Dry eye something new Wayne Gillan Definition Dry

- Slides: 29
Dry eye: something new? Wayne Gillan
Definition • Dry eye is a multifactorial disease of the tears and ocular surface that results in symptoms of discomfort, visual disturbance and tear film instability with potential damage to the ocular surface. It is accompanied by increased osmolarity of the tear film and inflammation of the ocular surface (DEWS The Oc Surf 2007 75 -92)
Challenges in epidemiology • There is no single diagnostic test • There is no correlation between signs and • • • symptoms There is poor repeatability in clinical tests Questionnaires are the most repeatable diagnostic tests (symptoms are the reason that patients present to you) (DEWS the Oc Surf 2007 93 -106)
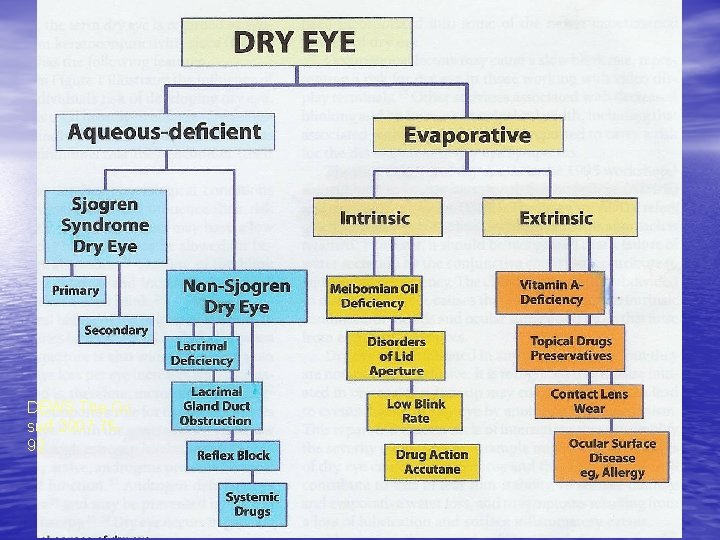
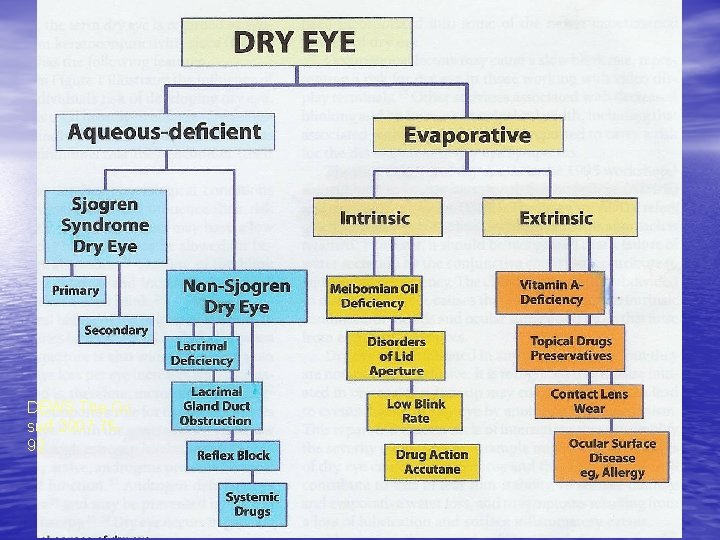
DEWS The Oc surf 2007 7592
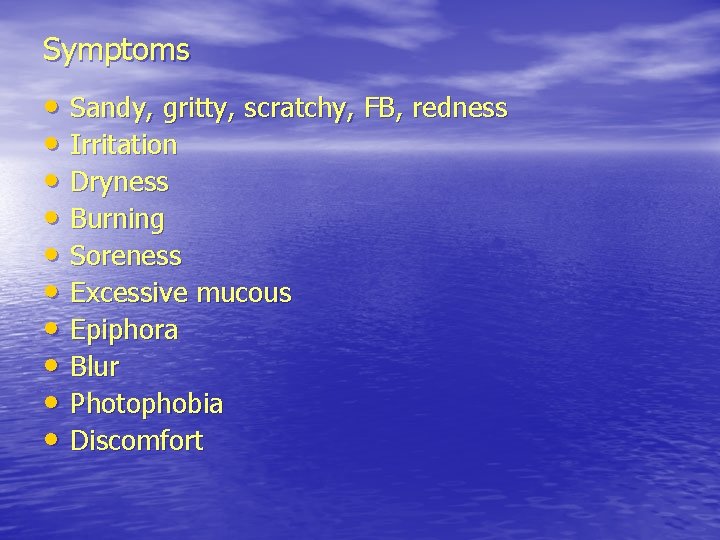
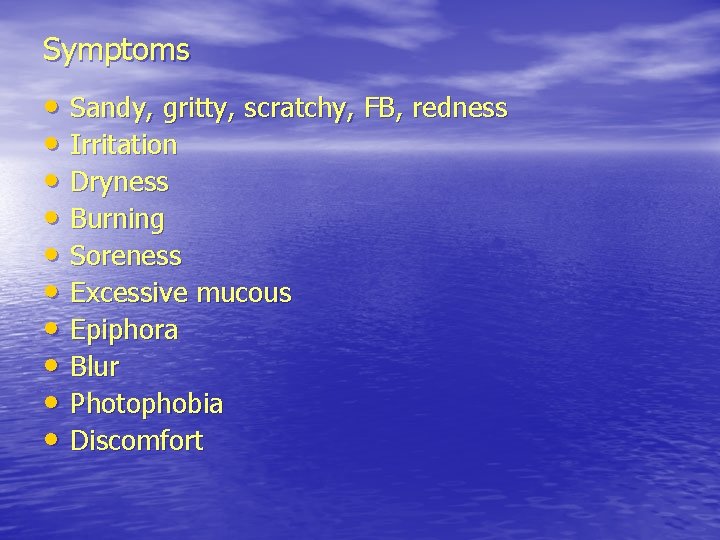
Symptoms • Sandy, gritty, scratchy, FB, redness • Irritation • Dryness • Burning • Soreness • Excessive mucous • Epiphora • Blur • Photophobia • Discomfort
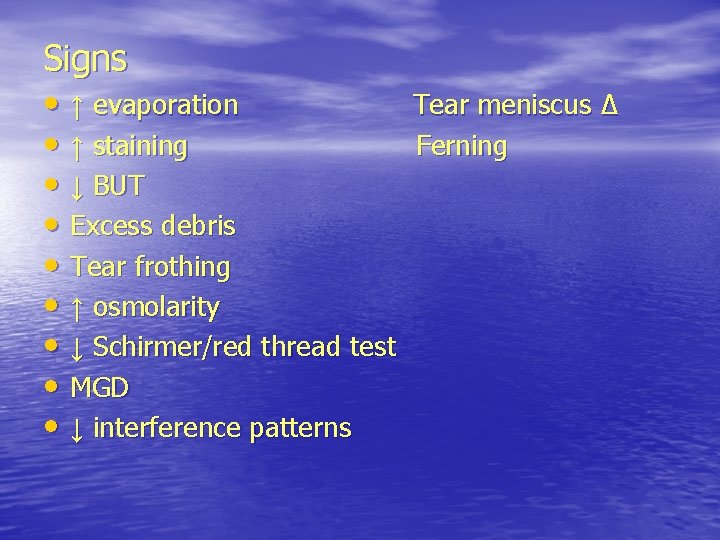
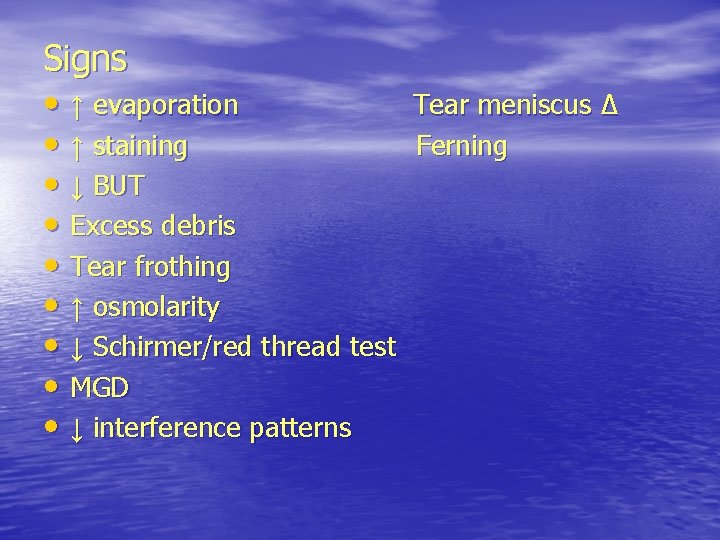
Signs • ↑ evaporation Tear meniscus Δ • ↑ staining Ferning • ↓ BUT • Excess debris • Tear frothing • ↑ osmolarity • ↓ Schirmer/red thread test • MGD • ↓ interference patterns

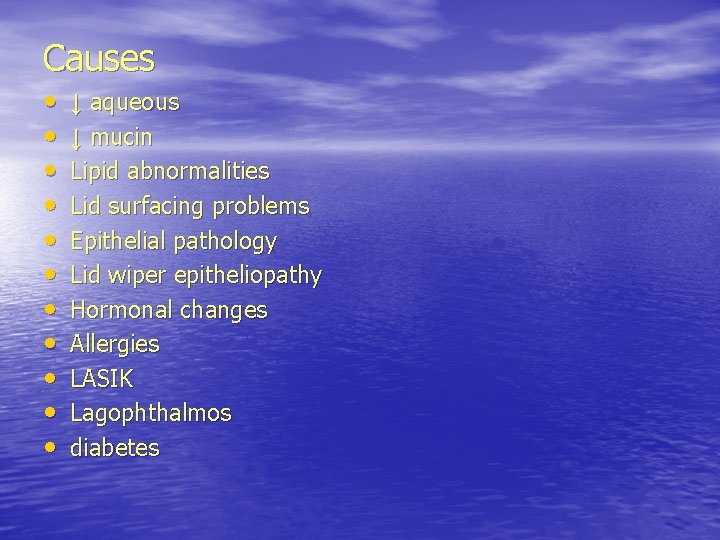
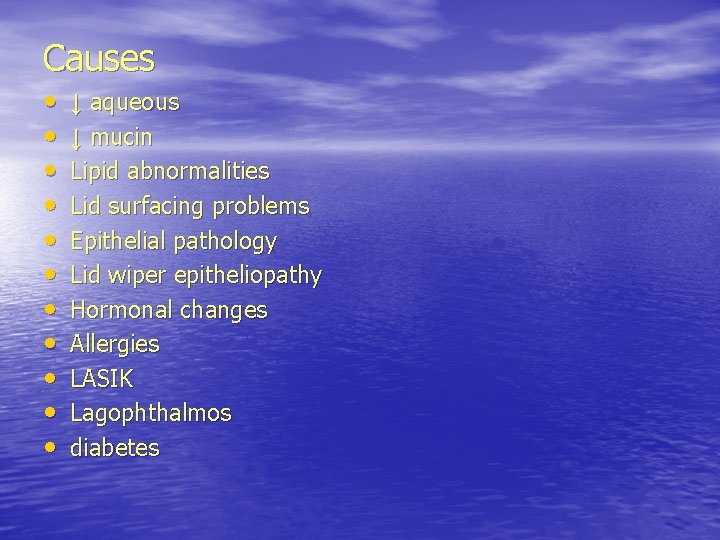
Causes • • • ↓ aqueous ↓ mucin Lipid abnormalities Lid surfacing problems Epithelial pathology Lid wiper epitheliopathy Hormonal changes Allergies LASIK Lagophthalmos diabetes
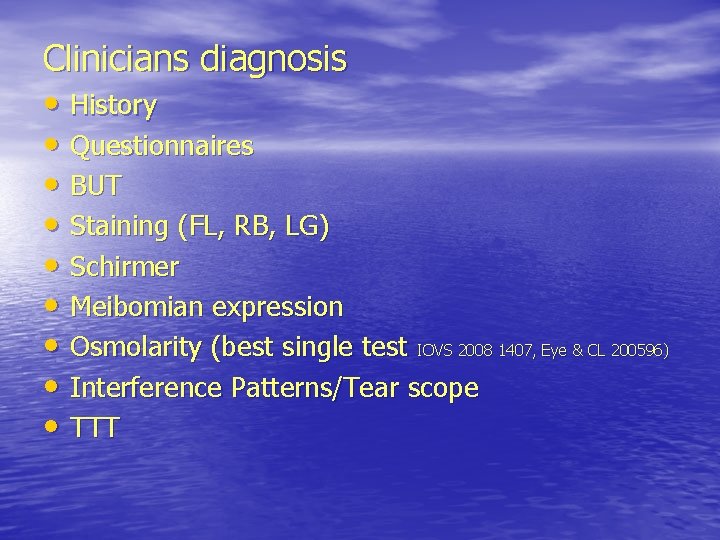
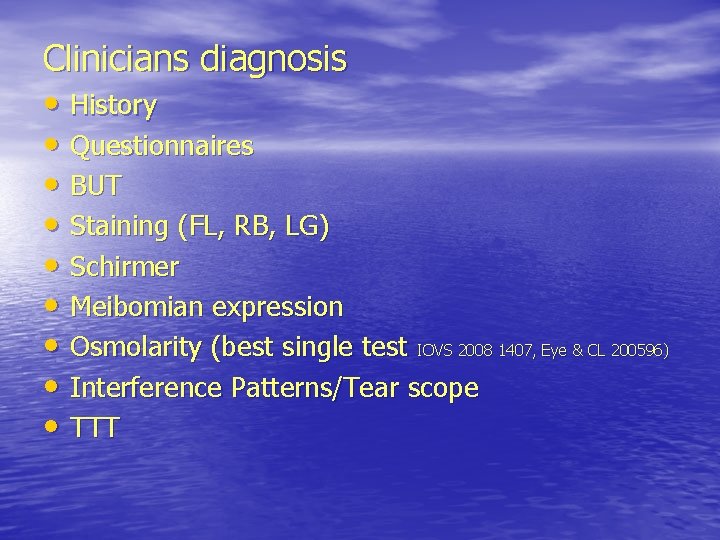
Clinicians diagnosis • History • Questionnaires • BUT • Staining (FL, RB, LG) • Schirmer • Meibomian expression • Osmolarity (best single test IOVS 2008 1407, Eye & CL 200596) • Interference Patterns/Tear scope • TTT
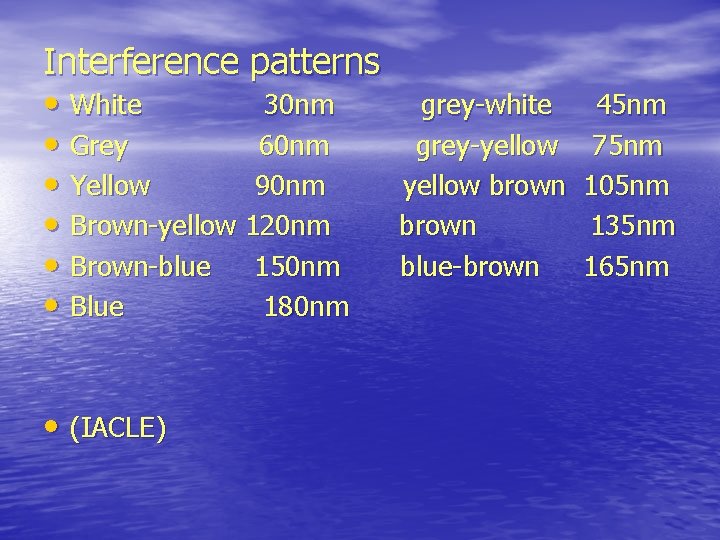
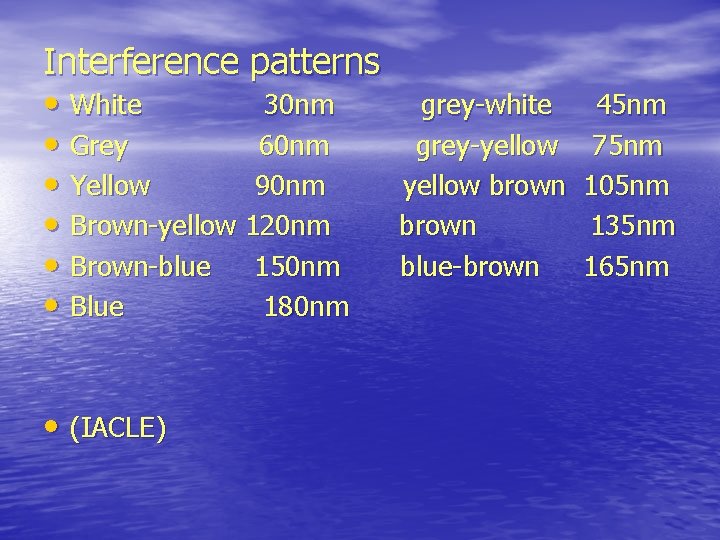
Interference patterns • White 30 nm • Grey 60 nm • Yellow 90 nm • Brown-yellow 120 nm • Brown-blue 150 nm • Blue 180 nm • (IACLE) grey-white grey-yellow brown blue-brown 45 nm 75 nm 105 nm 135 nm 165 nm
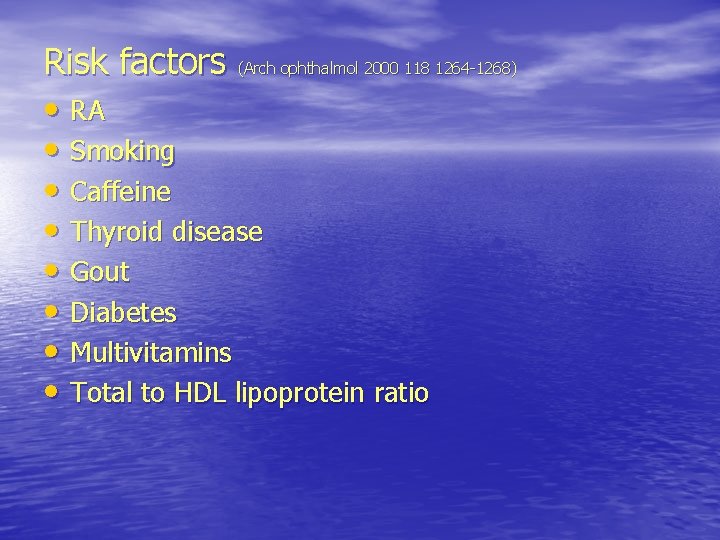
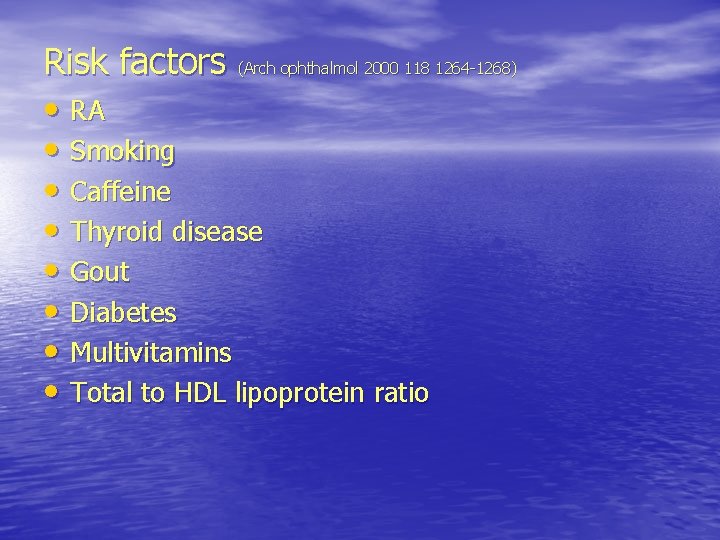
Risk factors (Arch ophthalmol 2000 118 1264 -1268) • RA • Smoking • Caffeine • Thyroid disease • Gout • Diabetes • Multivitamins • Total to HDL lipoprotein ratio
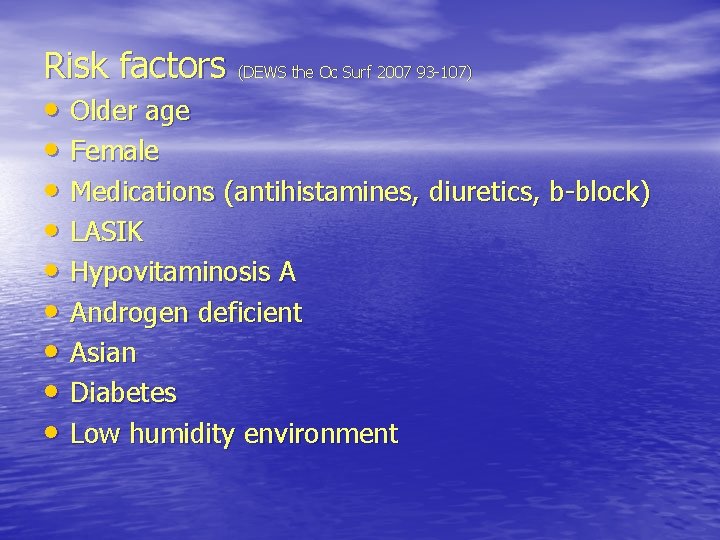
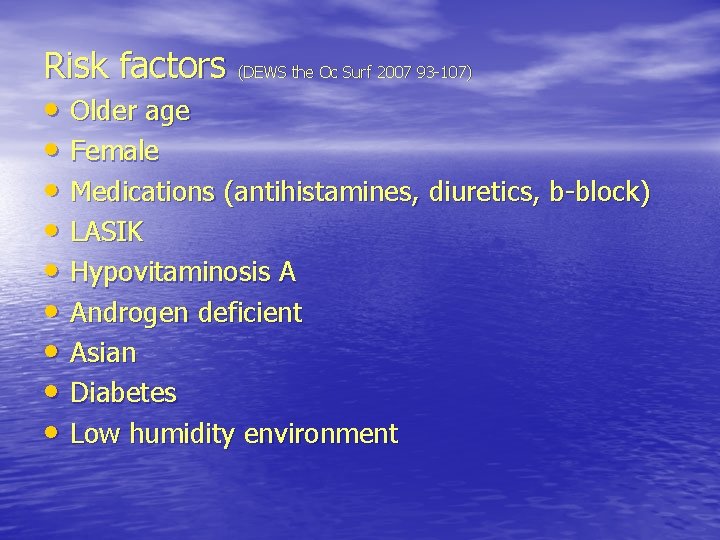
Risk factors (DEWS the Oc Surf 2007 93 -107) • Older age • Female • Medications (antihistamines, diuretics, b-block) • LASIK • Hypovitaminosis A • Androgen deficient • Asian • Diabetes • Low humidity environment
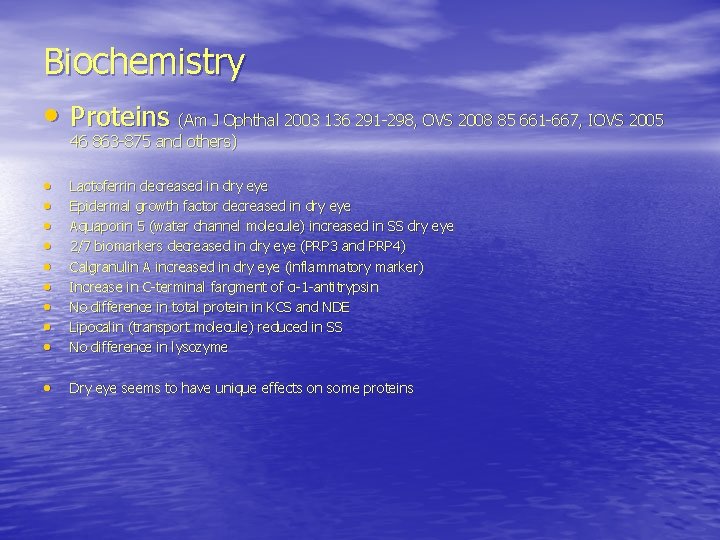
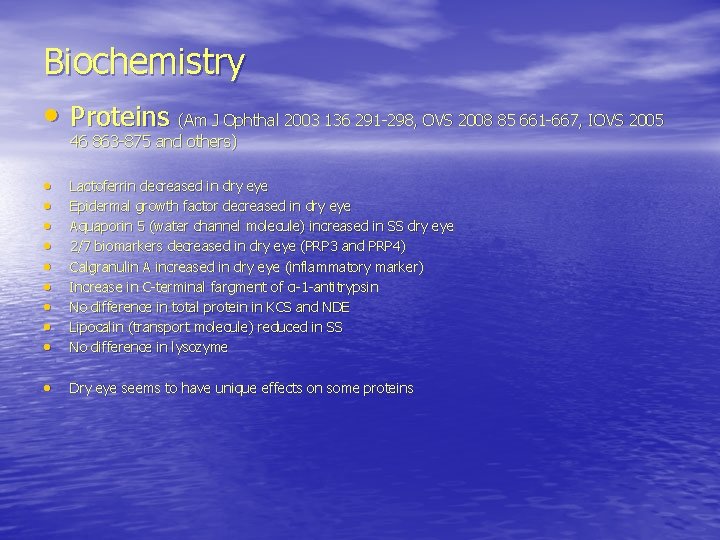
Biochemistry • Proteins (Am J Ophthal 2003 136 291 -298, OVS 2008 85 661 -667, IOVS 2005 46 863 -875 and others) • • • Lactoferrin decreased in dry eye Epidermal growth factor decreased in dry eye Aquaporin 5 (water channel molecule) increased in SS dry eye 2/7 biomarkers decreased in dry eye (PRP 3 and PRP 4) Calgranulin A increased in dry eye (inflammatory marker) Increase in C-terminal fargment of α-1 -antitrypsin No difference in total protein in KCS and NDE Lipocalin (transport molecule) reduced in SS No difference in lysozyme • Dry eye seems to have unique effects on some proteins
• Lipids (meibomian gland) (J lipid res 2007 48 2220 -2235, Arch Ophthal 2006 124 1286 -1292, IOVS 2008 49 3779 -3789 and others) • Oleic acid, stearic acid, wax esters, cholesterol esters • Aging associated with significant changes in lipid profile ( ↑ dry eye with age) • Androgen deficiency seems implicated in cause of dry eye in SS • Thousands of species estimated • Non-polar: sterols, steryl esters, acyl glycerols, hydroxy fatty acids, fatty acid amides • (presently involved with M student)
• Mucins (IOVS 1998 39 2602 -2609, OVS 2008 85 631 -642, IOVS 2002 43 10041010 and others) • Alteration in mucin distribution or glycosylation in dry eye • Glycosylation changes with disease • Mucin gene expression and secretion may be deficient in dry eye • MUC 5 AC (secreted mucin)↓ associated with ↓goblet cell density in dry eye • MUC 1 (membrane mucin) up-regulated in dry eye • Mucin expression decreased, mutated and under glycosylated in dry eye • Expression seems affected by inflammation and hormone expression (androgens)
• Apoptosis (programmed cell death) (Exp Eye Res 2003 76 233 -240) • Lacrimal gland function related to apoptosis in acinar cells of lacrimal gland • Correlation exists between apoptotic cells and gland function • Fas receptor is a death receptor on cell surface. Fas ligand expression highly correlated with lacrimal gland function
• Inflammation (IOVS 2006 47 2445 -2450, IOVS 2010 51 122 -128, IOVS 2001 42 2283 -2292, IOVS 2004 45 4293 -4301) • No difference in cytokine expression between groups • IL-1β does not play a role • Langerhans cells and leucocytes may play a role in dry eye • IL-1 ↑ in dry eye • TNF-α and MMP-9 ↑ in dry eye • Mitogen-activated protein kinase signaling ↑
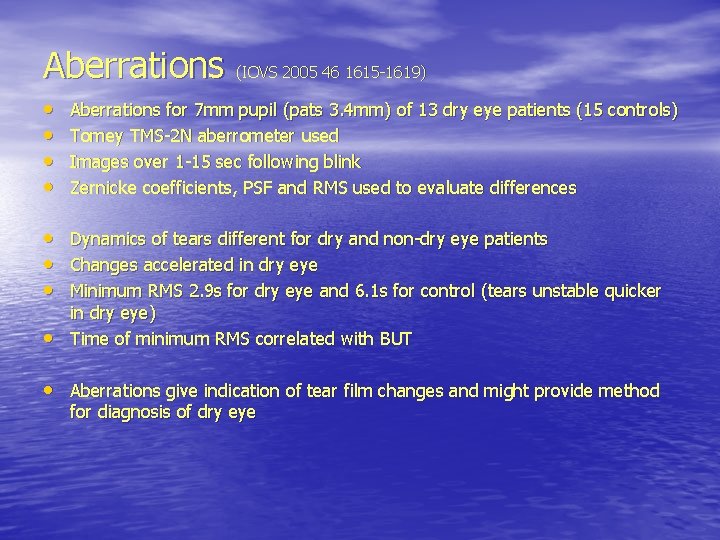
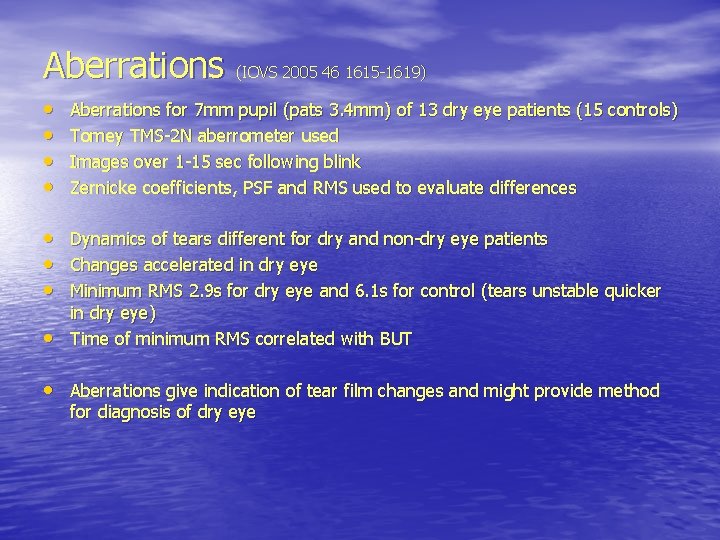
Aberrations (IOVS 2005 46 1615 -1619) • • Aberrations for 7 mm pupil (pats 3. 4 mm) of 13 dry eye patients (15 controls) Tomey TMS-2 N aberrometer used Images over 1 -15 sec following blink Zernicke coefficients, PSF and RMS used to evaluate differences • • • Dynamics of tears different for dry and non-dry eye patients Changes accelerated in dry eye Minimum RMS 2. 9 s for dry eye and 6. 1 s for control (tears unstable quicker in dry eye) Time of minimum RMS correlated with BUT • • Aberrations give indication of tear film changes and might provide method for diagnosis of dry eye
Management • Key factors (IACLE) • ID cause (not so easy to do) • Treat cause, not just effect (not so easy to do) • Many regimens possible • Individualize treatment • Palliative treatment only • Treat promptly if to protect anterior surface of eye
• Tear volume abnormality • ↑ humidity • Avoid drugs that cause problems • Control air-conditioning • Artificial tears • • lacrisert Punctal plugs
• Tear mucin abnormality • Artificial tears • Remove mucous
• Tear lipid abnormality • Eyelid hygiene • Topical antibiotics • Systemic tetracycline
• Surfacing abnormality • Tape eyes shut • Tarsorraphy • Artificial tears • Ointments • Surgery • Scleral shells/semi-scleral lenses
• Classic interventions • Tear substitutes • Ointments • Environmental interventions • Punctal occlusion • Lid hygiene • Tarsorraphy
• Ron and Randall’s approach: • Soothe XP (at least 4 X a day) and lotoprednol 0. 5% (4 X a day) for one month (20 -30 minutes between drops) • At one month: assess success and modify • Assuming success: decrease lotoprednol to BID and decrease frequency of Soothe XP • At 2 months: try stop lotoprednol and continue with artificial tears • Supplement with Omega-3 fish oil • Plug if necessary
• Modern interventions • Scleral/semi-scleral shells (Boston Vision Institute) • Goblet cell stimulation: histamine, antigens, immune complexes • Mucin secretion: 15 -(S)-HETE, Diquafosol tetrasodium, topical corticosteroids, vitamin A, Rebamipide (experimental drug), cyclosporine • Oral administration of Omega-6 fatty acids alleviate dry eye • Topical application of alpha-linolenic acid omega-3 fatty acid (essential FA) • Secretogogues: stimulate aqueous, mucous (or both) secretion. New drugs investigated include: diquafosol, rebapimide, gefarnate and 15 -(S)-HETE • Autologous biological tear substitutes: contain epitheliotrophic factors, immunoglobulins, neurotrophins, vitamins and extracellular matrix protein Serum • Salivary gland autotransplantation
• • • Anti-inflammatory therapy: Cyclosporine immunomodulator (restasis) Corticosteroids Androgens tetracycline (antibiotic, anti-inflammatory and anti-angiogenic) essential fatty acids • Trehalose (disaccharide) produces effects similar to serum and reduces apoptosis • • • Gene therapy (autoimmune disease). Problems: choice of vector spread of vector to other tissue Expression of gene only in special conditions Efficient and low-cost production of vehicle Targets of therapy need to be more carefully defined • •
• Dry eye ubiquitous • Signs and symptoms do not correlate • Diagnosing properly is difficult • Optometry limited in its options • Disease not fully understood
• I qualified in 1979, received a Master’s degree in 1993 and a doctoral degree in 2004. I was a part-time lecturer at the Rand Afrikaans University from 1987 to 2000 and was appointed on a full-time basis from October 2000 (presently the University of Johannesburg). At present I lecture contact lenses and binocular vision to fourth year students. My interests at present are keratoconus, tear biochemistry and contact lenses in general. I have over 60 publications in the local optometry journal (The South African Optometrist). • Affiliates: Employed by the University of Johannesburg, Fellow of the South African Optometric Association, Fellow of the American Academy of Optometry, FIACLE. I think that is all.