Universal Health Coverage The goal of universal health













- Slides: 50
Universal Health Coverage The goal of universal health coverage is to ensure that all people obtain the health services they need without suffering financial hardship when paying for them.
Definition of Universal Health Coverage For a community or country to achieve universal health coverage, several factors must be in place, including: A strong, efficient, well-run health system that meets priority health needs through people-centered integrated care (including services for HIV, tuberculosis, malaria, no communicable diseases, maternal and child health) by: q informing and encouraging people to stay healthy and prevent illness; q detecting health conditions early; q having the capacity to treat disease; and q helping patients with rehabilitation. Affordability – a system for financing health services so people do not suffer financial hardship when using them. This can be achieved in a variety of ways. Access to essential medicines and technologies to diagnose and treat medical problems. A sufficient capacity of well-trained, motivated health workers to provide the services to meet patients’ needs based on the best available evidence.
Definition of Universal Health Coverage (contd. ) It also requires recognition of the critical role played by all sectors in assuring human health, including transport, education and urban planning. Universal health coverage has a direct impact on a population’s health. Access to health services enables people to be more productive and active contributors to their families and communities. It also ensures that children can go to school and learn. At the same time, financial risk protection prevents people from being pushed into poverty when they have to pay for health services out of their own pockets. Universal health coverage is thus a critical component of sustainable development and poverty reduction, and a key element of any effort to reduce social inequities. Universal coverage is the hallmark of a government’s commitment to improve the wellbeing of all its citizens. Universal coverage is firmly based on the WHO constitution of 1948 declaring health a fundamental human right and on the Health for All agenda set by the Alma-Ata declaration in 1978. Equity is paramount. This means that countries need to track progress not just across the

What is Universal Coverage? Universal coverage (UC), or universal health coverage (UHC), is defined as ensuring that all people can use the promotive, preventive, curative, rehabilitative and palliative health services they need, of sufficient quality to be effective, while also ensuring that the use of these services does not expose the user to financial hardship. This definition of UC embodies three related objectives: q equity in access to health services - those who need the services should get them, not only those who can pay for them; q that the quality of health services is good enough to improve the health of those receiving services; and q financial-risk protection - ensuring that the cost of using care does not put people at risk of financial hardship. Universal coverage brings the hope of better health and protection from poverty for hundreds of millions of people - especially those in the most vulnerable situations. Universal coverage is firmly based on the WHO constitution of 1948 declaring health a fundamental human right and on the Health for All agenda set by the Alma‑Ata declaration in 1978. Achieving the health Millennium Development Goals and the next
History The first move towards a national health insurance system was launched in Germany in 1883, with the Sickness Insurance Law. Industrial employers were mandated to provide injury and illness insurance for their low-wage workers, and the system was funded and administered by employees and employers through "sick funds", which were drawn from deductions in workers' wages and from employers' contributions. Other countries soon began to take examples – in the United Kingdom, the National Insurance Act 1911 provided coverage for primary care (though not specialist or hospital care) for wage earners, covering about one-third of the population. The Russian Empire established a similar system in 1912, and other European countries began following suit. By the 1930 s, similar systems existed in virtually all of Western and Central Europe. Following the Russian Revolution of 1917, the Soviet Union came close to a universal health care system. It established a fully public and centralized health care system in 1920. However, it was not a truly
History (contd. ) In New Zealand, a universal health care system was created in a series of steps from 1939 to 1941. Following World War II, universal health care systems began to be set up around the world. On July 5, 1948, the United Kingdom launched its universal National Health Service. Universal health care was next introduced in the Nordic countries of Sweden (1955), Iceland (1956), Norway (1956), Denmark (1 961), and Finland (1964). Universal health insurance was then introduced in Japan (1961), and in Canada through stages, starting with the province of Saskatchewan in 1962, followed by the rest of Canada from 1968 to 1972. The Soviet Union extended universal health care to its rural residents in 1969. Italy introduced its Servizio Sanitario Nazionale (National Health Service) in 1978. Universal health insurance was implemented in Australia beginning with the Medibank system in 1975, which led to universal
History (contd. ) From the 1970 s to the 2000 s, Southern and Western European countries began introducing universal coverage, most of them building upon previous health insurance programs to cover the whole population. For example, France built upon its 1928 national health insurance system with subsequent legislation covering a larger and larger percentage of the population, until the remaining 1% of the population that was uninsured received coverage in 2000. In addition, universal health coverage was introduced in some Asian countries, including South Korea (1989), Taiwan (1995), Israel (1995), and Thailand (2001). Following the collapse of the Soviet Union, Russia retained and reformed its universal health care system, as did other former Soviet nations and Eastern bloc countries. Beyond the 1990 s, many countries in Latin America, the Caribbean, Africa, and the Asia-Pacific region, including developing countries, took steps to bring their populations under universal health coverage. A 2012 study examined progress being made by these
The Goal of Universal Health Coverage Although this report is not primarily about why countries should pursue UHC, it is useful to outline the strong and multifaceted rationale for that goal. First, securing access to health services is motivated by the individual benefits from service utilization. These improvements in health can be seen as an end in themselves as well as crucial to overall well-being and the related concepts of capabilities and opportunities. Health can affect overall well-being directly and indirectly, for example, through income and wealth. Health can also be seen as of great importance due to its
The Goal of Universal Health Coverage (contd. ) q From the same perspectives, it is also evident why affordable access is so important. Like poor health, large payments for services can severely limit well-being and opportunities, not only for the individual who uses the service, but also for his or her family. Affordable access across the entire continuum of care also facilitates these of preventive services, and these services are often more costeffective than the corresponding curative services. Moreover, affordable access confers benefits even to those who do not eventually need health services. Among other things, knowledge of affordable access can reduce anxiety and the fear of becoming ill and make people sleep better at night. Such knowledge can also facilitate q Widespread coverage is also beneficial to society at large. Improved coverage improves population health, and health contributes to development directly, as indicated by, for example, the Human Development Index (HDI). In addition, health affects development and the overall well-being of society indirectly. Healthy children are better able to learn, and a healthy population facilitates economic growth. According to one study, for every dollar spent on key services, the direct and indirect economic returns—measured as “full income”—can be multiplied
The Goal of Universal Health Coverage (contd. ) q UHC can further be motivated by its distributional effects. Irrespective of the total benefits to society, universal health coverage can be supported by the idea that coverage should not be restricted to the better-off part of the population or, more specifically, by the idea that such a restriction is unfair. Insofar as it improves coverage for the worse off, progress toward UHC can also promote fairer distribution of health and well -being. q UHC is also a way to meet rights to health care and the human right of “the enjoyment of the highest attainable standard of physical and mental health, ” which is recognized under international law. Every country in the world has ratified at least one treaty that specifies obligations regarding the right to health. Under international law, states have an obligation to adopt appropriate measures to realize the right to health or the right to health care on a nondiscriminatory basis (as some treaties specify). This obligation involves a strategy and plan of action for how to achieve that goal as wells mechanisms for oversight and redress. Parties to specific international treaties also have obligations to allocate sufficient resources to realize the right to health. In other words, states have an obligation to adopt appropriate measures to realize the right to health, and the pursuit of UHC is crucial to this
The Scope of Universal Health Coverage UHC must be understood in a comprehensive way. More specifically, the goal of UHC calls for quality services of many kinds, for strengthening the entire health system, and for intersectoral action.
The Scope of Universal Health Coverage (contd. ) q As for services, UHC goes beyond clinical and curative services to include public health and population measures and promotive, preventive, and rehabilitative services. Public health coverage and population measures include, for example, informational campaigns on hygiene and food safety, vector control, and tobacco regulation. Services, broadly understood, also include the provision of drugs, devices, and other goods. Especially regarding essential medicines, considerable effort has been exerted to promote universal access. For all services, quality, not only quantity, is paramount. When moving toward UHC, countries must ensure that everyone has q UHC calls for action going beyond the health sector and the health system, as the means for improving access to health services and financial protection are not confined to that sector and system. For example, affordable access may crucially depend on policies in sectors concerned with transportation, employment, education, and finance. The pursuit of UHC therefore requires intersectoral action. In addition, the underlying objective of improving health—and not only health services—requires approaches that go beyond the health sector also more generally. Countries must address the broader determinants of health, including social determinants such as education,
The Scope of Universal Health Coverage (contd. ) q Finally, although most UHC initiatives concentrate on domestic health policy, the broader, ultimate goal of comprehensive coverage for everyone in the world should be kept in view. Today, differences in health and service coverage are profound both across and within countries. For example, in 2010, healthy life expectancy at birth formals ranged from 37. 7 healthy life years in the Central African Republic to 70. 6 in Japan. Likewise, under-five mortality rate (U 5 MR) varied from 180 to 2 per 1, 000 live births. Differences in service coverage are no less pronounced. For example, the percentage of one-year-olds who has received the third those of diphtheriatetanuspertussisvaccine varies (DTP 3) from 33 percent to 99 percent, and the percentage of births attended by skilled health personnel ranges from 9 percent to 100 percent. What is particularly troubling is that inequalities in health and inequalities in service coverage are often correlated, so that coverage is the least where needs are the greatest. These inequalities and the variation in country capacity to address health needs raise number of important issues. In particular, there is a question about how capable countries can and should assist countries that alone are unable to adequately address domestic needs. Concerns for global justice, global solidarity, and human rights

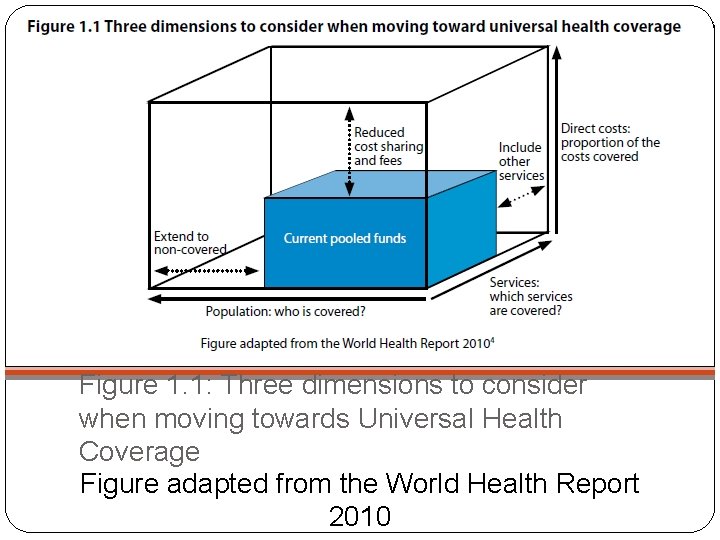
Dimensions of Progress and Critical Choices q. Several countries have recently demonstrated that significant steps toward UHC can be taken, even in resourceconstrained settings. Among these countries are. Cambodia, Chile, China, Colombia, Ghana, Indonesia, Mexico, the Philippines, q Obviously, no country starts from zero coverage, and there is no single path to UHC that every country must follow. To achieve UHC, however, every country must make progress in at least three dimensions. Countries must expand priority services, include more people, and reduce out-of-pocket payments. These three dimensions closely correspond to those often emphasized in the context of financing and, more specifically, the dimensions of the now well-known UHC box. This box is shown in figure 1. 1. The box illustrates three dimensions to consider when moving toward UHC. These concern (a) the proportion of the population to be covered, (b) the range of services to be made available, and (c) the proportion of the total costs to be met. More specifically, the first dimension is linked to the proportion of people covered from pooled funds, while third dimension refers to the proportion of total costs to be met by pooled funds.
Dimensions of Progress and Critical Choices (contd. ) q As indicated, in this report the three dimensions are interpreted somewhat more broadly. Although expanding priority services typically requires changes in financing, expansion can also follow from other changes. For example, coverage for priority services can be expanded through a change in the use of health personnel or the use of existing technologies and infrastructure. Moreover, reducing barriers to coverage requires action on many nonfinancial barriers and the use of nonfinancial means. These barriers include stigma and cultural norms, for example. q In each dimension, countries moving forward will face at least one critical choice regarding fairness and equity. When expanding priority services, countries must decide which services to expand first. When including more people, countries must decide whom to include first. And when reducing out-ofpocket payments, countries must decide how to shift from such payment toward prepayment. The dimensions of progress and the related choices are summarized in box 1. 1.
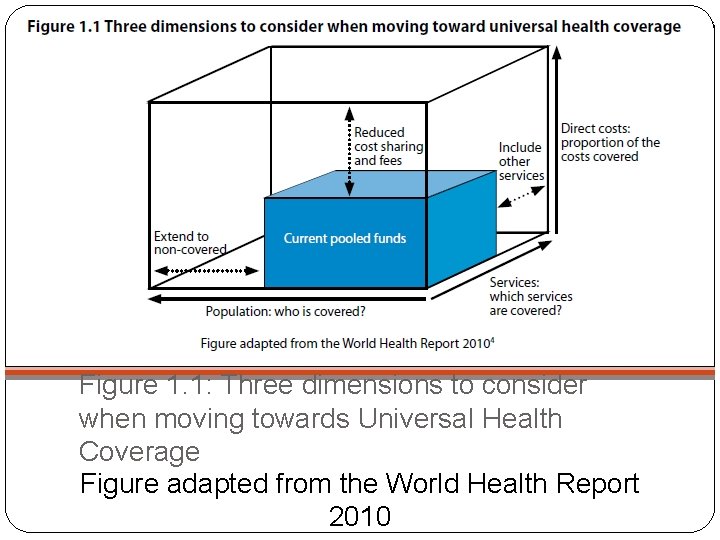
Figure 1. 1: Three dimensions to consider when moving towards Universal Health Coverage Figure adapted from the World Health Report 2010

Dimensions of Progress and Critical Choices (contd. ) Dimensions of progress Expanding priority services Including more people Critical Choice Which services to expand first? Whom to include first? How to shift from out-of Reducing out-of-pocket payments toward prepayment? Box 1. 1: Critical dimensions and choices on the path to universal health coverage
Expanding priority services Progress toward UHC can be sought by expanding priority services. However, no country can cover all services that are expected to be beneficial. For each step toward UHC, countries must therefore choose among different services that all need to be expanded. Countries are then faced with the following choice: Which
Including more people Progress toward UHC can be sought by including more people. To do so, countries must seek to reduce all barriers to effective coverage. Among these barriers are prohibitive payments for services and other financial barriers and many nonfinancial barriers. The latter include legal, organizational, technological, informational, geographic, and cultural barriers. Since these barriers cannot be eliminated for everyone immediately, countries are faced with
Reducing out-of-pocket payments Progress toward UHC can be sought by reducing out-of-pocket payments while increasing mandatory prepayment, for example, in the form of taxes or premiums. When doing so, countries are faced with the following choice: How to shift from out -of-pocket payment toward prepayment?
The Context of Choice Numerous actors influence the progress toward UHC. These actors are institutions, groups, and individuals, within and outside government, locally, nationally, and internationally. Their choices are shaped by multiple considerations, which include economic and political circumstances and the actors’ economic and political interests as well as their ideals. Central among these ideals are those related to fair and equitable distribution of benefits and burdens in society. This report addresses issues of fairness and equity arising on the path to UHC. For all actors affecting that path, it is crucial to be keenly aware of these issues and to make the accompanying decisions with care. Central among these actors are obviously health workers. This report, however, mainly addresses the choice situations relevant for governments in charge of overseeing and guiding the progress toward UHC. In particular, the
Key Facts q At least a billion people suffer each year because they cannot obtain the health services they need. q People-centered and integrated health services are critical for reaching universal health coverage. q About 150 million of the people who do use health services are subjected to financial catastrophe annually, and 100 million are pushed below the poverty line as a result of paying for the services they receive. q In the next twenty years, 40 -50 million new health care workers will need to be trained and deployed to meet the need. q Globally, two-thirds (38 million) of 56 million annual deaths are still not registered.

Dispelling Myths about UHC q UHC is not just health financing, it should cover all components of the health system to be successful: health service delivery systems, health workforce, health facilities or communications networks, health technologies, information systems, quality assurance mechanisms, governance and legislation. q UHC is not only about assuring a minimum package of health services, but also about assuring a progressive expansion of coverage of health services and financial risk protection as more resources become available. q UHC does not mean free coverage for all possible health interventions, regardless of the cost, as no country can provide all services free of charge on a sustainable basis. q UHC is comprised of much more than just health; taking steps towards UHC means steps towards equity, development priorities, social inclusion and cohesion.
Strong Health Systems for UHC � Moving towards UHC requires strengthening health systems in many countries. An important component of UHC is health financing where attention needs to be paid to raising sufficient funds, minimizing out of pocket payments through prepayment and pooling, and using available funds (including donor funding where relevant) efficiently and equitably. � Countries must also have a health workforce that can support an affordable, efficient, well-run health system that meets priority health needs through quality people -centered integrated care. Good governance, sound systems of procurement and supply of medicines and health technologies and well-functioning health information systems are other critical elements.

Strong Health Systems for UHC (contd. ) q UHC emphasizes not only what services are covered, but also how they are covered through focusing on peoplecentered health care and integration of care. A shift in health service delivery is necessary to better tailor services to the individuals of the population they serve. Health systems should be organized around the needs and expectations of people in terms of holistic long-term health to help them better understand their own health-care needs. q Integrated health services mean a delivery that enables people to receive a continuum of health promotion, disease prevention, diagnosis, treatment, disease-management, rehabilitation and palliative care services, through the different levels and sites of care within the health system over the course of a lifetime. Members of a community are then better equipped to take preventative measures on their own creating cost-saving efficiency in the long term.

Benefits of Implementing UHC q UHC maintains and improves health. Good health allows children to learn and adults to earn. This helps people escape from poverty and provides the basis for long-term economic development. q At the same time, financial risk protection in health prevents people from being pushed into poverty because unexpected illness requires them to use up their life savings, sell assets, or borrow – destroying their futures and often those of their children.
Can progress be monitored? q Monitoring progress towards UHC should focus on both coverage of the population with essential quality health services and on financial protection against catastrophic out-of-pocket health payments. Special attention should be given to the most disadvantaged population groups, such as the poorest individuals or those living in remote rural areas. q Monitoring should be placed within a broader health systems performance framework which allows health workers, medicines, technologies to be tracked, and impacts on health and financial security to be measured. q It is important for countries to measure their progress towards UHC. Given each unique country-specific context the measuring indicators may be focused on different areas. There is also value in a global framework for monitoring UHC that uses standardized measures that are internationally recognized so that they are comparable across borders and over time.
WHO Response q WHO is supporting countries to develop their health systems to move towards, and to sustain, UHC, and to monitor progress. q WHO along with the World Bank has developed a framework to track the progress of UHC. By monitoring UHC countries can check objectives and focus on areas that need extra attention. The framework has 3 overall indicators: Ø health service coverage; Ø financial risk protection; and Ø equity or coverage for the entire population. q The purpose of measuring these indicators is to progressively achieve UHC for all countries.

WHO Response (contd. ) q This is but one of the many forms of partnership around strengthening health systems in the search for UHC. This need, despite large inflows of disease-specific funding in recent years, has been starkly illustrated by the Ebola outbreak. Other forms of partnership include: Ø International Health Partnerships (IHP+) Ø Alliance for Health Policy and Systems Research Ø Providing for Health (P 4 H) Ø Global Health Workforce Alliance Ø UHC Partnership q In 2008 Member States endorsed the resolution on ‘Strengthening national policy dialogue to build more robust health policies, strategies and plans’. WHO is currently writing a handbook on national health policies, strategies and plans towards UHC in the hopes that it will be adapted for capacity-building workshops for health ministries. q All countries can do more to improve health outcomes and tackle poverty, by increasing coverage of health services, and by reducing the impoverishment associated with payment for health services.
Universal Health Coverage: Bangladesh Perspective Recently, BRAC, ICDDR, B, Centre of Excellence for Universal Health Coverage and The Daily Star have organized a roundtable on “Universal Health Coverage: Bangladesh Perspective”. Here we publish a summary of the discussion.
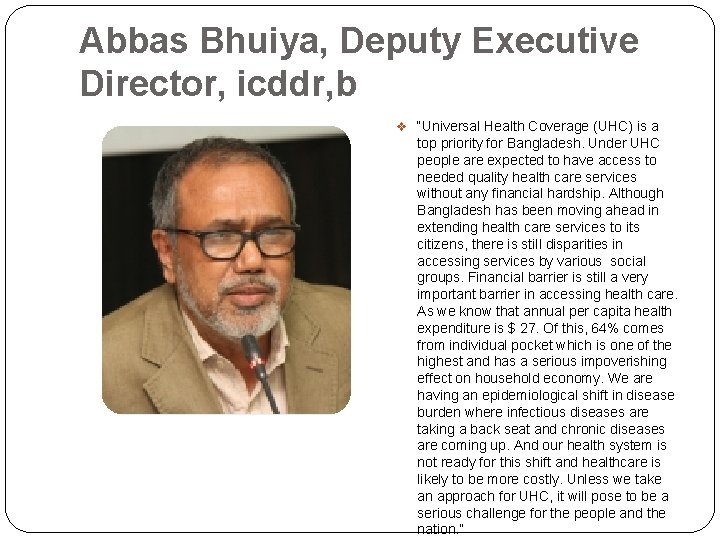
Abbas Bhuiya, Deputy Executive Director, icddr, b v “Universal Health Coverage (UHC) is a top priority for Bangladesh. Under UHC people are expected to have access to needed quality health care services without any financial hardship. Although Bangladesh has been moving ahead in extending health care services to its citizens, there is still disparities in accessing services by various social groups. Financial barrier is still a very important barrier in accessing health care. As we know that annual per capita health expenditure is $ 27. Of this, 64% comes from individual pocket which is one of the highest and has a serious impoverishing effect on household economy. We are having an epidemiological shift in disease burden where infectious diseases are taking a back seat and chronic diseases are coming up. And our health system is not ready for this shift and healthcare is likely to be more costly. Unless we take an approach for UHC, it will pose to be a serious challenge for the people and the nation. ”
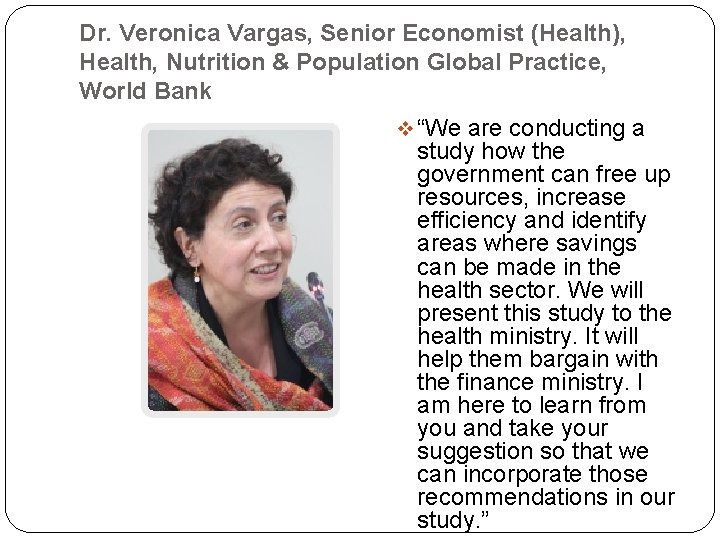
Dr. Veronica Vargas, Senior Economist (Health), Health, Nutrition & Population Global Practice, World Bank v “We are conducting a study how the government can free up resources, increase efficiency and identify areas where savings can be made in the health sector. We will present this study to the health ministry. It will help them bargain with the finance ministry. I am here to learn from you and take your suggestion so that we can incorporate those recommendations in our study. ”

Kelvin Hui, Principal Advisor, GIZ v “UHC is not only about access. It is also about quality of health service. The challenges and the landscape keep changing. Locally we always hear about the negative perception of pooling money through health insurance. Government collecting taxes and providing health services is actually also a method of pooling money. Some countries like UK, Norway and Malaysia have done remarkably through this type of pooling system but it requires very strong governance. There are countries which pools money differently, through a system of social health insurances and give patients the choice of accessing either private or public facilities which has also done very well in achieving UHC. v At the end of the day, what is necessary is that we learn from examples of various countries and pick the most suitable for Bangladesh. From the German Development Cooperation perspective what we want to do is to facilitate this learning. We need to consider coverage, quality of health care, out of pocket expenses and stimulate debate amongst civil society and policy makers so to
Dr. Sukumar Sarkar, Senior Technical & Policy Advisor, USAID v “From USAID we see UHC as a goal as well as a process of incremental policies and program decisions. UHC is mainly for resource poor setting. Here comes the question of prioritization. Do we need to prioritize in terms of population segment? UHC has not yet defined any definite approach, strategy, target, objective and all those things. Even, what are the services we should provide under UHC? That is something we need to think about. Our demography is changing. More and more population is getting into the aged group. There is a need for services of noncommunicable diseases. So we need to define a strategy for UHC in Bangladesh. v Another issue is domestic resource mobilization. Donors' funds are shrinking. So we have to think about how we can mobilize our own resources to sustain what we have achieved. Leveraging private resources and pulling it into health program can be one of the alternatives. In India they have already started such programs. In the health ministry there is no such cell that can look after pulling private resources for the health sector
Dr. A. M. Zakir Hussain, Former Director Primary Health Care & Disease Control, Directorate of Health Services and former Regional Advisor, South East Regional Office of WHO v “What do we need healthcare? We need it basically for diagnosis and treatment of diseases and for prevention of diseases. Private health insurance system will never include preventive care. That's why we talk about universal health coverage. Universal health coverage, i. e. UHC, is there, but actually it is not there, in Bangladesh. Government tries to cover everyone with all types of health care but it fails to do so. v Social health insurance, is a UHC, which is a mandatory process, where somebody is paying for somebody else, in addition to his or her own, although he/she doesn't need services all the time. So the question is who will pay how much, to whom and for what. The payment system is itself complex, different payment approaches have different degrees of efficiency and complexity, based on the type and magnitude of coverage. Who will ensure this? Patients cannot, because they are not health literate. So some
Questions and Answers on Universal Health Coverage and the post-2015 Framework
How does universal health coverage contribute to sustainable development? Universal health coverage (UHC) has a direct impact on a population’s health and welfare. Access to health services enables people to be more productive and active contributors to their families and communities. It also ensures that children can go to school and learn. At the same time, financial risk protection prevents people from being pushed into poverty when they have to pay for health services out of their own pockets. Universal health coverage, requiring coverage with needed health services and with financial risk protection, is thus a critical component of sustainable development and poverty reduction, and a key element of any effort to reduce social inequities. Universal coverage is the hallmark of a government’s commitment to improve the wellbeing of all its
How can universal health coverage contribute to continued progress on the current Millennium Development Goals (MDGs) while taking into account new health priorities? Moving closer to universal health coverage requires increasing equitable access to all types of needed health services. This implies continuing efforts to increase the availability and quality of services linked to the current MDGs, such as for HIV/AIDS, TB, malaria, child health or maternal health. It also requires considering how best to improve availability, quality and access to key interventions targeting newer health priorities including non-communicable diseases and injuries. Universal health coverage is, therefore, a way of ensuring continued progress towards the current health MDGs, while also helping countries address the growing
If UHC is included in the post 2015 framework, how can progress be measured? Universal health coverage requires that people have access to the health services they need without fear of the financial consequences. Measurement is straightforward. Do people obtain the health services they need and do they have financial risk protection in doing so? There is agreement on the range of indicators currently used to measure the health MDGs, some tracking service coverage (e. g. deliveries attended by skilled health workers) and some showing the impact of this (e. g. maternal mortality rates). There is also general agreement about the indicators that can be used to measure financial risk protection – the proportion of the population pushed into poverty by out-of-pocket health payments and/or the proportion suffering severe financial consequences (usually defined as paying more than 40% of their disposable income on health in any time period). The indicators currently used for the health MDGs could still be used to measure progress towards a goal of universal health coverage, particularly if they are categorized by income group and other determinants of inequality to allow countries to track progress in improving access across the entire
If UHC is included in the post 2015 framework, how can progress be measured? (contd. ) Discussions are still underway regarding indicators to measure coverage for non-communicable diseases – how to capture the large number of health interventions spanning the range of promotion, prevention, treatment and rehabilitation. A small set of tracer indicators needs to be chosen for the post-2015 framework, although countries themselves could monitor much larger sets. As an example, the proportion of smokers in the adult population is a good indicator of the effectiveness of anti-smoking interventions that are so critical to the control of non-

Does UHC improve equity and meet the needs of vulnerable populations? UHC is all about equity and is fundamental to providing social protection for health. The poorest populations usually face the highest health risks and need more health services. A key element of financing for universal health coverage is that the health costs of the poor and vulnerable are shared by the society as a whole. The financing system should aim to spread the financial risks of illness across a wide population, by collecting large pools of prepaid funds that people can draw on to cover their health care costs at times of need, regardless of their ability to pay.
Does UHC improve equity and meet the needs of vulnerable populations? (contd. ) Ensuring access to health facilities, workers and medicines in remote, rural areas is also important, as well as providing special interventions for certain ethnic groups and stigmatized populations. This means that countries need to monitor if they are increasing access to needed services not just for the population as a whole but for different groups as well (e. g. by income level,
Is UHC strong enough politically to commit decision-makers and gain public support? Availability, affordability and access to health services are increasingly becoming election issues, engaging the attention of politicians as well as voters. People all over the world want the reassurance that they can use good quality health services without worrying whether they can afford them. It is easy for people to understand that this requires accessible health facilities, well-trained and motivated health workers, medicines and equipment, and that the costs for those services are affordable. Many governments have realized that this is a major concern among their populations and more than 80 countries are in the process of evaluating and revising their health and health financing strategies with a
Would it be better to have separate targets for each of the individual disease areas rather than them being under the umbrella of UHC? The question is: how many health-specific goals will it be possible to include in the post-2015 framework? Many other sectors are pushing to include additional goals on areas they argue were neglected in the current MDGs – e. g. climate change and the environment. The United Nations has made a commitment to act to reduce the burden of noncommunicable diseases in addition to addressing the unfinished agenda for the current health-MDGs. Most observers feel that it is unlikely that it will be possible to have more health-specific goals than in the current set, and many are predicting that it will be possible to have only one. If that turns out to be true, an umbrella goal that covers all of the important health problems seems to be the appropriate solution, each of them can then have separate targets and

Is UHC too ambitious a goal? Universal Health Coverage is a dynamic process. It is not about a fixed minimum package, it is about making progress on several fronts: the range of services that are available to people; the proportion of the costs of those services that are covered; and the proportion of the population that are covered. Few countries reach the ideal, but all – rich and poor – can make progress. It thus has the potential to be a universal goal. Countries will move towards this goal at different paces depending on disease problems, levels of income and many other factors. In human rights terms, there needs to be a vision of where the country wants to go, and how it plans to get there, with a clear indication of how it aims

Could this progressive implementation be an excuse for countries not fulfilling their responsibilities towards the right to health? Countries, with the meaningful participation of all stakeholders including communities, would set their own goals and targets for improving access to services, increasing availability and quality, and improving financial risk protection. At the global level, the targets for expanding coverage in each area (e. g. HIV, TB, malaria, maternal and child health, non-communicable diseases and injuries) will be set by international consensus depending partly on the time frame adopted in the post-2015 framework. The availability of a common set of indicators would make possible to compare countries' implementation and help them move more rapidly to improving access, availability, quality and financial risk

Is UHC a way to promote private insurance? UHC is a way to increase access to health care for all without fear of financial ruin. The way countries do this will vary according to their incomes, institutions and values. Two things are clear from country experience. First, the health costs of the poor need to be met by government revenue. Governments do that in different ways. In the United Kingdom, for example, everybody receives health services paid directly by the state with resources raised by general taxation. In Thailand’s Universal Coverage Scheme, the government pays the insurance premiums of the poor from general revenues. Countries cannot provide health services to everyone by relying principally on voluntary private insurance. Second, fragmentation of insurance systems – where the rich or the formal sector have their own forms of health insurance while the poor are covered by government separately – makes it very difficult to ensure solidarity between the rich and poor and between the healthy and the sick. Fragmentation should be avoided wherever possible as
Isn’t UHC simply a means to an end rather than an end in itself? UHC is certainly a means to an end. It improves health and protects household incomes, and through this improves educational and economic opportunities – all critical components of human development. At the same time, people are reassured when they have access to affordable, quality health services. This sense of security is a critical part of human welfare. It is part of the role of governments to ensure every citizen can access a range of services that they need – in education, water and sanitation, justice or health.
What is the role of civil society and communities to support UHC? Many civil society organizations (CSOs) are actively engaged in increasing coverage with certain interventions needed by stigmatized or vulnerable groups. Others take a broader view of the need to expand coverage across a range of diseases and conditions as well as supporting communities to obtain better financial risk protection. Some CSOs are promoting that health should get a higher share of overall government budgets or that the funds should be used more equitably. Some focus on more affordable medicines. People run the risks of contracting many different types of diseases and conditions over their lives and communities are interested in ensuring they receive the appropriate services, at an affordable price, to promote and maintain their health overall. How CSOs can work together on this broader agenda while continuing to focus on their particular interests is critical. More than that, it is the meaningful participation of CSOs in the decision making process (definition, monitoring and evaluation) of national health and health financing strategies that can help to increase the range and quality of health services and the extent of financial risk protection for the population.

Credits and Sources http: //www. who. int/universal_health_coverage/e n/ http: //www. who. int/health_financing/universal_c overage_definition/en/ http: //www. thedailystar. net/universal-healthcoverage-bangladesh-perspective-64453 http: //apps. who. int/iris/bitstream/10665/112671/ 1/9789241507158_eng. pdf? ua=1
 Universal health coverage in tamil
Universal health coverage in tamil Goals of universal health coverage
Goals of universal health coverage Dimensions of universal health coverage
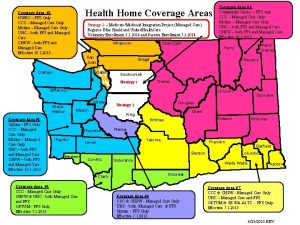
Dimensions of universal health coverage Indiana health coverage programs
Indiana health coverage programs Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Tư thế worms-breton
Tư thế worms-breton Hát lên người ơi
Hát lên người ơi Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính thế năng
Công thức tính thế năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ về giọng cùng tên
Ví dụ về giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Các số nguyên tố
Các số nguyên tố Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Ce winslow goal of public health
Ce winslow goal of public health Condition coverage
Condition coverage Current cash debt coverage
Current cash debt coverage Exclusive vs selective distribution
Exclusive vs selective distribution Fault coverage in vlsi
Fault coverage in vlsi