Current CMS Quality Reporting Programs Physician Quality Reporting
- Slides: 15
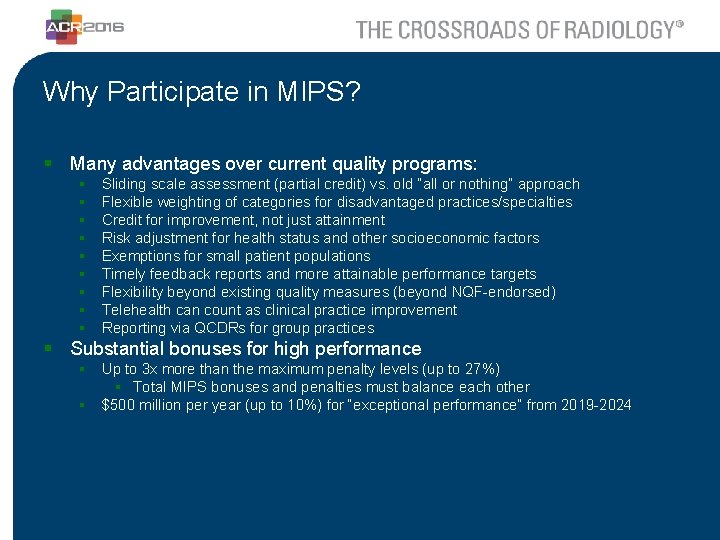
Current CMS Quality Reporting Programs • Physician Quality Reporting System (PQRS) • Electronic Health Records (EHR) Incentive Program (Meaningful Use) • Value-Based Payment Modifier
Physician Quality Reporting System (PQRS) § What is PQRS? § PQRS is a pay-for-reporting system that penalizes providers for not reporting quality measures data on Medicare patients. § Goals § Collect data on quality process and outcome measures on Medicare beneficiaries. § Penalties § Failure to participate -2. 0% penalty § Measures Reported § Individual Measures § Measures Group
EHR Incentive Program – Meaningful Use § What is Meaningful Use? § Program that uses a incentive payments and penalties to promote meaningful use of certified EHR technologies. § The EHR Incentive Program is split into three stages, with each stage having its own set of measures for demonstrating meaningful use. § Goals § Transition from paper records to electronic health records (EHRs) § Using EHRs to achieve benchmarks for quality care, leading to improved patient care. § Penalties § Failure to participate in 2016 PQRS program -4. 0% penalty in 2018 § Measures Reported? § Core and Menu Objectives § Clinical Quality Measures (CQMs)
Meaningful Use Modified Stage 2 § Objectives: § § § § § Protect Patient Health Information Clinical Decision Support Computerized Provider Order Entry Electronic Prescriptions Health Information Exchange Patient-Specific Education Resources Medication Reconciliation Patient Electronic Access Secure Electronic Messaging Public Health Reporting § CQMs § Similar to quality measures reported under PQRS.
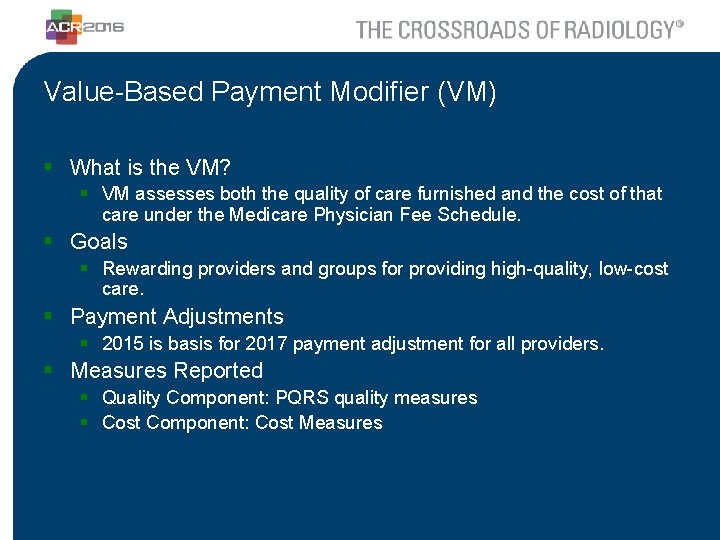
Value-Based Payment Modifier (VM) § What is the VM? § VM assesses both the quality of care furnished and the cost of that care under the Medicare Physician Fee Schedule. § Goals § Rewarding providers and groups for providing high-quality, low-cost care. § Payment Adjustments § 2015 is basis for 2017 payment adjustment for all providers. § Measures Reported § Quality Component: PQRS quality measures § Cost Component: Cost Measures
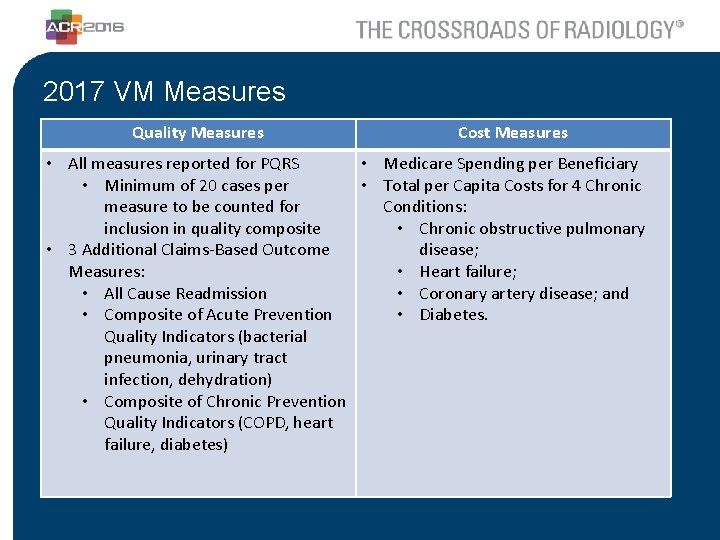
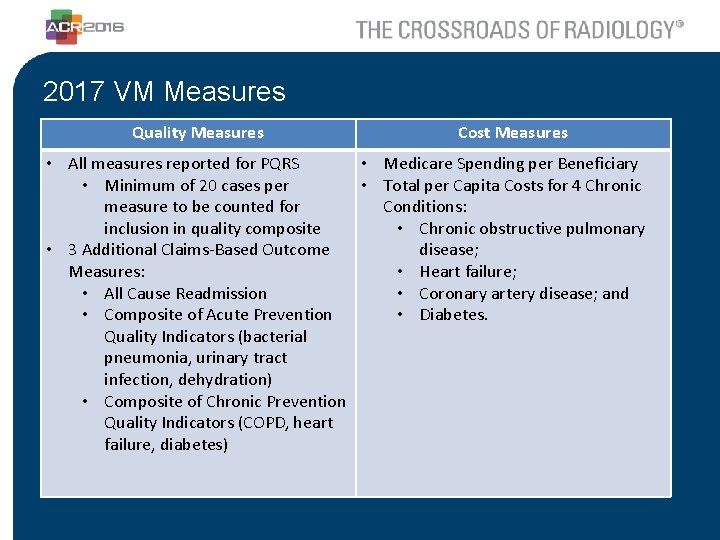
2017 VM Measures Quality Measures Cost Measures • All measures reported for PQRS • Medicare Spending per Beneficiary • Minimum of 20 cases per • Total per Capita Costs for 4 Chronic measure to be counted for Conditions: inclusion in quality composite • Chronic obstructive pulmonary • 3 Additional Claims-Based Outcome disease; Measures: • Heart failure; • All Cause Readmission • Coronary artery disease; and • Composite of Acute Prevention • Diabetes. Quality Indicators (bacterial pneumonia, urinary tract infection, dehydration) • Composite of Chronic Prevention Quality Indicators (COPD, heart failure, diabetes)
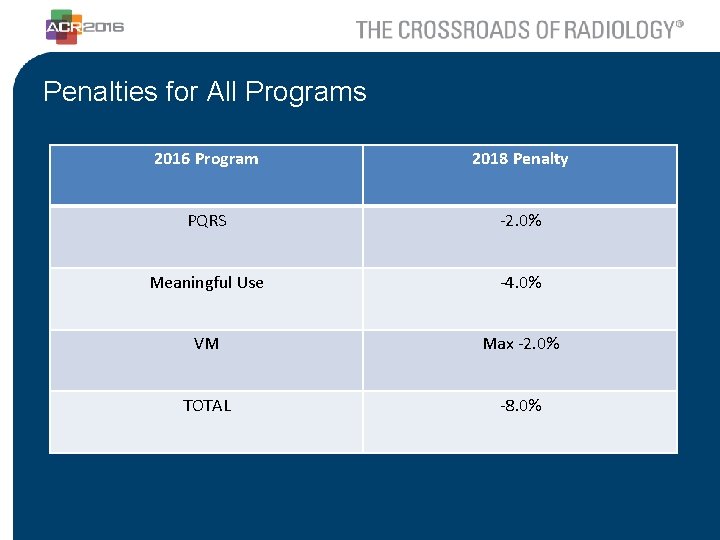
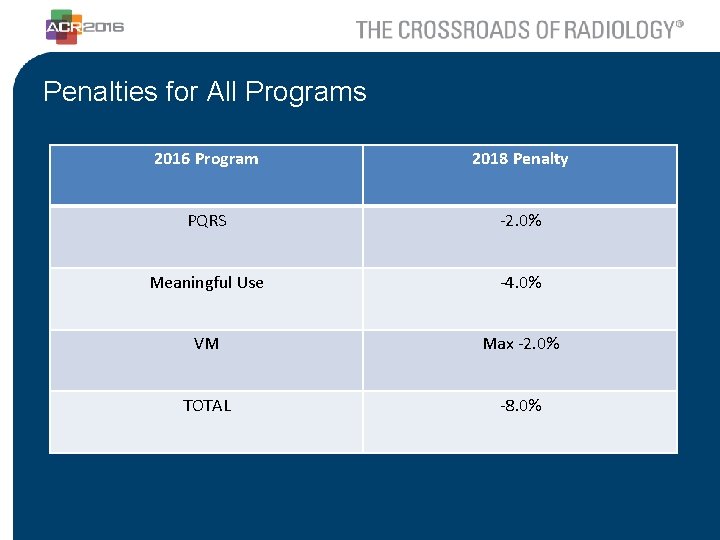
Penalties for All Programs 2016 Program 2018 Penalty PQRS -2. 0% Meaningful Use -4. 0% VM Max -2. 0% TOTAL -8. 0%
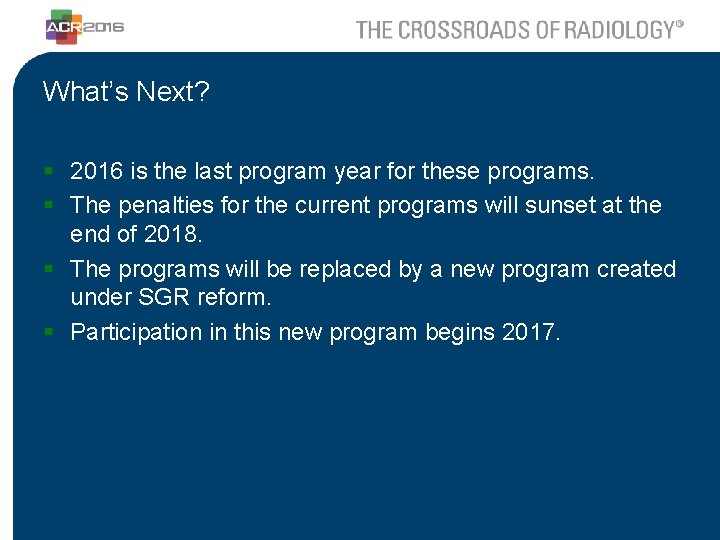
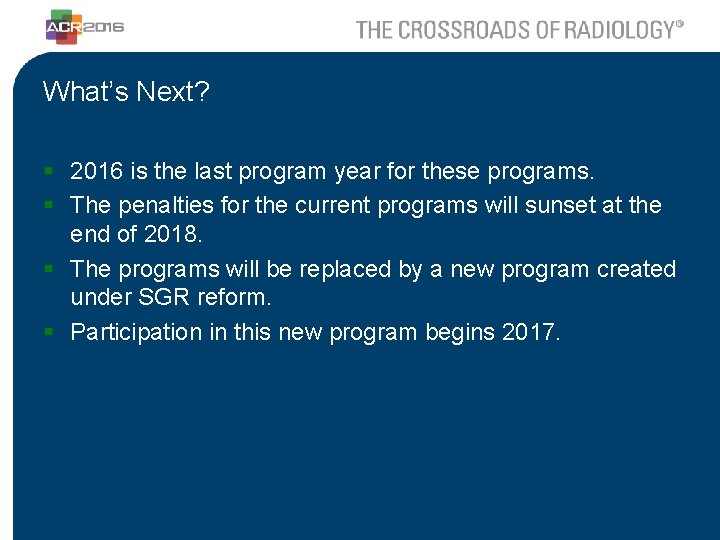
What’s Next? § 2016 is the last program year for these programs. § The penalties for the current programs will sunset at the end of 2018. § The programs will be replaced by a new program created under SGR reform. § Participation in this new program begins 2017.
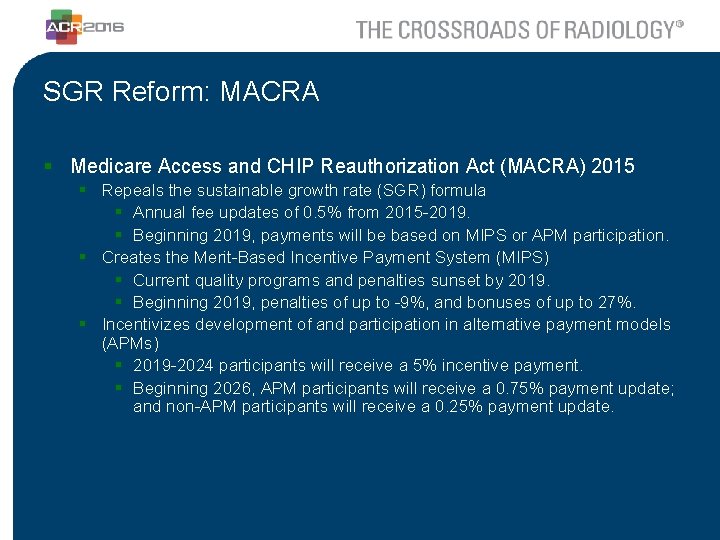
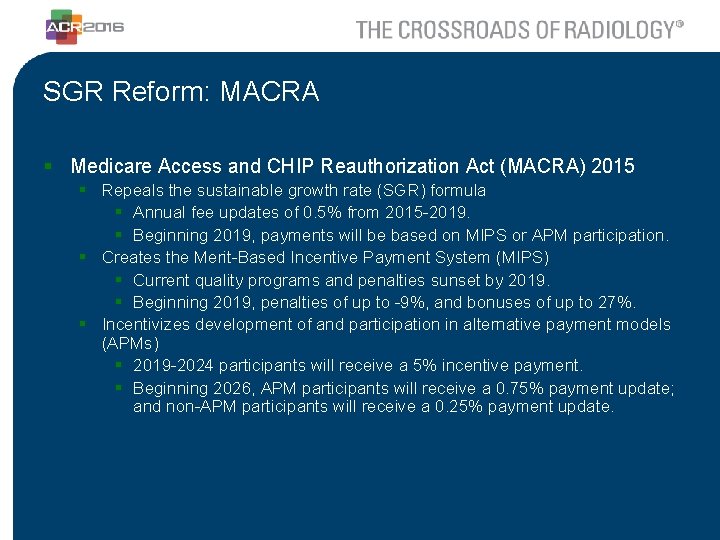
SGR Reform: MACRA § Medicare Access and CHIP Reauthorization Act (MACRA) 2015 § Repeals the sustainable growth rate (SGR) formula § Annual fee updates of 0. 5% from 2015 -2019. § Beginning 2019, payments will be based on MIPS or APM participation. § Creates the Merit-Based Incentive Payment System (MIPS) § Current quality programs and penalties sunset by 2019. § Beginning 2019, penalties of up to -9%, and bonuses of up to 27%. § Incentivizes development of and participation in alternative payment models (APMs) § 2019 -2024 participants will receive a 5% incentive payment. § Beginning 2026, APM participants will receive a 0. 75% payment update; and non-APM participants will receive a 0. 25% payment update.
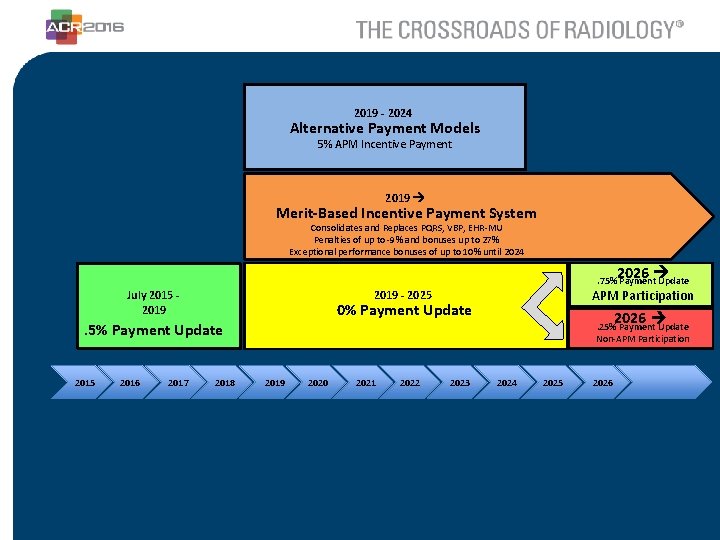
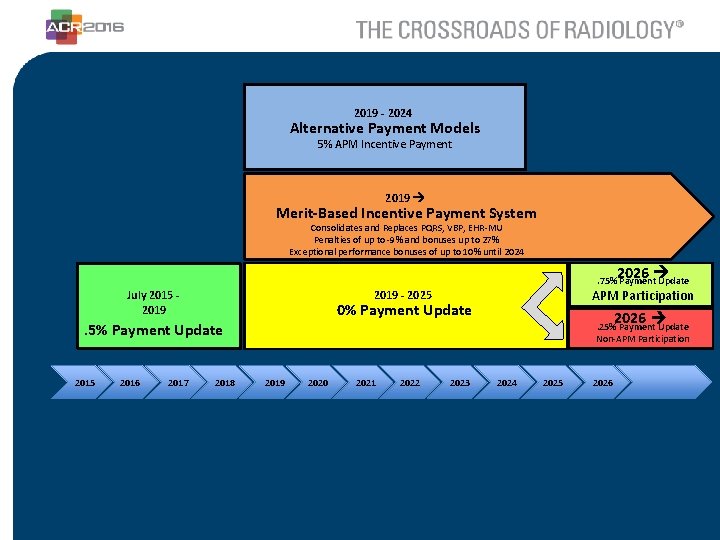
2019 - 2024 Alternative Payment Models 5% APM Incentive Payment 2019 Merit-Based Incentive Payment System Consolidates and Replaces PQRS, VBP, EHR-MU Penalties of up to -9% and bonuses up to 27% Exceptional performance bonuses of up to 10% until 2024 2026 . 75% Payment Update 0% Payment Update . 5% Payment Update 2015 2016 2017 APM Participation 2019 - 2025 July 2015 2019 2018 2026 . 25% Payment Update Non-APM Participation 2019 2020 2021 2022 2023 2024 2025 2026
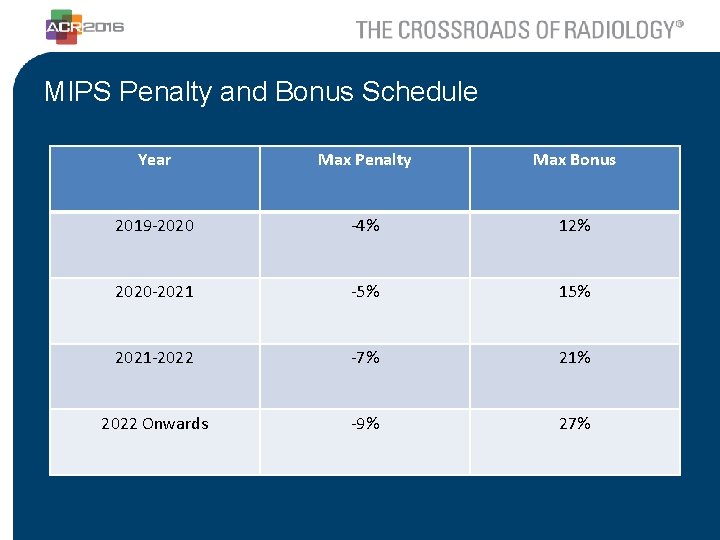
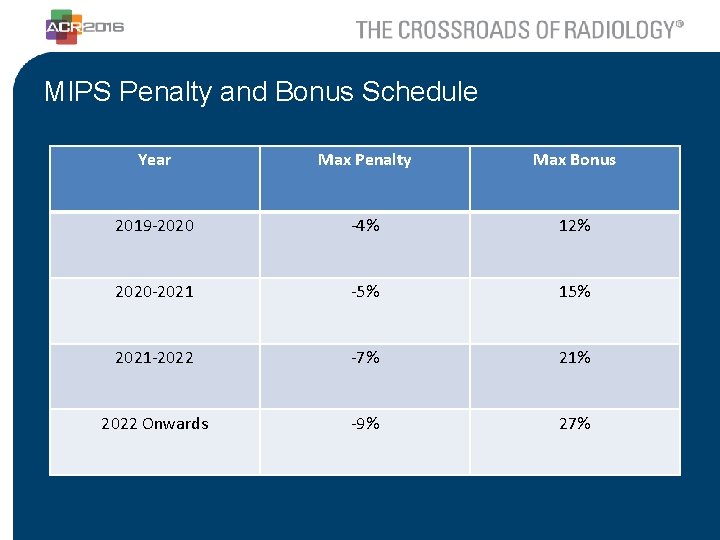
MIPS Penalty and Bonus Schedule Year Max Penalty Max Bonus 2019 -2020 -4% 12% 2020 -2021 -5% 15% 2021 -2022 -7% 21% 2022 Onwards -9% 27%
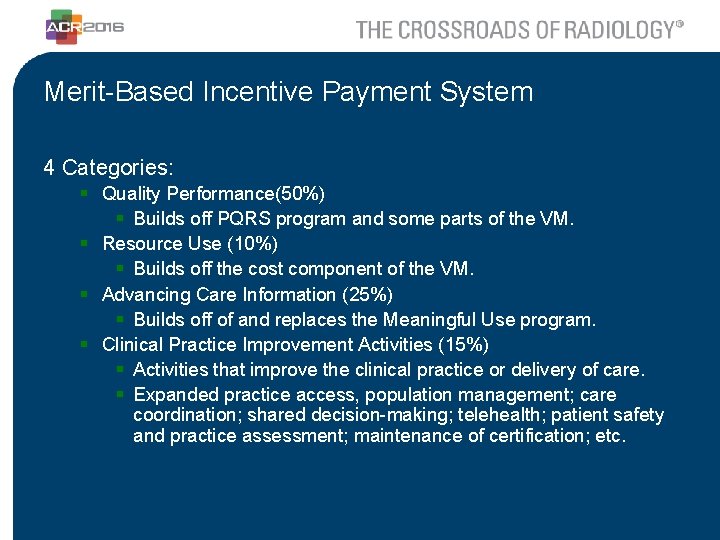
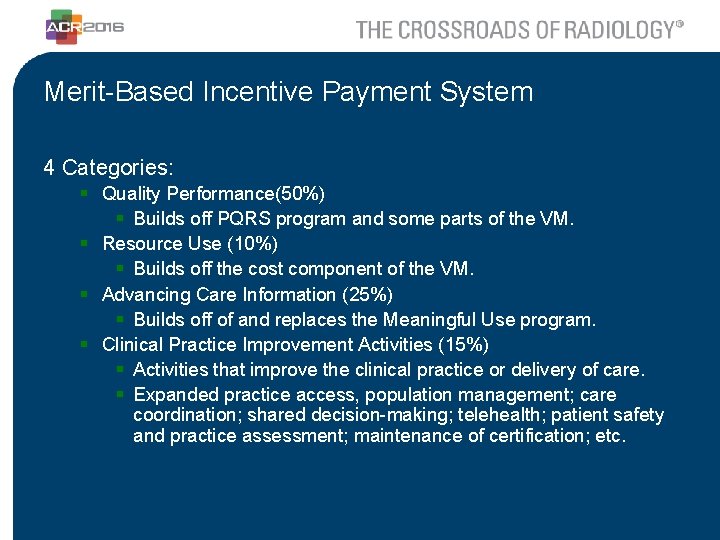
Merit-Based Incentive Payment System 4 Categories: § Quality Performance(50%) § Builds off PQRS program and some parts of the VM. § Resource Use (10%) § Builds off the cost component of the VM. § Advancing Care Information (25%) § Builds off of and replaces the Meaningful Use program. § Clinical Practice Improvement Activities (15%) § Activities that improve the clinical practice or delivery of care. § Expanded practice access, population management; care coordination; shared decision-making; telehealth; patient safety and practice assessment; maintenance of certification; etc.
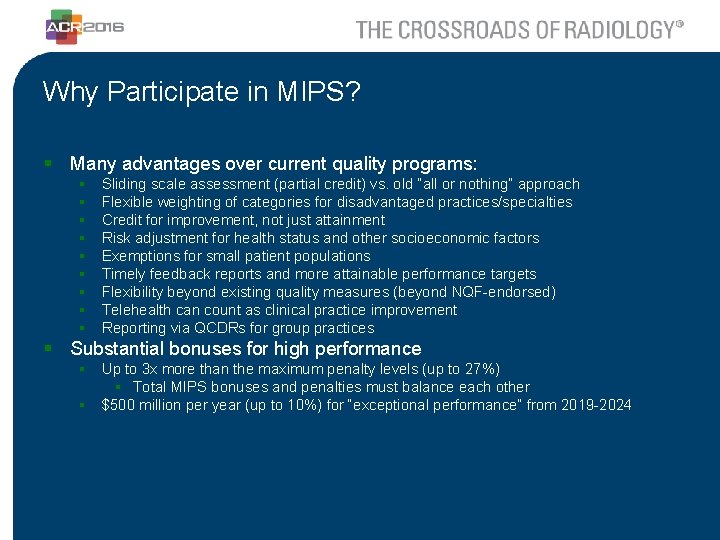
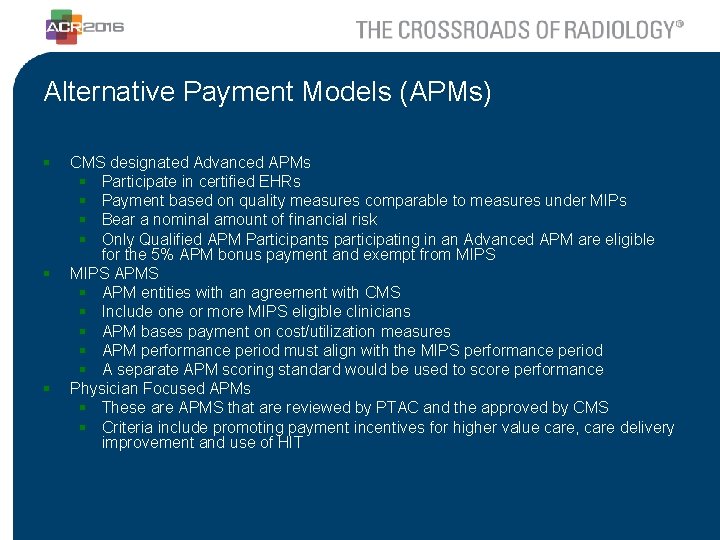
Why Participate in MIPS? § Many advantages over current quality programs: § § § § § Sliding scale assessment (partial credit) vs. old “all or nothing” approach Flexible weighting of categories for disadvantaged practices/specialties Credit for improvement, not just attainment Risk adjustment for health status and other socioeconomic factors Exemptions for small patient populations Timely feedback reports and more attainable performance targets Flexibility beyond existing quality measures (beyond NQF-endorsed) Telehealth can count as clinical practice improvement Reporting via QCDRs for group practices § Substantial bonuses for high performance § Up to 3 x more than the maximum penalty levels (up to 27%) § Total MIPS bonuses and penalties must balance each other § $500 million per year (up to 10%) for “exceptional performance” from 2019 -2024
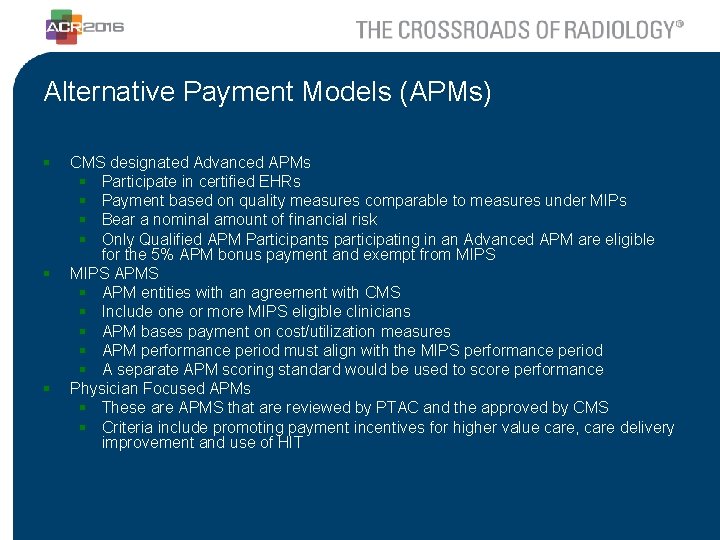
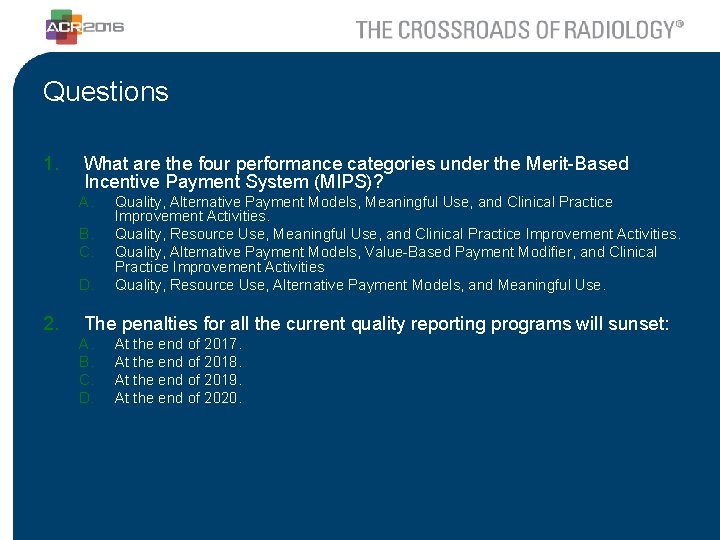
Alternative Payment Models (APMs) § § § CMS designated Advanced APMs § Participate in certified EHRs § Payment based on quality measures comparable to measures under MIPs § Bear a nominal amount of financial risk § Only Qualified APM Participants participating in an Advanced APM are eligible for the 5% APM bonus payment and exempt from MIPS APMS § APM entities with an agreement with CMS § Include one or more MIPS eligible clinicians § APM bases payment on cost/utilization measures § APM performance period must align with the MIPS performance period § A separate APM scoring standard would be used to score performance Physician Focused APMs § These are APMS that are reviewed by PTAC and the approved by CMS § Criteria include promoting payment incentives for higher value care, care delivery improvement and use of HIT
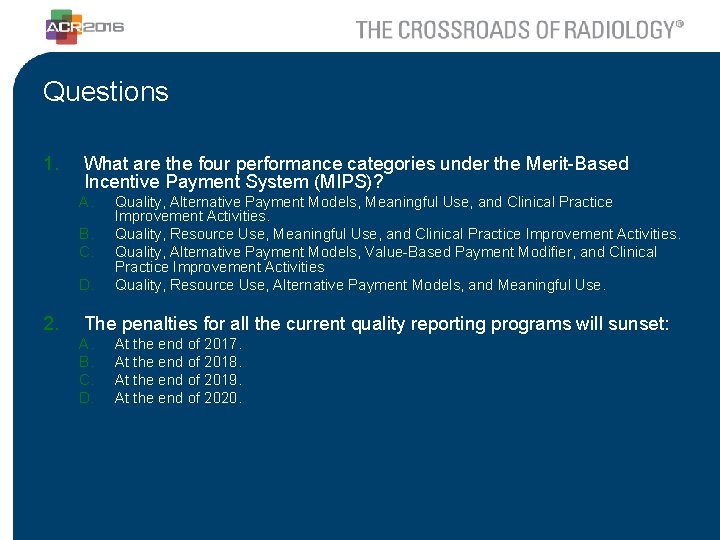
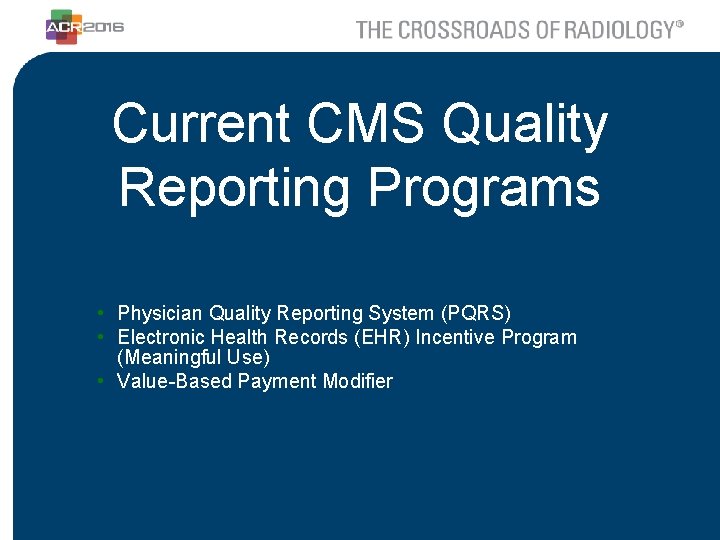
Questions 1. What are the four performance categories under the Merit-Based Incentive Payment System (MIPS)? A. B. C. D. 2. Quality, Alternative Payment Models, Meaningful Use, and Clinical Practice Improvement Activities. Quality, Resource Use, Meaningful Use, and Clinical Practice Improvement Activities. Quality, Alternative Payment Models, Value-Based Payment Modifier, and Clinical Practice Improvement Activities Quality, Resource Use, Alternative Payment Models, and Meaningful Use. The penalties for all the current quality reporting programs will sunset: A. B. C. D. At the end of 2017. At the end of 2018. At the end of 2019. At the end of 2020.