Congenital SucraseIsomaltase Deficiency CSID among Alaska Native People






- Slides: 35


Congenital Sucrase-Isomaltase Deficiency (CSID) among Alaska Native People Presented by: Claire Siekaniec, MS, RD, LD - CSID Outreach and Education Coordinator Community Health Services, ANTHC
Disclosure ANTHC CSID Program and Coordinator position received past support through a grant from QOL Medical, LLC.
Objectives • Increase awareness of CSID among Alaska Native people • Identify symptoms of CSID • Understand management of CSID symptoms • Discuss ANTHC’s CSID Outreach and Education Program
Outline • Background – Symptoms – Genetics – Diagnosis – Prevalence • Management – Nutrition therapy – Medication therapy • ANTHC CSID Program
Congenital Sucrase-Isomaltase Deficiency (CSID) • Genetic disorder - affects ability to digest certain sugars • Polysaccharides – starch, glycogen • Disaccharides – sucrose, maltose, lactose • Monosaccharides – glucose, fructose, galactose • Digestive enzymes break down poly and disaccharides to monosaccharides
Digestive Enzyme Activity • Sucrase-isomaltase (SI) is a disaccharidase on the brush border membrane of the small intestines – Sucrase • Breaks down sucrose and maltose • Sucrose = fructose + glucose – Isomaltase • Breaks down isomaltose and maltose • Maltose = glucose + glucose • In CSID, activity of the SI enzyme is absent or reduced
CSID Symptoms When disaccharides are not broken down: • Bacteria feed off the sugar in the colon causing fermentation • Undigested sugars retain water causing osmotic diarrhea
CSID Symptoms Common symptoms: • Watery diarrhea • Bloating/gas • Abdominal pain Severe symptoms may lead to malnutrition or failure to thrive
Possible Indicators of CSID • History of watery diarrhea that can be traced to introduction of table foods • Family history of “allergy” or intolerance to sugar • Symptoms appear when eating more store bought foods and less Alaska Native traditional foods
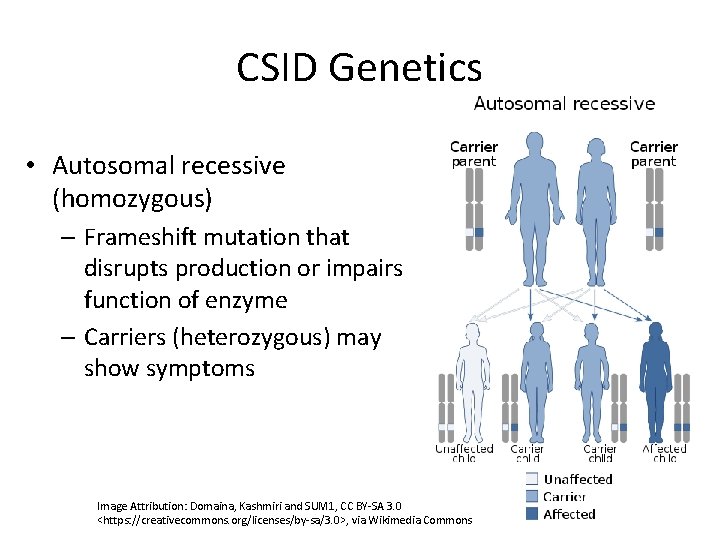
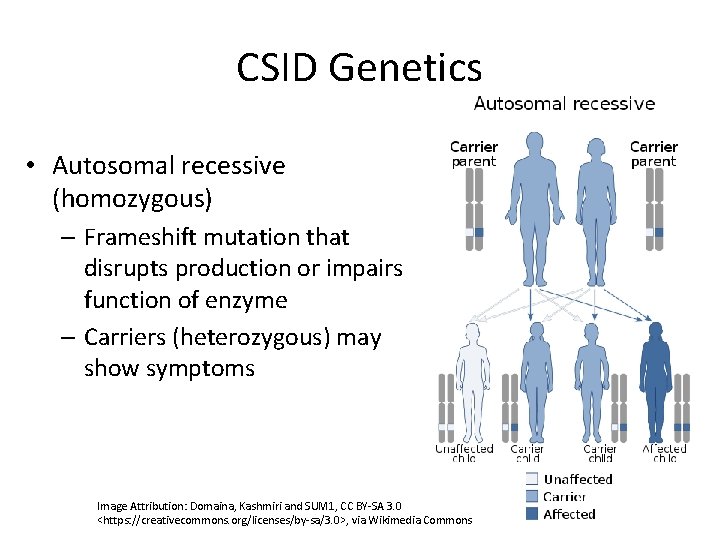
CSID Genetics • Autosomal recessive (homozygous) – Frameshift mutation that disrupts production or impairs function of enzyme – Carriers (heterozygous) may show symptoms Image Attribution: Domaina, Kashmiri and SUM 1, CC BY-SA 3. 0 <https: //creativecommons. org/licenses/by-sa/3. 0>, via Wikimedia Commons
CSID Genetics Title: Congenital sucrase-isomaltase deficiency: identification of a common Inuit founder mutation Authors: Marcadier JL, Boland M, Scott R, et al. Published in Canadian Medical Association Journal in 2015 Results and Interpretation: identification of a homozygous, frameshift mutation, SI c. 273_274 del. AG (p. Gly 92 Leufs*8), responsible for high prevalence of CSID among Inuit people.
CSID Testing • Genetic testing through Fulgent Genetics • Blood sample + test requisition form + testing consent • Full sequencing of SI gene • Cost: $895 • Known mutation • Cost: $200 • Other testing methods – Intestinal biopsy: disaccharidase assay – Breath tests
Breath Test • Carbon-13 sucrose breath test – 8 hours fasting – 20 g sucrose – Series of 4 small tubes the patient blows into over a period of 90 minutes • A healthcare professional can order the test by calling 1 -800 -705 -1962
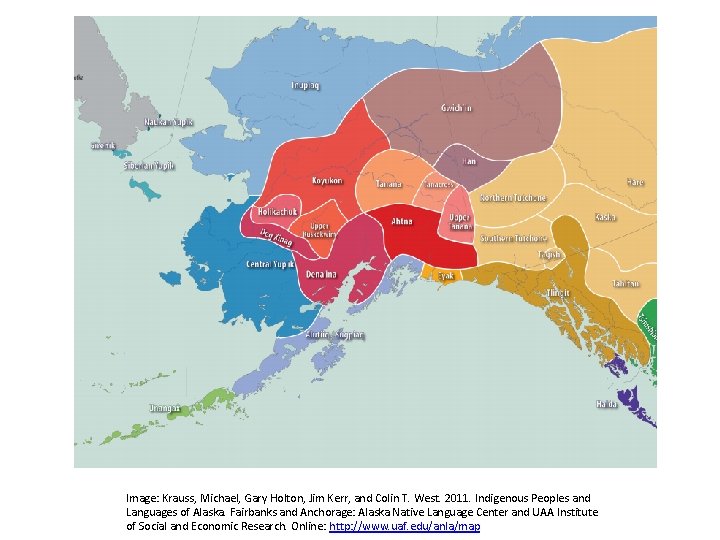
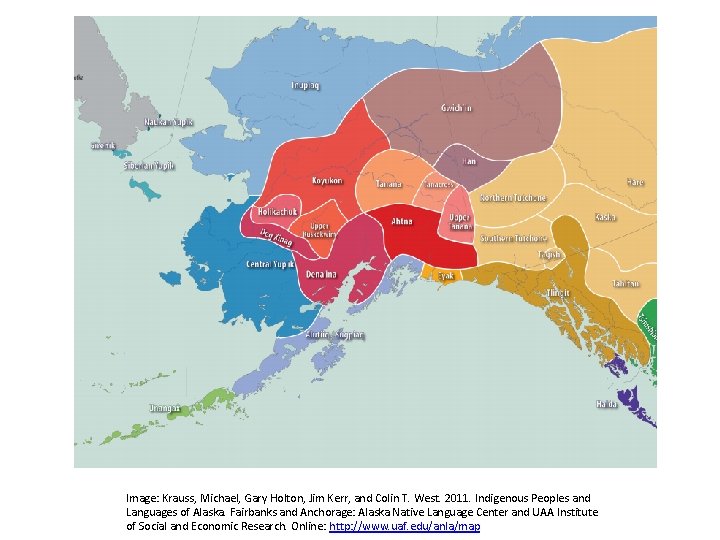
CSID Prevalence • 0. 2% of North Americans of European ancestry • 5 -10% of Greenland/Canadian Inuit people • Unknown at this time in Alaska Native people Image: Krauss, Michael, Gary Holton, Jim Kerr, and Colin T. West. 2011. Indigenous Peoples and Languages of Alaska. Fairbanks and Anchorage: Alaska Native Language Center and UAA Institute of Social and Economic Research. Online: http: //www. uaf. edu/anla/map
Management of CSID
CSID Management Goals: • Minimize symptoms • Improve quality of life • Promote physical growth for infants and children
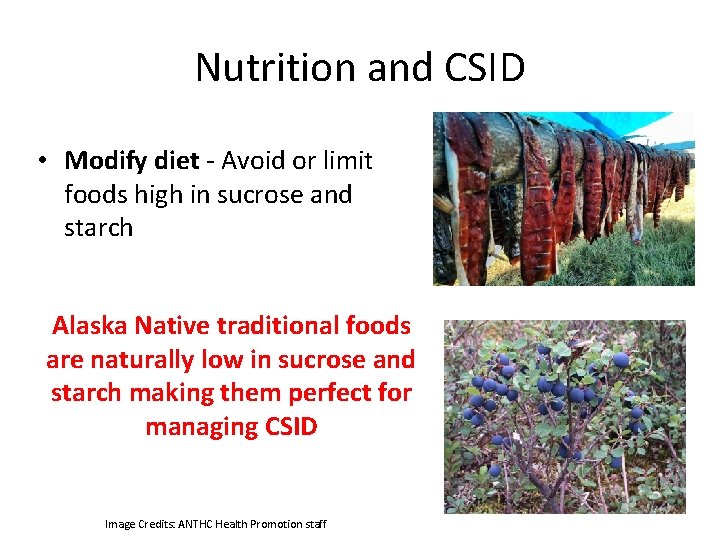
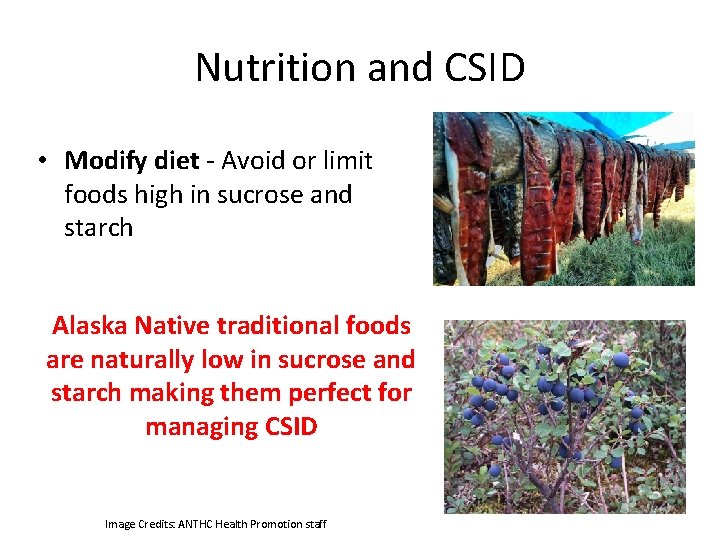
Nutrition and CSID • Modify diet - Avoid or limit foods high in sucrose and starch Alaska Native traditional foods are naturally low in sucrose and starch making them perfect for managing CSID Image Credits: ANTHC Health Promotion staff
Changes in Eating Patterns • May be increase in sedentary lifestyle • May be decrease or loss of traditional knowledge – Move out of village – Busy lives (working, other priorities) – Increase in store bought foods with cash economy – Gas is expensive for travel/hunting – Climate change
Nutrition and CSID • Store bought foods are often high in sucrose and/or starch • Can be difficult to manage CSID symptoms with higher intake of foods that contain sucrose and starch – Leads to poor nutrition, failure to thrive, and/or poor quality of life
Nutrition and CSID • Fruits and Vegetables – Many fruits and vegetables contain sucrose – use food guides to help determine tolerances • Dairy – Most plain/unsweetened dairy products are tolerated • Fats and Oils – Most are tolerated
Nutrition and CSID • Protein – Most animal protein sources are tolerated – Starchy plant based proteins such as beans/lentils/nuts may not be tolerated • Starches – Individual tolerance varies – Processed foods often contain sucrose and starch o Read ingredient labels
Infant Formula & Supplements • • Infants Breast milk and standard, lactose-based formulas are usually tolerated Most other formulas contain sucrose and/or starch Carbohydrate free (RCF ®) formula available – not nutritionally complete Children Nutritional supplements (Pediasure ®, Ensure ®, etc. ) all contain sucrose and/or starch as carbohydrate source
CSID Management and Tolerance • Will not “outgrow” disorder but tolerances may change as the GI tract lengthens • Food tolerances are different for every person – Determine individual tolerances • Introduce 1 new food at a time and track symptoms • Work with a Registered Dietitian for nutrition education and ongoing support
Prescription Medication • Sacrosidase (Brand name: Sucraid®) – Enzyme replacement therapy for sucrase – Dosage weight dependent • Taken with every meal/snack that contains sucrose – Is not covered by Medicaid • Covered by most private insurance – Requires refrigeration – Does not help with starch digestion
T-SHIP Tribally Sponsored Health Insurance Program – Aids in coverage of sacrosidase – ANTHC TSHIP assists with enrolling patients – Visit anthc. org/tship for more information
ANTHC CSID Program Goals of the Program: • Increase awareness of CSID • Resource center for patients, families, and medical staff • Maintain culturally relevant educational materials – CSID education materials for clinics, waiting rooms, health fairs – Find materials and other resources on anthc. org/csid



Resources and References • ANTHC CSID webpage: anthc. org/csid • Pocket Guide to Alaska Native Pediatric Diagnoses http: //anmc. org/files/Pocket-Guide-to-Alaska-Native-Pediatric. Diagnoses_web. pdf • CSID Cares: http: //csidcares. org/ • Sucraid®: http: //sucraid. com • Fulgent Genetics https: //www. fulgentgenetics. com/congenital-sucrase-isomaltase-deficiency • CSID ADN article http: //www. adn. com/article/20150119/sugar-intolerance-northernpopulations-linked-specific-gene-researchers-say
Additional References 1. Treem, W. (2012). Clinical Aspects and Treatment of Congenital Sucrase-Isomaltase Deficiency. Journal of Pediatric Gastroenterology and Nutrition, 55, pp. S 7 -S 13. 2. Gericke, B. , Amiri, M. and Naim, H. (2016). The multiple roles of sucrase-isomaltase in the Intestinal physiology. Molecular and Cellular Pediatrics, 3(1). 3. Marcadier, J. , Boland, M. , Scott, C. , Issa, K. , Wu, Z. , Mc. Intyre, A. , Hegele, R. , Geraghty, M. and Lines, M. (2014). Congenital sucrase–isomaltase deficiency: identification of a common Inuit founder mutation. Canadian Medical Association Journal, 187(2), pp. 102107. 4. Husein, D. , Wanes, D. , Marten, L. , Zimmer, K-P. , and Naim, H. (2019). Heterozygotes Are a Potential New Entity among Homozygotes and Compound Heterozygotes in Congenital Sucrase-Isomaltase Deficiency. Nutrients, 11 (10), 2290; https: //doi. org/10. 3390/nu 11102290. 5. Genetics. edu. au. (2020). [online] Available at: http: //www. genetics. edu. au/publications -and-resources/facts-sheets/fact-sheet-7 -autosomal-recessive-inheritance [Accessed Dec. 2020]. 6. Rarediseases. info. nih. gov. (2018). Congenital sucrase-isomaltase deficiency | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program. [online] Available at: https: //rarediseases. info. nih. gov/diseases/7710/congenital-sucrase-isomaltasedeficiency [Accessed 4 Sep. 2018].
Thank You Image by Samantha Maloney in Kotzebue

 Congenital
Congenital Thank you in alaska native languages
Thank you in alaska native languages Alaska native health board
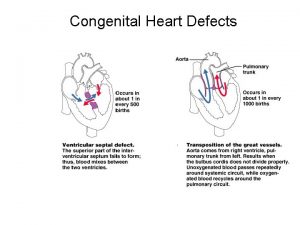
Alaska native health board Congenital heart defect
Congenital heart defect Hutchinson's triad
Hutchinson's triad Micrognathia definition
Micrognathia definition Congenital toxoplasmosis
Congenital toxoplasmosis Congenital rubella syndrome
Congenital rubella syndrome Congenital glaucoma triad
Congenital glaucoma triad Congenital rubella syndrome triad
Congenital rubella syndrome triad Congenital glaucoma
Congenital glaucoma Potencity
Potencity Murmur in asd
Murmur in asd Congenital diaphragmatic hernia
Congenital diaphragmatic hernia Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Picior varus equin
Picior varus equin Dr dawn lim
Dr dawn lim Fnac test for lymph node
Fnac test for lymph node Spina bifida
Spina bifida Choledocolithaisis
Choledocolithaisis Congenital malformations
Congenital malformations Vulvodynia
Vulvodynia Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Ortolani and barlow
Ortolani and barlow Congenital
Congenital Congenital heart
Congenital heart Classification of congenital heart disease
Classification of congenital heart disease Stumped cloudy cornea
Stumped cloudy cornea Congenital toxoplasmosis
Congenital toxoplasmosis Congenital rubella syndrome triad
Congenital rubella syndrome triad Disease penis
Disease penis Greater and lesser pelvis
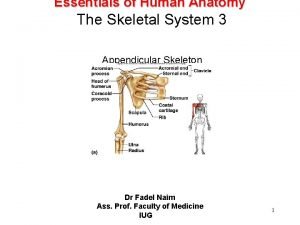
Greater and lesser pelvis Canadian congenital heart alliance
Canadian congenital heart alliance Congenital voice disorders
Congenital voice disorders Hymen
Hymen Potter face oligohydramnios
Potter face oligohydramnios