CostEffectiveness of Transcatheter Mitral Valve Repair versus Medical

- Slides: 17
Cost-Effectiveness of Transcatheter Mitral Valve Repair versus Medical Therapy in Patients with Heart Failure and Secondary Mitral Regurgitation: Results from the COAPT Trial Suzanne J. Baron, MD MSc On behalf of the COAPT Investigators Lahey Hospital and Medical Center, Burlington MA Saint Luke‘s Mid America Heart Institute, Kansas City MO TCT 2019 | San Francisco, CA | September 28, 2019
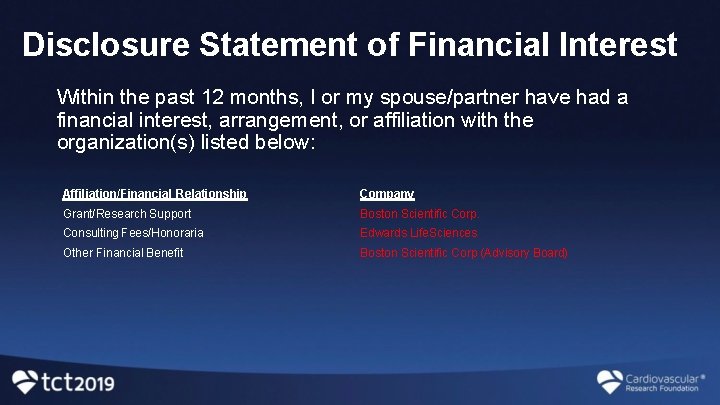
Disclosure Statement of Financial Interest Within the past 12 months, I or my spouse/partner have had a financial interest, arrangement, or affiliation with the organization(s) listed below: Affiliation/Financial Relationship Company Grant/Research Support Boston Scientific Corp. Consulting Fees/Honoraria Edwards Life. Sciences Other Financial Benefit Boston Scientific Corp (Advisory Board)
Background • The COAPT trial demonstrated that transcatheter mitral valve repair (TMVr) using the Mitra. Clip device resulted in reduced mortality and heart failure hospitalizations when compared with guideline-directed medical therapy (GDMT) in patients with symptomatic heart failure and 3 -4+ secondary mitral regurgitation (SMR) • In order to further understand the economic impact of TMVr in this population, we conducted a formal, patient-level, economic analysis alongside the COAPT trial to evaluate the long-term costs and costeffectiveness of TMVr using the Mitra. Clip device compared with GDMT in patients with heart failure and 3 -4+ SMR
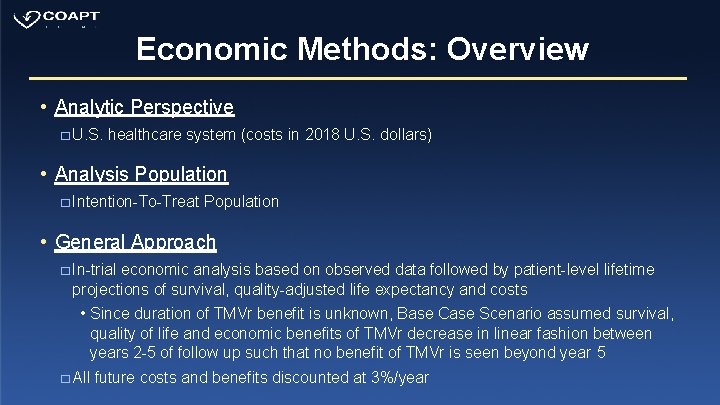
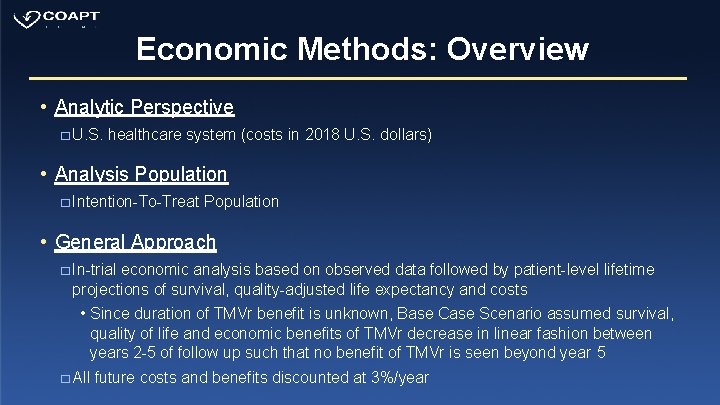
Economic Methods: Overview • Analytic Perspective � U. S. healthcare system (costs in 2018 U. S. dollars) • Analysis Population � Intention-To-Treat Population • General Approach � In-trial economic analysis based on observed data followed by patient-level lifetime projections of survival, quality-adjusted life expectancy and costs • Since duration of TMVr benefit is unknown, Base Case Scenario assumed survival, quality of life and economic benefits of TMVr decrease in linear fashion between years 2 -5 of follow up such that no benefit of TMVr is seen beyond year 5 � All future costs and benefits discounted at 3%/year
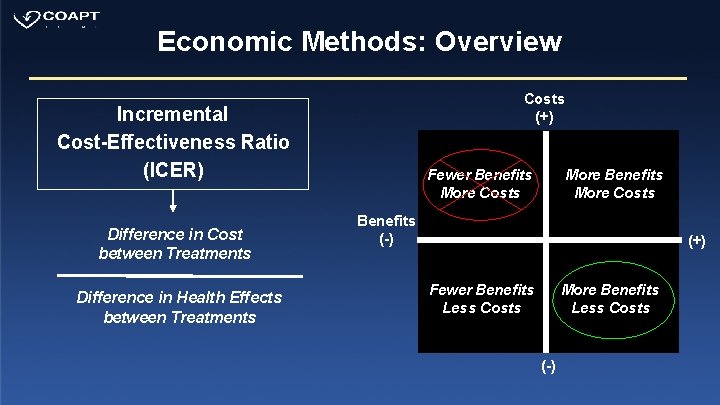
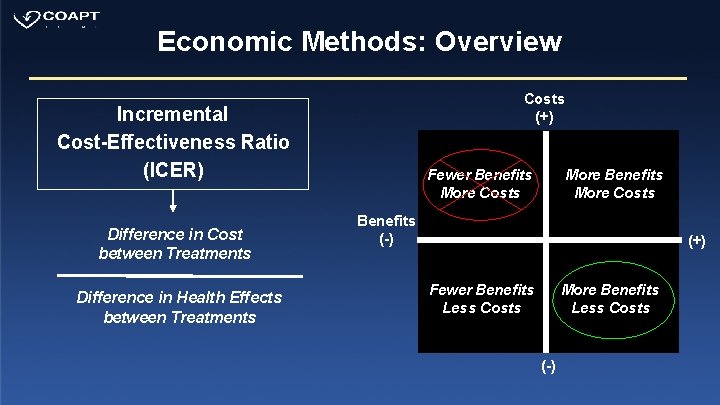
Economic Methods: Overview Costs (+) Incremental Cost-Effectiveness Ratio (ICER) Difference in Cost between Treatments Difference in Health Effects between Treatments Fewer Benefits More Costs More Benefits More Costs Benefits (-) (+) Fewer Benefits Less Costs More Benefits Less Costs (-)
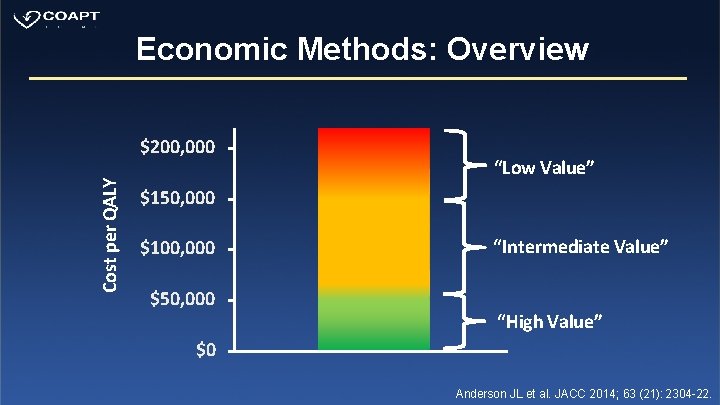
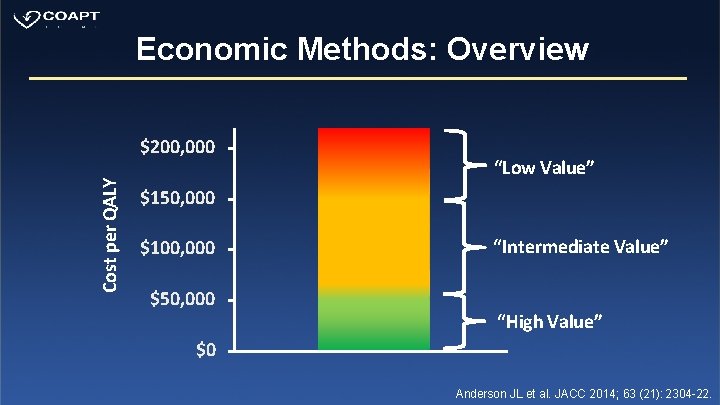
Economic Methods: Overview Cost per QALY $200, 000 “Low Value” $150, 000 $100, 000 $50, 000 “Intermediate Value” “High Value” $0 Anderson JL et al. JACC 2014; 63 (21): 2304 -22.
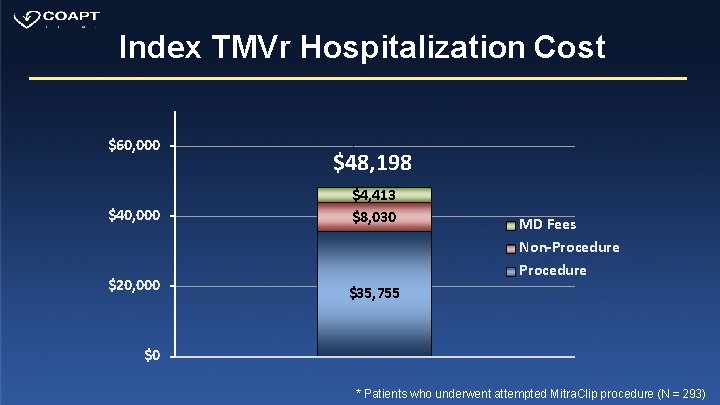
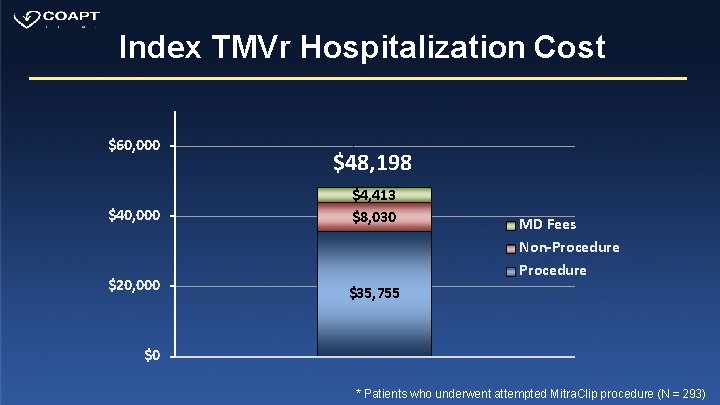
Index TMVr Hospitalization Cost $60, 000 $40, 000 $20, 000 $48, 198 $4, 413 $8, 030 MD Fees Non-Procedure $35, 755 $0 * Patients who underwent attempted Mitra. Clip procedure (N = 293)
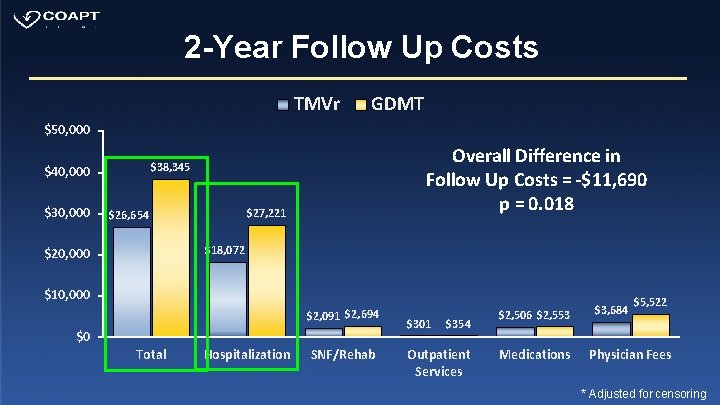
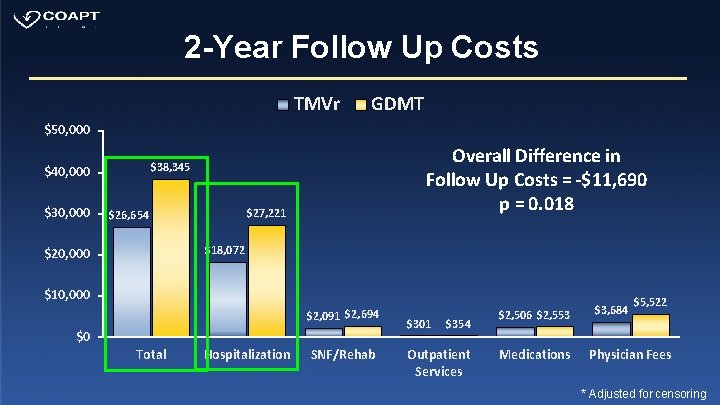
2 -Year Follow Up Costs TMVr GDMT $50, 000 $30, 000 Overall Difference in Follow Up Costs = -$11, 690 p = 0. 018 $38, 345 $40, 000 $27, 221 $26, 654 $18, 072 $20, 000 $10, 000 $2, 091 $2, 694 $0 Total Hospitalization SNF/Rehab $301 $354 Outpatient Services $2, 506 $2, 553 Medications $3, 684 $5, 522 Physician Fees * Adjusted for censoring
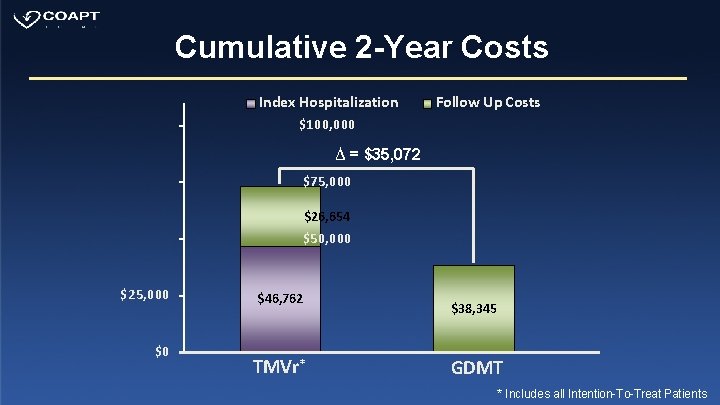
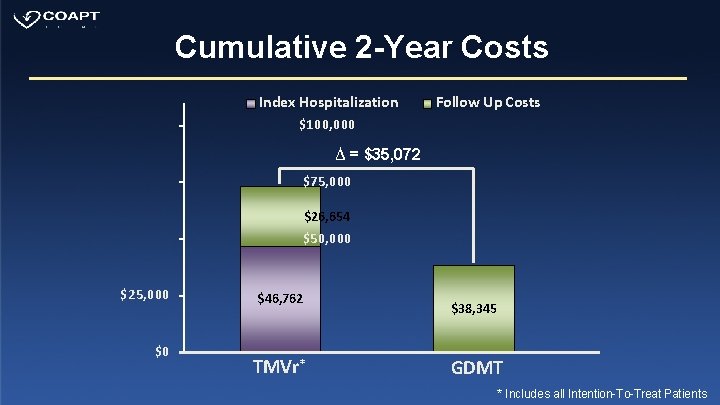
Cumulative 2 -Year Costs Index Hospitalization Follow Up Costs $100, 000 ∆ = $35, 072 $75, 000 $26, 654 $50, 000 $25, 000 $0 $46, 762 TMVr* $38, 345 GDMT * Includes all Intention-To-Treat Patients
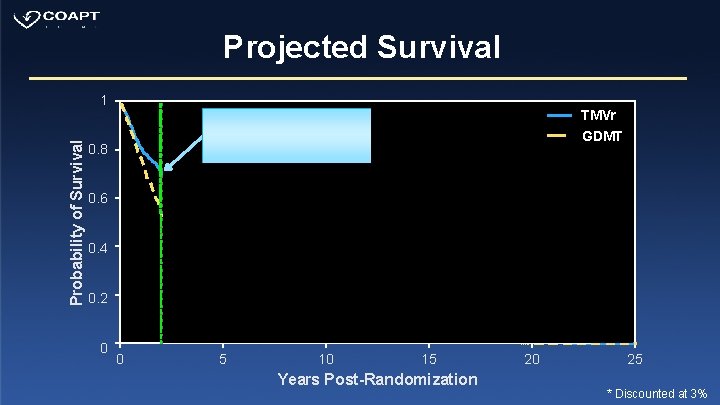
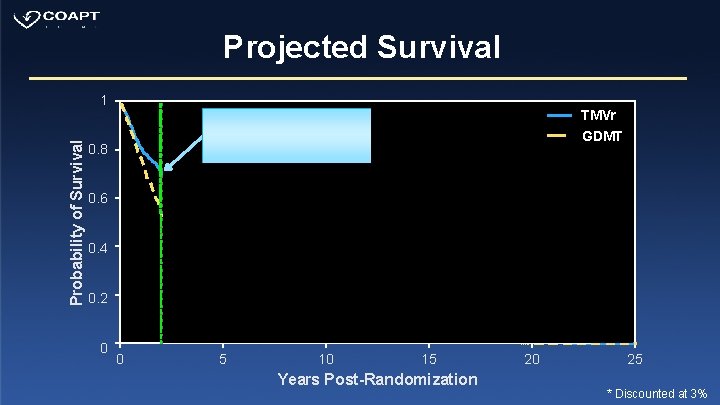
Projected Survival Probability of Survival 1 0. 8 0. 6 Projected Life-Expectancy* TMVr: 5. 05 yrs GDMT: 3. 92 yrs 0. 4 Δ Life Expectancy = 1. 13 yrs Δ QALE = 0. 82 QALYs 0. 2 0 TMVr GDMT In-Trial 0. 14 LYs 0. 13 QALYs 0 5 10 15 Years Post-Randomization 20 25 * Discounted at 3%
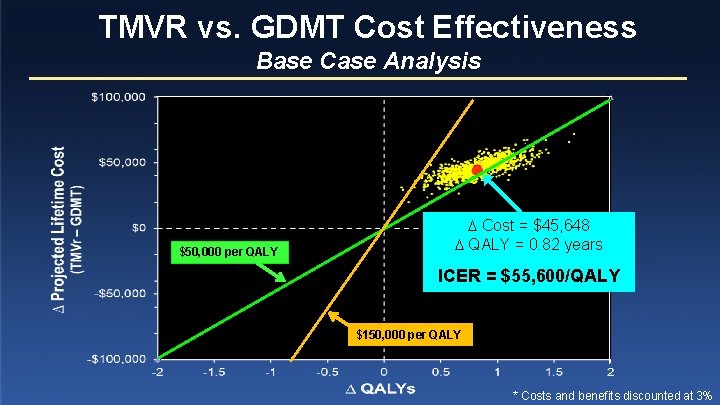
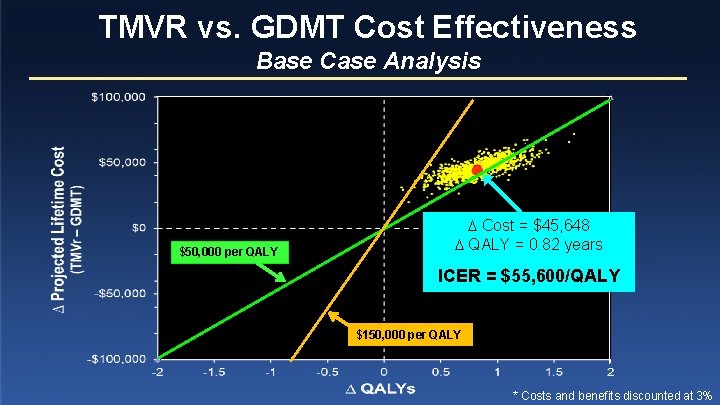
TMVR vs. GDMT Cost Effectiveness Base Case Analysis $50, 000 per QALY Cost = $45, 648 QALY = 0. 82 years ICER = $55, 600/QALY $150, 000 per QALY * Costs and benefits discounted at 3%
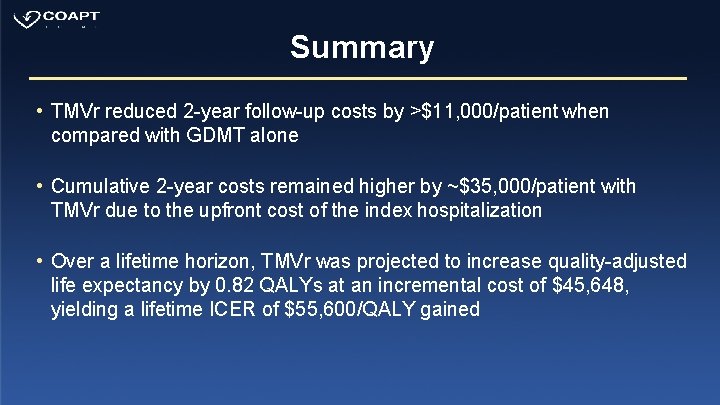
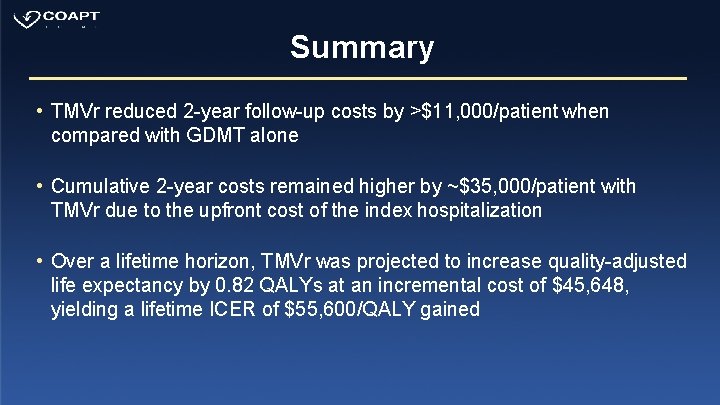
Summary • TMVr reduced 2 -year follow-up costs by >$11, 000/patient when compared with GDMT alone • Cumulative 2 -year costs remained higher by ~$35, 000/patient with TMVr due to the upfront cost of the index hospitalization • Over a lifetime horizon, TMVr was projected to increase quality-adjusted life expectancy by 0. 82 QALYs at an incremental cost of $45, 648, yielding a lifetime ICER of $55, 600/QALY gained
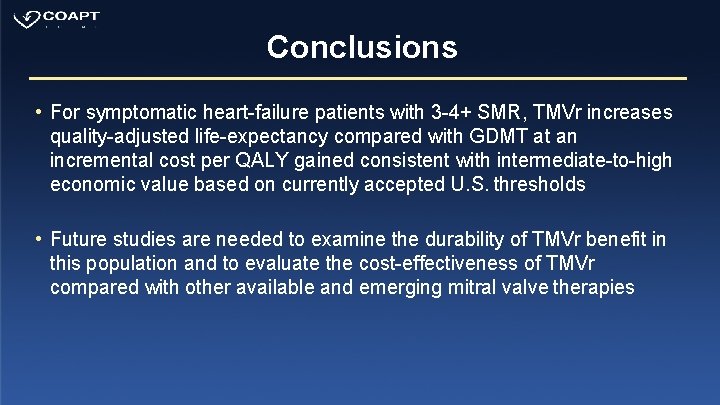
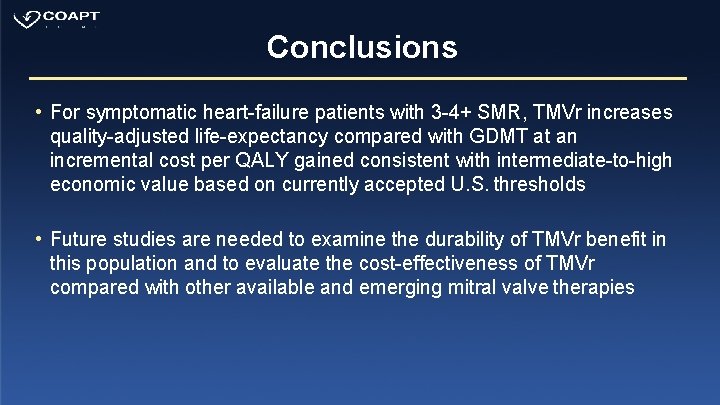
Conclusions • For symptomatic heart-failure patients with 3 -4+ SMR, TMVr increases quality-adjusted life-expectancy compared with GDMT at an incremental cost per QALY gained consistent with intermediate-to-high economic value based on currently accepted U. S. thresholds • Future studies are needed to examine the durability of TMVr benefit in this population and to evaluate the cost-effectiveness of TMVr compared with other available and emerging mitral valve therapies

Back-Up Slides
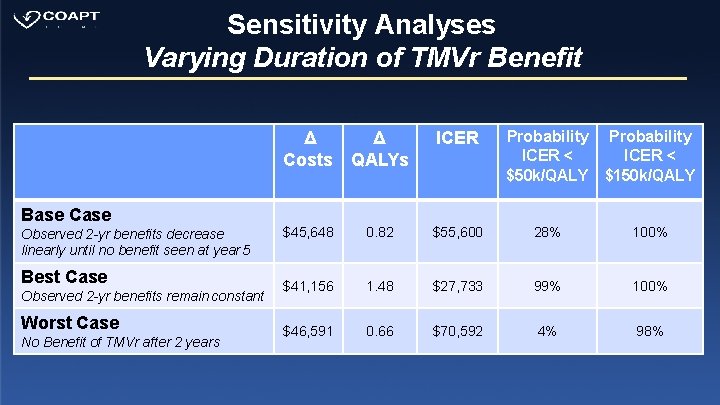
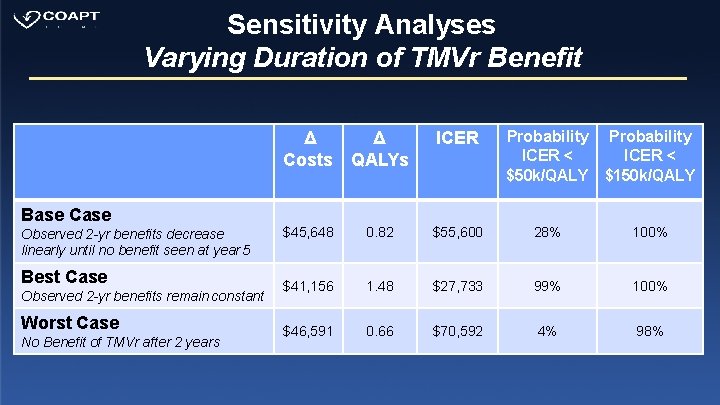
Sensitivity Analyses Varying Duration of TMVr Benefit Base Case Observed 2 -yr benefits decrease linearly until no benefit seen at year 5 Best Case Observed 2 -yr benefits remain constant Worst Case No Benefit of TMVr after 2 years Probability ICER < $50 k/QALY $150 k/QALY Δ Δ Costs QALYs ICER $45, 648 0. 82 $55, 600 28% 100% $41, 156 1. 48 $27, 733 99% 100% $46, 591 0. 66 $70, 592 4% 98%
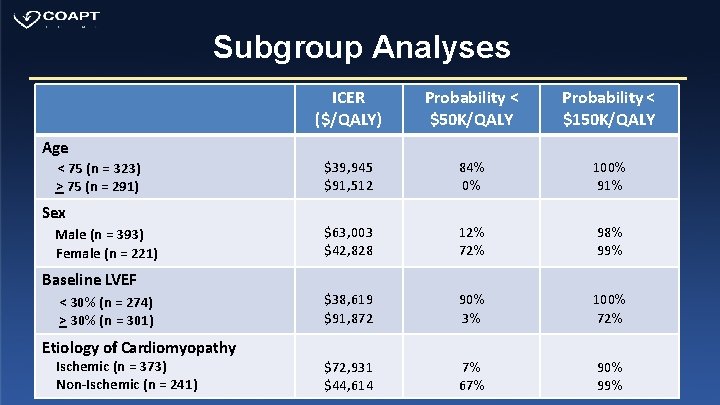
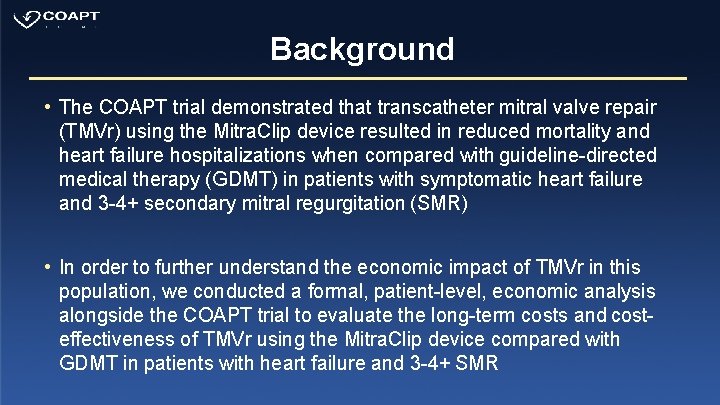
Subgroup Analyses ICER ($/QALY) Probability < $50 K/QALY Probability < $150 K/QALY $39, 945 $91, 512 84% 0% 100% 91% $63, 003 $42, 828 12% 72% 98% 99% $38, 619 $91, 872 90% 3% 100% 72% $72, 931 $44, 614 7% 67% 90% 99% Age < 75 (n = 323) > 75 (n = 291) Sex Male (n = 393) Female (n = 221) Baseline LVEF < 30% (n = 274) > 30% (n = 301) Etiology of Cardiomyopathy Ischemic (n = 373) Non-Ischemic (n = 241)
 Ef slope in echo
Ef slope in echo Pressure half time formula
Pressure half time formula Tendyne
Tendyne Apical pulse and mitral valve
Apical pulse and mitral valve Dna repair pathways
Dna repair pathways Base excision repair vs mismatch repair
Base excision repair vs mismatch repair Servo valve symbol
Servo valve symbol Location of heart sounds
Location of heart sounds Pistol shot bulgusu
Pistol shot bulgusu Mitral facies
Mitral facies Mediastino
Mediastino Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Tendinous cords
Tendinous cords Atheromatous thoracic aorta
Atheromatous thoracic aorta Valvula mitral
Valvula mitral Iam
Iam Define mitral stenosis
Define mitral stenosis Mushuk xirillashi simptomi
Mushuk xirillashi simptomi