Delawares Health Insurance Marketplace Update on Activity Delaware


- Slides: 34
Delaware’s Health Insurance Marketplace: Update on Activity Delaware Health Care Commission, June 5, 2014 Secretary Rita Landgraf, Department of Health and Social Services Commissioner Karen Weldin Stewart, Department of Insurance
Agenda • Secretary Landgraf ü Enrollment Update ü Important Consumer Information • Commissioner Stewart ü Regulatory Updates ü Employer-based Coverage and SHOP for 2015 ü The Role of Agents and Brokers ü Plan Management Update 2
Enrollment Update
Marketplace Enrollment Update: Paid Premiums 14, 397: Marketplace plan enrollment for first Open Enrollment (as reported by the Insurers) as of April 15, 2014, and communicated at the May 6, 2014, HCC meeting. 11, 961 (83%): Number of enrollees who have paid the first month’s premium to effectuate (begin) coverage. 4
Total Enrollment Update • As of May 30, 2014, 5, 793 individuals have enrolled in Medicaid through the expansion. • This is a 37% increase since April 15 th. 20, 190 Delawareans have enrolled in health care coverage through expanded Medicaid and the Marketplace since October 1, 2013. 5
Important Consumer Reminders
Special Enrollment Period: COBRA coverage • Individuals who have COBRA continuation coverage may qualify for a Special Enrollment Period for a limited time. This allows them to enroll in a Marketplace plan instead. • The deadline to enroll in a new plan during this one-time Special Enrollment Period is July 1, 2014. • To do this, contact the Marketplace Call Center at 1 -800 -318 -2596 (TTY: 1 -855 -889 -4325). Once individuals are approved for a Special Enrollment Period, they can apply for and enroll in a Marketplace plan either online or by phone. • For more information: https: //www. healthcare. gov/what-if-icurrently-have-cobra-coverage/ 7
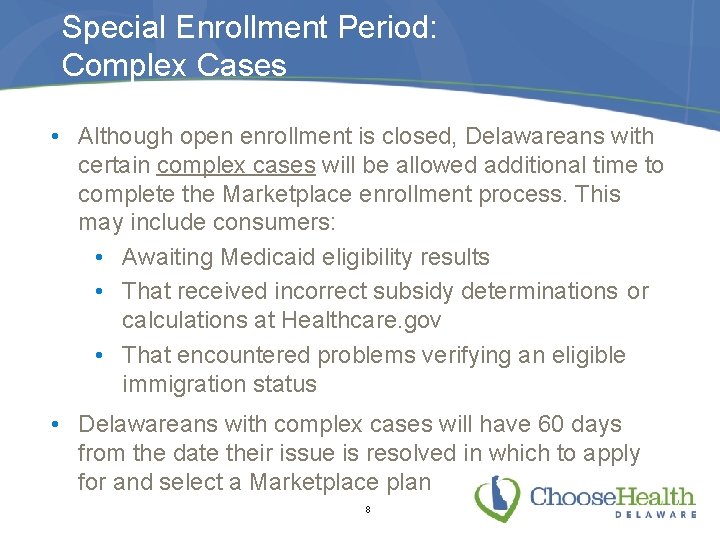
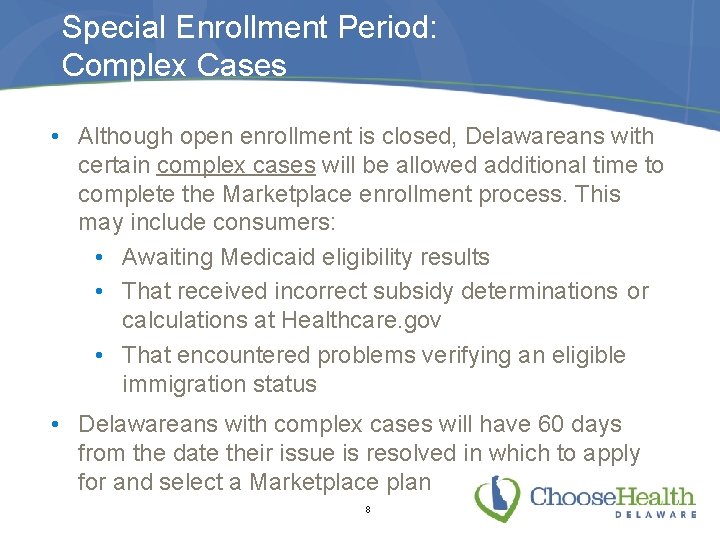
Special Enrollment Period: Complex Cases • Although open enrollment is closed, Delawareans with certain complex cases will be allowed additional time to complete the Marketplace enrollment process. This may include consumers: • Awaiting Medicaid eligibility results • That received incorrect subsidy determinations or calculations at Healthcare. gov • That encountered problems verifying an eligible immigration status • Delawareans with complex cases will have 60 days from the date their issue is resolved in which to apply for and select a Marketplace plan 8
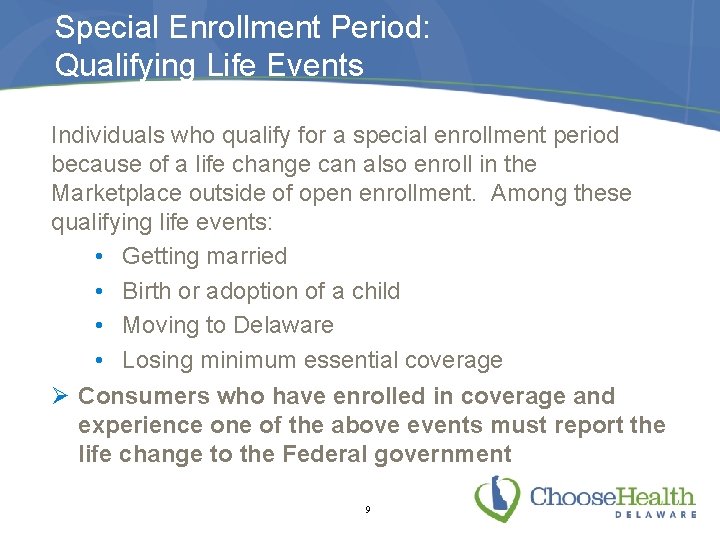
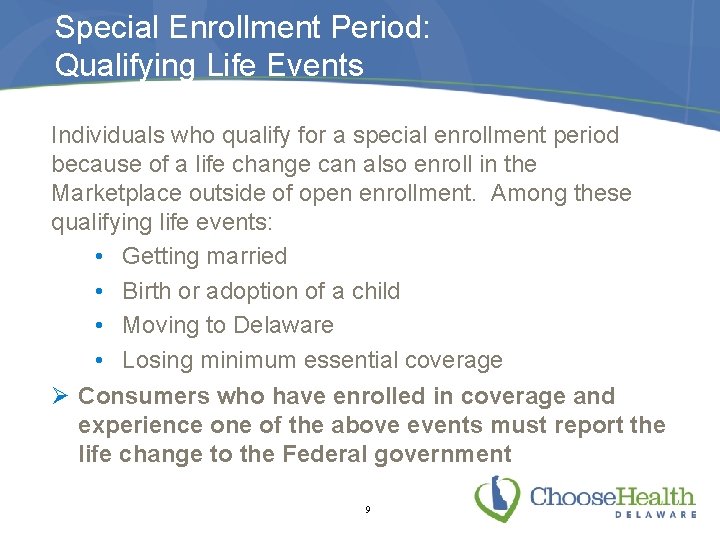
Special Enrollment Period: Qualifying Life Events Individuals who qualify for a special enrollment period because of a life change can also enroll in the Marketplace outside of open enrollment. Among these qualifying life events: • Getting married • Birth or adoption of a child • Moving to Delaware • Losing minimum essential coverage Ø Consumers who have enrolled in coverage and experience one of the above events must report the life change to the Federal government 9
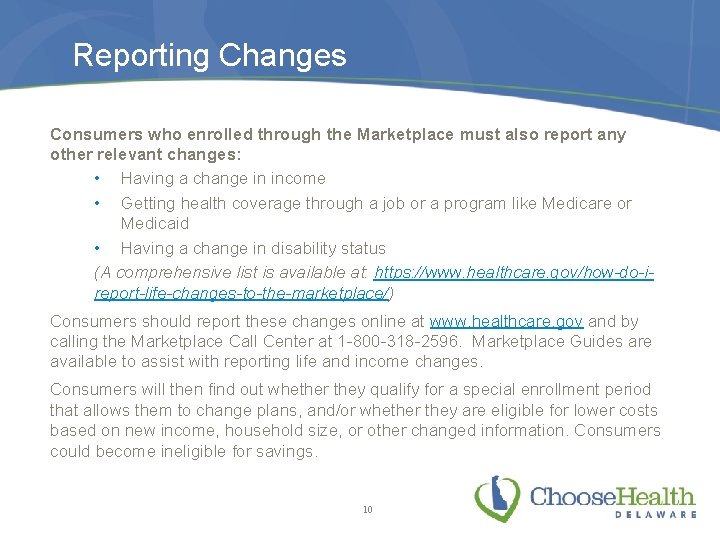
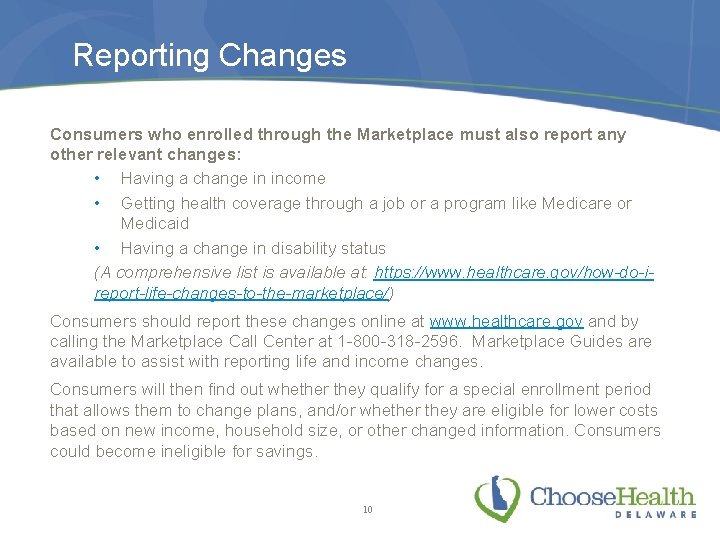
Reporting Changes Consumers who enrolled through the Marketplace must also report any other relevant changes: • Having a change in income • Getting health coverage through a job or a program like Medicare or Medicaid • Having a change in disability status (A comprehensive list is available at: https: //www. healthcare. gov/how-do-ireport-life-changes-to-the-marketplace/) Consumers should report these changes online at www. healthcare. gov and by calling the Marketplace Call Center at 1 -800 -318 -2596. Marketplace Guides are available to assist with reporting life and income changes. Consumers will then find out whether they qualify for a special enrollment period that allows them to change plans, and/or whether they are eligible for lower costs based on new income, household size, or other changed information. Consumers could become ineligible for savings. 10
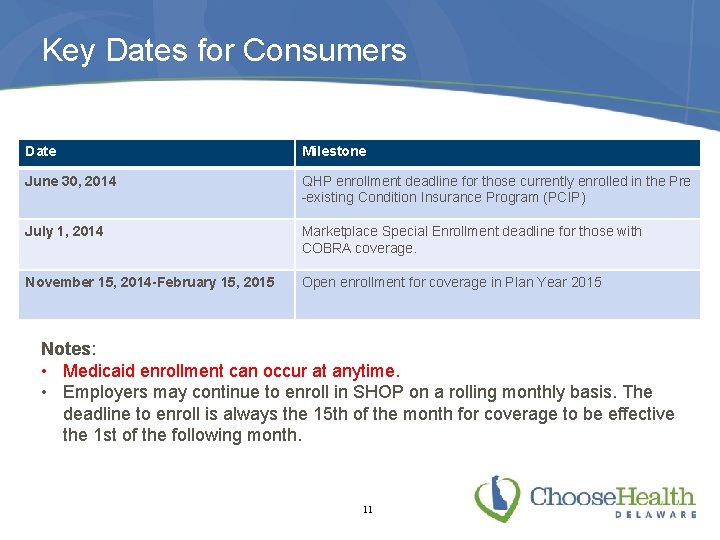
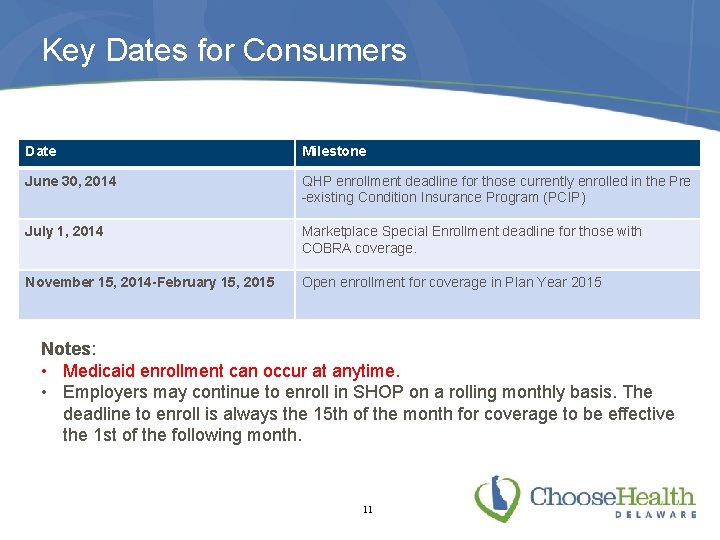
Key Dates for Consumers Date Milestone June 30, 2014 QHP enrollment deadline for those currently enrolled in the Pre -existing Condition Insurance Program (PCIP) July 1, 2014 Marketplace Special Enrollment deadline for those with COBRA coverage. November 15, 2014 -February 15, 2015 Open enrollment for coverage in Plan Year 2015 Notes: • Medicaid enrollment can occur at anytime. • Employers may continue to enroll in SHOP on a rolling monthly basis. The deadline to enroll is always the 15 th of the month for coverage to be effective the 1 st of the following month. 11

Highlights of Recent Regulatory Guidance
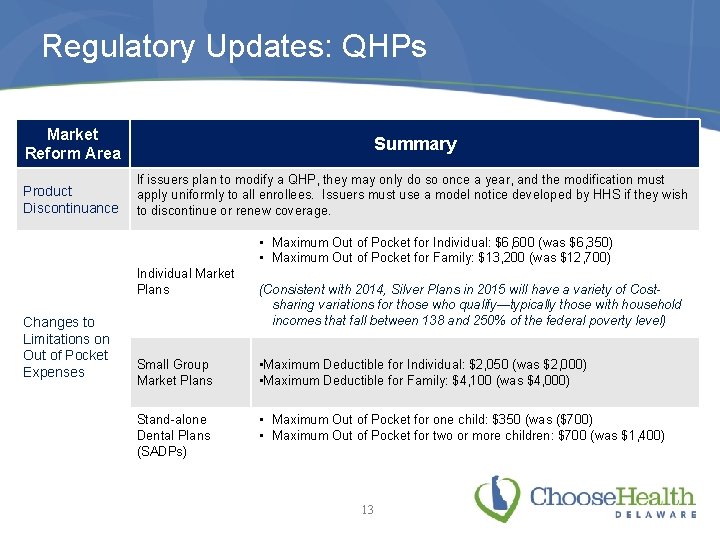
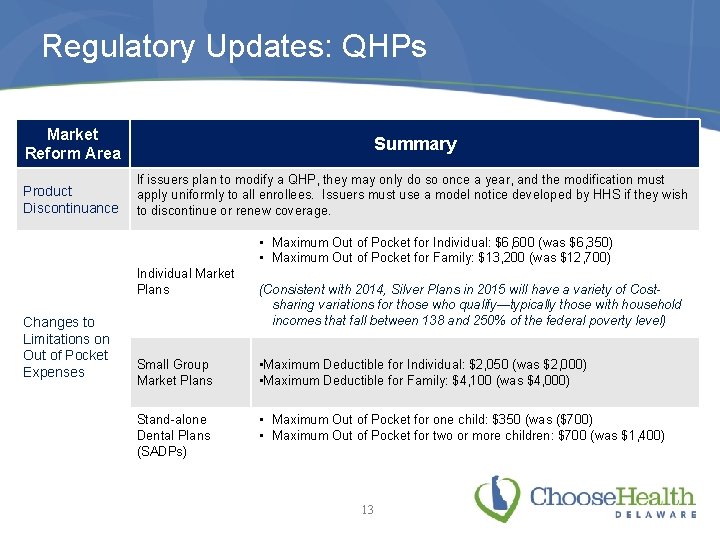
Regulatory Updates: QHPs Market Reform Area Summary Product Discontinuance If issuers plan to modify a QHP, they may only do so once a year, and the modification must apply uniformly to all enrollees. Issuers must use a model notice developed by HHS if they wish to discontinue or renew coverage. • Maximum Out of Pocket for Individual: $6, 600 (was $6, 350) • Maximum Out of Pocket for Family: $13, 200 (was $12, 700) Individual Market Plans Changes to Limitations on Out of Pocket Expenses (Consistent with 2014, Silver Plans in 2015 will have a variety of Costsharing variations for those who qualify—typically those with household incomes that fall between 138 and 250% of the federal poverty level) Small Group Market Plans • Maximum Deductible for Individual: $2, 050 (was $2, 000) • Maximum Deductible for Family: $4, 100 (was $4, 000) Stand-alone Dental Plans (SADPs) • Maximum Out of Pocket for one child: $350 (was ($700) • Maximum Out of Pocket for two or more children: $700 (was $1, 400) 13
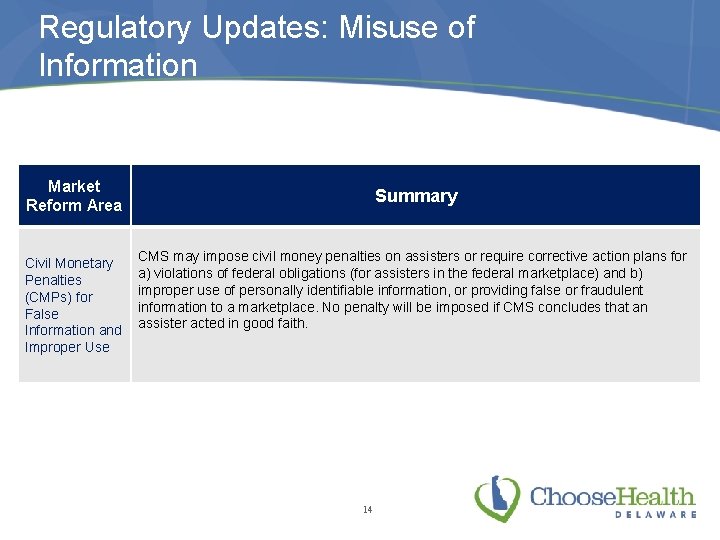
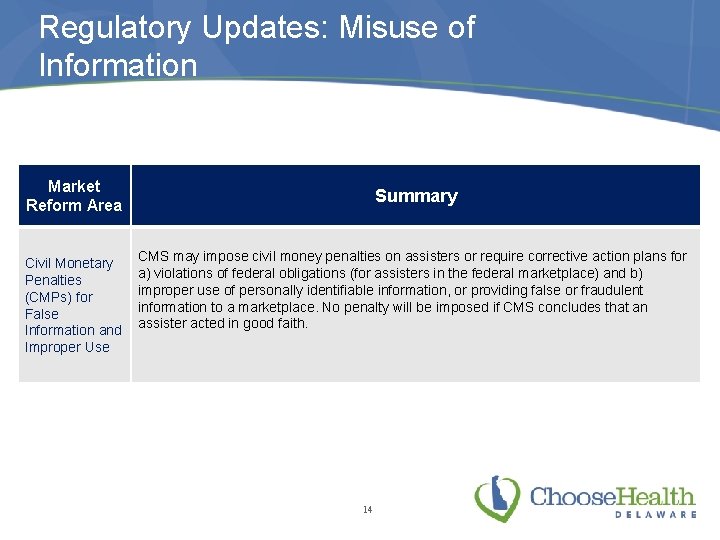
Regulatory Updates: Misuse of Information Market Reform Area Civil Monetary Penalties (CMPs) for False Information and Improper Use Summary CMS may impose civil money penalties on assisters or require corrective action plans for a) violations of federal obligations (for assisters in the federal marketplace) and b) improper use of personally identifiable information, or providing false or fraudulent information to a marketplace. No penalty will be imposed if CMS concludes that an assister acted in good faith. 14
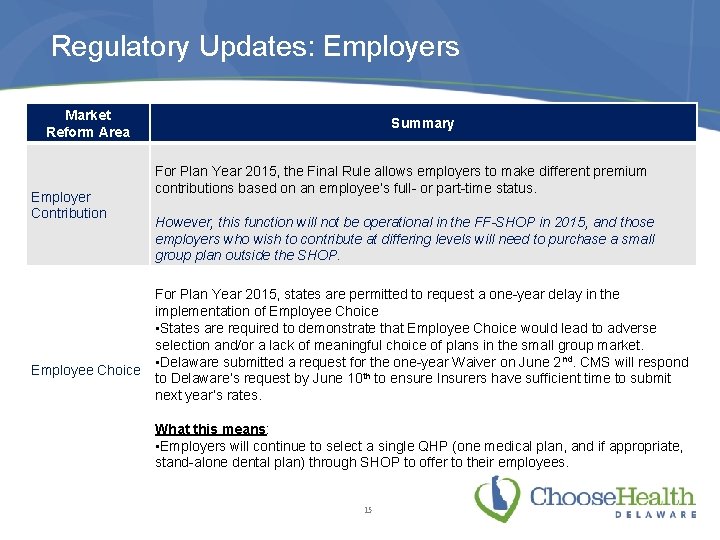
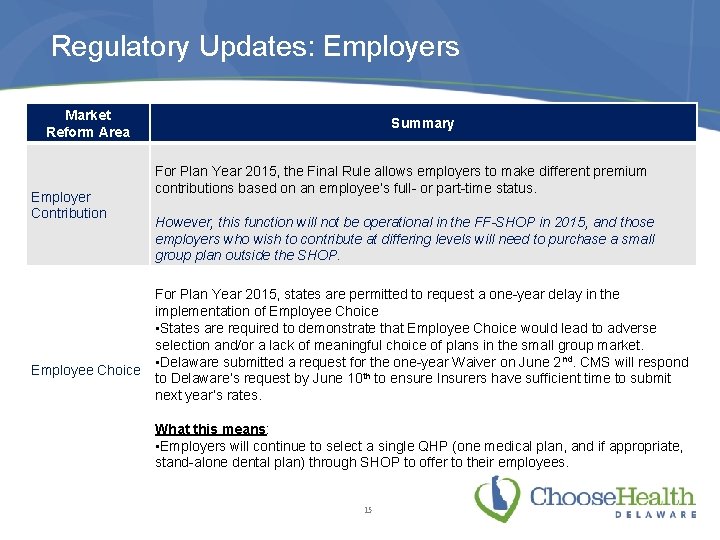
Regulatory Updates: Employers Market Reform Area Employer Contribution Employee Choice Summary For Plan Year 2015, the Final Rule allows employers to make different premium contributions based on an employee’s full- or part-time status. However, this function will not be operational in the FF-SHOP in 2015, and those employers who wish to contribute at differing levels will need to purchase a small group plan outside the SHOP. For Plan Year 2015, states are permitted to request a one-year delay in the implementation of Employee Choice • States are required to demonstrate that Employee Choice would lead to adverse selection and/or a lack of meaningful choice of plans in the small group market. • Delaware submitted a request for the one-year Waiver on June 2 nd. CMS will respond to Delaware’s request by June 10 th to ensure Insurers have sufficient time to submit next year’s rates. What this means: • Employers will continue to select a single QHP (one medical plan, and if appropriate, stand-alone dental plan) through SHOP to offer to their employees. 15
Employer-based Coverage and SHOP for 2015
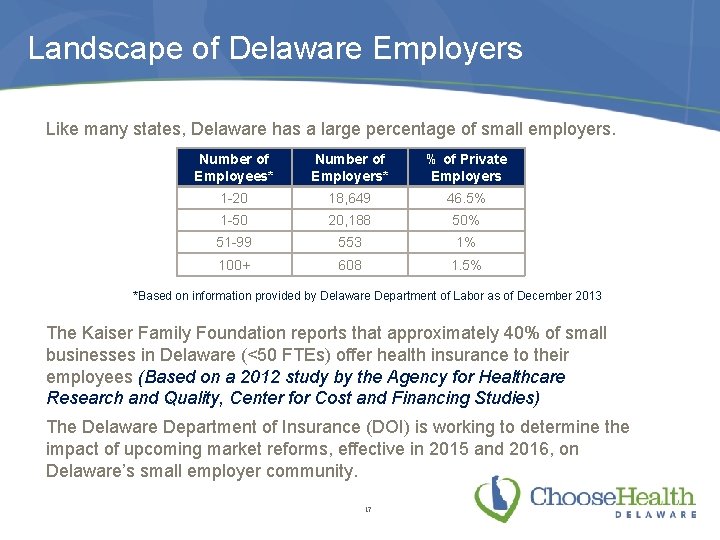
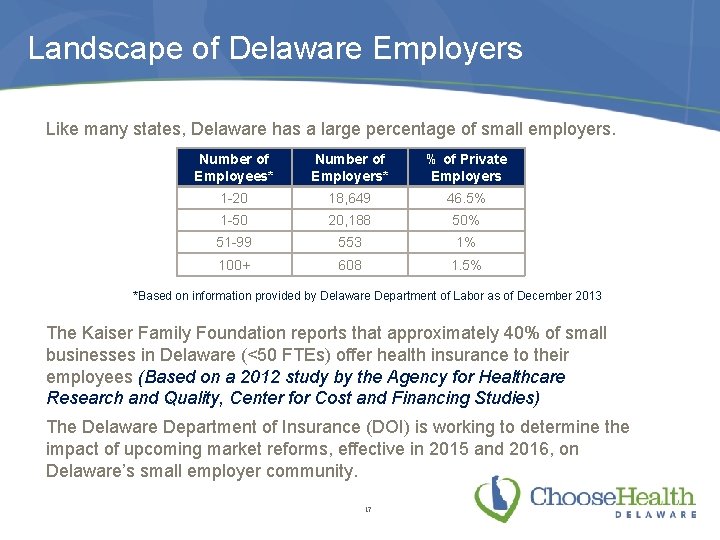
Landscape of Delaware Employers Like many states, Delaware has a large percentage of small employers. Number of Employees* Number of Employers* % of Private Employers 1 -20 18, 649 46. 5% 1 -50 20, 188 50% 51 -99 553 1% 100+ 608 1. 5% *Based on information provided by Delaware Department of Labor as of December 2013 The Kaiser Family Foundation reports that approximately 40% of small businesses in Delaware (<50 FTEs) offer health insurance to their employees (Based on a 2012 study by the Agency for Healthcare Research and Quality, Center for Cost and Financing Studies) The Delaware Department of Insurance (DOI) is working to determine the impact of upcoming market reforms, effective in 2015 and 2016, on Delaware’s small employer community. 17
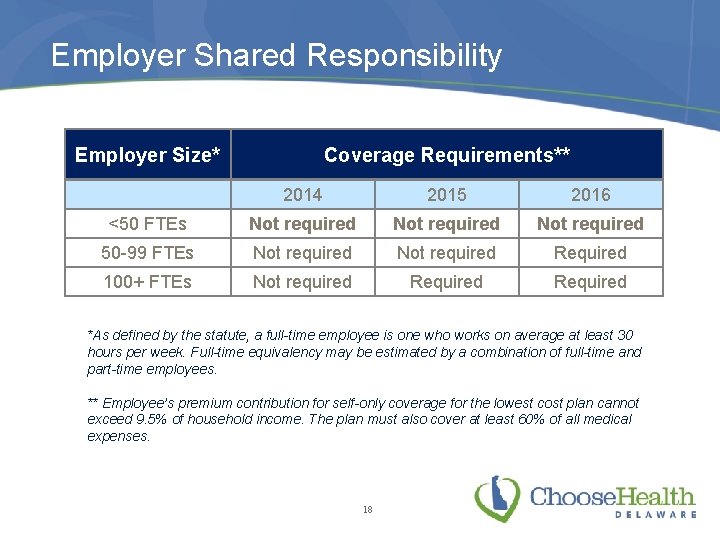
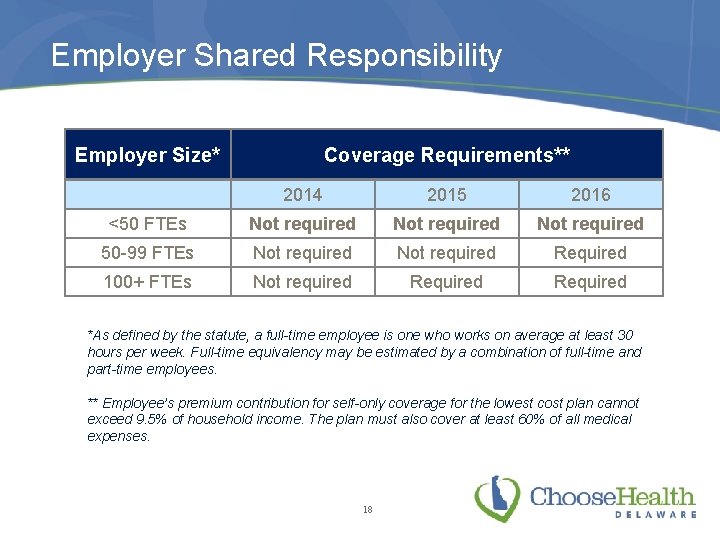
Employer Shared Responsibility Employer Size* Coverage Requirements** 2014 2015 2016 <50 FTEs Not required 50 -99 FTEs Not required Required 100+ FTEs Not required Required *As defined by the statute, a full-time employee is one who works on average at least 30 hours per week. Full-time equivalency may be estimated by a combination of full-time and part-time employees. ** Employee’s premium contribution for self-only coverage for the lowest cost plan cannot exceed 9. 5% of household income. The plan must also cover at least 60% of all medical expenses. 18
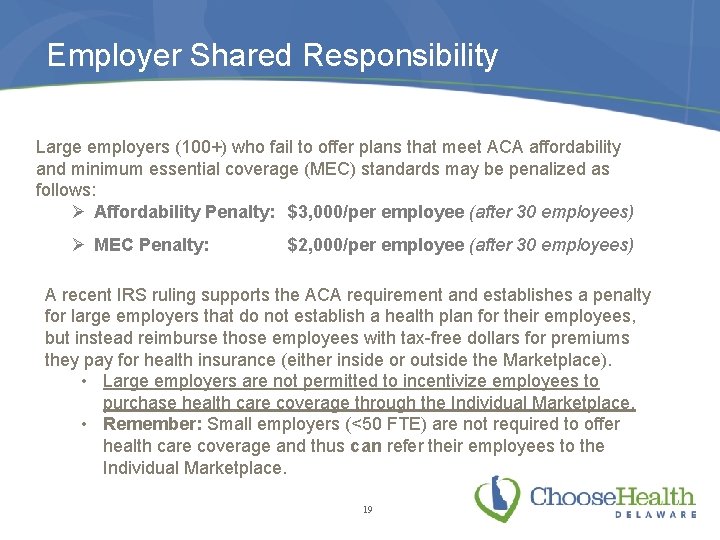
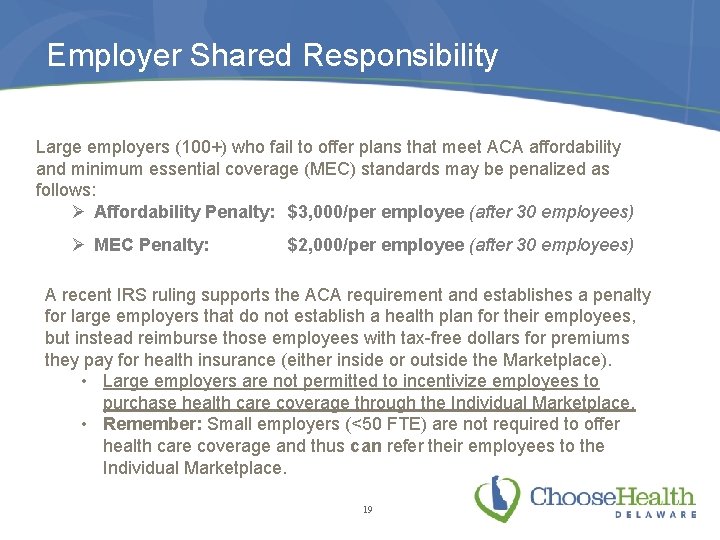
Employer Shared Responsibility Large employers (100+) who fail to offer plans that meet ACA affordability and minimum essential coverage (MEC) standards may be penalized as follows: Ø Affordability Penalty: $3, 000/per employee (after 30 employees) Ø MEC Penalty: $2, 000/per employee (after 30 employees) A recent IRS ruling supports the ACA requirement and establishes a penalty for large employers that do not establish a health plan for their employees, but instead reimburse those employees with tax-free dollars for premiums they pay for health insurance (either inside or outside the Marketplace). • Large employers are not permitted to incentivize employees to purchase health care coverage through the Individual Marketplace. • Remember: Small employers (<50 FTE) are not required to offer health care coverage and thus can refer their employees to the Individual Marketplace. 19
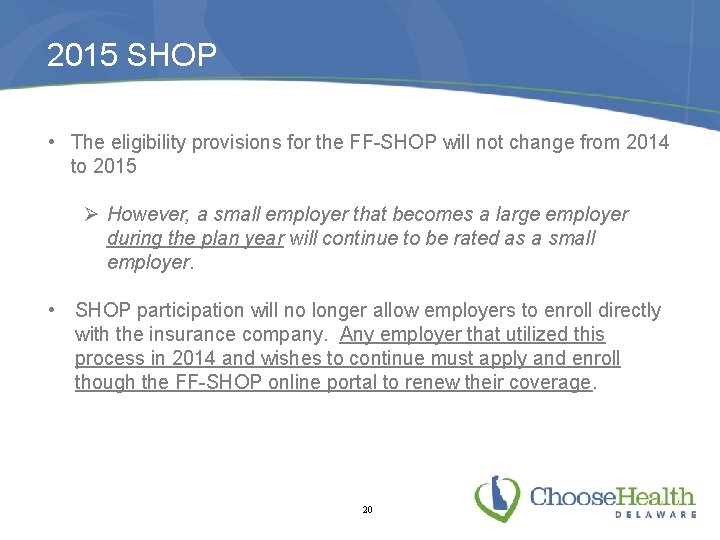
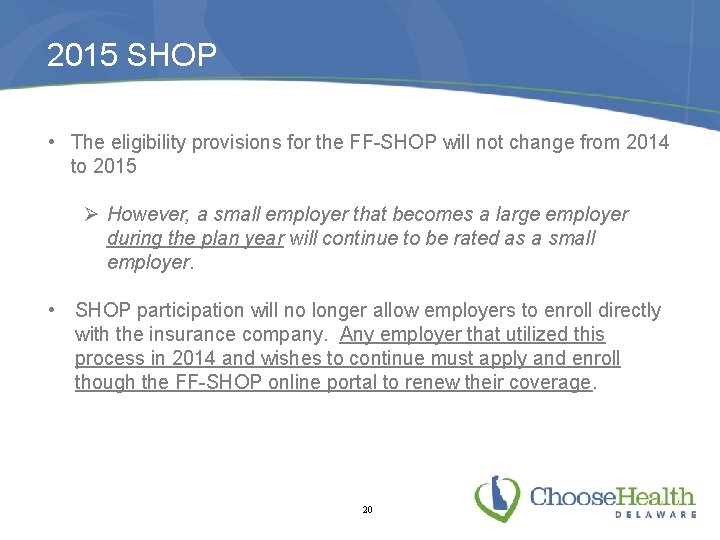
2015 SHOP • The eligibility provisions for the FF-SHOP will not change from 2014 to 2015 Ø However, a small employer that becomes a large employer during the plan year will continue to be rated as a small employer. • SHOP participation will no longer allow employers to enroll directly with the insurance company. Any employer that utilized this process in 2014 and wishes to continue must apply and enroll though the FF-SHOP online portal to renew their coverage. 20
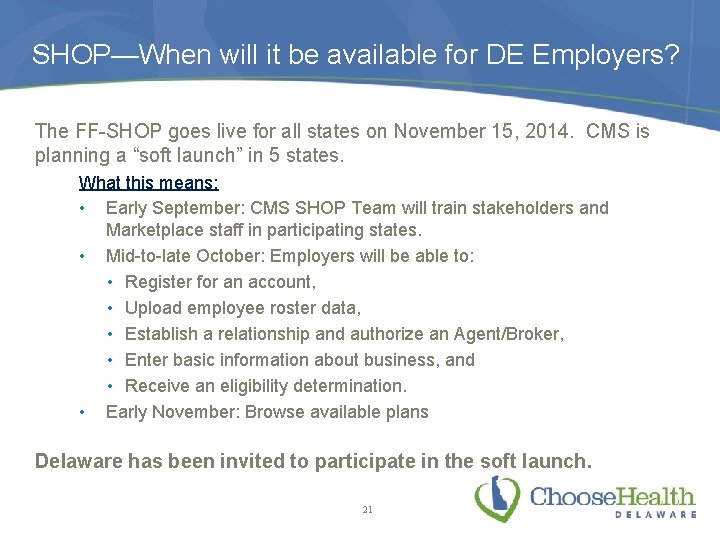
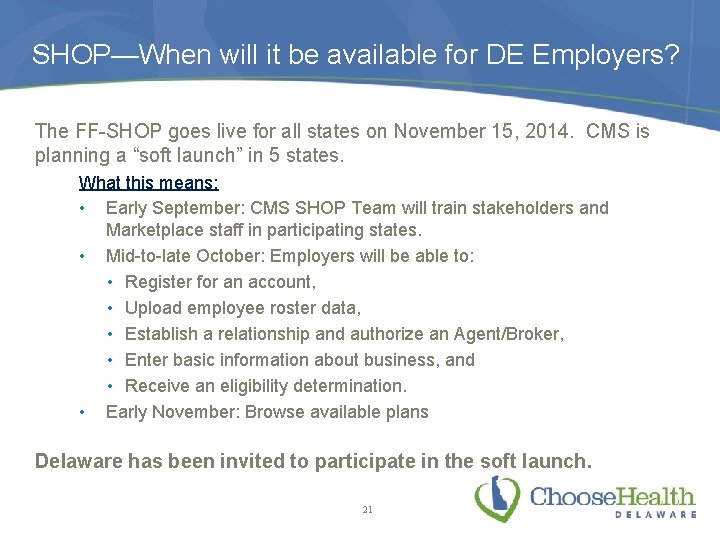
SHOP—When will it be available for DE Employers? The FF-SHOP goes live for all states on November 15, 2014. CMS is planning a “soft launch” in 5 states. What this means: • Early September: CMS SHOP Team will train stakeholders and Marketplace staff in participating states. • Mid-to-late October: Employers will be able to: • Register for an account, • Upload employee roster data, • Establish a relationship and authorize an Agent/Broker, • Enter basic information about business, and • Receive an eligibility determination. • Early November: Browse available plans Delaware has been invited to participate in the soft launch. 21
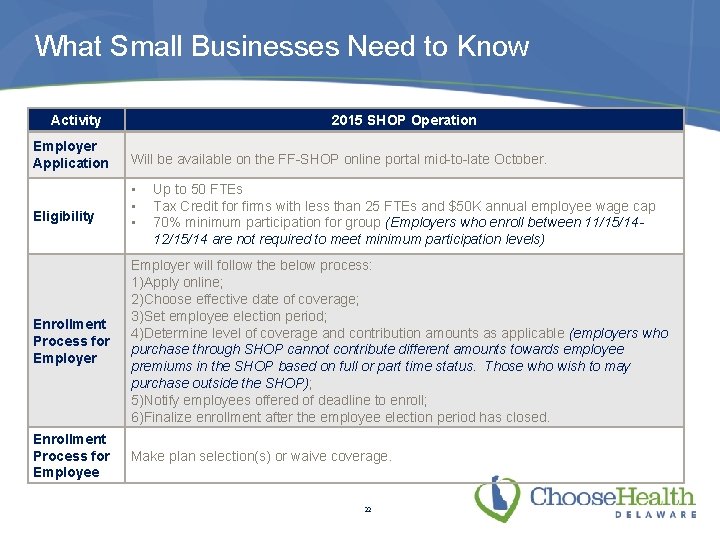
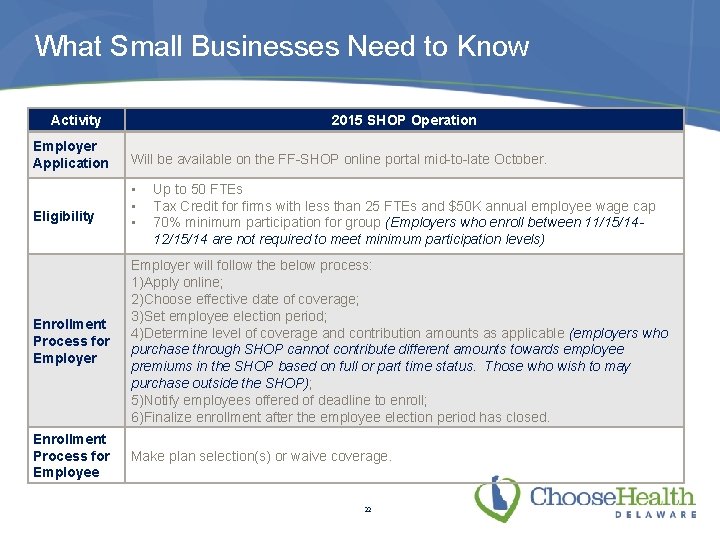
What Small Businesses Need to Know Activity 2015 SHOP Operation Employer Application Will be available on the FF-SHOP online portal mid-to-late October. Eligibility • • • Up to 50 FTEs Tax Credit for firms with less than 25 FTEs and $50 K annual employee wage cap 70% minimum participation for group (Employers who enroll between 11/15/1412/15/14 are not required to meet minimum participation levels) Enrollment Process for Employer will follow the below process: 1)Apply online; 2)Choose effective date of coverage; 3)Set employee election period; 4)Determine level of coverage and contribution amounts as applicable (employers who purchase through SHOP cannot contribute different amounts towards employee premiums in the SHOP based on full or part time status. Those who wish to may purchase outside the SHOP); 5)Notify employees offered of deadline to enroll; 6)Finalize enrollment after the employee election period has closed. Enrollment Process for Employee Make plan selection(s) or waive coverage. 22
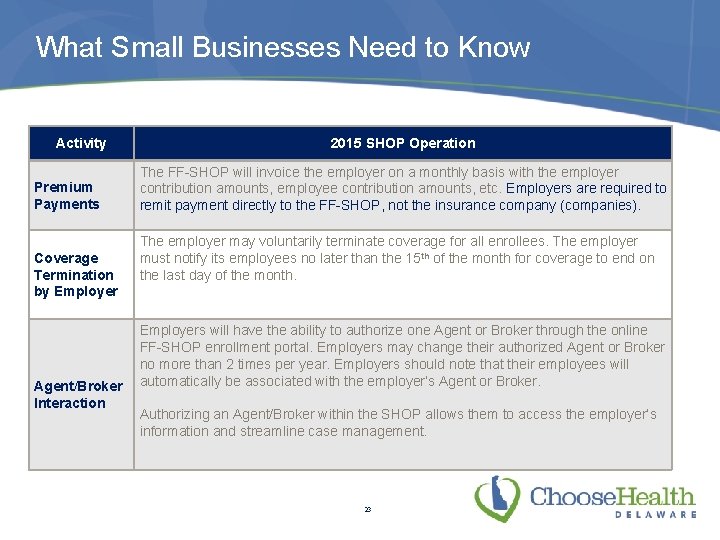
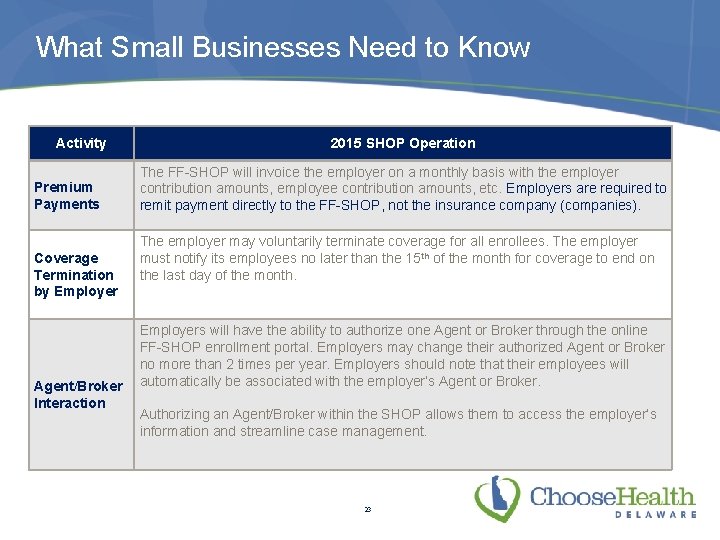
What Small Businesses Need to Know Activity Premium Payments Coverage Termination by Employer Agent/Broker Interaction 2015 SHOP Operation The FF-SHOP will invoice the employer on a monthly basis with the employer contribution amounts, employee contribution amounts, etc. Employers are required to remit payment directly to the FF-SHOP, not the insurance company (companies). The employer may voluntarily terminate coverage for all enrollees. The employer must notify its employees no later than the 15 th of the month for coverage to end on the last day of the month. Employers will have the ability to authorize one Agent or Broker through the online FF-SHOP enrollment portal. Employers may change their authorized Agent or Broker no more than 2 times per year. Employers should note that their employees will automatically be associated with the employer’s Agent or Broker. Authorizing an Agent/Broker within the SHOP allows them to access the employer’s information and streamline case management. 23
Resources for Small Businesses The FF-SHOP now has tools—available on Healthcare. gov—to help employers get ready for the next Open Enrollment period: • Full-time Equivalent (FTE) Employee Calculator: https: //www. healthcare. gov/fte-calculator/ • SHOP Tax Credit Estimator: https: //www. healthcare. gov/small-business-tax-credit-calculator/ 24
The Role of Agents and Brokers
Enrollment Pathway for Agents and Brokers • The launch of the FF-SHOP online experience will change how Agents and Brokers interact with SHOP consumers and the FF-SHOP. • Agents and Brokers who choose to work with the FFSHOP will do so through the “SHOP Enrollment Pathway, ” by directly accessing the SHOP online system. The “side-by-side” approach, where enrollments can be facilitated through the Agent or Broker’s website, will not be supported in the 2015 FF-SHOP. 26
Agent and Broker Registration and Training Requirements In addition to having an active state insurance license, Agents and Brokers are: Ø Encouraged to complete the FF-SHOP Agent/Broker Training available on the Medicare Learning Network; Ø Required to complete the SHOP Privacy and Security agreement available on the Medicare Learning Network; Ø Required to complete identity proofing on the CMS Enterprise Portal (new for 2015). Agents and Brokers who wish to participate in the FF-SHOP must complete required agreement(s) and/or training on an annual basis. 27
FF-SHOP Agent/Broker Portal Functionality Agents/Brokers may: • Search for prospective FF-SHOP clients based on: • Username • Application ID • Business Name • Monitor enrollment progress and status of employer clients. • Update employee rosters of employer clients. • Receive messages (monthly invoices and late payment warnings). 28
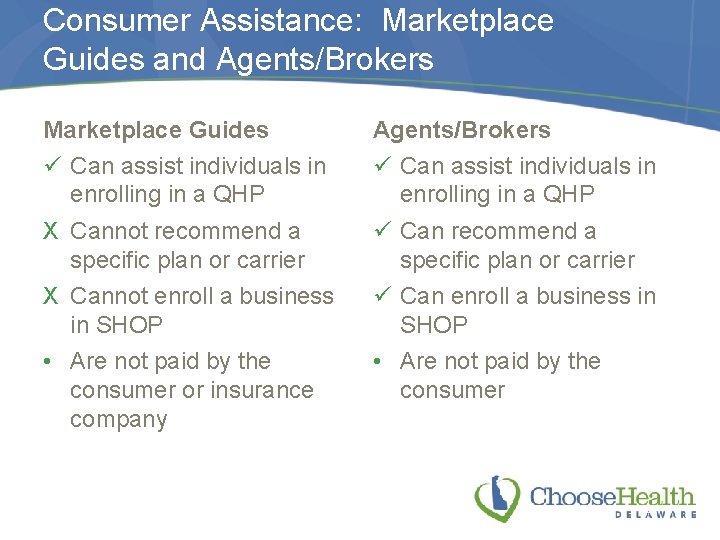
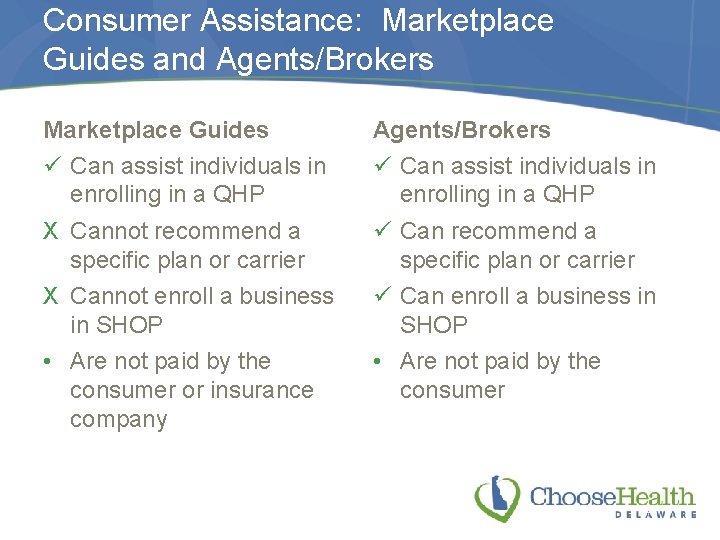
Consumer Assistance: Marketplace Guides and Agents/Brokers Marketplace Guides ü Can assist individuals in enrolling in a QHP X Cannot recommend a specific plan or carrier X Cannot enroll a business in SHOP • Are not paid by the consumer or insurance company Agents/Brokers ü Can assist individuals in enrolling in a QHP ü Can recommend a specific plan or carrier ü Can enroll a business in SHOP • Are not paid by the consumer 29
Consumer Assistance: Marketplace Guides and Agents/Brokers • Agents and Brokers continue to play a key role in assisting consumers and business owners in selecting a QHP that fits their needs. • DOI and DHSS will continue to dialogue with the Agent and Broker community to explore ways to increase their visibility to consumers and to allow Marketplace Guides to make referrals for those individuals who need additional support. 30
Plan Management Update
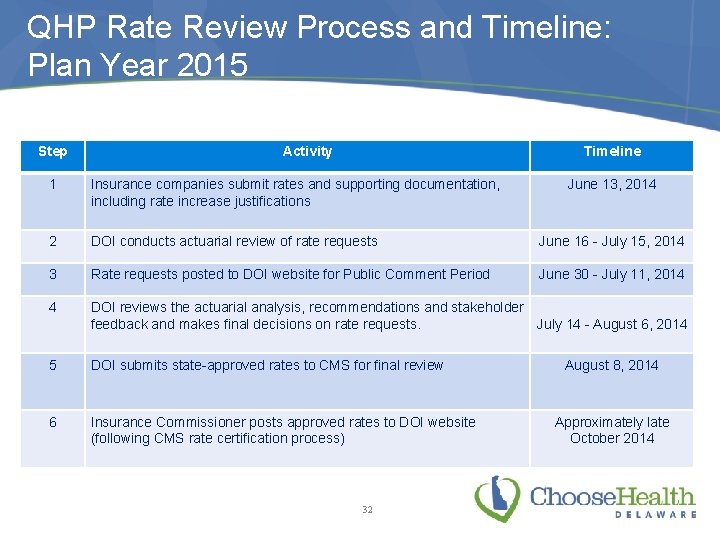
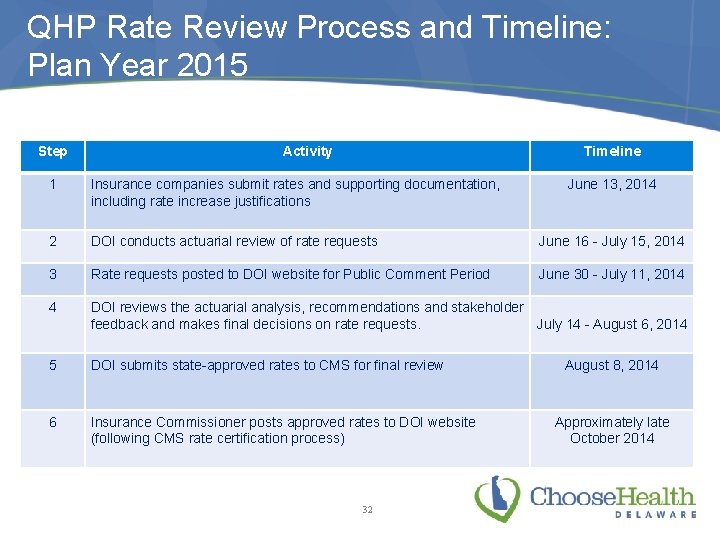
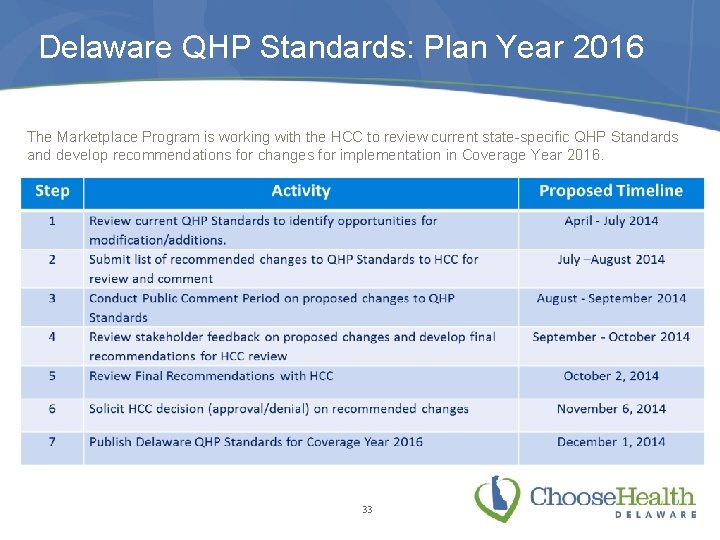
QHP Rate Review Process and Timeline: Plan Year 2015 Step Activity Timeline 1 Insurance companies submit rates and supporting documentation, including rate increase justifications 2 DOI conducts actuarial review of rate requests June 16 - July 15, 2014 3 Rate requests posted to DOI website for Public Comment Period June 30 - July 11, 2014 4 DOI reviews the actuarial analysis, recommendations and stakeholder feedback and makes final decisions on rate requests. July 14 - August 6, 2014 5 DOI submits state-approved rates to CMS for final review 6 Insurance Commissioner posts approved rates to DOI website (following CMS rate certification process) 32 June 13, 2014 August 8, 2014 Approximately late October 2014
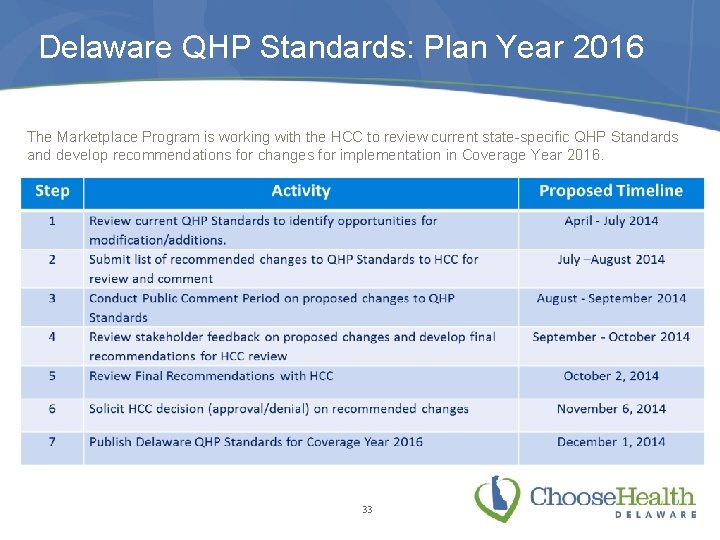
Delaware QHP Standards: Plan Year 2016 The Marketplace Program is working with the HCC to review current state-specific QHP Standards and develop recommendations for changes for implementation in Coverage Year 2016. 33

Thank you!
 Small business health insurance delaware
Small business health insurance delaware Small business health insurance delaware
Small business health insurance delaware Backup and recovery techniques
Backup and recovery techniques Choose health delaware
Choose health delaware Delaware health care commission
Delaware health care commission Delaware health resources board
Delaware health resources board Choose health delaware
Choose health delaware Choose health delaware
Choose health delaware Features of fire insurance
Features of fire insurance Ngpf activity bank insurance
Ngpf activity bank insurance Texas tech health insurance
Texas tech health insurance Fau employee benefits
Fau employee benefits Umms benefits
Umms benefits Tonik health insurance
Tonik health insurance Ouhsc student health
Ouhsc student health Raksha tpa office
Raksha tpa office Ucf employee benefits
Ucf employee benefits Health insurance market segmentation
Health insurance market segmentation Deloitte health insurance
Deloitte health insurance What is deductible in health insurance
What is deductible in health insurance Health insurance premium payment program ny
Health insurance premium payment program ny Commonwealth health insurance connector authority
Commonwealth health insurance connector authority Chapter 14 health disability and life insurance
Chapter 14 health disability and life insurance Aditya birla nuvo health insurance
Aditya birla nuvo health insurance Uw madison health insurance
Uw madison health insurance Statewide health insurance benefits advisors
Statewide health insurance benefits advisors Paramount health insurance
Paramount health insurance Ceww health insurance consortium
Ceww health insurance consortium Religare health insurance franchise
Religare health insurance franchise Missouri state health insurance assistance program
Missouri state health insurance assistance program Ira b wilson
Ira b wilson Healthscopebenefits.com
Healthscopebenefits.com Pace university health insurance
Pace university health insurance Cm insurance belgium
Cm insurance belgium Chickasaw nation health insurance
Chickasaw nation health insurance