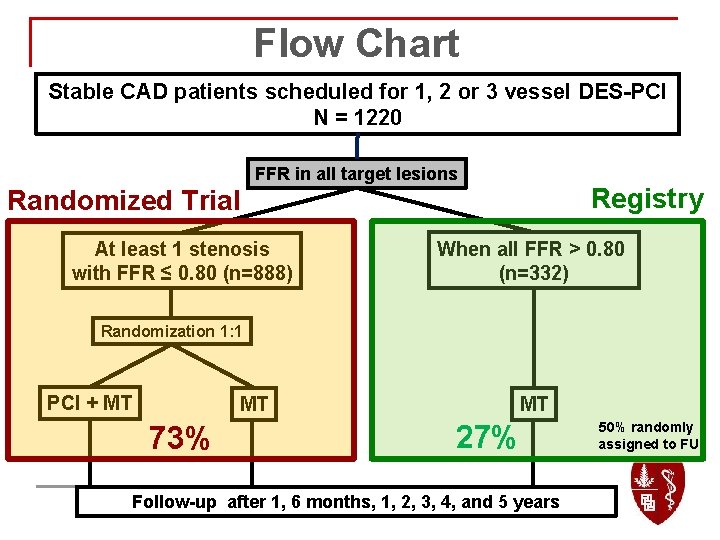
Flow Chart Stable CAD patients scheduled for 1, 2 or 3 vessel DES-PCI N = 1220 FFR in all target lesions Registry Randomized Trial At least 1 stenosis with FFR ≤ 0. 80 (n=888) When all FFR > 0. 80 (n=332) Randomization 1: 1 PCI + MT MT 73% MT 27% Follow-up after 1, 6 months, 1, 2, 3, 4, and 5 years 50% randomly assigned to FU
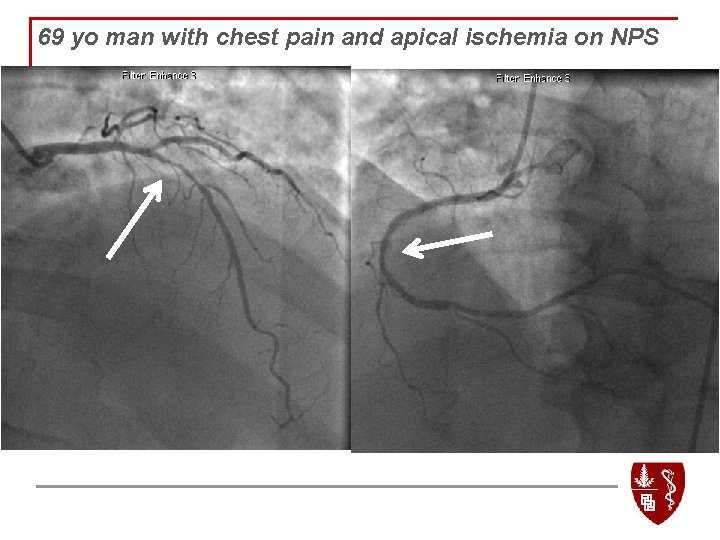
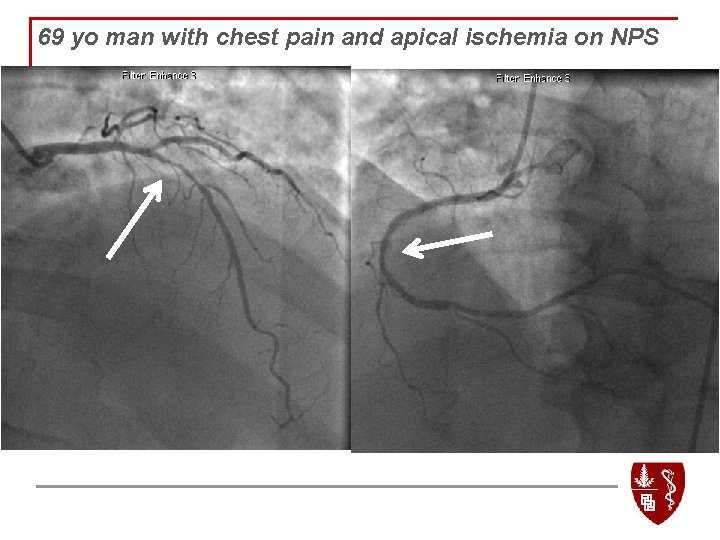
69 yo man with chest pain and apical ischemia on NPS
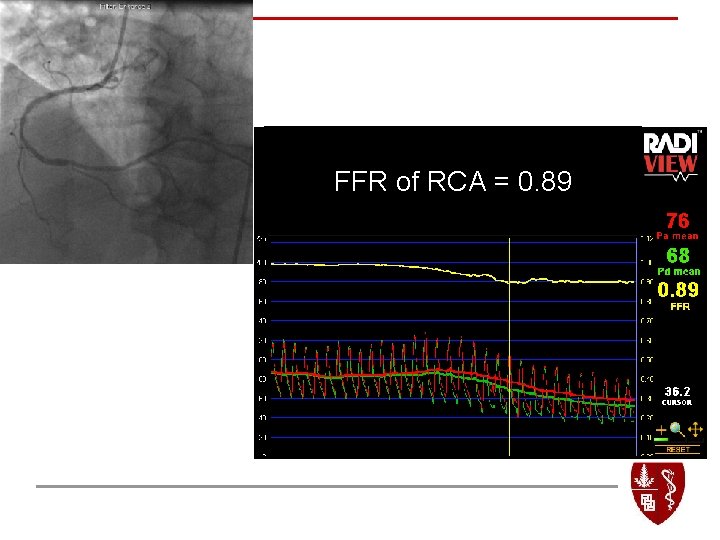
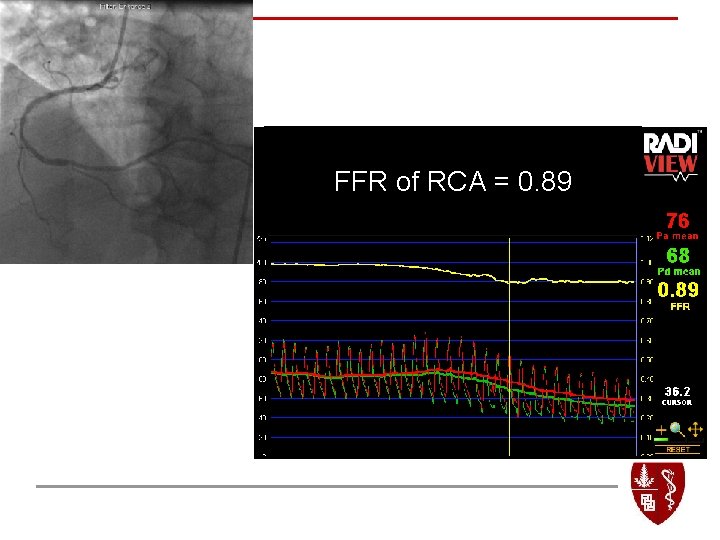
FFR of RCA = 0. 89
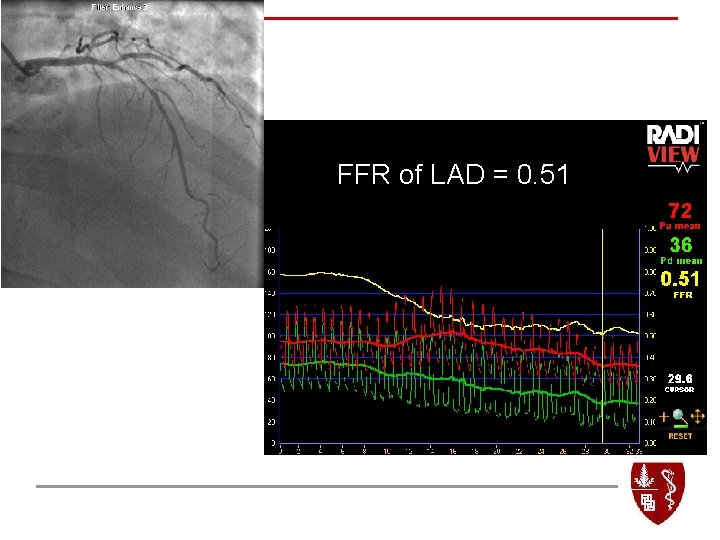
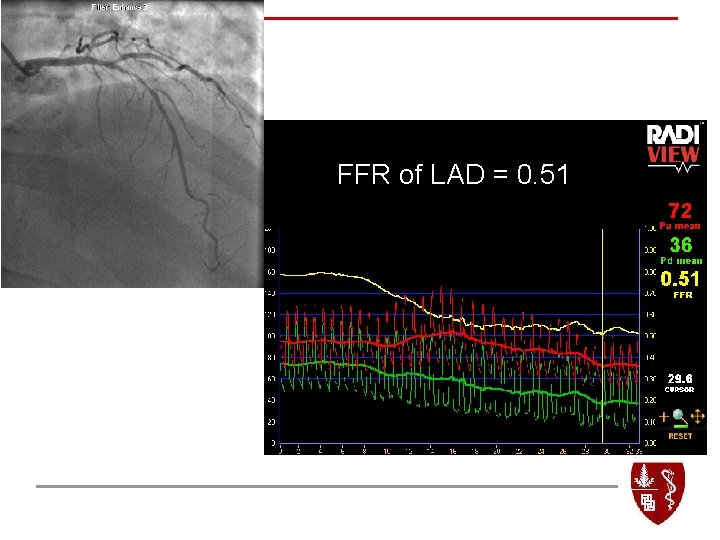
FFR of LAD = 0. 51
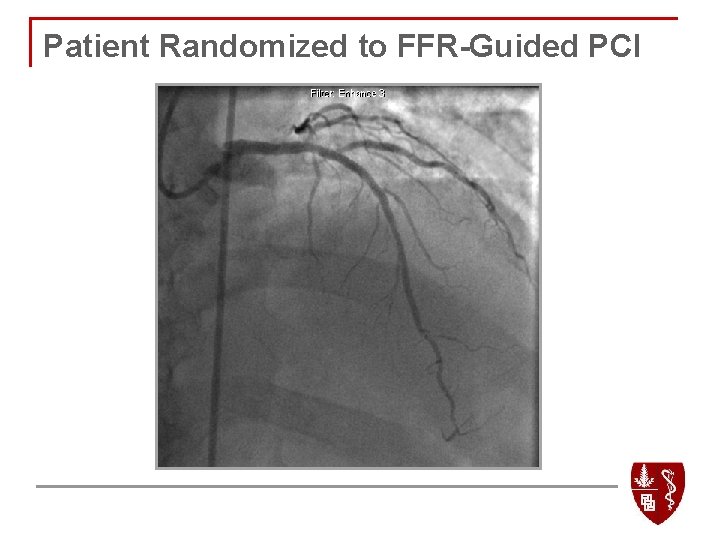
LAD after PCI Patient Randomized to FFR-Guided PCI
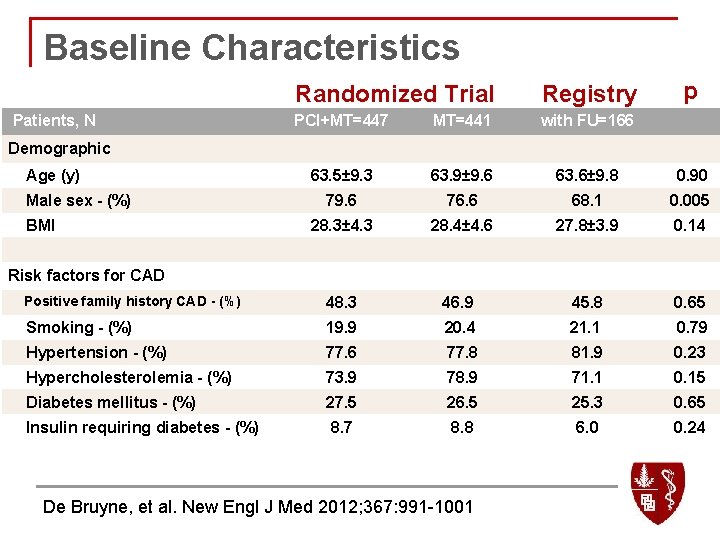
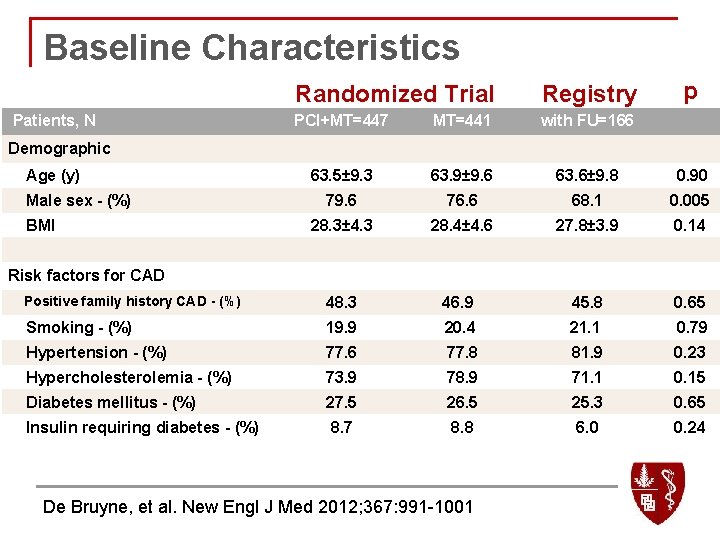
Baseline Characteristics Randomized Trial Registry Patients, N p PCI+MT=447 MT=441 with FU=166 63. 5± 9. 3 63. 9± 9. 6 63. 6± 9. 8 0. 90 79. 6 76. 6 68. 1 0. 005 28. 3± 4. 3 28. 4± 4. 6 27. 8± 3. 9 0. 14 Positive family history CAD - (%) 48. 3 46. 9 45. 8 0. 65 Smoking - (%) 19. 9 20. 4 21. 1 0. 79 Hypertension - (%) 77. 6 77. 8 81. 9 0. 23 Hypercholesterolemia - (%) 73. 9 78. 9 71. 1 0. 15 Diabetes mellitus - (%) 27. 5 26. 5 25. 3 0. 65 Insulin requiring diabetes - (%) 8. 7 8. 8 6. 0 0. 24 Demographic Age (y) Male sex - (%) BMI Risk factors for CAD De Bruyne, et al. New Engl J Med 2012; 367: 991 -1001
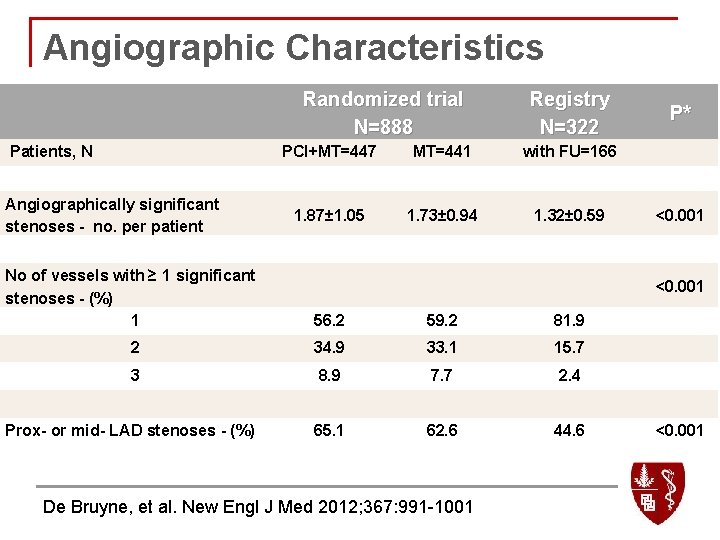
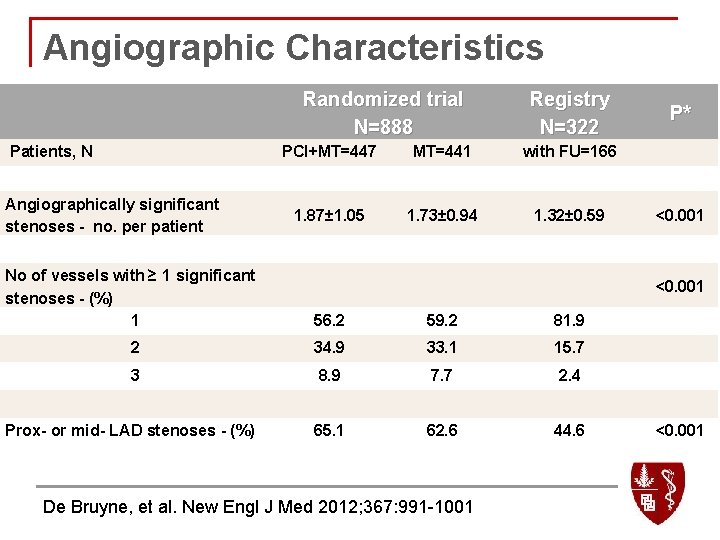
Angiographic Characteristics Randomized trial N=888 Patients, N Angiographically significant stenoses - no. per patient Registry N=322 P* PCI+MT=447 MT=441 with FU=166 1. 87± 1. 05 1. 73± 0. 94 1. 32± 0. 59 <0. 001 No of vessels with ≥ 1 significant stenoses - (%) 1 56. 2 59. 2 81. 9 2 34. 9 33. 1 15. 7 3 8. 9 7. 7 2. 4 Prox- or mid- LAD stenoses - (%) 65. 1 62. 6 44. 6 <0. 001 De Bruyne, et al. New Engl J Med 2012; 367: 991 -1001 <0. 001
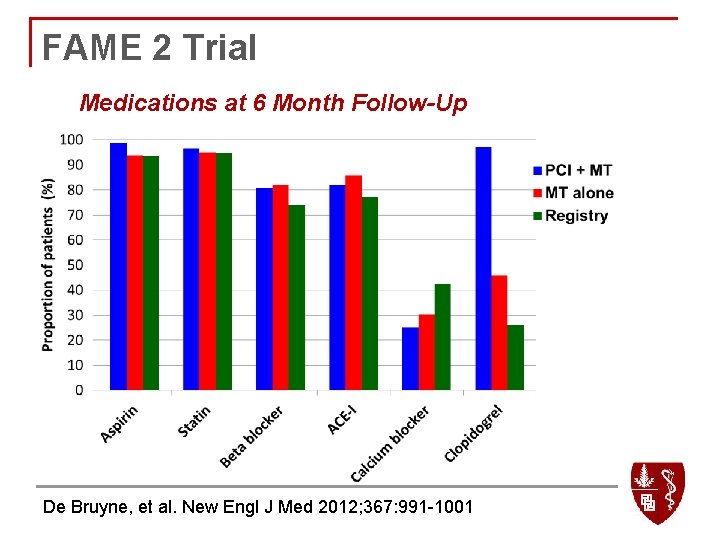
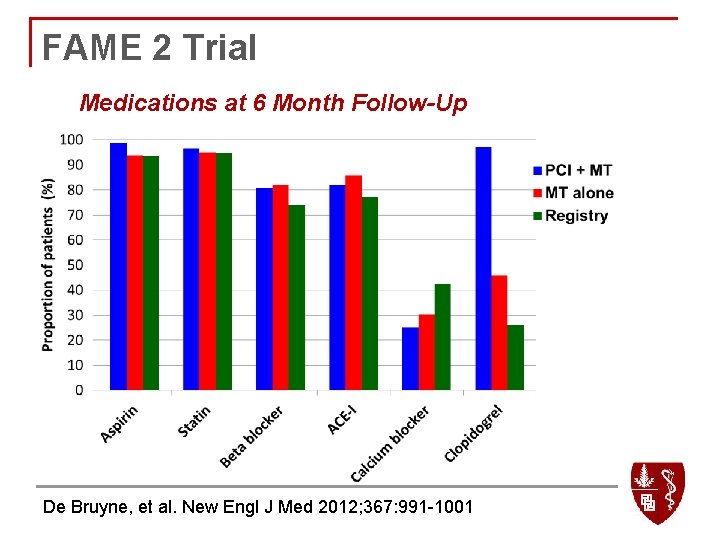
FAME 2 Trial Medications at 6 Month Follow-Up De Bruyne, et al. New Engl J Med 2012; 367: 991 -1001
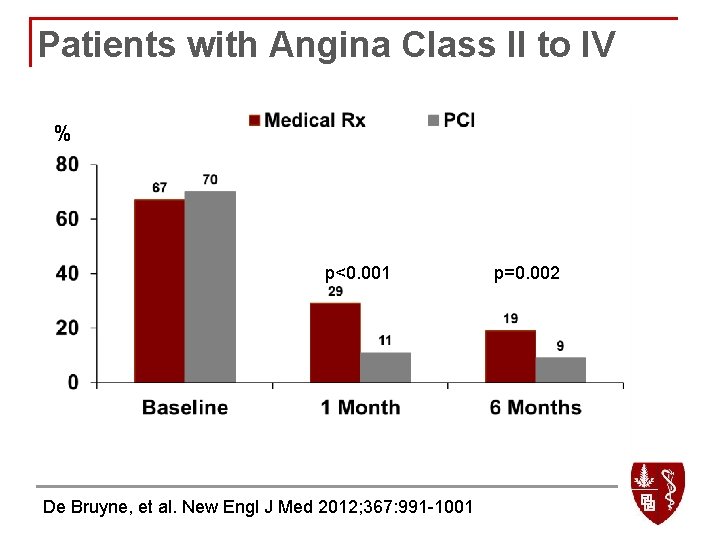
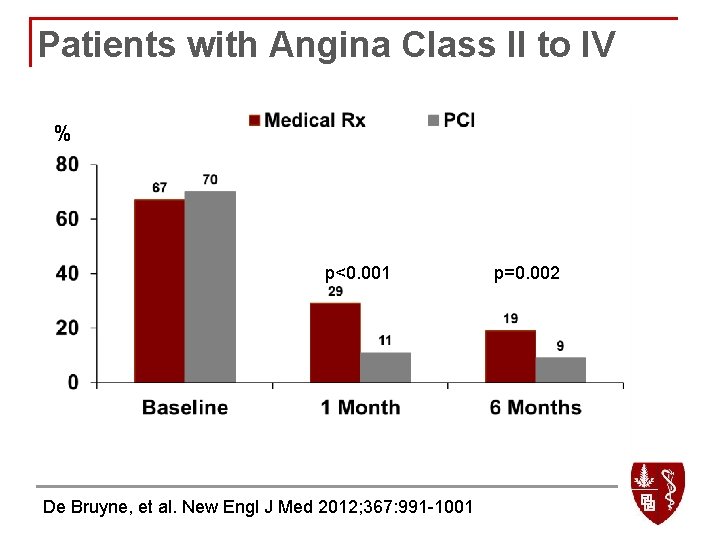
Patients with Angina Class II to IV % p<0. 001 De Bruyne, et al. New Engl J Med 2012; 367: 991 -1001 p=0. 002
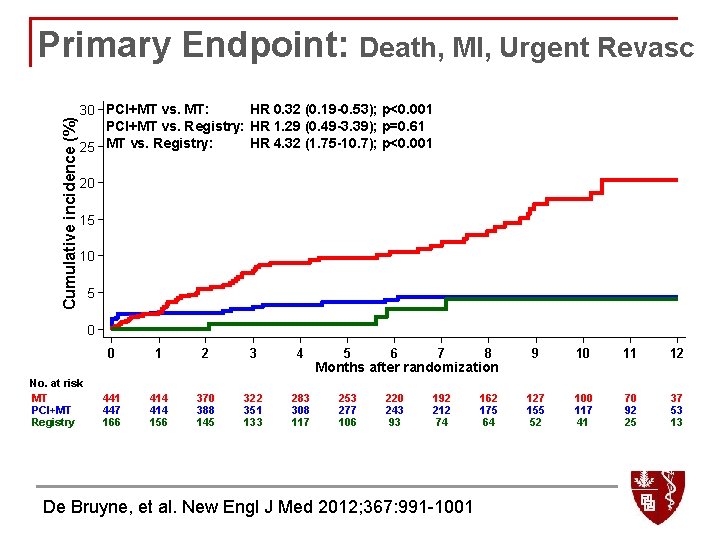
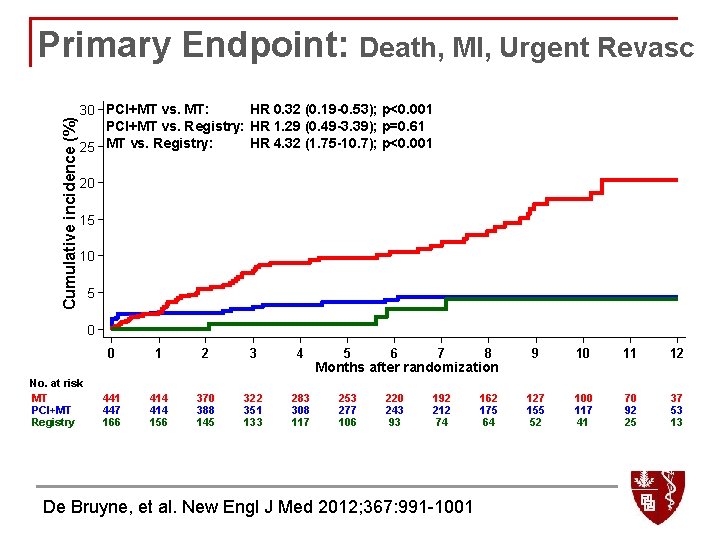
Cumulative incidence (%) Primary Endpoint: Death, MI, Urgent Revasc 30 PCI+MT vs. MT: HR 0. 32 (0. 19 -0. 53); p<0. 001 PCI+MT vs. Registry: HR 1. 29 (0. 49 -3. 39); p=0. 61 25 MT vs. Registry: HR 4. 32 (1. 75 -10. 7); p<0. 001 20 15 10 5 0 No. at risk MT PCI+MT Registry 0 1 2 3 4 441 447 166 414 156 370 388 145 322 351 133 283 308 117 5 6 7 8 9 10 11 12 253 277 106 220 243 93 192 212 74 162 175 64 127 155 52 100 117 41 70 92 25 37 53 13 Months after randomization De Bruyne, et al. New Engl J Med 2012; 367: 991 -1001
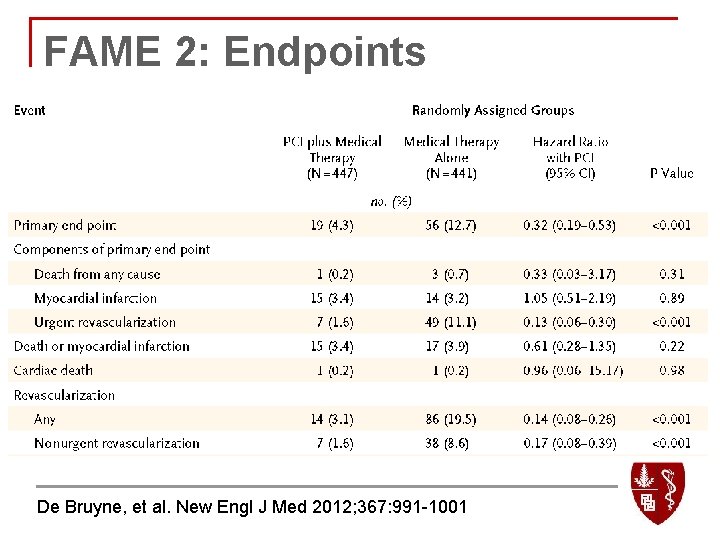
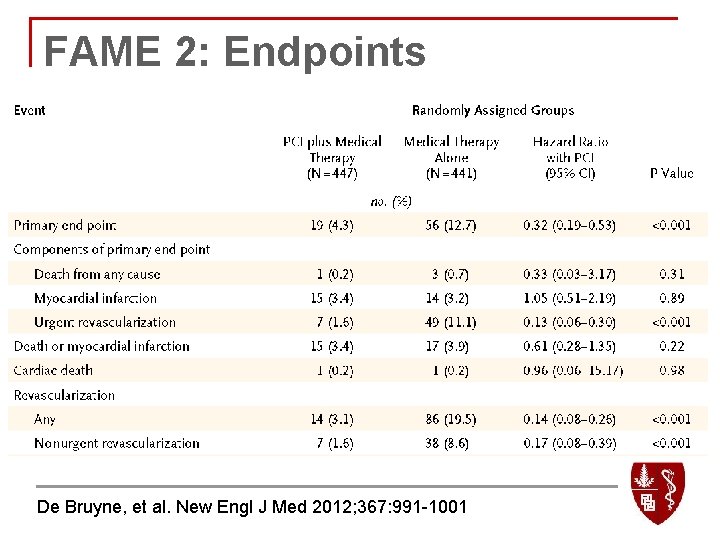
FAME 2: Endpoints De Bruyne, et al. New Engl J Med 2012; 367: 991 -1001
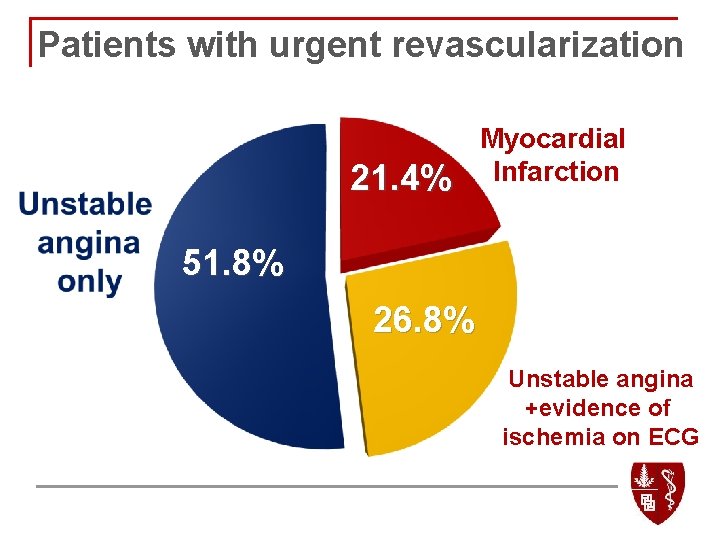
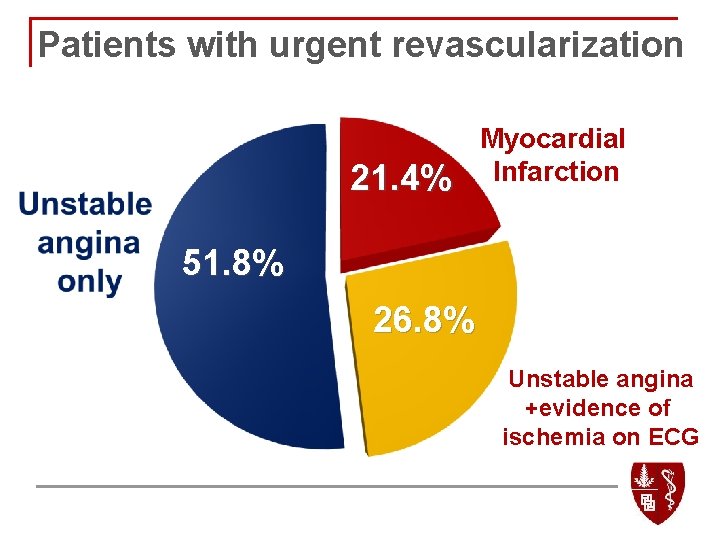
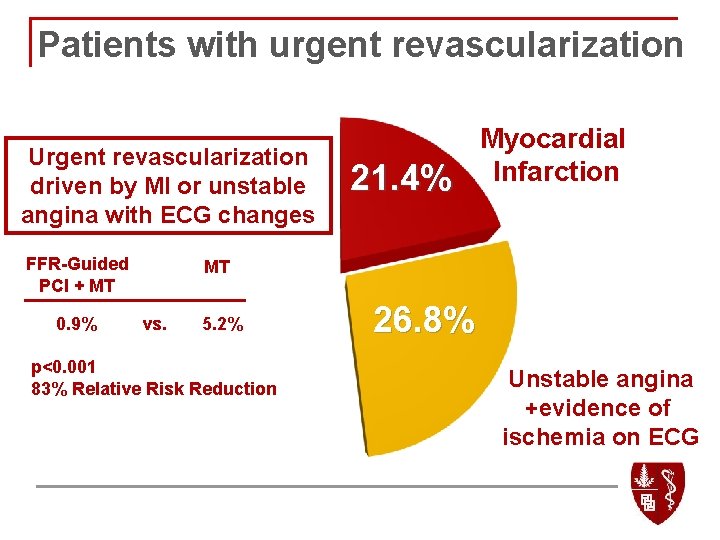
Patients with urgent revascularization 21. 4% Myocardial Infarction 51. 8% 26. 8% Unstable angina +evidence of ischemia on ECG
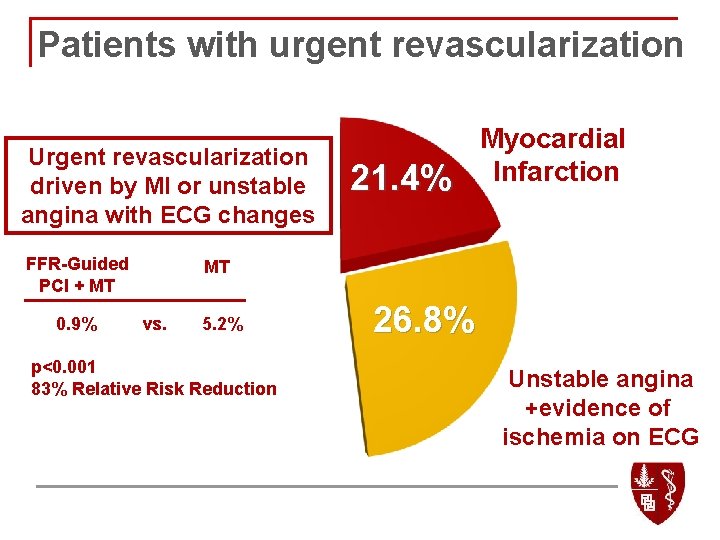
Patients with urgent revascularization Urgent revascularization driven by MI or unstable angina with ECG changes FFR-Guided PCI + MT 21. 4% Myocardial Infarction MT 51. 8% 0. 9% vs. 5. 2% p<0. 001 83% Relative Risk Reduction 26. 8% Unstable angina +evidence of ischemia on ECG
FAME 2: Two Lessons Learned n Patient selection q n Importance of identifying hemodynamically significant narrowings! Cost implications of FFR-guided PCI
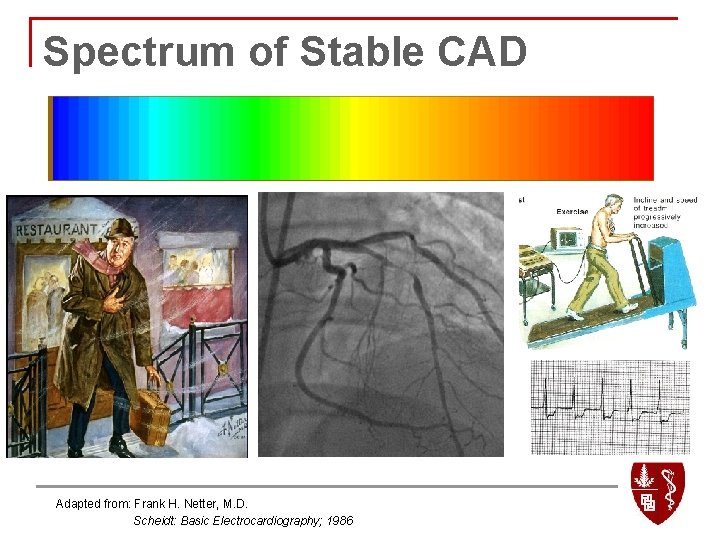
Spectrum of Stable CAD Adapted from: Frank H. Netter, M. D. Scheidt: Basic Electrocardiography; 1986
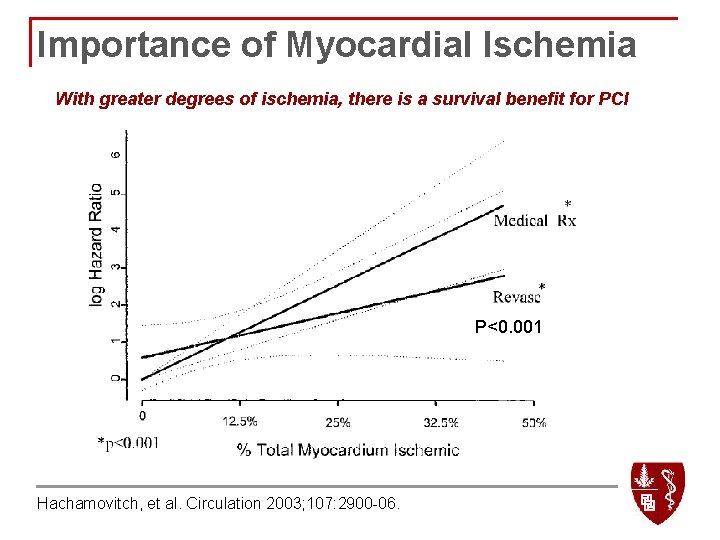
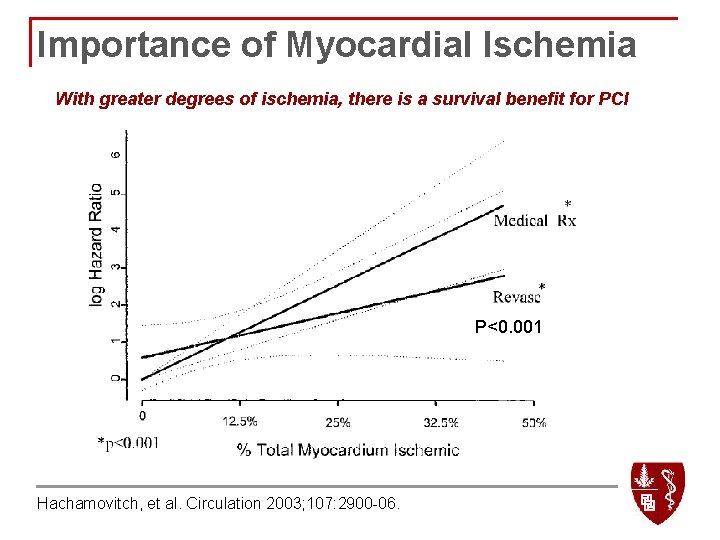
Importance of Myocardial Ischemia With greater degrees of ischemia, there is a survival benefit for PCI P<0. 001 Hachamovitch, et al. Circulation 2003; 107: 2900 -06.
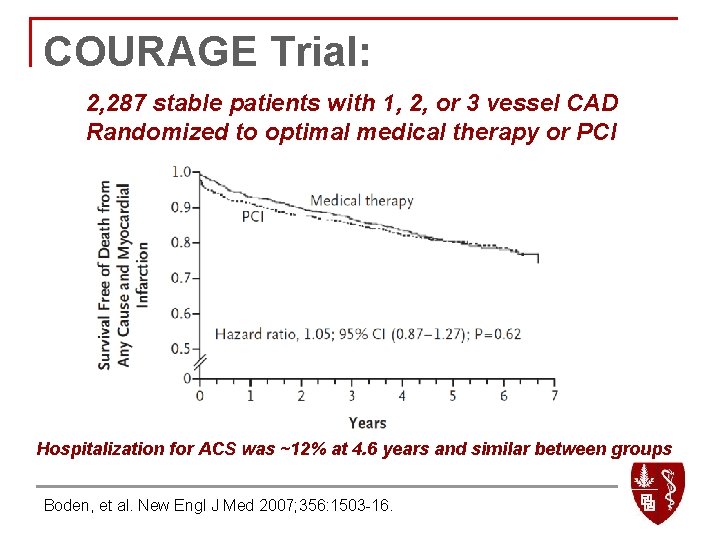
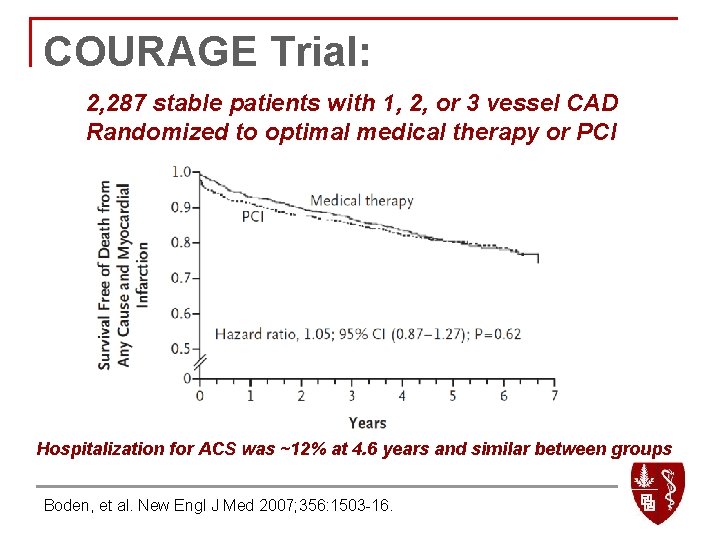
COURAGE Trial: 2, 287 stable patients with 1, 2, or 3 vessel CAD Randomized to optimal medical therapy or PCI Hospitalization for ACS was ~12% at 4. 6 years and similar between groups Boden, et al. New Engl J Med 2007; 356: 1503 -16.
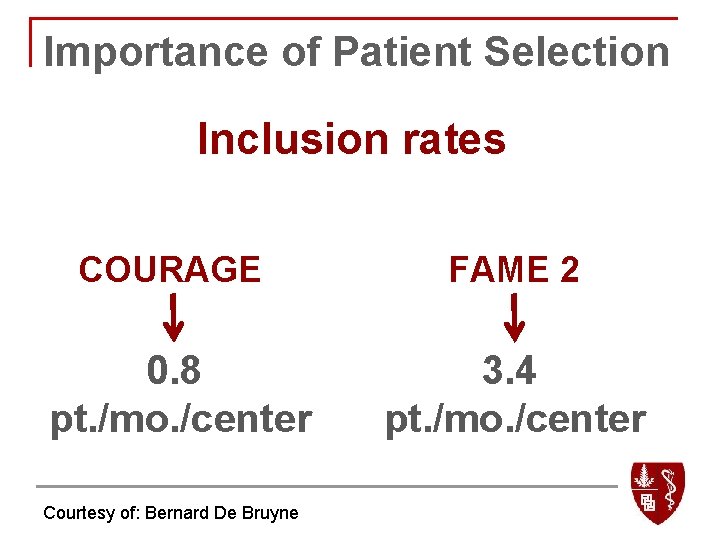
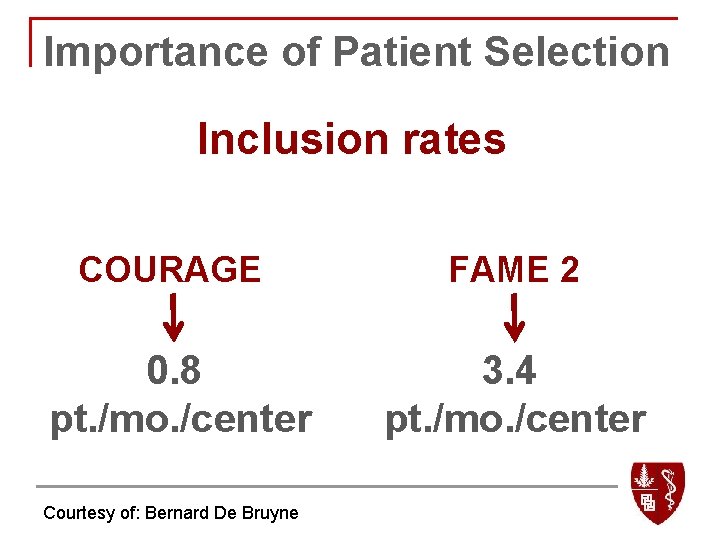
Importance of Patient Selection Inclusion rates COURAGE FAME 2 0. 8 pt. /mo. /center 3. 4 pt. /mo. /center Courtesy of: Bernard De Bruyne
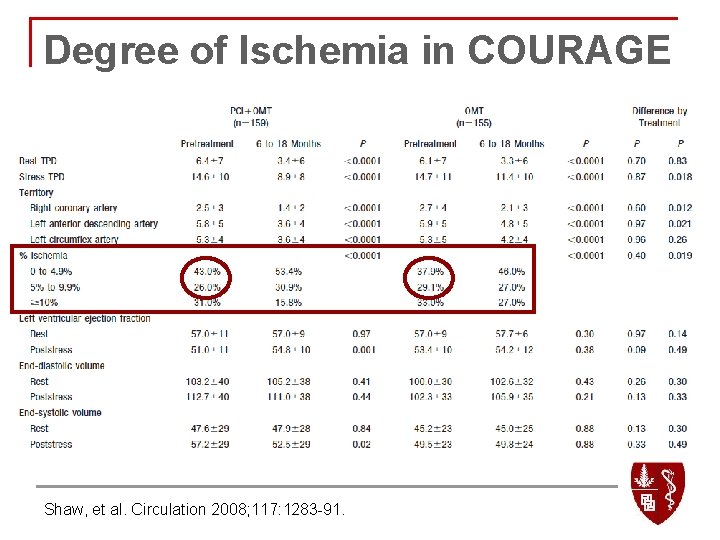
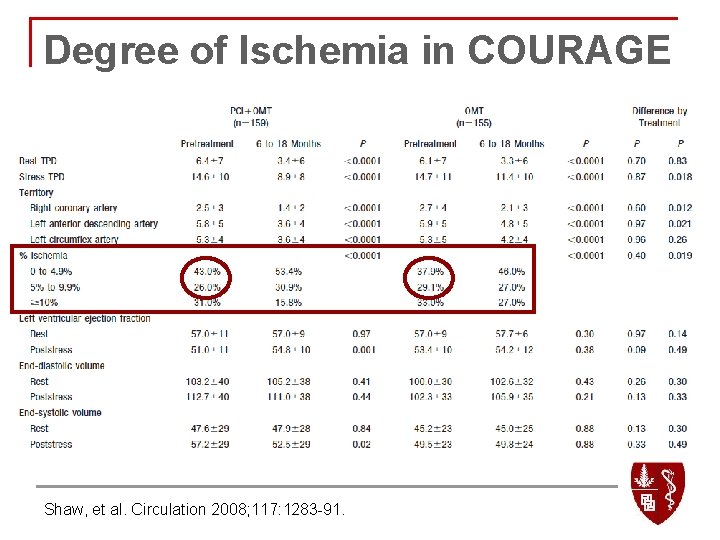
Degree of Ischemia in COURAGE Shaw, et al. Circulation 2008; 117: 1283 -91.
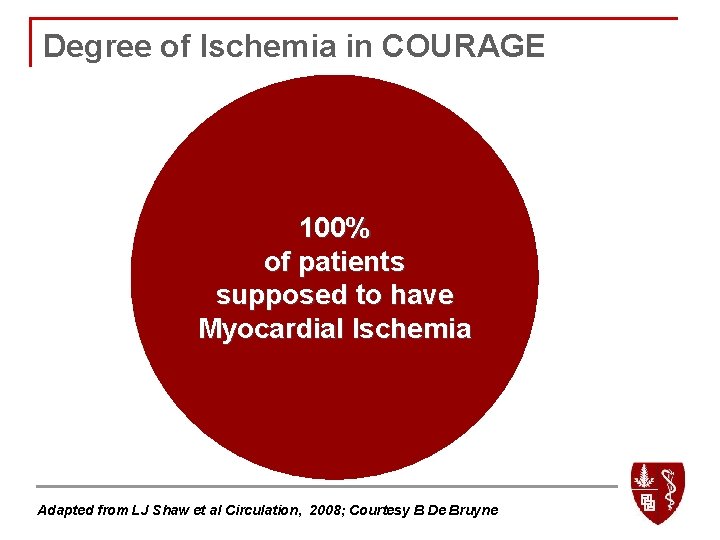
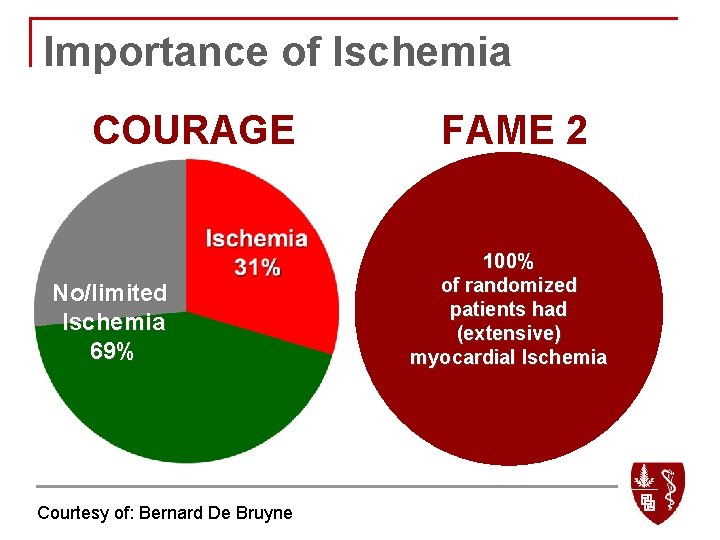
Degree of Ischemia in COURAGE 100% No/limited of patients Ischemia supposed to have Myocardial Ischemia 69% Adapted from LJ Shaw et al Circulation, 2008; Courtesy B De Bruyne
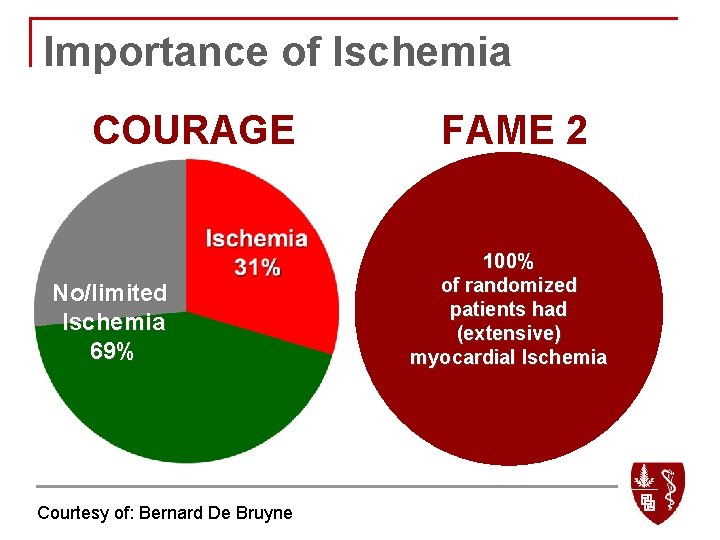
Importance of Ischemia COURAGE No/limited Ischemia 69% Courtesy of: Bernard De Bruyne FAME 2 100% of randomized patients had (extensive) myocardial Ischemia
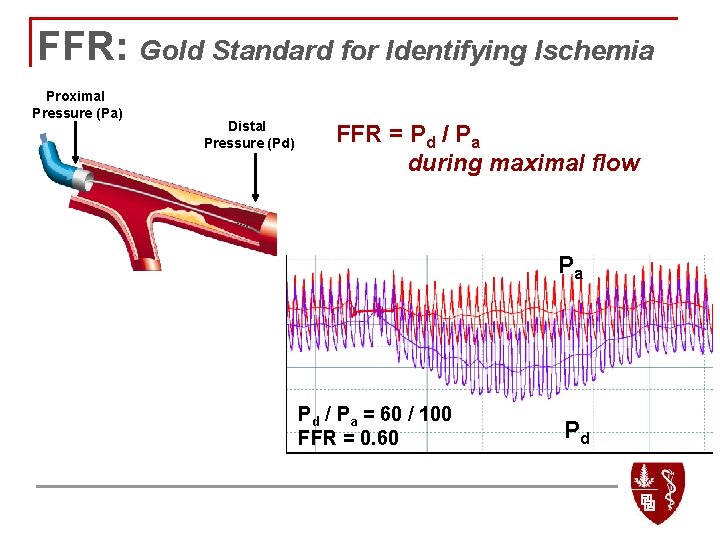
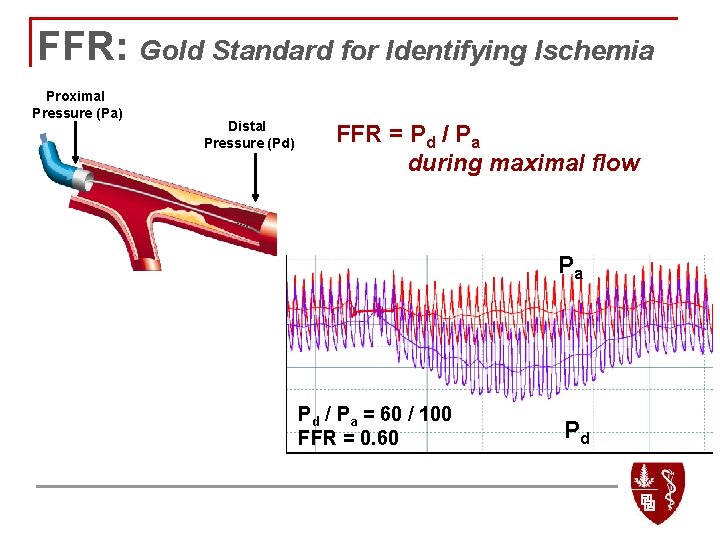
FFR: Gold Standard for Identifying Ischemia Proximal Pressure (Pa) Distal Pressure (Pd) FFR = Pd / Pa during maximal flow Pa Pd / Pa = 60 / 100 FFR = 0. 60 Pd
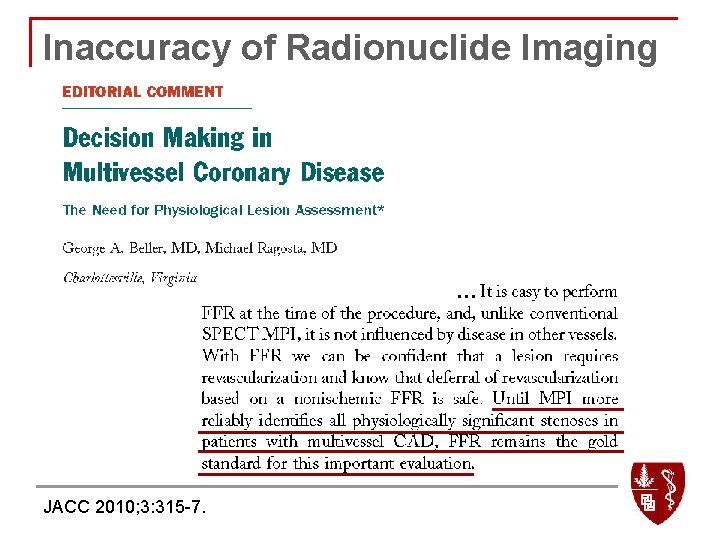
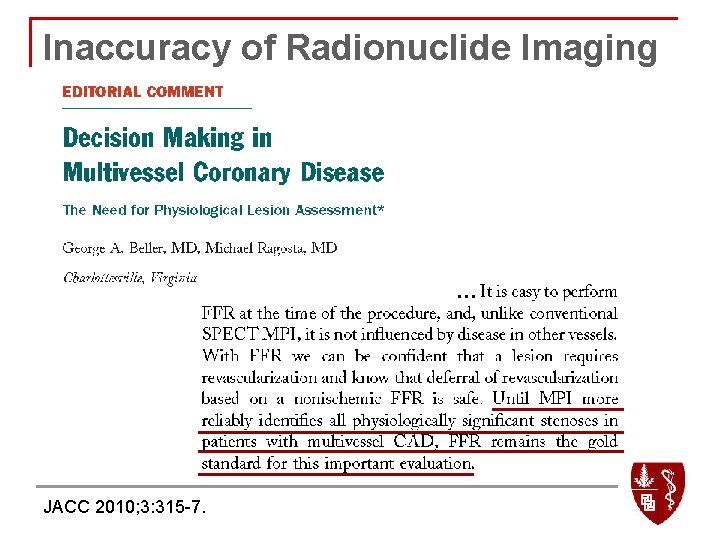
Inaccuracy of Radionuclide Imaging … JACC 2010; 3: 315 -7.
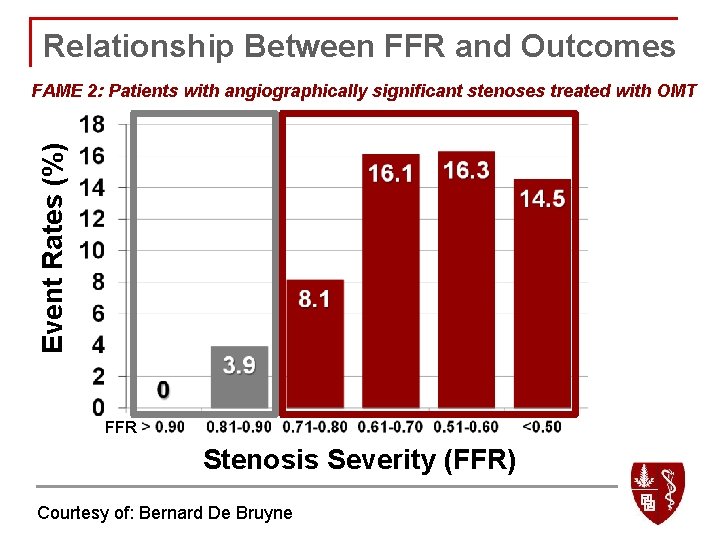
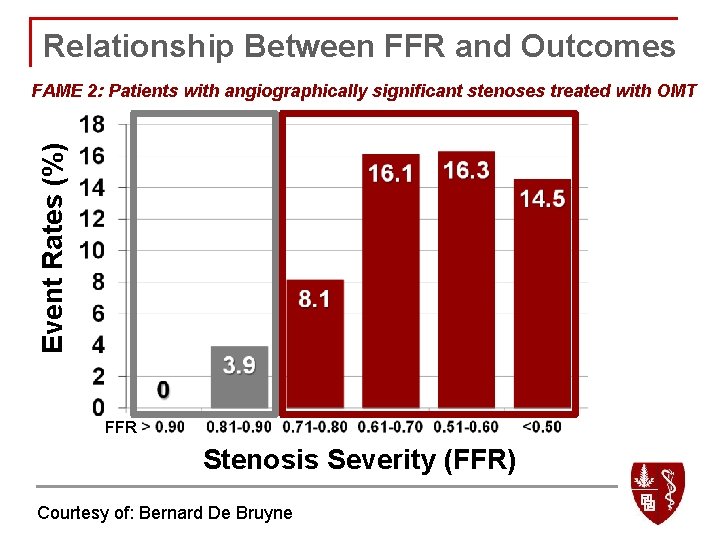
Relationship Between FFR and Outcomes Event Rates (%) FAME 2: Patients with angiographically significant stenoses treated with OMT 4. 3 FFR Stenosis Severity (FFR) Courtesy of: Bernard De Bruyne
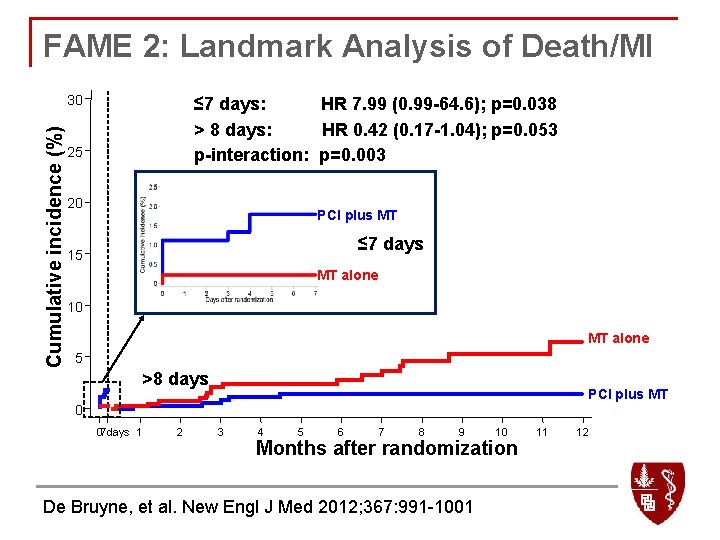
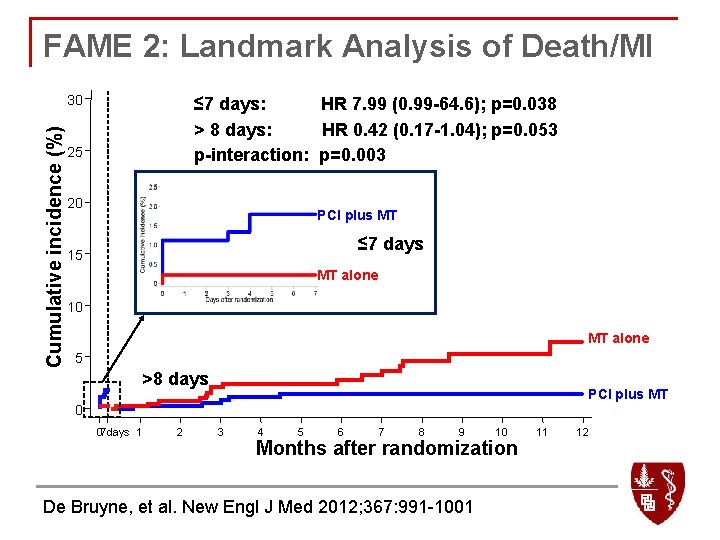
FAME 2: Landmark Analysis of Death/MI Cumulative incidence (%) 30 ≤ 7 days: HR 7. 99 (0. 99 -64. 6); p=0. 038 > 8 days: HR 0. 42 (0. 17 -1. 04); p=0. 053 p-interaction: p=0. 003 25 20 PCI plus MT ≤ 7 days 15 MT alone 10 MT alone 5 >8 days PCI plus MT 0 07 days 1 2 3 4 5 6 7 8 9 10 Months after randomization De Bruyne, et al. New Engl J Med 2012; 367: 991 -1001 11 12
FAME 2: Two Lessons Learned n Patient selection q n Importance of identifying hemodynamically significant narrowings! Cost implications of FFR-guided PCI
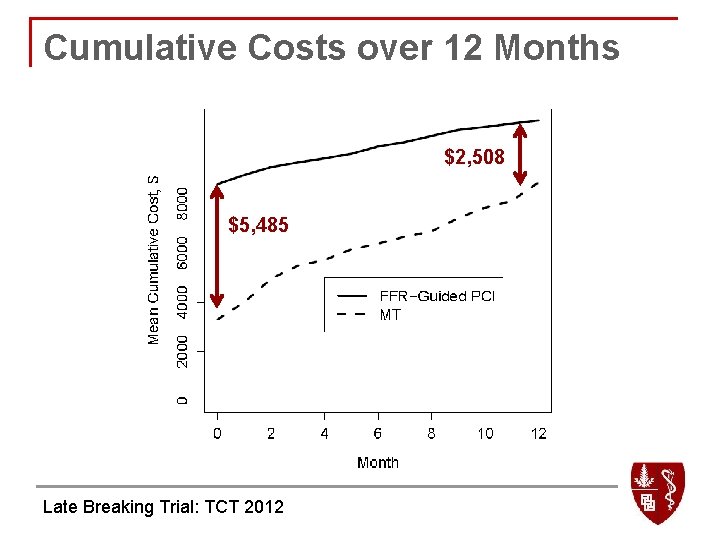
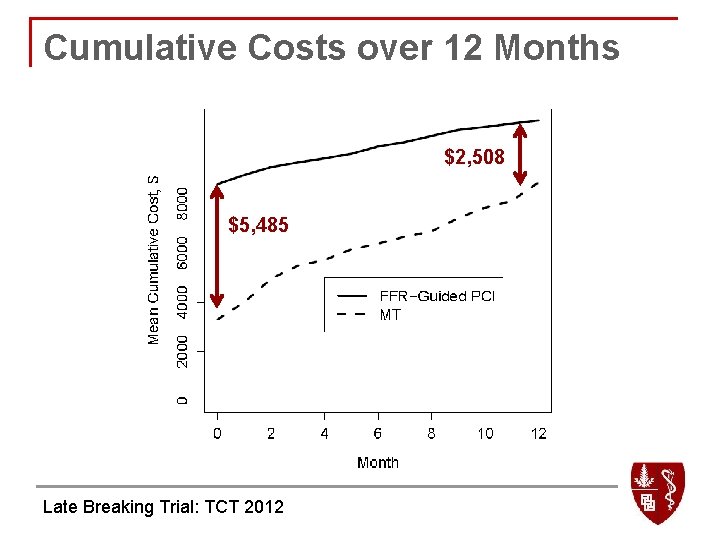
Cumulative Costs over 12 Months $2, 508 $5, 485 Late Breaking Trial: TCT 2012
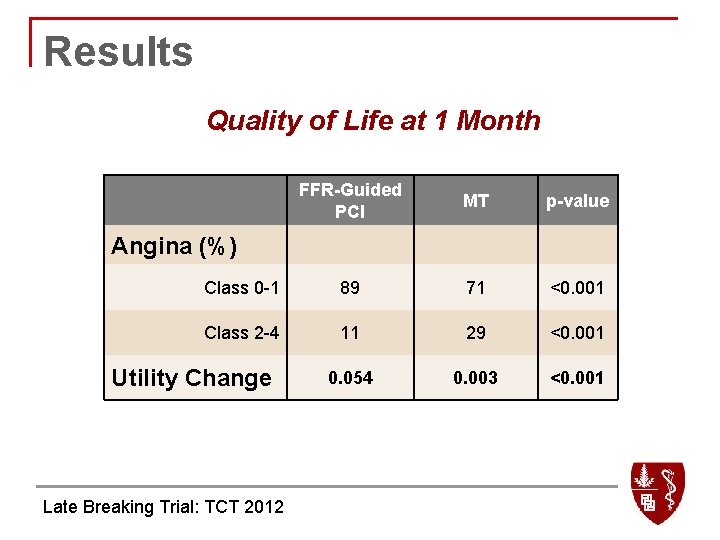
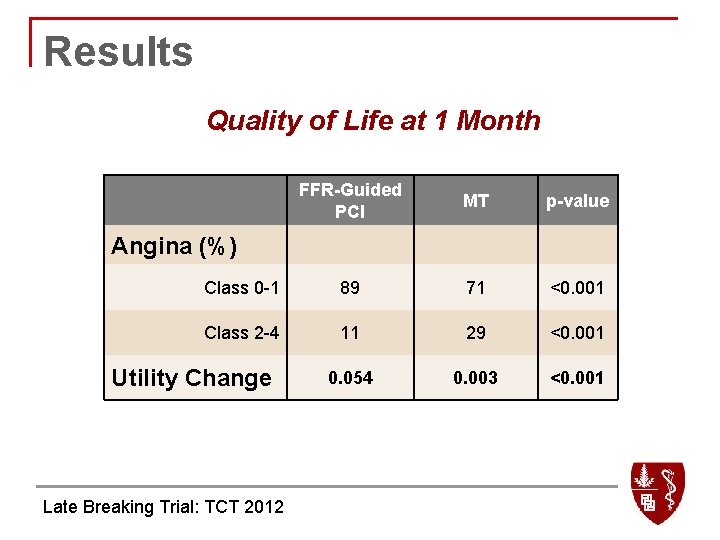
Results Quality of Life at 1 Month FFR-Guided PCI MT p-value Class 0 -1 89 71 <0. 001 Class 2 -4 11 29 <0. 001 0. 054 0. 003 <0. 001 Angina (%) Utility Change Late Breaking Trial: TCT 2012
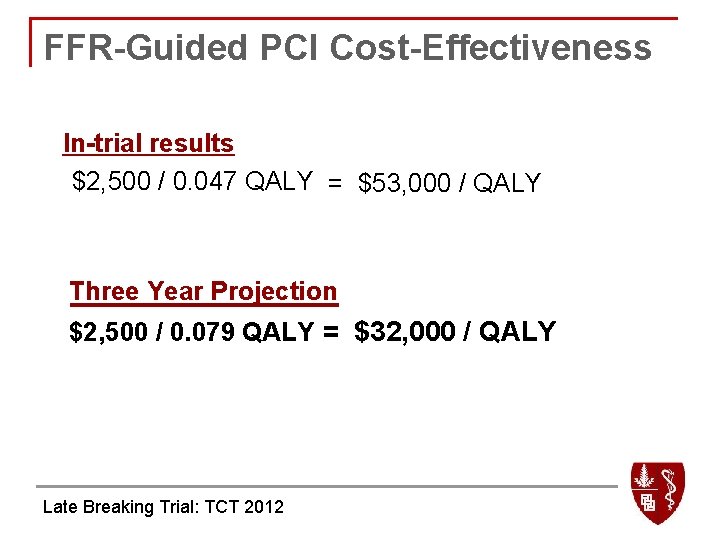
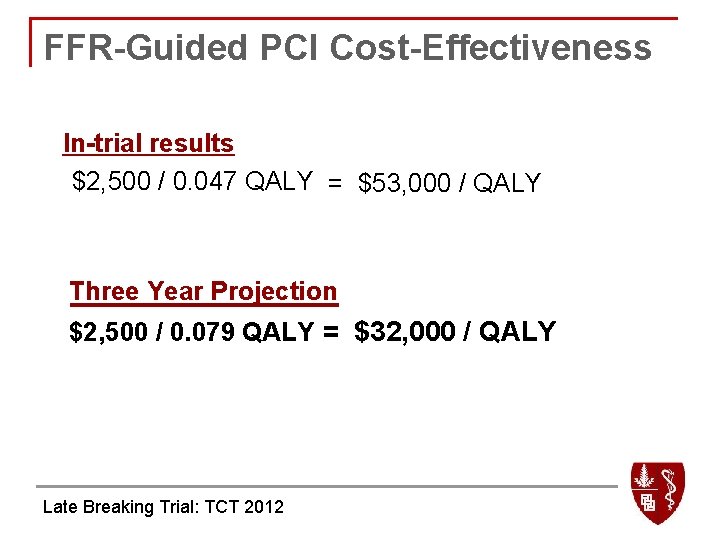
FFR-Guided PCI Cost-Effectiveness In-trial results $2, 500 / 0. 047 QALY = $53, 000 / QALY Three Year Projection $2, 500 / 0. 079 QALY = $32, 000 / QALY Late Breaking Trial: TCT 2012
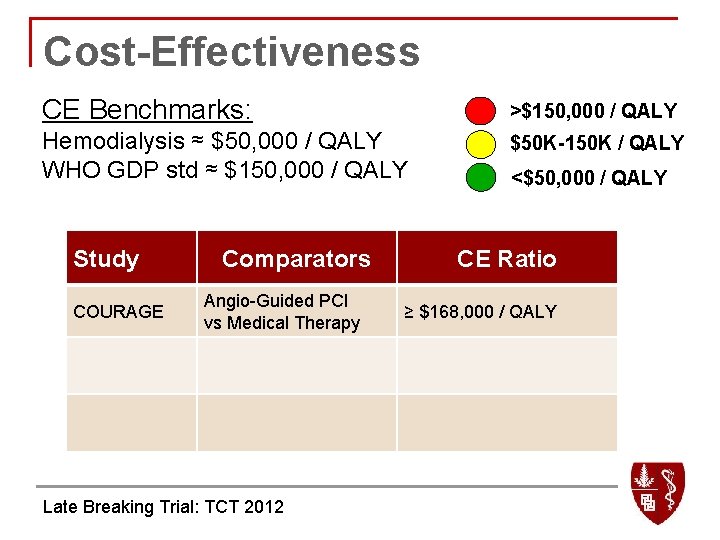
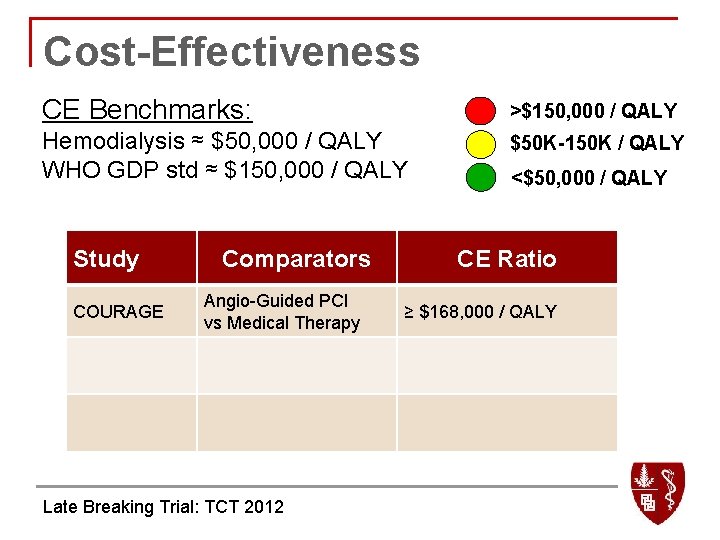
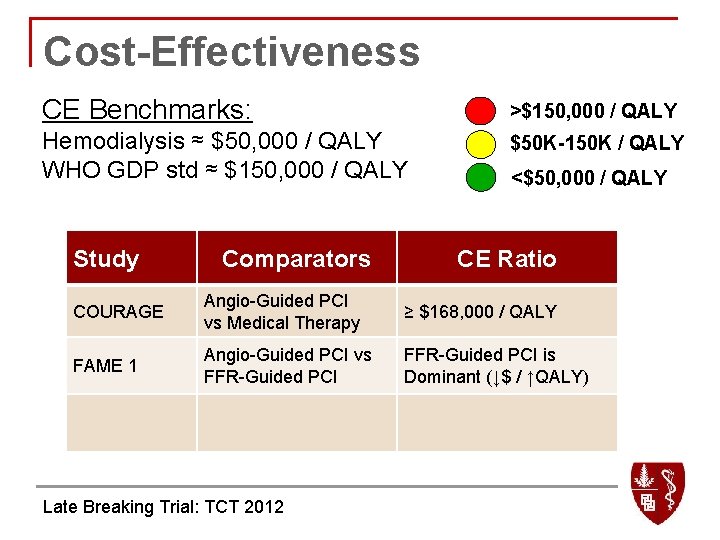
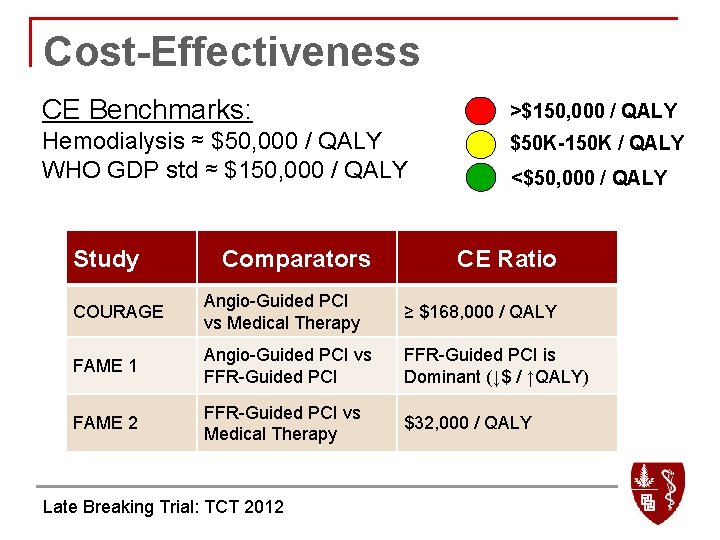
Cost-Effectiveness CE Benchmarks: >$150, 000 / QALY Hemodialysis ≈ $50, 000 / QALY WHO GDP std ≈ $150, 000 / QALY $50 K-150 K / QALY Study COURAGE Comparators Angio-Guided PCI vs Medical Therapy Late Breaking Trial: TCT 2012 <$50, 000 / QALY CE Ratio ≥ $168, 000 / QALY
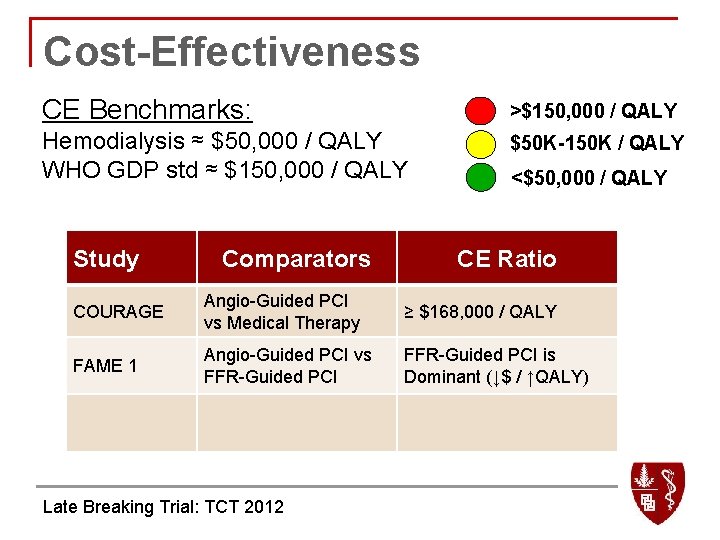
Cost-Effectiveness CE Benchmarks: >$150, 000 / QALY Hemodialysis ≈ $50, 000 / QALY WHO GDP std ≈ $150, 000 / QALY $50 K-150 K / QALY Study Comparators <$50, 000 / QALY CE Ratio COURAGE Angio-Guided PCI vs Medical Therapy ≥ $168, 000 / QALY FAME 1 Angio-Guided PCI vs FFR-Guided PCI is Dominant (↓$ / ↑QALY) Late Breaking Trial: TCT 2012
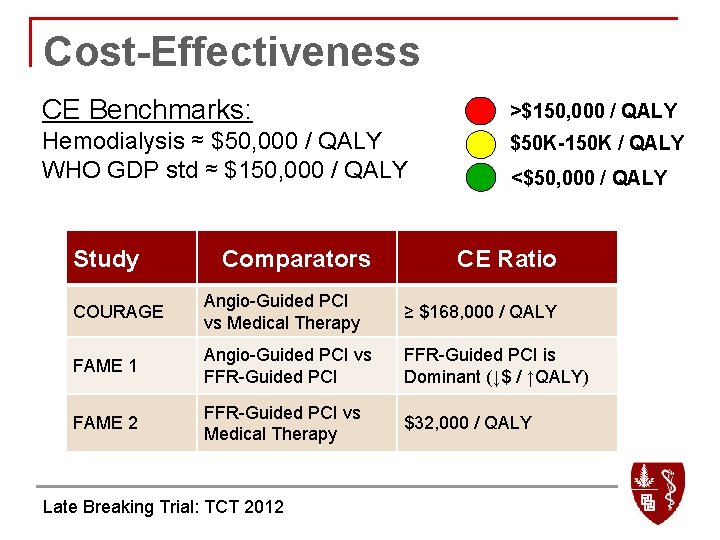
Cost-Effectiveness CE Benchmarks: >$150, 000 / QALY Hemodialysis ≈ $50, 000 / QALY WHO GDP std ≈ $150, 000 / QALY $50 K-150 K / QALY Study Comparators <$50, 000 / QALY CE Ratio COURAGE Angio-Guided PCI vs Medical Therapy ≥ $168, 000 / QALY FAME 1 Angio-Guided PCI vs FFR-Guided PCI is Dominant (↓$ / ↑QALY) FAME 2 FFR-Guided PCI vs Medical Therapy $32, 000 / QALY Late Breaking Trial: TCT 2012
FAME 2 Trial Take Home Messages: § In patients with stable coronary artery disease, FFRguided PCI improves patient outcome and is costeffective when compared to medical therapy alone. § This improvement is driven by a dramatic decrease in the need for urgent revascularization for ACS. § In patients with functionally non-significant stenoses, medical therapy alone resulted in an excellent outcome, regardless of the angiographic appearance of the stenoses.