Tearing hyperlacrimation epiphora Dry eye tear breakup time
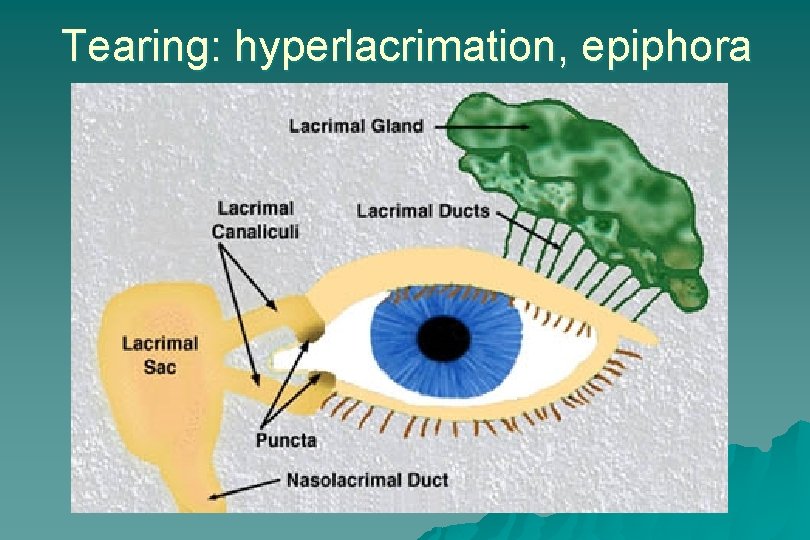
Tearing: hyperlacrimation, epiphora

Dry eye: tear break-up time, Schirmer test
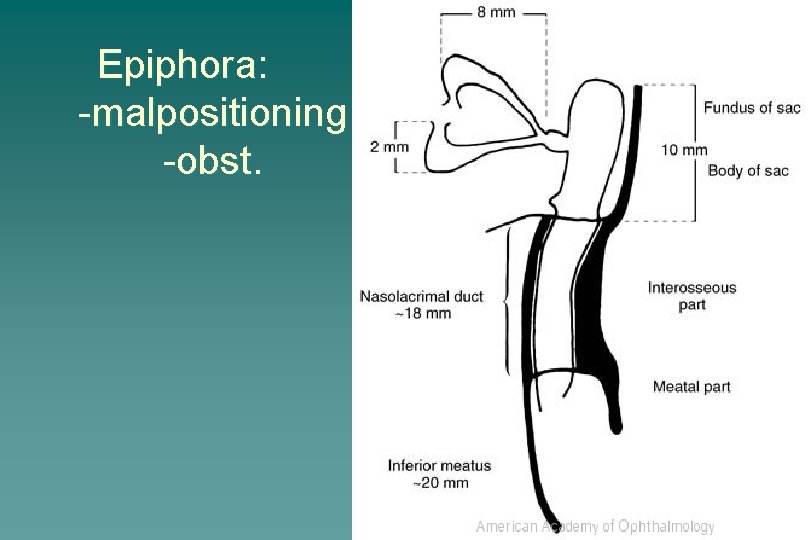
Epiphora: -malpositioning -obst.
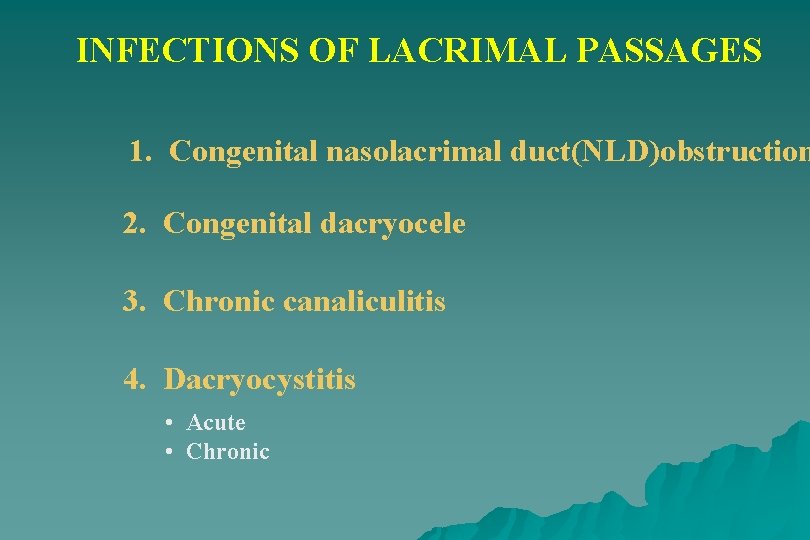
INFECTIONS OF LACRIMAL PASSAGES 1. Congenital nasolacrimal duct(NLD)obstruction 2. Congenital dacryocele 3. Chronic canaliculitis 4. Dacryocystitis • Acute • Chronic
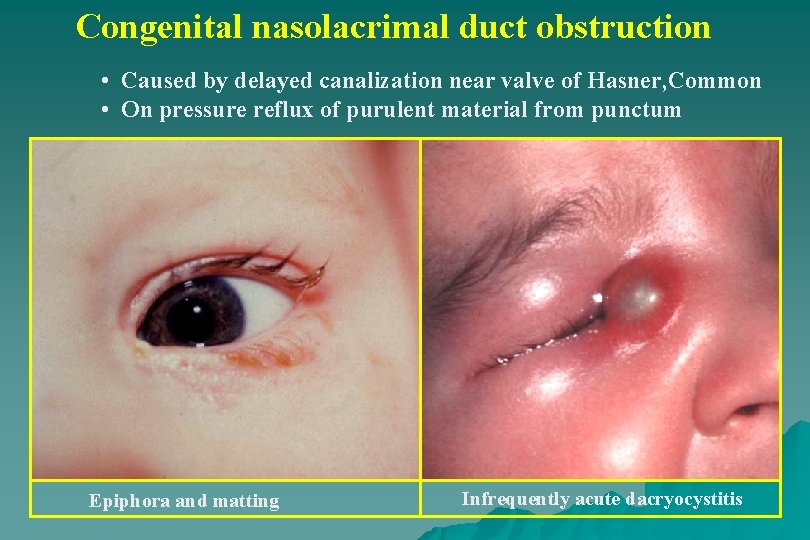
Congenital nasolacrimal duct obstruction • Caused by delayed canalization near valve of Hasner, Common • On pressure reflux of purulent material from punctum Epiphora and matting Infrequently acute dacryocystitis
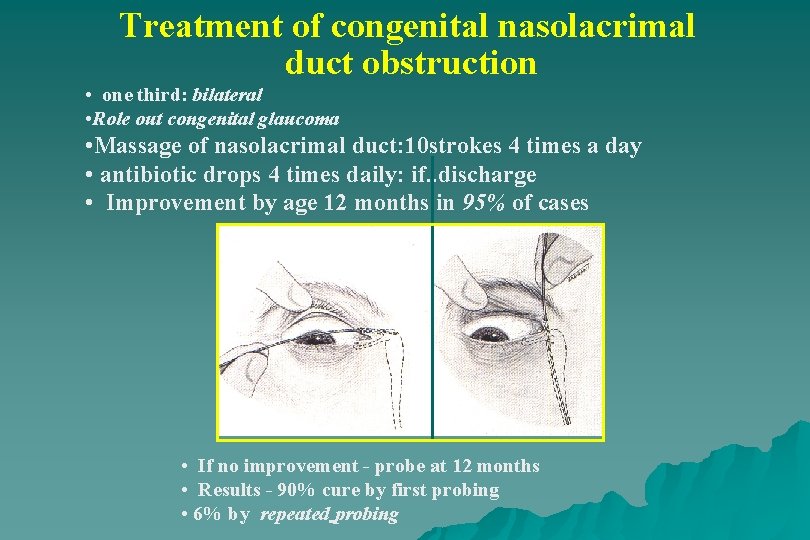
Treatment of congenital nasolacrimal duct obstruction • one third: bilateral • Role out congenital glaucoma • Massage of nasolacrimal duct: 10 strokes 4 times a day • antibiotic drops 4 times daily: if. . discharge • Improvement by age 12 months in 95% of cases • If no improvement - probe at 12 months • Results - 90% cure by first probing • 6% by repeated probing
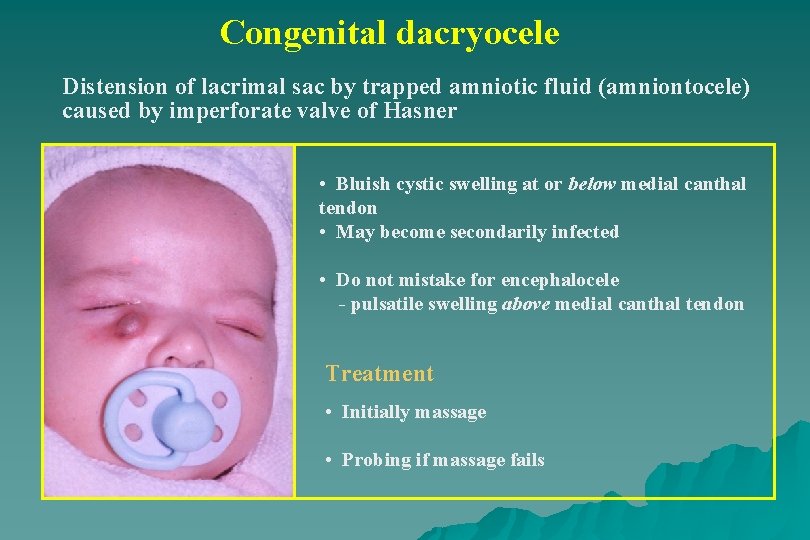
Congenital dacryocele Distension of lacrimal sac by trapped amniotic fluid (amniontocele) caused by imperforate valve of Hasner • Bluish cystic swelling at or below medial canthal tendon • May become secondarily infected • Do not mistake for encephalocele - pulsatile swelling above medial canthal tendon Treatment • Initially massage • Probing if massage fails
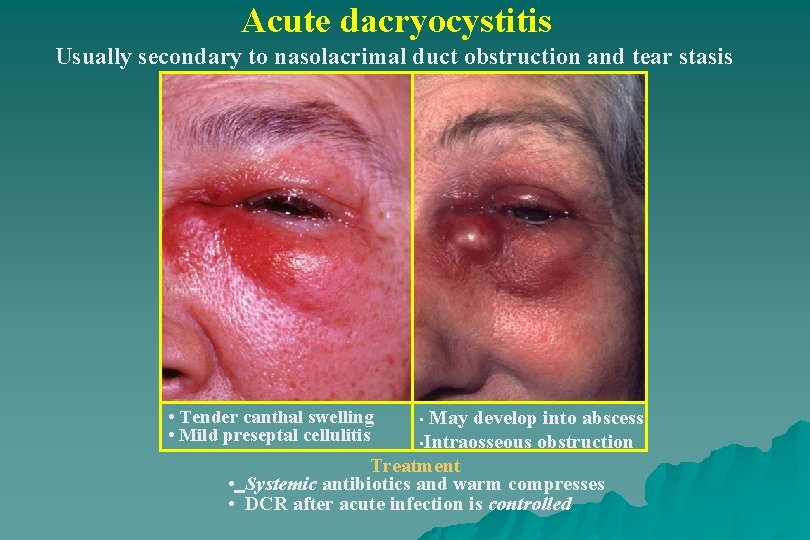
Acute dacryocystitis Usually secondary to nasolacrimal duct obstruction and tear stasis • Tender canthal swelling • Mild preseptal cellulitis May develop into abscess • Intraosseous obstruction Treatment • Systemic antibiotics and warm compresses • DCR after acute infection is controlled •

Chronic dacryocystitis Epiphora and chronic or recurrent unilateral conjunctivitis Painless swelling at inner canthus Expressed mucopurulent material Treatment - DCR
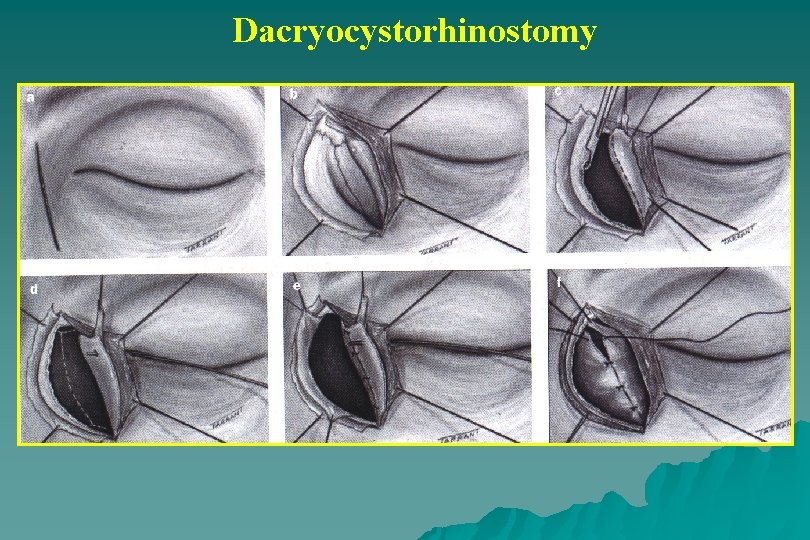
Dacryocystorhinostomy
- Slides: 10