Coverage decisionmaking under universal health coverage Dr Jeanette










- Slides: 26
Coverage decision-making under universal health coverage Dr. Jeanette Vega Washington DC, March 11 2013
Presentation Overview 1 Universal Health Coverage (UHC): Definition and concepts 2 Implementing UHC: 3 Country case study 4 Final reflections
Universal Health Coverage Definition: All people can access the health services they need without incurring financial hardship. Indicators: 1. Access 2. Financial protection

UHC is Not Only Health Financing Inputs & Processes Health Financing Health Workforce Infrastructure Information Governance Outputs Outcomes Impact Service Access and Readiness Coverage of Interventions Health Status Service Quality and Safety Service Coverage with a Method of Financial Risk Protection Utilization Risk Factors Household Financial Wellbeing Responsiveness Prepaid Funds Service Delivery Level and Distribution (equity) Social Determinants
Presentation Overview 1 2 3 4 Implementing UHC
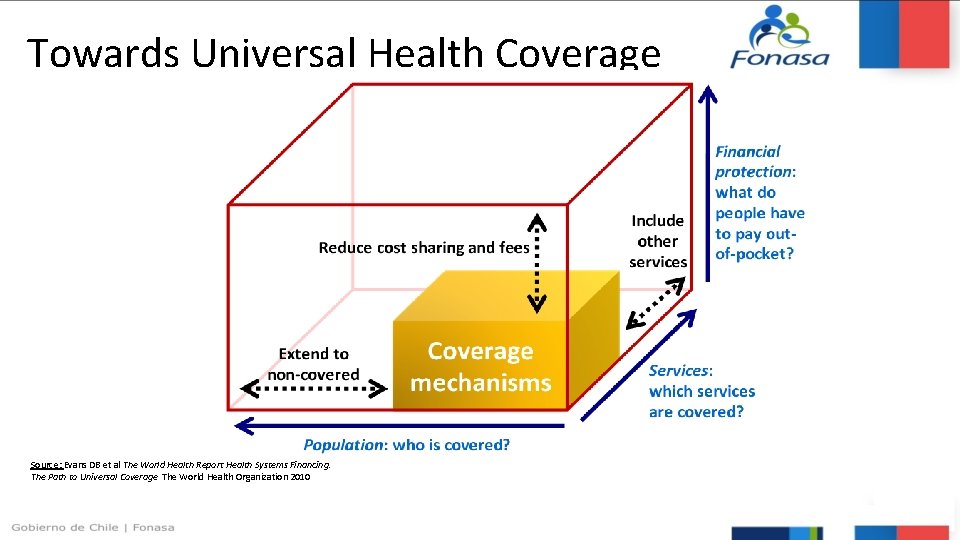
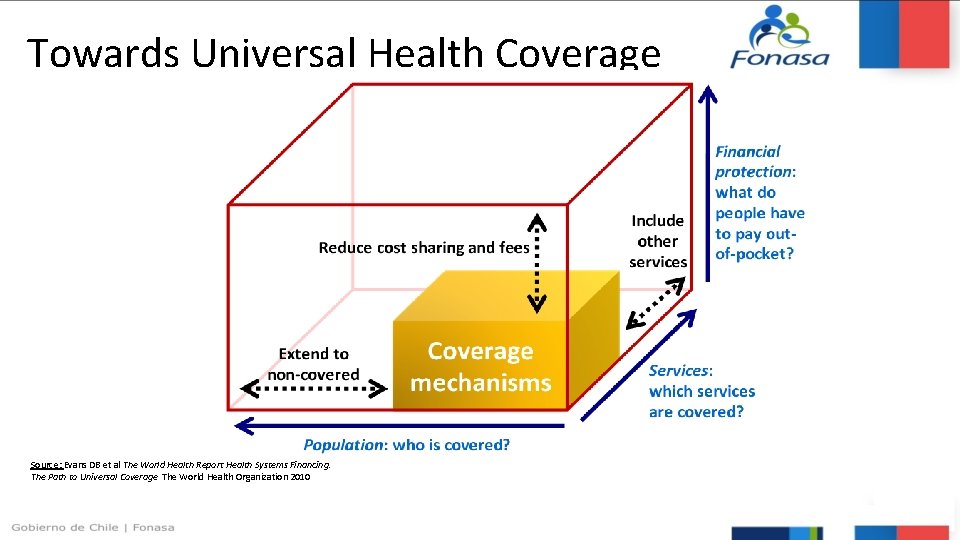
Towards Universal Health Coverage Source: Evans DB et al The World Health Report Health Systems Financing. The Path to Universal Coverage The World Health Organization 2010
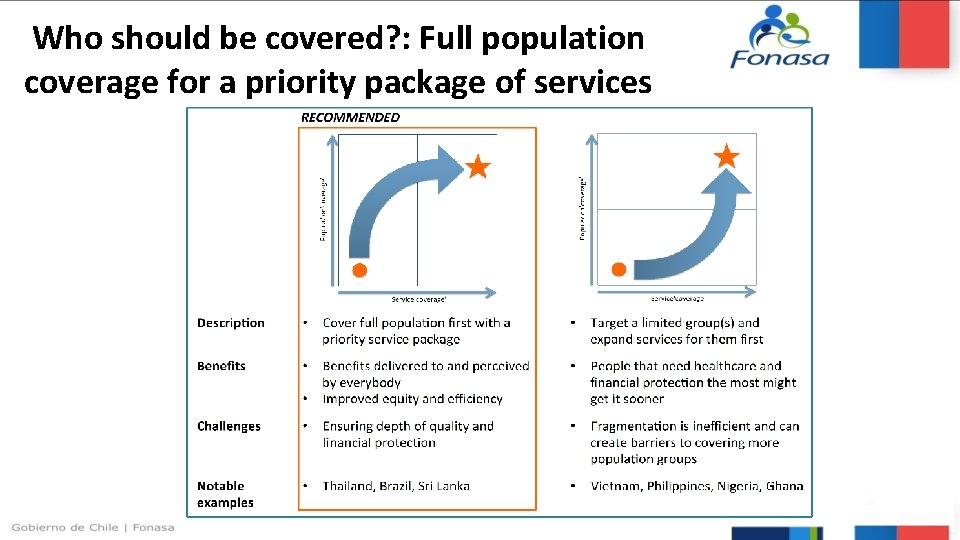
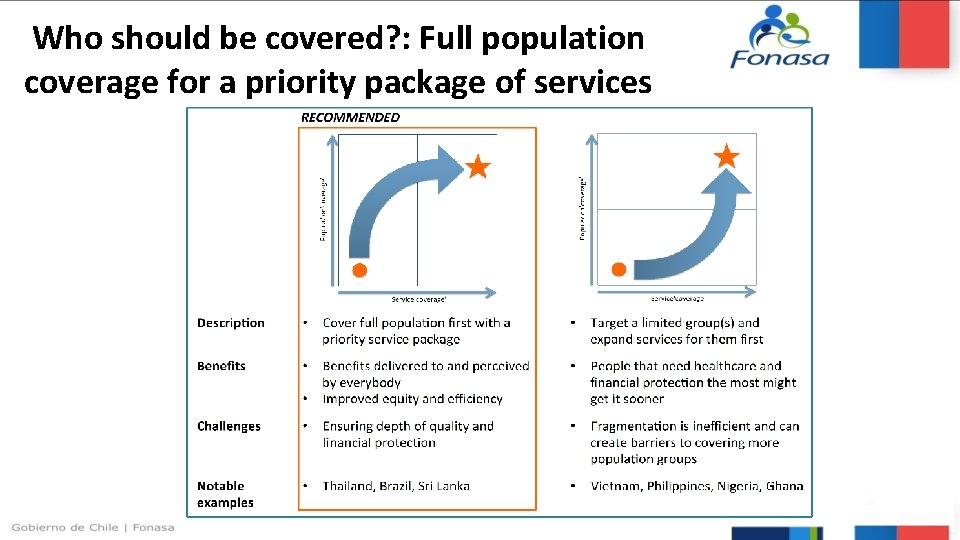
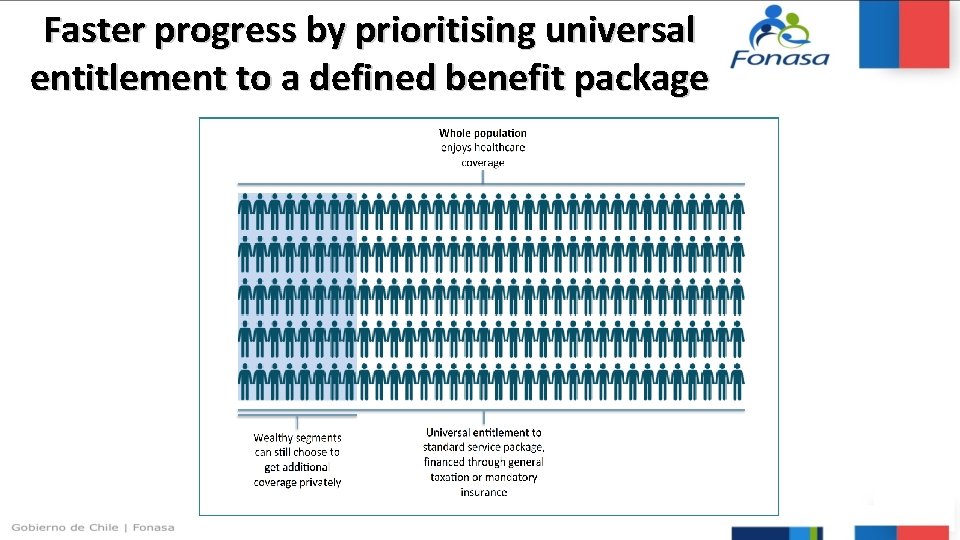
Who should be covered? : Full population coverage for a priority package of services
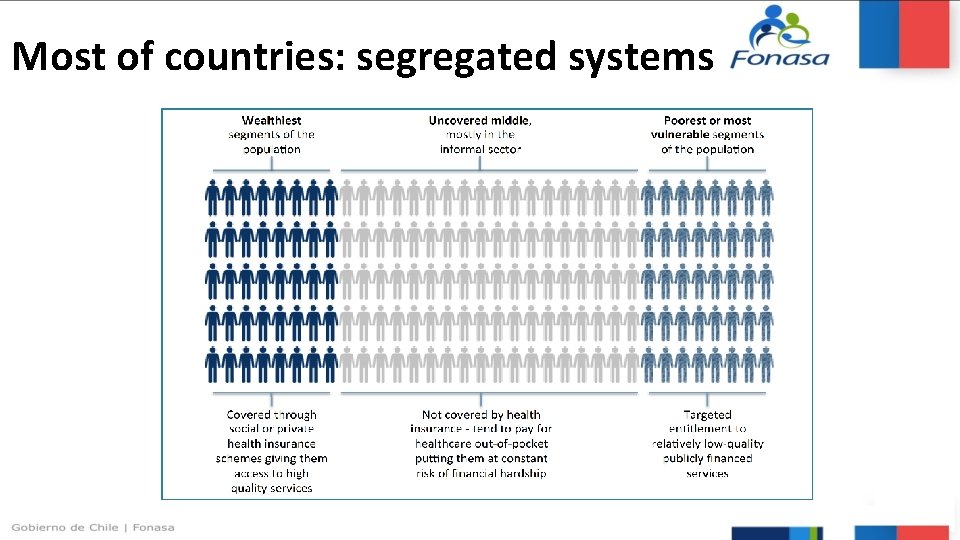
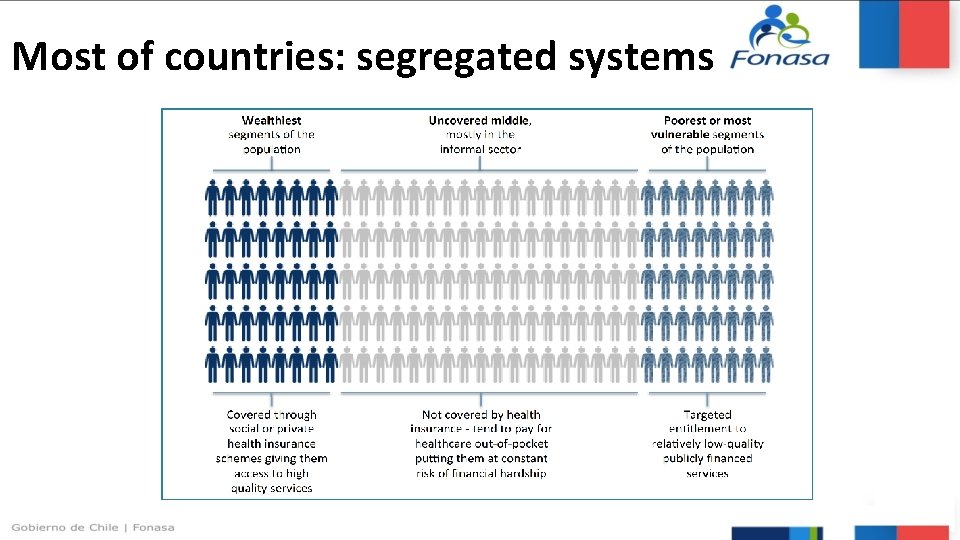
Most of countries: segregated systems

How to pay for UHC?

Defining priority setting in health “the task of determining the priority to be assigned to a service, a service development or an individual patient at a given point in time”. (NHS, 2009)

Why priority setting? • Because claims (whether needs or demands) on healthcare resources are always greater than the resources available. • Because the absence of or ad-hoc priority-setting approaches can disproportionately impact the least well-off and distort a national health system’s ability to progress towards UHC. • Because healthcare costs growth is always greater than income growth • To increase efficiency and equity of health funding. 11

The opportunity for policy-makers • Many applications for priority-setting – Achieving national objectives – Allocating resources – Defining the benefit package – Introducing and assessing new technologies including drugs

Critical priority setting choices and levels critical choices for priority setting and resource Proportion of available funds spent on capital development relative to operating costs Allocation of resources to different levels of the health service and to specific disease control programs Definition of who should be eligible to receive such treatment Definition of the amount to be spent on individual patients Government, national agencies Meso Health system providers Micro Individual providers Public, consumer and provider input allocation: Forms of treatment that should be available through public funding Proportion of public revenues allocated to health Distribution of the health budget between geographical areas/population aggregations Macro
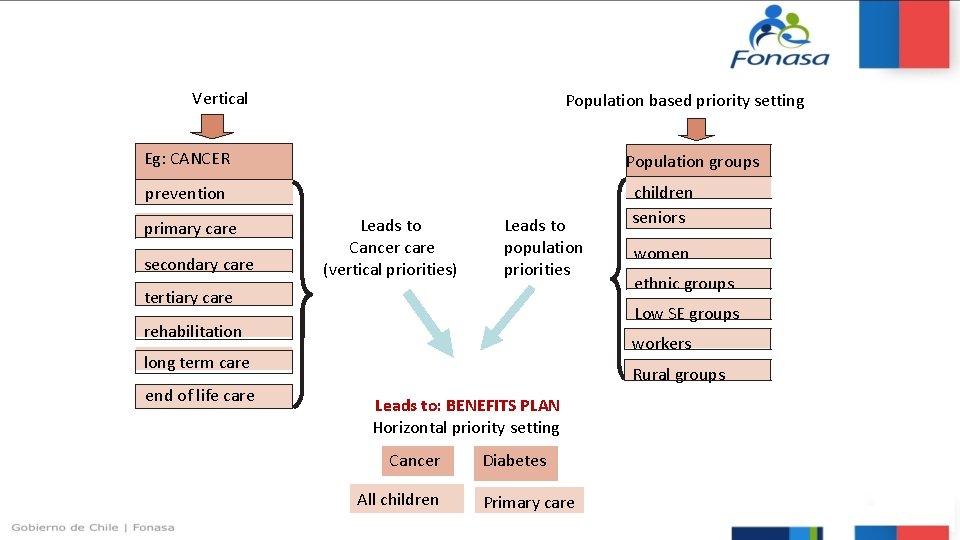
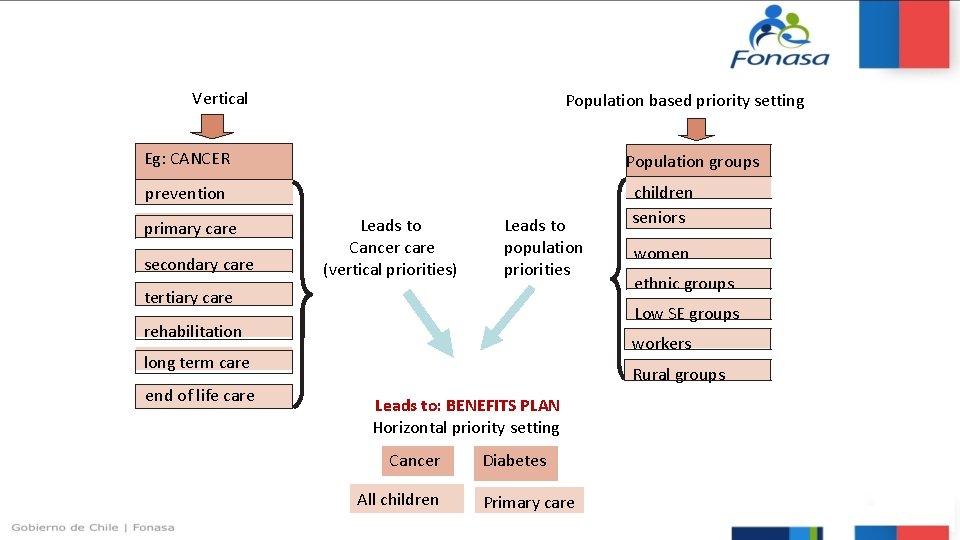
Vertical Population based priority setting Eg: CANCER Population groups prevention primary care secondary care Leads to Cancer care (vertical priorities) Leads to population priorities tertiary care women ethnic groups Low SE groups rehabilitation workers long term care end of life care children seniors Rural groups Leads to: BENEFITS PLAN Horizontal priority setting Cancer All children Diabetes Primary care
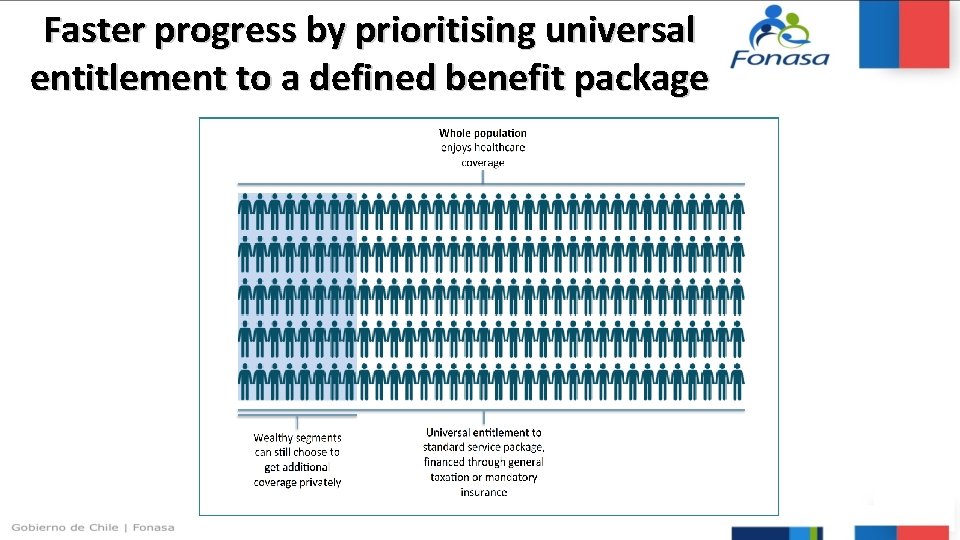
Faster progress by prioritising universal entitlement to a defined benefit package
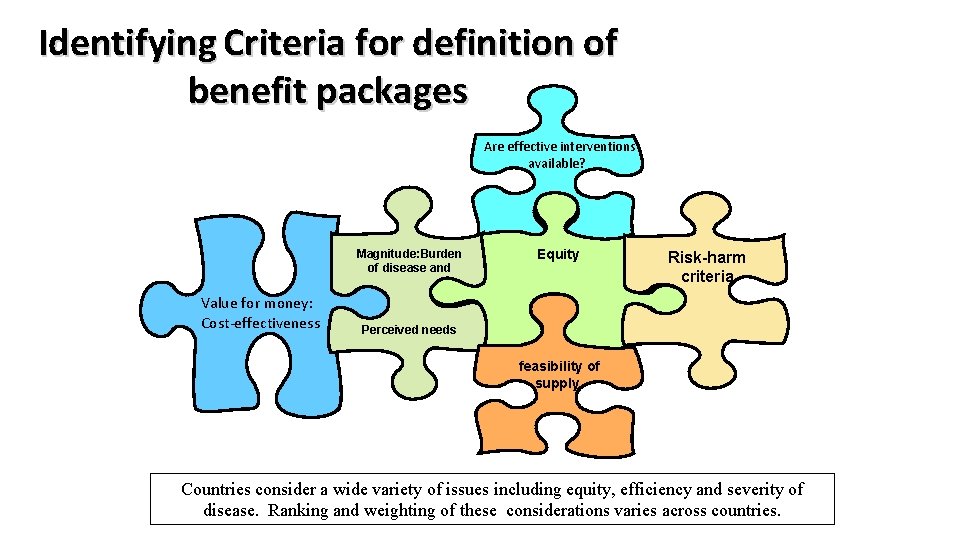
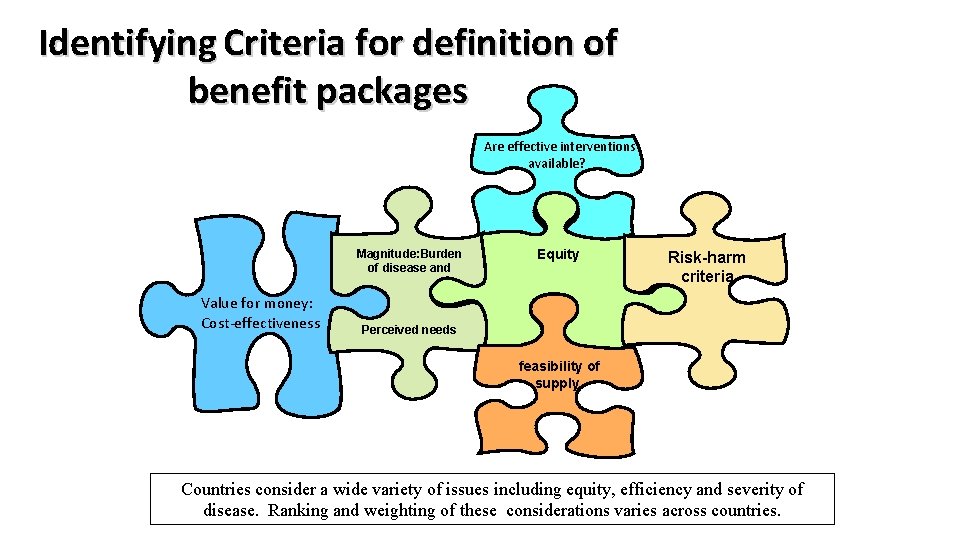
Identifying Criteria for definition of benefit packages Magnitude: Burden of disease and Value for money: Cost-effectiveness Are effective interventions available? Equity Risk-harm criteria Perceived needs feasibility of supply Countries consider a wide variety of issues including equity, efficiency and severity of disease. Ranking and weighting of these considerations varies across countries.
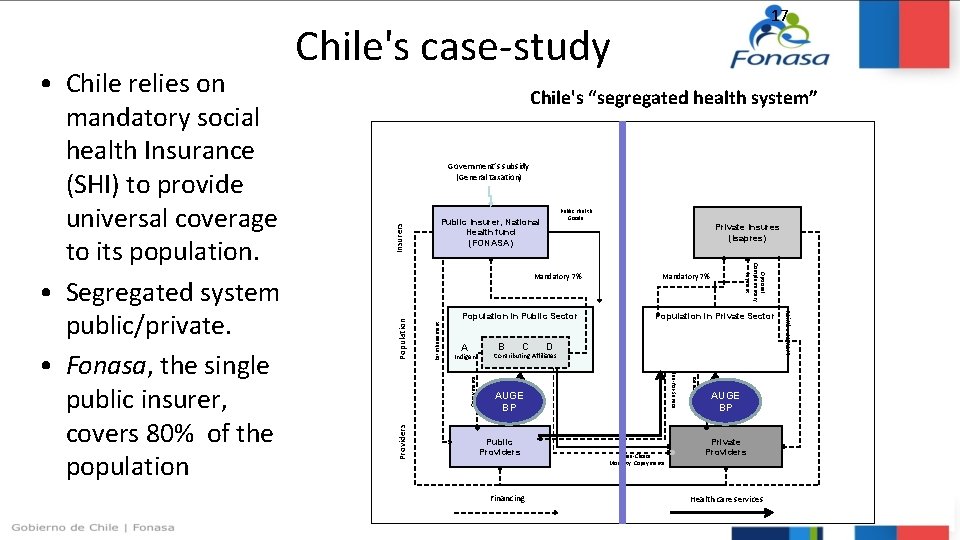
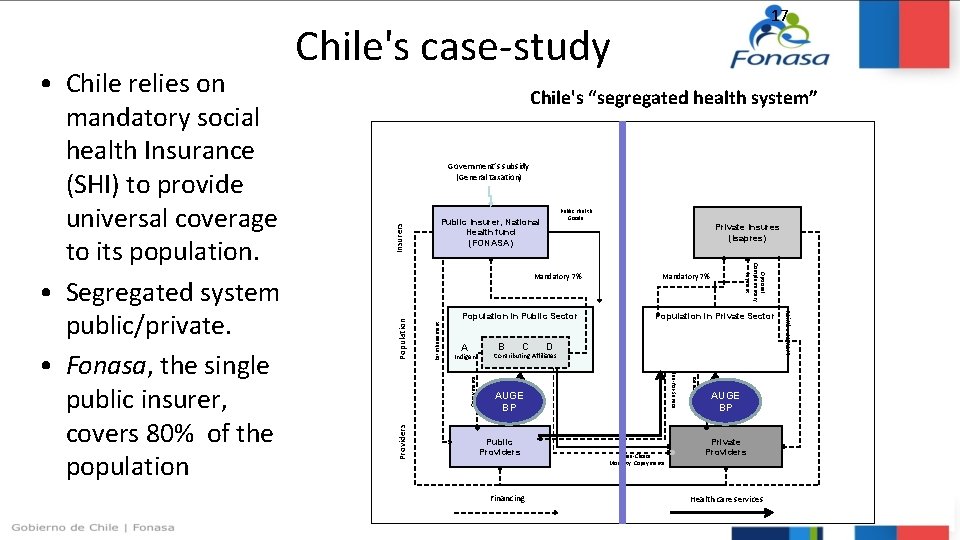
Costing a BP: Chile’s case Chile's case-study Chile's “segregated health system” Public Insurer, National Health fund (FONASA) Public Health Goods Population in Private Sector B C D A Indigent Copayments Reimbursement Population Providers Mandatory 7% Contributing Affiliates AUGE BP Public Providers Financing Free-Choice Modality: Copayments AUGE BP Private Providers Health care services Reimbursement Population in Public Sector Optional Complementary Payment Mandatory 7% Private Insures (Isapres) Copayments Insurers Government’s subsidy (General taxation) Fee-for-Service • Chile relies on mandatory social health Insurance (SHI) to provide universal coverage to its population. • Segregated system public/private. • Fonasa, the single public insurer, covers 80% of the population 17

Chile: A segregated health social security system • Isapre beneficiaries belong mainly to the two upper income quintiles. 18
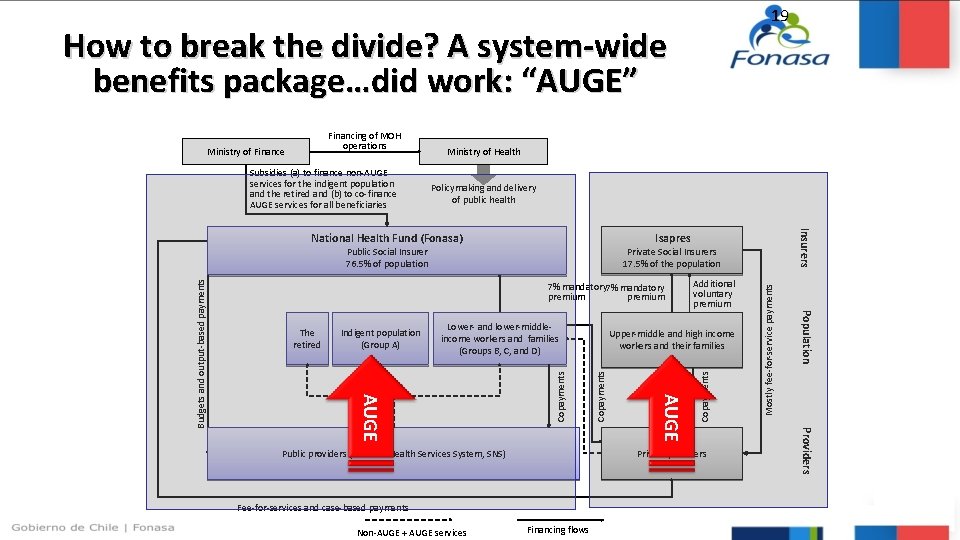
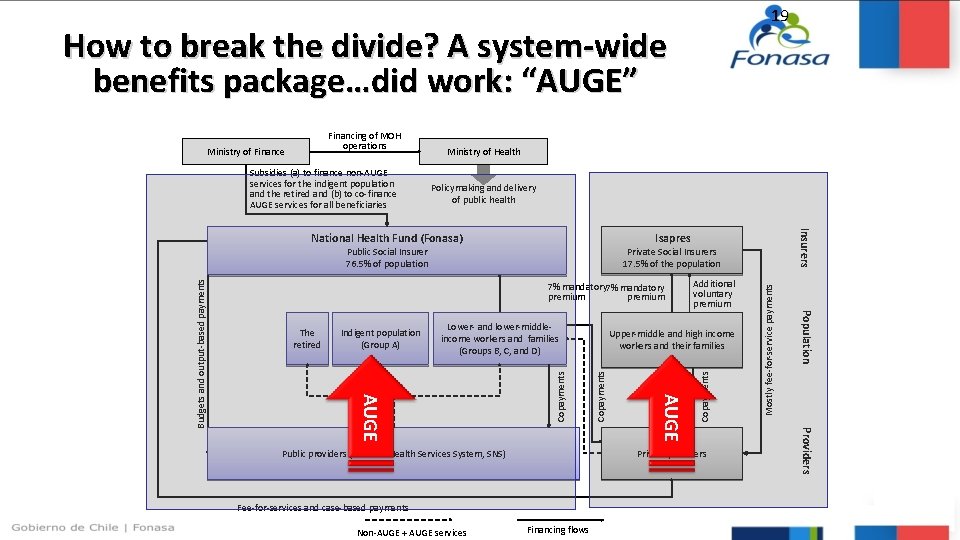
19 How to break the divide? A system-wide benefits package…did work: “AUGE” Subsidies (a) to finance non-AUGE services for the indigent population and the retired and (b) to co-finance AUGE services for all beneficiaries Ministry of Health Policymaking and delivery of public health Private Social Insurers 17. 5% of the population 7% mandatory premium Fee-for-services and case-based payments Financing flows Providers Copayments Private providers Public providers (National Health Services System, SNS) Non-AUGE + AUGE services Upper-middle and high income workers and their families AUGE Copayments Lower- and lower-middleincome workers and families (Groups B, C, and D) Additional voluntary premium Population Indigent population (Group A) AUGE Budgets and output-based payments Public Social Insurer 76. 5% of population The retired Insurers Isapres National Health Fund (Fonasa) Mostly fee-for-service payments Ministry of Finance Copayments Financing of MOH operations
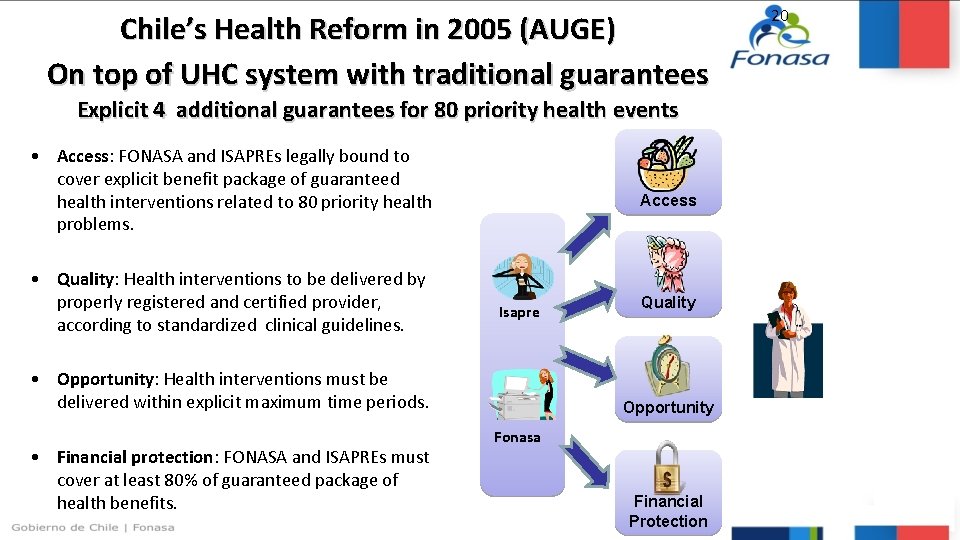
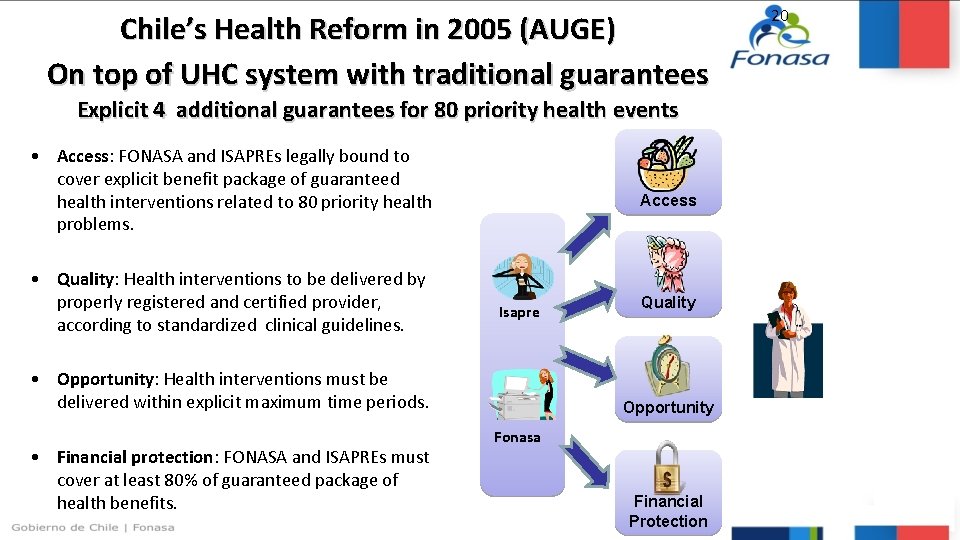
Chile’s Health Reform in 2005 (AUGE) On top of UHC system with traditional guarantees Explicit 4 additional guarantees for 80 priority health events • Access: FONASA and ISAPREs legally bound to cover explicit benefit package of guaranteed health interventions related to 80 priority health problems. • Quality: Health interventions to be delivered by properly registered and certified provider, according to standardized clinical guidelines. Access Isapre • Opportunity: Health interventions must be delivered within explicit maximum time periods. • Financial protection: FONASA and ISAPREs must cover at least 80% of guaranteed package of health benefits. Quality Opportunity Fonasa Financial Protection 20

21 AUGE’s prioritized list of 80 medical problems Health problem Year of adoption: 2005 1. End-stage chronic renal failure 2. Operable congenital heart disease (under 15 years of age) 3. Cancer of the uterus or cervix 4. Cancer pain relief and palliative care 5. Acute Myocardial Infarction 6. Diabetes Mellitus Type I 7. Diabetes Mellitus Type II 8. Breast cancer (15 years of age or more) 9. Spinal Dysraphia 10. Scoliosis surgery (under 25 years of age) 11. Cataract surgery 12. Total hip replacement in people with severe osteoarthritis of the hip (65 years of age or more) 13. Cleft palate 14. Cancer (under 15 years of age) 15. Schizophrenia 16. Testicular cancer (15 years of age or more) 17. Lymphoma (15 years of age or more) 18. HIV/AIDS 19. Ambulatory care lower ARI (under 5 years of age) 20. Ambulatory pneumonia (65 years of age or more) 21. Primary or essential arterial hypertension 22. Epilepsy (non-refractory) (1 to 15 years of age) 23. Prevention and education for oral health (6 years old) 24. Prematurity-Retinopathy of prematurity-Deafness of prematurity 25. Conduction disturbance for those with pacemakers (15 years of age or more) Year of adoption: 2006 26. Bladder cancer preventive cholecystectomy 27. Gastric cancer 28. Prostate cancer 29. Adult leukemia 30. Strabismus (under 9 years of age) 31. Diabetic retinopathy 32. Retinal detachment 33. Hemophilia 34. Depression (15 years of age or more) 35. Benign prostatic hyperplasia 36. Acute stroke 37. Chronic obstructive pulmonary disease 38. Bronchial asthma 39. Newborn respiratory distress syndrome 40. Orthesis and aids (65 years of age or more) Health problem Year of adoption: 2007 41. Deafness (65 years of age or more) 42. Ametropia (65 years of age or more) 43. Eye trauma Cystic fibrosis 44. Severe burns 45. Alcohol and drug dependency (10 to 19 years of age) 46. Pregnancy and delivery integral care 47. Rheumatoid arthritis 48. Knee arthrosis (55 years of age or more) and hip arthrosis (60 years of age or more) 49. Intracranial aneurysm and venous malformation rupture 50. Central nervous system tumors 51. Herniated nucleus pulposus 52. Dental emergencies 53. Dental care (65 years of age or more) 54. Politrauma 55. Traumatic brain injury 56. Retinopathy of Prematurity Year of adoption: 2010 57. Bronchopulmonary dysplasia of prematurity 58. Bilateral sensorineural hearing loss of prematurity 59. Epilepsy in patients over 15 year 60. Bronchial asthma in patients over 15 year 61. Parkinson 62. Juvenile idiopathic arthritis 63. Secondary prevention of chronic renal failure 64. Hip dysplasia 65. Integral oral health in pregnant women 66. Multiple Sclerosis 67. Hepatitis B 68. Hepatitis C Year of adoption: 2013 69. Colorectal cancer in people aged 15 years and over 70. Epithelial ovarian cancer 71. Bladder cancer in persons 15 years and over 72. Osteosarcoma in persons 15 years and over 73. Surgical treatment of chronic lesions of the aortic valve in people aged 15 years and more 74. Bipolar disorder in persons 15 years and over 75. Hypothyroidism in persons 15 years and over 76. Treatment of moderate hearing loss in children under 2 years (1) 77. Note: Applies to a hearing deficit at or above 40 decibels secondary to a histological damage to the inner ear 78. Systemic lupus erythematosus 79. Surgical treatment of chronic lesions of the mitral and tricuspid valves in people 15 years and over 80. Treatment to eradicate helicobacter pylori
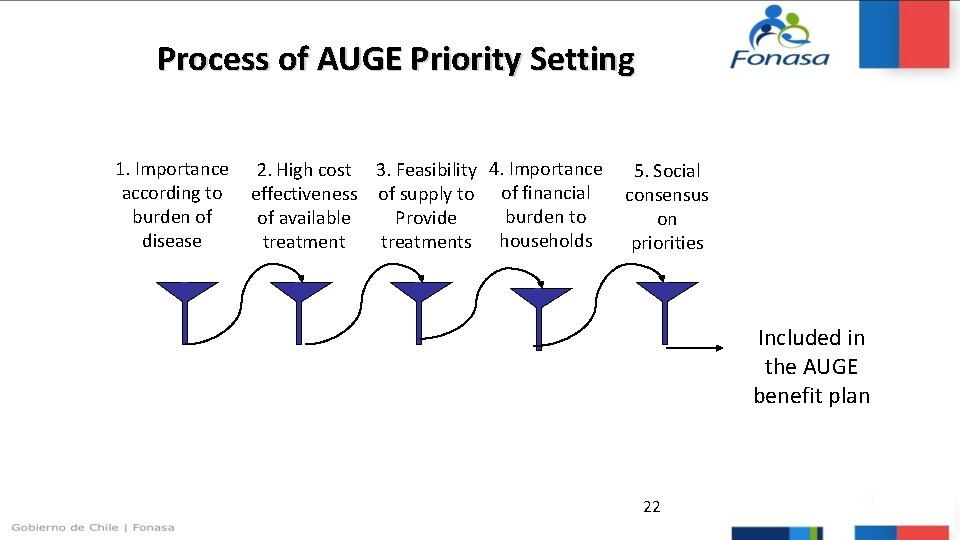
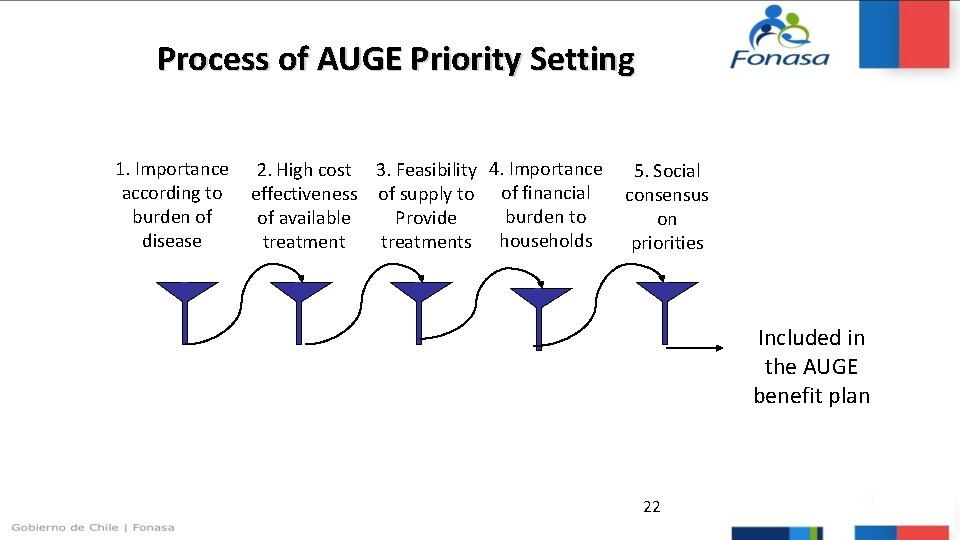
Implementation issues 22 Process of AUGE Priority Setting 1. Importance 2. High cost 3. Feasibility 4. Importance 5. Social according to effectiveness of supply to of financial consensus burden of burden to Provide of available on disease treatments households treatment priorities Included in the AUGE benefit plan 22
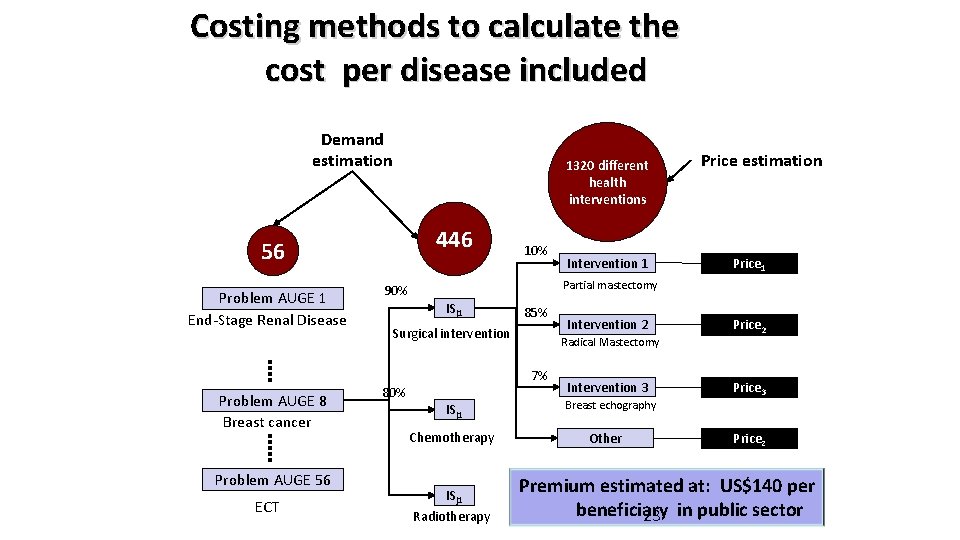
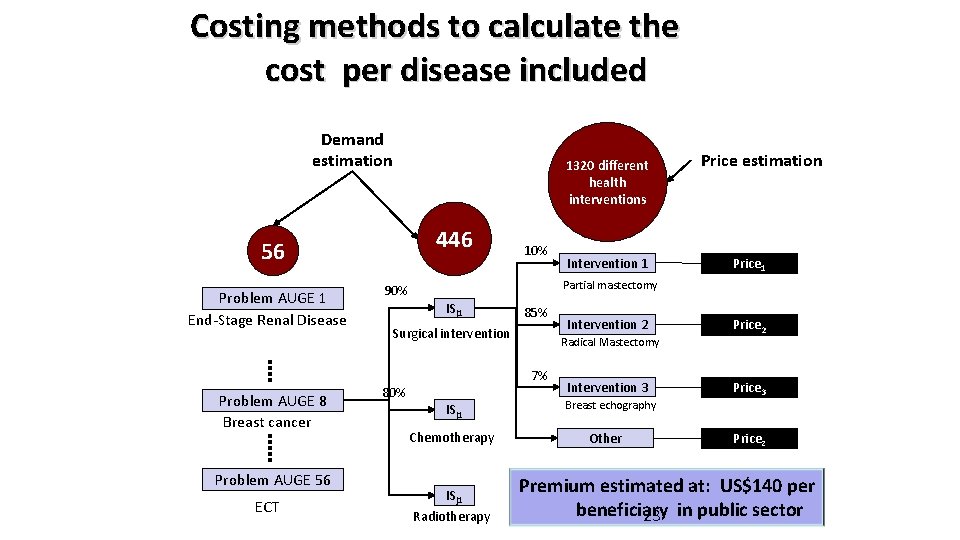
Costing methods to calculate the cost per disease included Demand estimation 1320 different health interventions 446 56 Problem AUGE 1 End-Stage Renal Disease Problem AUGE 8 Breast cancer Problem AUGE 56 ECT 10% Intervention 1 23 Price estimation Price 1 Partial mastectomy 90% ISj 1 85% Surgical intervention Radical Mastectomy 7% 80% ISj 1 Chemotherapy ISj 1 Radiotherapy Intervention 2 Intervention 3 Breast echography Other Price 2 Price 3 Pricez Premium estimated at: US$140 per beneficiary 23 in public sector

Final benefit package is a mixed of Diseases with high burden of disease • Schizophrenia • Hypertension Diseases with high financial burden • End-stage chronic renal failure • Variety of Cancers and Heart Disease • HIV/AIDS Diseases with existing • Cataracts • Hip fracture high cost effective interventions Diseases with high social priority • Lower acute respiratory • Oral health in children less than 6 years old
Conclusions 1. Advancing toward UHC includes defining: who should be covered? , how to pay for it, and what services should be covered first. 2. Priority setting is a complex, political and “muddy” process 3. Various tools for priority setting. Need to consider process and outcome when evaluating success 4. Priority setting usually translate into definition of the benefit package. • The benefit package must be constructed based in the local context, with explicit prioritization criteria and enforceable guarantees • Goal is that intentions meet the reality of advancing towards UHC 4. Need to monitor and measure to ensure

Thank you