END OF LIFE SPIRITUALITY OVERVIEW Ethics and Spirituality










- Slides: 39
END OF LIFE SPIRITUALITY OVERVIEW Ethics and Spirituality: It is about meaning Man is not destroyed by suffering; he is destroyed by suffering without meaning (Victor Frankl)
the possibility of non-being At the time of death, certain questions about meaning arise What are we made of? Material or Spirit or both? What does it mean to live? What does it mean to die? What does it mean to be a human being who lives and dies? If and How will I continue to exist? How will I be remembered? What’s my legacy? What's on the “other side”? Why me? Why now? Does death mean I become nothing? Does death mean non-being in one way but not in another way? Does it mean I continue to exist in a more real way?

What does it mean to live as a human being? Three basic metaphysical concepts of being human: Dualism and the resulting idealism Materialism Holism
Idealism Dualism/Idealism - Body vs mind-spirit. The real existence is the mind, the soul or spirit, and the realm of ideals. The resulting human project is to strive for idealized perfection.

Materialism - the only thing that exists is matter all phenomena including consciousness and social constructs are the result of biochemical & physical interactions, empirically verifiable. Non material realities such as individual identities, personal autonomy, interpersonal relationships, love, truth, hope, and dignity do not really exist; or they exist as illusions.
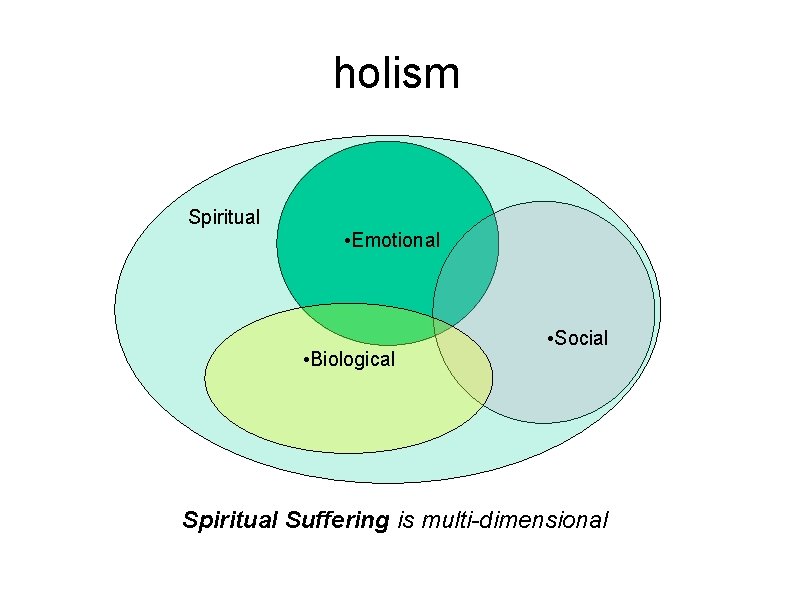
Holism Unity of Form and Substance, Body, Mind and Spirit. Holism comes from the Greek work ὅλος meaning whole, entire, or total. All the properties of a given system (physical, biological, chemical, social, historical, economic, mental, emotional, linguistic, or moral) cannot be determined or explained by its component parts alone. The orientation, consistency, beauty, and functionality of the system as a whole is determined by its parts and vice versa. Philosophical underpinning of medicine, ethics, the arts, anatomy. Physiology, engineering
Spirituality in the Holistic Approach spirituality is not just one aspect among other personality constructs including the physical, the emotional, and the social. It is the unifying and encompassing reality of being human in all these dimensions, The transcending reality that unifies persons to each other and to other transcendent realities such as God. A composite of human experiences, having intellectual, emotional, and behavioral dimensions. The intellectual dimension may contain various philosophical components such as the search for truth, identity, and meaning; The emotional aspect may include the desire for intimacy, love, hope, and peace; The behavioral aspect may include body language expressing discomfort or turning toward rituals that accompany the end of life transition.
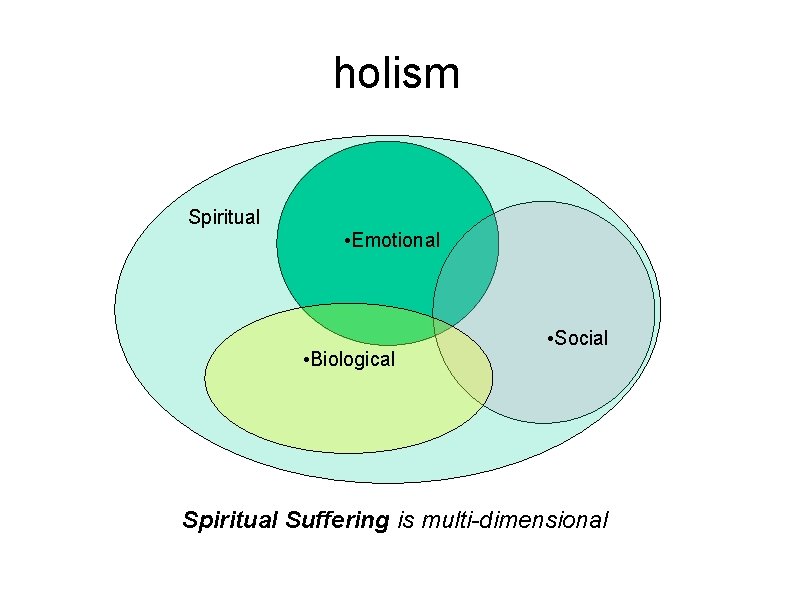
holism Spiritual • Emotional • Biological • Social Spiritual Suffering is multi-dimensional

Spiritual Care of the Dying The Holistic Approach To the dying person, the care of the spiritual dimension is not simply the job of one "spiritual specialist. ” All the care takers in one way or another have a distinct effect on the composition of the dying person's spirituality. We cannot give what we don’t have.
DEFINITIONS AND DISTINCTIONS Spirituality should not be confused with religious practice or belief in the after-life. Spirituality has to do with the most basic question about the meaning of life and death and ways of being. Spirituality encompasses concepts of value, identity, purpose, significance, and autonomy/freedom. “In man, the things which are not measurable are more important than those which are measurable” (Alexis Carrel) “Not everything that counts can be measured. Not everything that can be measured counts” (Albert Einstein)
The Guidelines for Spiritual Care in Hospice for the National Council of Hospice Professionals (NCHP) "Spirituality entails the universal longing for meaning of life; that which gives purpose, direction and the ability to cope with crisis. It may be experienced through a sense of [connectedness] to the transcendent, to other people, or the natural world around us. Spirituality manifests itself in one's longings, interests, relationships, convictions, values, beliefs, traditions and rituals. It can foster a sense of comfort, peace, reconciliation, and wholeness. "
The National Hospice and Palliative Care Organization (NHPCO) 2008 guideline Foundation of Spiritual Care in Hospice “At the heart of spirituality is the universal human capacity for transcendence, that is, the awareness that we humans, individually and collectively, participate in a spiritual reality greater than ourselves. "
The agreed definition in Improving the Quality of Spiritual Care as a Dimension of Palliative Care: A Consensus Conference Convened February 2009: "Spirituality is the aspect of humanity that refers to the way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred. "
The Association of American Medical Colleges (1999: 25) “Spirituality is recognized as a factor that contributes to health in many persons. The concept of spirituality is found in all cultures and societies. It is expressed in an individual’s search for ultimate meaning through participation in religion and/or belief in God, family, naturalism, rationalism, humanism, and the arts. All of these factors can influence how patients and health care professionals perceive health and illness and how they interact with one another. ”

A SPIRITUAL CARE PLAN Adopting a spiritual care model Taking a spiritual history and making an assessment Spiritual diagnosis Spiritual treatment and intervention Documentation Evaluation

spiritual care model The Care Model: "care" rather than "cure" “I think medicine had offered up until the last hundred years or so, basically, care. You probably were not going to get much better but we could teach you how to live with your illness. Now medicine, allegedly because of scientific breakthroughs, is about cure. That puts an extraordinary pressure on physicians to do more than they can. The fact of the matter is, you’re not going to get out of life alive, but people want to ask of physicians more than they can deliver and it’s very tempting to try to deliver that. ” (Stanley Hauerwas in “Learning How to Die: Q&A with Stanley Hauerwas” by Sarah Toneking)

spiritual care model Biopsychosocial-spiritual model: Seeing patients as whole persons and "beings-in-relationship. " This realization of relationships implies self-transcendence, which is the core of spiritual concerns. Diseases can be considered a pathology in biological relationships that mutually affects all other relational realities--familial, friendships, divine. To care is to address everything in the patient's relational web of existence—physical, psychological, social, and spiritual (Daniel Sulmasy, MD)
spiritual care model Interprofessional spiritual care model: A more focused application of the Biopsychosocial model where the relationship of patient and care-giver is prioritized, and where "they work together in a process of discovery, collaborative dialogue, treatment and ongoing evaluation, and follow-up“ (Christina Puchalski, MD Improving the Quality of Spiritual care as a Dimension of Palliative Care)
spiritual history and assessment Understanding the range of response, Physicians can address spiritual issues of patients to the extent that is appropriate. This does not mean staying only in the comfort zone. The spiritual histories are patient-centered, designed to create trust by letting the patient know that the physician is concerned about his/her transcendent issues.
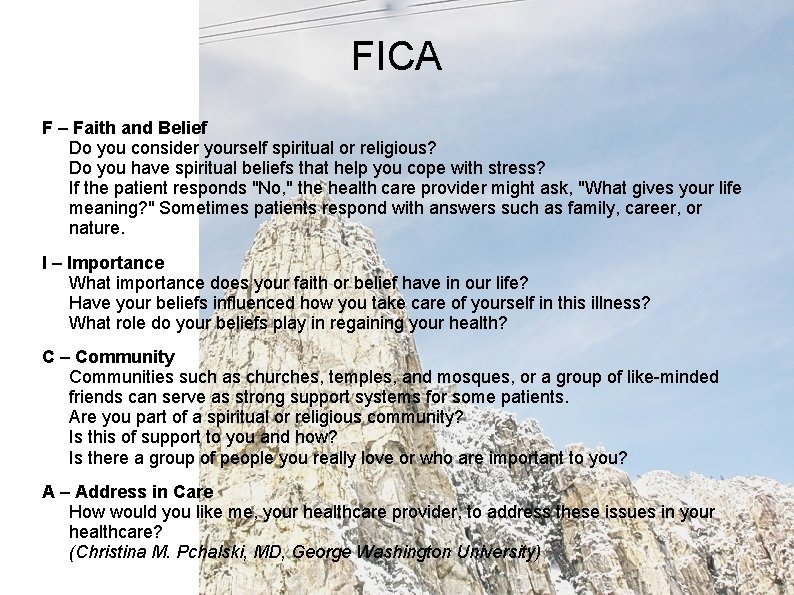
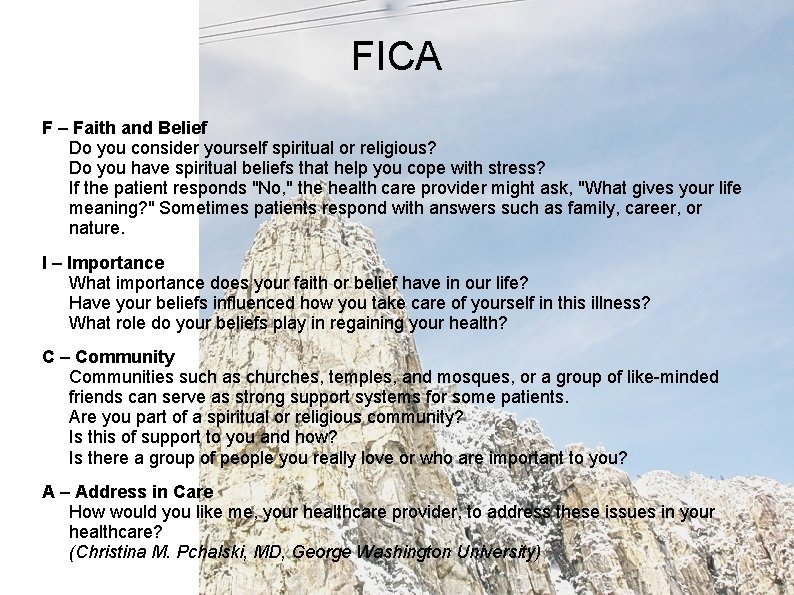
FICA F – Faith and Belief Do you consider yourself spiritual or religious? Do you have spiritual beliefs that help you cope with stress? If the patient responds "No, " the health care provider might ask, "What gives your life meaning? " Sometimes patients respond with answers such as family, career, or nature. I – Importance What importance does your faith or belief have in our life? Have your beliefs influenced how you take care of yourself in this illness? What role do your beliefs play in regaining your health? C – Community Communities such as churches, temples, and mosques, or a group of like-minded friends can serve as strong support systems for some patients. Are you part of a spiritual or religious community? Is this of support to you and how? Is there a group of people you really love or who are important to you? A – Address in Care How would you like me, your healthcare provider, to address these issues in your healthcare? (Christina M. Pchalski, MD, George Washington University)
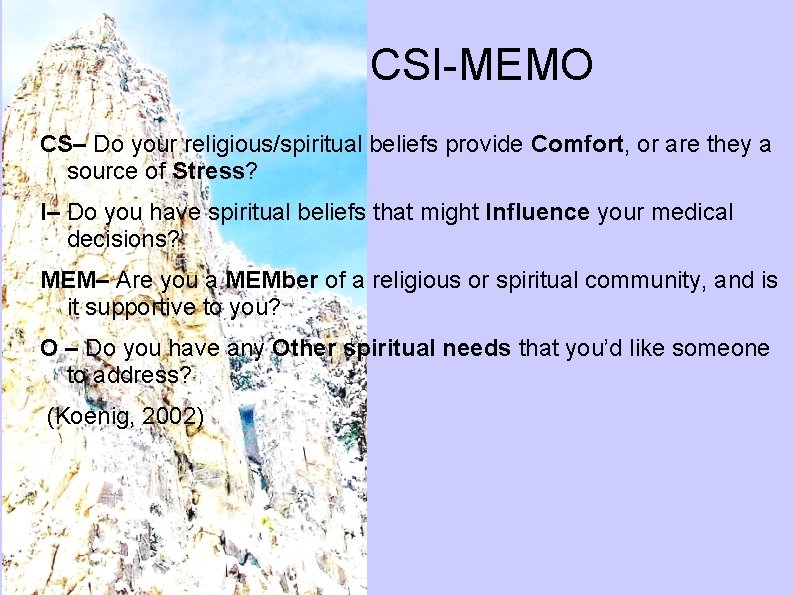
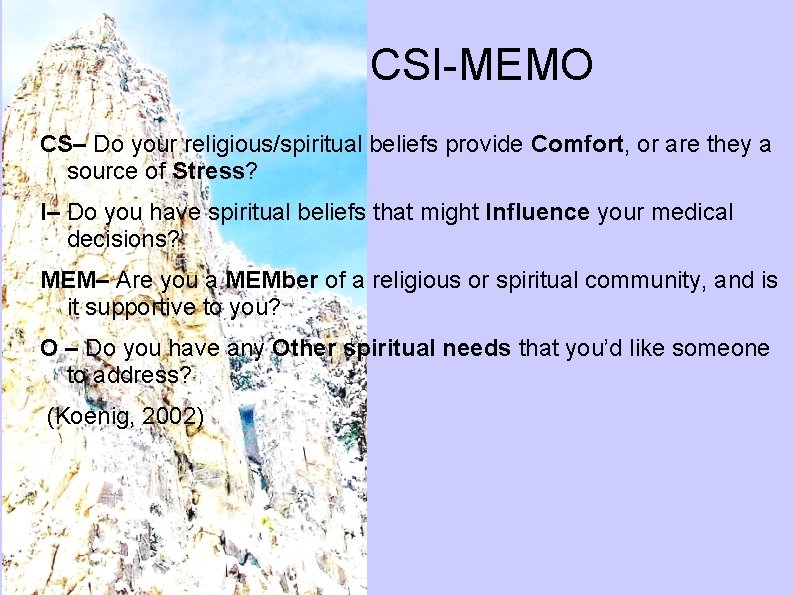
CSI-MEMO CS– Do your religious/spiritual beliefs provide Comfort, or are they a source of Stress? I– Do you have spiritual beliefs that might Influence your medical decisions? MEM– Are you a MEMber of a religious or spiritual community, and is it supportive to you? O – Do you have any Other spiritual needs that you’d like someone to address? (Koenig, 2002)
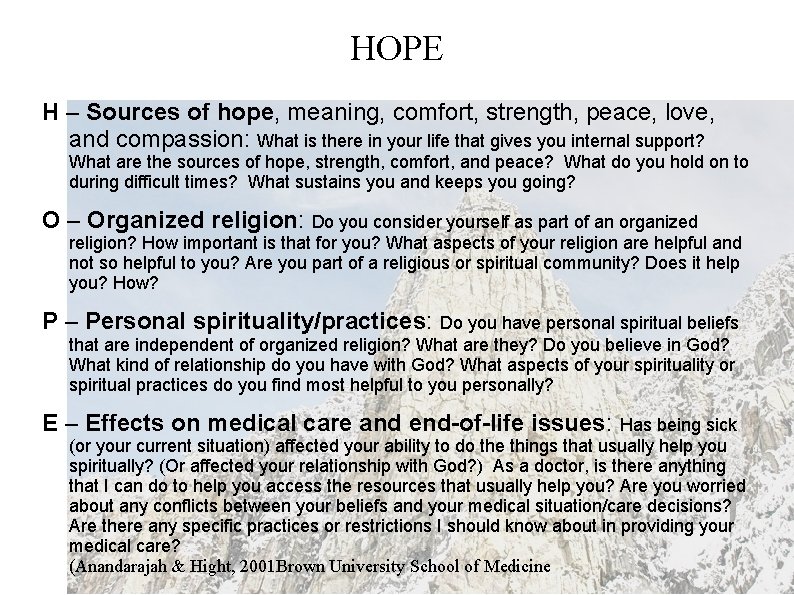
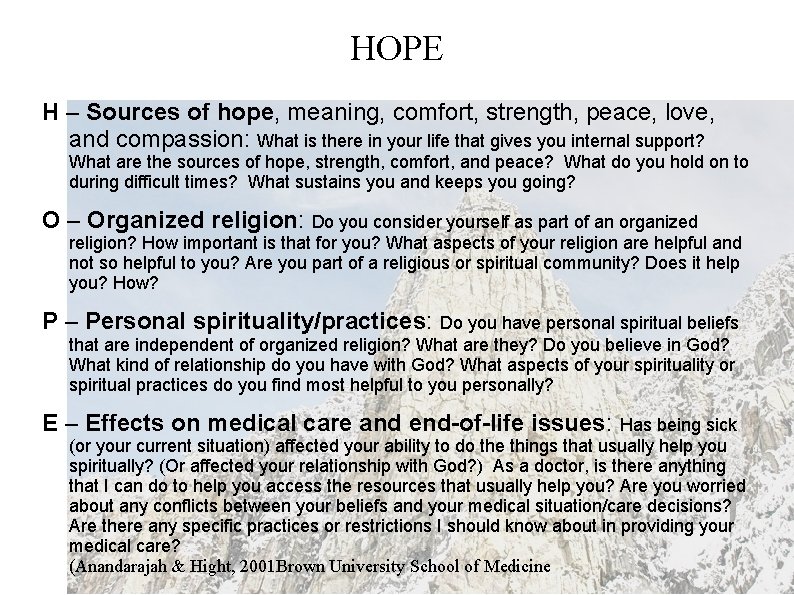
HOPE H – Sources of hope, meaning, comfort, strength, peace, love, and compassion: What is there in your life that gives you internal support? What are the sources of hope, strength, comfort, and peace? What do you hold on to during difficult times? What sustains you and keeps you going? O – Organized religion: Do you consider yourself as part of an organized religion? How important is that for you? What aspects of your religion are helpful and not so helpful to you? Are you part of a religious or spiritual community? Does it help you? How? P – Personal spirituality/practices: Do you have personal spiritual beliefs that are independent of organized religion? What are they? Do you believe in God? What kind of relationship do you have with God? What aspects of your spirituality or spiritual practices do you find most helpful to you personally? E – Effects on medical care and end-of-life issues: Has being sick (or your current situation) affected your ability to do the things that usually help you spiritually? (Or affected your relationship with God? ) As a doctor, is there anything that I can do to help you access the resources that usually help you? Are you worried about any conflicts between your beliefs and your medical situation/care decisions? Are there any specific practices or restrictions I should know about in providing your medical care? (Anandarajah & Hight, 2001 Brown University School of Medicine
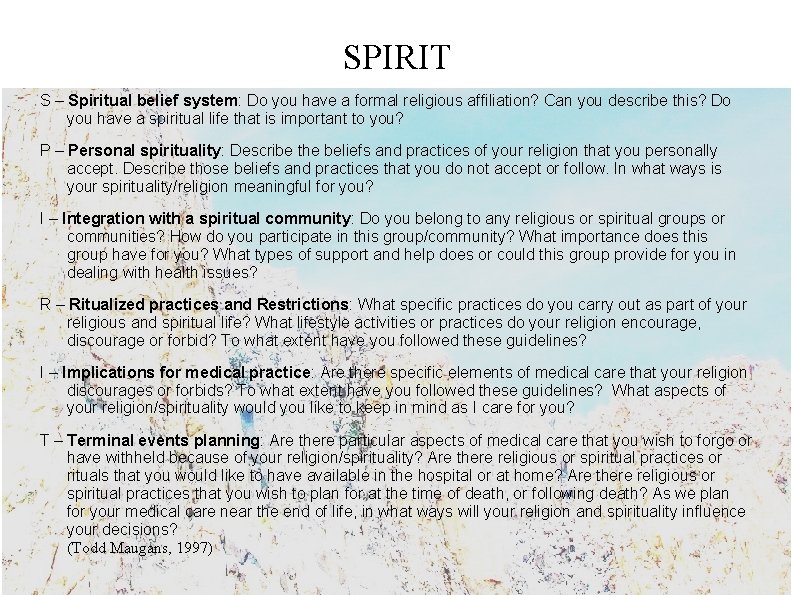
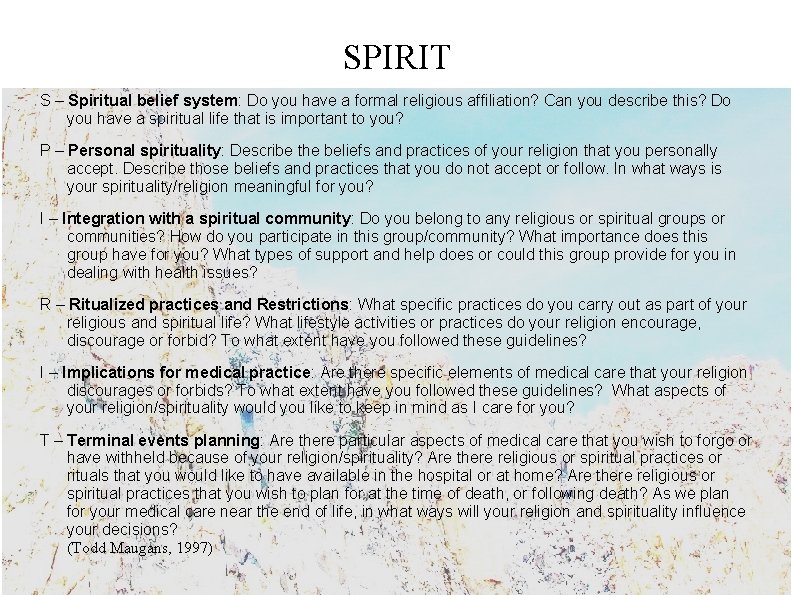
SPIRIT S – Spiritual belief system: Do you have a formal religious affiliation? Can you describe this? Do you have a spiritual life that is important to you? P – Personal spirituality: Describe the beliefs and practices of your religion that you personally accept. Describe those beliefs and practices that you do not accept or follow. In what ways is your spirituality/religion meaningful for you? I – Integration with a spiritual community: Do you belong to any religious or spiritual groups or communities? How do you participate in this group/community? What importance does this group have for you? What types of support and help does or could this group provide for you in dealing with health issues? R – Ritualized practices and Restrictions: What specific practices do you carry out as part of your religious and spiritual life? What lifestyle activities or practices do your religion encourage, discourage or forbid? To what extent have you followed these guidelines? I – Implications for medical practice: Are there specific elements of medical care that your religion discourages or forbids? To what extent have you followed these guidelines? What aspects of your religion/spirituality would you like to keep in mind as I care for you? T – Terminal events planning: Are there particular aspects of medical care that you wish to forgo or have withheld because of your religion/spirituality? Are there religious or spiritual practices or rituals that you would like to have available in the hospital or at home? Are there religious or spiritual practices that you wish to plan for at the time of death, or following death? As we plan for your medical care near the end of life, in what ways will your religion and spirituality influence your decisions? (Todd Maugans, 1997)
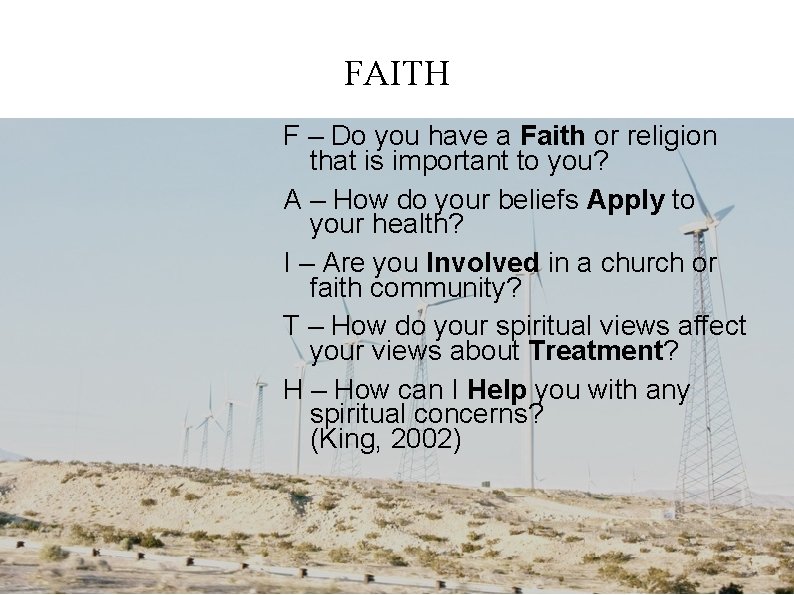
FAITH F – Do you have a Faith or religion that is important to you? A – How do your beliefs Apply to your health? I – Are you Involved in a church or faith community? T – How do your spiritual views affect your views about Treatment? H – How can I Help you with any spiritual concerns? (King, 2002)
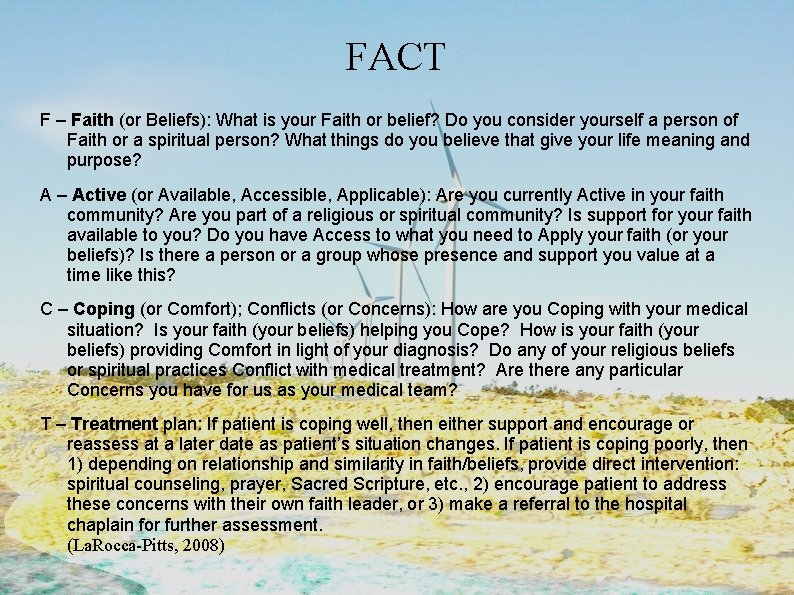
FACT F – Faith (or Beliefs): What is your Faith or belief? Do you consider yourself a person of Faith or a spiritual person? What things do you believe that give your life meaning and purpose? A – Active (or Available, Accessible, Applicable): Are you currently Active in your faith community? Are you part of a religious or spiritual community? Is support for your faith available to you? Do you have Access to what you need to Apply your faith (or your beliefs)? Is there a person or a group whose presence and support you value at a time like this? C – Coping (or Comfort); Conflicts (or Concerns): How are you Coping with your medical situation? Is your faith (your beliefs) helping you Cope? How is your faith (your beliefs) providing Comfort in light of your diagnosis? Do any of your religious beliefs or spiritual practices Conflict with medical treatment? Are there any particular Concerns you have for us as your medical team? T – Treatment plan: If patient is coping well, then either support and encourage or reassess at a later date as patient’s situation changes. If patient is coping poorly, then 1) depending on relationship and similarity in faith/beliefs, provide direct intervention: spiritual counseling, prayer, Sacred Scripture, etc. , 2) encourage patient to address these concerns with their own faith leader, or 3) make a referral to the hospital chaplain for further assessment. (La. Rocca-Pitts, 2008)
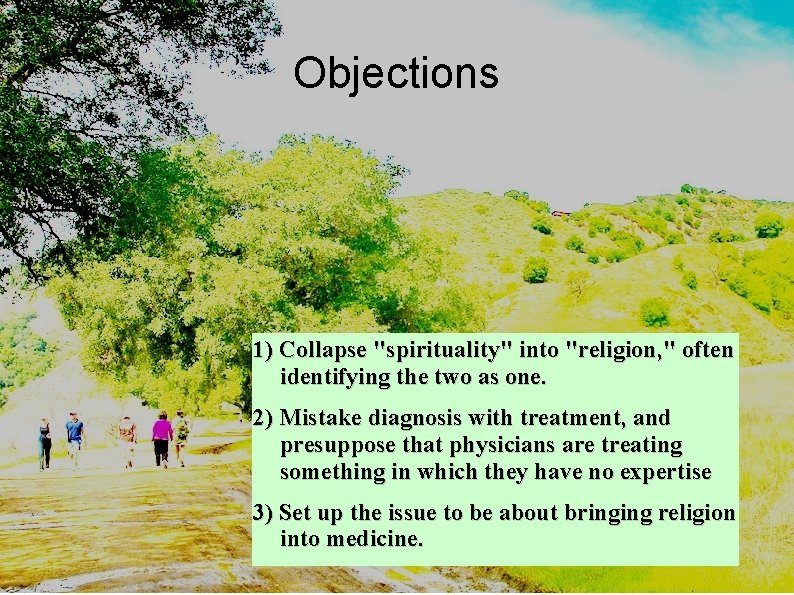
Objections 1) Collapse "spirituality" into "religion, " often identifying the two as one. 2) Mistake diagnosis with treatment, and presuppose that physicians are treating something in which they have no expertise 3) Set up the issue to be about bringing religion into medicine.
Professional and Ethical Guidelines 1)Assessment and History Tools should not become rigid checklists, but aid in fiduciary healing relationships 2)Patient privacy should be respected. 3)They are not tools for proselytizing or imposing a certain religious belief 4)They are not substitutes for professional spiritual care providers. Physicians must try to be as non-judgmental as possible, but there are times when the patient's unhealthy beliefs and spiritual practices must be challenged by appropriate spiritual care experts. 5)They are not meant to expose vulnerabilities but areas in which comfort can be provided. 6)Physicians must be aware of their own spiritual values, particularly those regarding their own mortality, so that they could empathize with the patients' responses. These tools can also be used for looking at the physicians' own spiritual history.
tools for self awareness "The essential work of providing spiritual care happens first in the caregivers. To notice the spiritual needs of the dying, they need to be familiar with these transcendent events. Some may object that they can get this only secondhand, by attending to what dying people express. But all self-transcendence in life involves dying because life's decisions always involve a dying to alternatives. . The more they recognize the death in every moment, the better company they will be to the dying and the more readily they will learn life-lessons from them” (Tad Dunne "Spiritual Care at the End of Life").

Spiritual Diagnosis "We are strange creatures, made up of body, mind, and spirit; these are interrelated and react upon one another. Many of our troubles in life are due to this fact, and to our failure to realize the place, function, and sphere of each of these realms. The devil, of course, takes full advantage of this, and attacks us along this line. " (Martyn Lloyd-Jones, MD, assistant physician to Winston Churchill)

Wrong Diagnosis #1: Confusing the physical with the spiritual. We confuse our physical well-being with our spiritual practice. We confuse our relationship to the physical world with the relationship to God. We prescribe more useless spiritual exercises instead of adjusting our attitude and prescribing proper medicine. Wrong Diagnosis #2: Confusing the psychological with the spiritual. Becoming religious may magnify the existing personality traits neurosis and all. Patients who suffer from psychological disorders do not necessarily suffer from spiritual deficiency. There is a distinction between the condition of our soul and the wellbeing of our psycho-social attributes. Wrong Diagnosis #3: Confusing the spiritual with the physical and the psychological, the reverse of the previous 2 wrong diagnoses. It is the propensity to rationalize spiritual sickness and evil, exculpating, evading, excusing, or alleviating responsibility with psychological diatribe or medical lyrics; framing spiritual sickness and resulting immoral behavior as psychological deficiency or inherited biological traits. This is bio-psychological determinism, and it defeats everything we know and cherish about individual freedom and responsibility.
When a person is dying, the least we can afford to let that person retain is the dignity of human freedom. It is much better for the person to seek final forgiveness than to seek the indignity of a thin cover-up.
Nursing Diagnoses Seven Manifestations of Spiritual Distress: +Spiritual pain, as evidenced by expressions of discomfort of suffering relative to one's relationship with God, verbalization of feelings of having a void or lack of spiritual fulfillment, and/or a lack of peace in terms of one's relationship to one's creator. Do you ever feel hurt or pain associated with the spiritual or religious beliefs which you hold? Do you feel pain related to uncertainty or non-belief? +spiritual alienation, as evidenced by expressions of loneliness or the feeling that God seems very far away and remote from one's everyday life, verbalization that one has to depend upon one's self in times of trial or need, and/or a negative attitude toward receiving any comfort or help from God. Do you frequently feel "far away" from God? Does it seem that He is remote and far removed from your everyday life?
+Spiritual anxiety , as evidenced by expression of fear of God's wrath and punishment; fear that God might not take care of one, either immediately or in the future; and/or worry that God is displeased with one's behavior. Are you afraid that God might not take care of your needs? That God might not "be there" when you are in need? +Spiritual guilt, as evidenced by expressions suggesting that one has failed to do the things which he should have done in life and/or done things which were not pleasing to God; articulation of concerns about the "kind" of life one has lived. Have you ever done things which God would be angry at you for? Are you feeling badly about things which you have done or failed to do in your life? +Spiritual anger, as evidenced by expression of frustration or outrage at God for having allowed illness or other trials, comments about the "unfairness" of God, and/or negative remarks about institutionalized religion and/or its ministers or spiritual care givers. Are you angry at God for allowing you to be ill? Do you ever feel like blaming God for your illness? Do you think God is unfair to you?
+Spiritual loss, as evidenced by expression of feelings of having temporarily lost or terminated the love of God, fear that one's relationship with God has been threatened, and/or a feeling of emptiness with regard to spiritual things. Do you ever feel that you have lost God's love? That you have broken or weakened your relationship with God? Has God turned His back on you? +Spiritual despair, as evidenced by expressions suggesting that there is no hope of ever having a relationship with God or of pleasing Him and/or a feeling that God no longer can or does care for one. " Do you ever feel that there is no hope of having God's love? Of pleasing God? That God doesn't love you anymore? " (www. learnwell. org, based on O'Brien, pp. 102, 106, 107)
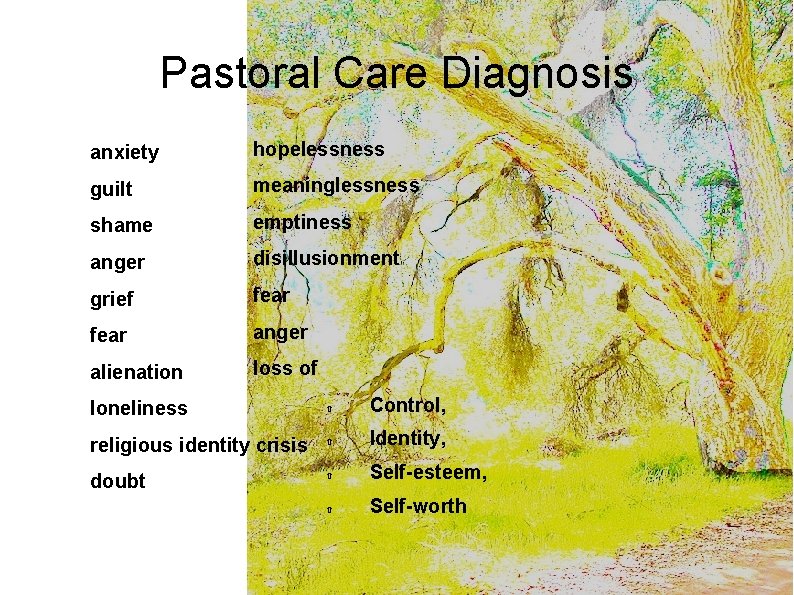
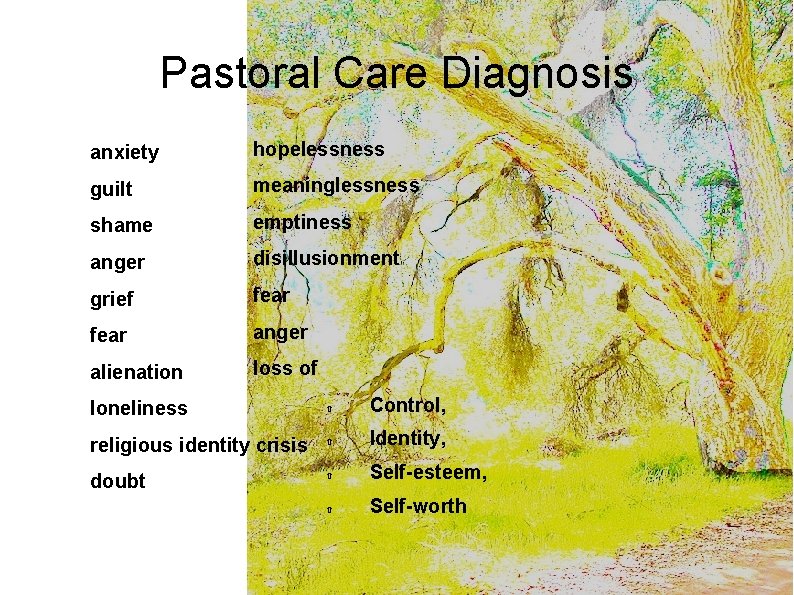
Pastoral Care Diagnosis anxiety hopelessness guilt meaninglessness shame emptiness anger disillusionment grief fear anger alienation loss of loneliness Control, religious identity crisis Identity, doubt Self-esteem, Self-worth

Treatment plan and Intervention Meditation and peaceful prayer practices Rituals Confession and reconciliation Symbols and rituals such as Anointing, Commendation Focus chants Narrative, stories, poetry, art, films Support groups (use technology, networking) Books Journaling Reconciliation with family and friends Communication: Listening, Accepting what the patient says, Validation, Self disclosure, Being present, Touch, Intimacy.
End-of-Life Spiritual Goals Love Peace Acceptance Comfort Reconciliation and Forgiveness Faith Hope Legacy Remembrance
Xroads of spirituality and ethics Spirituality. . . Provides moral authority grounded in common humanity, Common language of morality and common currency, Moral impetus, Narrative content of ethical situations, Poses the moral questions or concerns. Ethics. . . Situates spirituality in concrete form, Provides boundaries for spiritual care providers, Philosophical foundation and methodological consistency for spirituality, Deciphers bogus claims and genuine spiritual values

An Ethic of Spirituality Health care givers should engage in spirituality discourse, guided by an ethic of friendship, and marked by wisdom, candor, and respect for patient autonomy--which is consistent with the principle value of benevolence (Curlin & Hall “Strangers or Friend, ” 2008). To relieve suffering, neutrality is not an ethical value, nor an option, nor even possible.
 End to end accounting life cycle tasks
End to end accounting life cycle tasks End-to-end procurement life cycle
End-to-end procurement life cycle Benedictine spirituality in everyday life
Benedictine spirituality in everyday life Importance of spirituality
Importance of spirituality What is micro-ethics
What is micro-ethics Front end and back end in compiler design
Front end and back end in compiler design Front end compiler
Front end compiler Descriptive ethics
Descriptive ethics Briefly summarise
Briefly summarise Factual inquiry in ethics
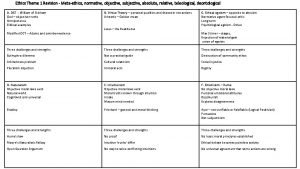
Factual inquiry in ethics Metaethics vs normative ethics
Metaethics vs normative ethics Descriptive ethics vs normative ethics
Descriptive ethics vs normative ethics Beneficence
Beneficence Is/ought distinction
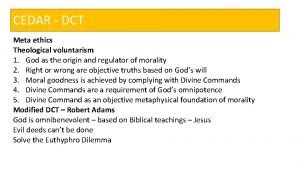
Is/ought distinction Branches of ethics
Branches of ethics Deontology examples
Deontology examples Teleological ethics vs deontological ethics
Teleological ethics vs deontological ethics End of the act in ethics
End of the act in ethics Reds motivational interviewing
Reds motivational interviewing Ways to improve spiritual wellness
Ways to improve spiritual wellness Ottawa school of theology and spirituality
Ottawa school of theology and spirituality Spirituality and addiction
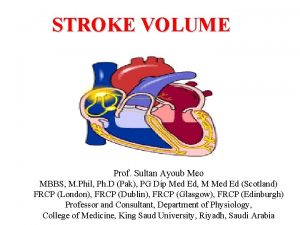
Spirituality and addiction Heart stroke volume
Heart stroke volume Preload stroke volume
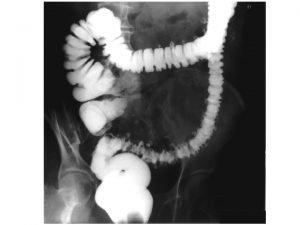
Preload stroke volume End zu end descendorektostomie
End zu end descendorektostomie End-to-end wireframe parsing
End-to-end wireframe parsing End to end argument
End to end argument End to end delay
End to end delay End to end delay
End to end delay End to end
End to end Comet knowledge graph
Comet knowledge graph Aristotle ethics happiness
Aristotle ethics happiness Cornelia m. ruland
Cornelia m. ruland Spirituality
Spirituality Spirituality meaning
Spirituality meaning Salesian youth spirituality
Salesian youth spirituality Aboriginal spirituality sacred texts
Aboriginal spirituality sacred texts Mi'kmaq feather
Mi'kmaq feather Spirituality vs religion
Spirituality vs religion Spirituality definition
Spirituality definition