Clinical Evaluation of Neuromyelitis Optica Spectrum Disorder Module
![Module 1: References Wingerchuk DM et al with IPND [2015] International consensus diagnostic criteria Module 1: References Wingerchuk DM et al with IPND [2015] International consensus diagnostic criteria](https://slidetodoc.com/presentation_image/3106a3c4a68440e53690c69cecc0083e/image-22.jpg)
- Slides: 25
Clinical Evaluation of Neuromyelitis Optica Spectrum Disorder Module 1: Basic Diagnosis © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org
• About the Foundation The Guthy-Jackson Charitable Foundation is a non-profit 501(c)(3) organization that promotes research to understand the causes and advance effective solutions to Neuromyelitis Optica (NMO) / Neuromyelitis Optica Spectrum Disorder (NMO/SD). The Foundation adheres to a transparent and equitable model that does not favor or endorse any particular company, institution or drug candidate. • Clinical Position Statement GJCF supports efforts directed at the prevention, diagnosis, treatment and cure of Neuromyelitis optica (NMO) and NMO spectrum disorders (NMO/SD). It facilitates scientific and clinical advances directed toward these goals, including educational tools developed by academic and clinical experts. The Foundation neither performs clinical functions nor does it offer advice about the evaluation, care or treatment of patients. The GJCF does not participate in the performance, evaluation, analysis or management of clinical trials or in the interpretation of trial outcomes. • Equal Opportunity Advocate The Foundation functions in a transparent, neutral, and equitable manner in all of its interactions with academic experts, clinical trial sponsors, investigators, governmental and private agency or group representatives and other NMO/SD stakeholders. For more information, please visit the Foundation website: www. guthyjacksonfoundation. org © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 2
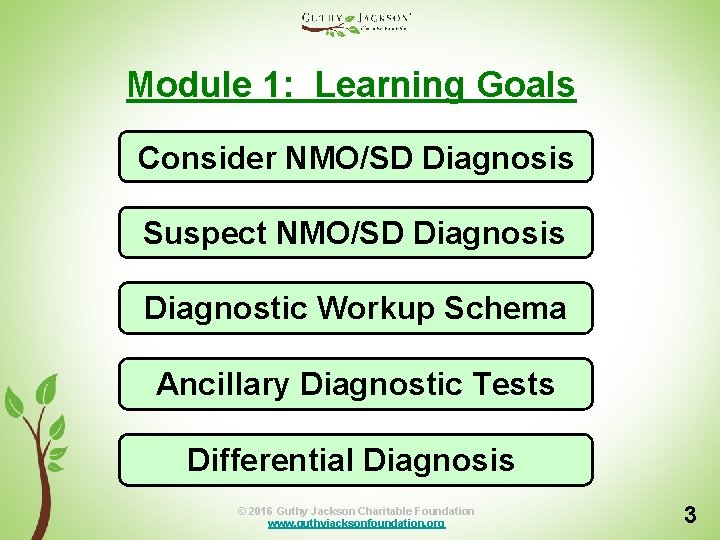
Module 1: Learning Goals Consider NMO/SD Diagnosis Suspect NMO/SD Diagnosis Diagnostic Workup Schema Ancillary Diagnostic Tests Differential Diagnosis © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 3
When to Consider NMO/SD: 1 • Any patient presenting with: § § § Optic neuritis Myelitis Unexplained intractable vomiting Unexplained intractable hiccups Other NMO-typical CNS lesion(s): o Inflammatory profile o Hypothalamic localization o Tumefactive brain lesion © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 4
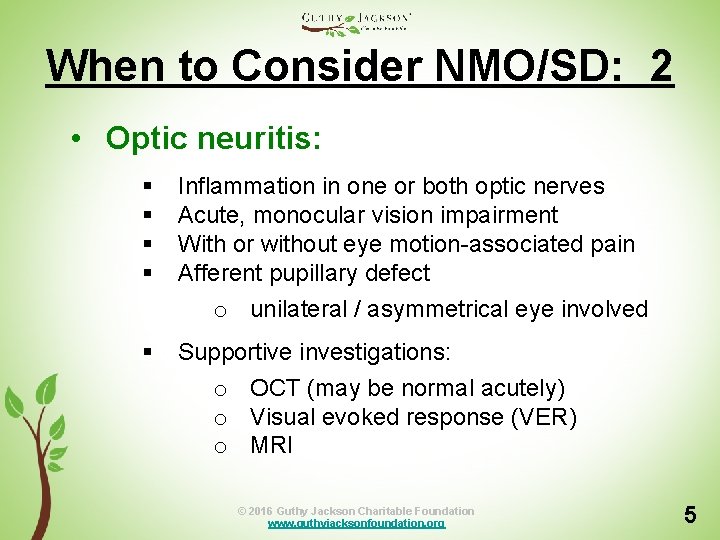
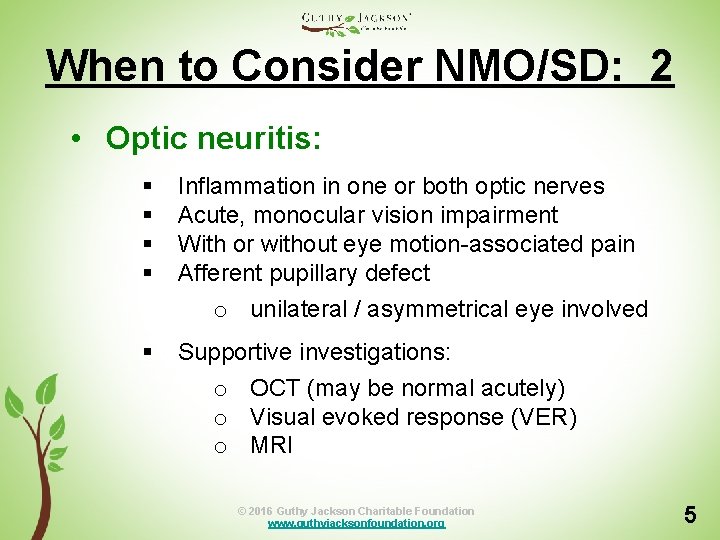
When to Consider NMO/SD: 2 • Optic neuritis: § § Inflammation in one or both optic nerves Acute, monocular vision impairment With or without eye motion-associated pain Afferent pupillary defect o unilateral / asymmetrical eye involved § Supportive investigations: o OCT (may be normal acutely) o Visual evoked response (VER) o MRI © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 5
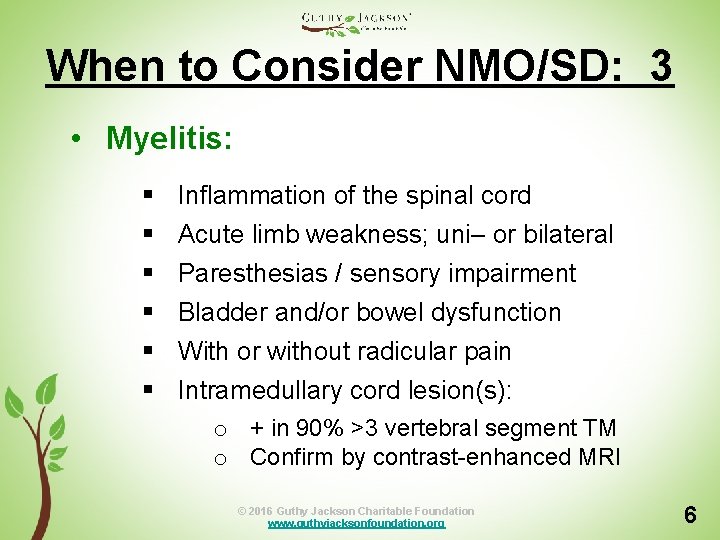
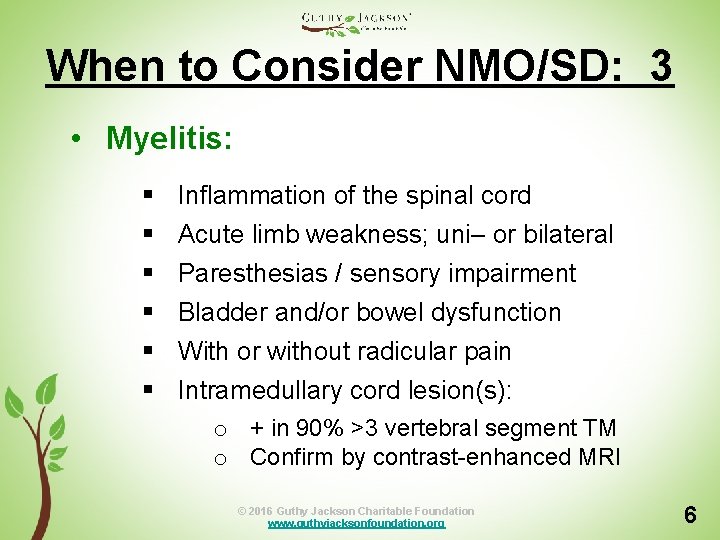
When to Consider NMO/SD: 3 • Myelitis: § § § Inflammation of the spinal cord Acute limb weakness; uni– or bilateral Paresthesias / sensory impairment Bladder and/or bowel dysfunction With or without radicular pain Intramedullary cord lesion(s): o + in 90% >3 vertebral segment TM o Confirm by contrast-enhanced MRI © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 6
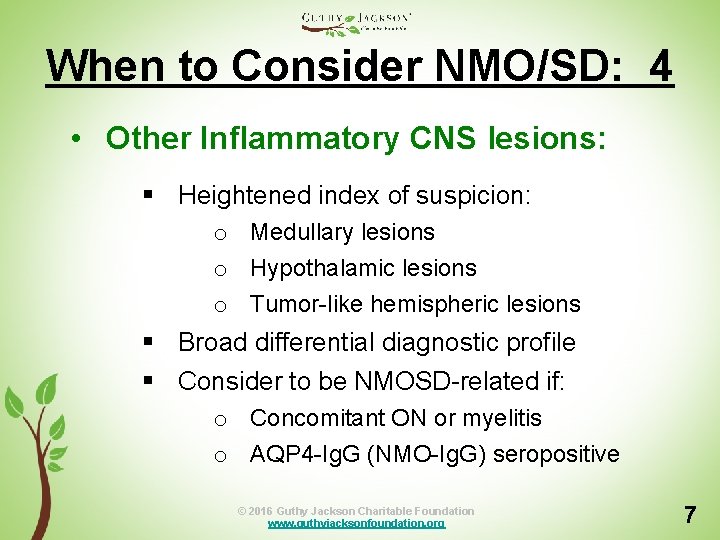
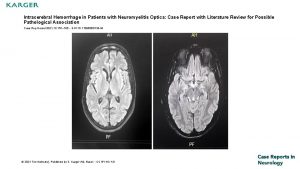
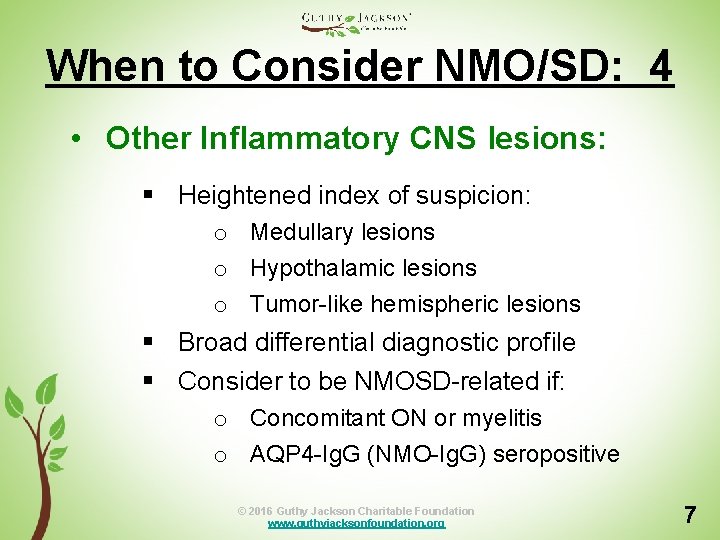
When to Consider NMO/SD: 4 • Other Inflammatory CNS lesions: § Heightened index of suspicion: o Medullary lesions o Hypothalamic lesions o Tumor-like hemispheric lesions § Broad differential diagnostic profile § Consider to be NMOSD-related if: o Concomitant ON or myelitis o AQP 4 -Ig. G (NMO-Ig. G) seropositive © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 7
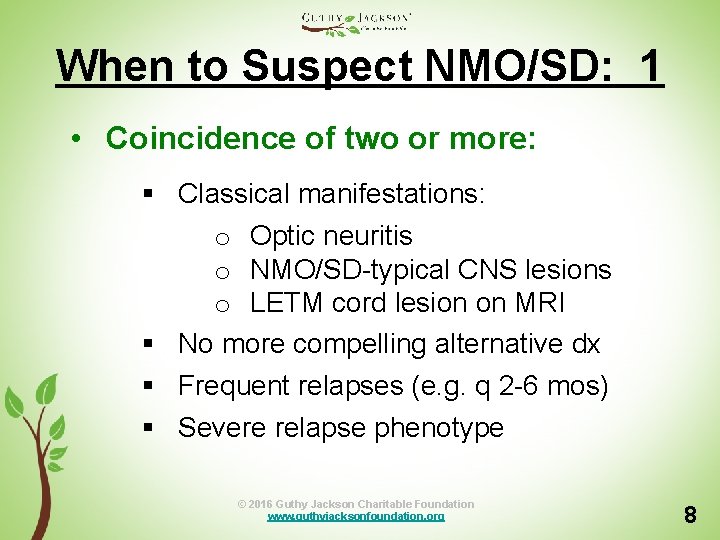
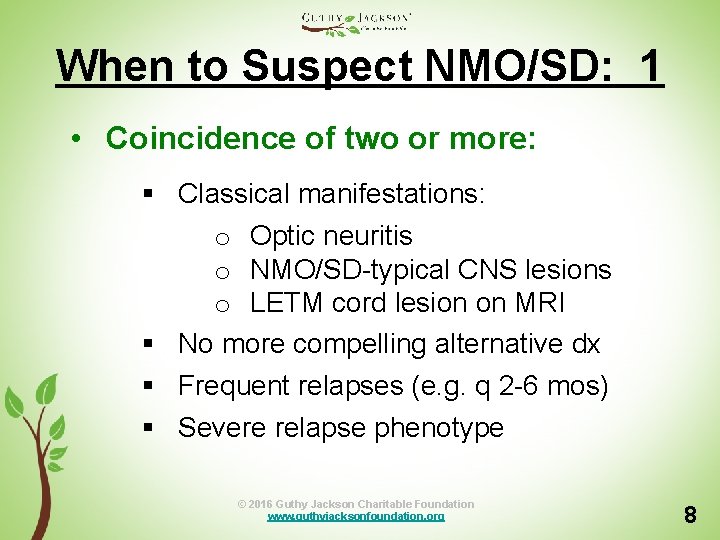
When to Suspect NMO/SD: 1 • Coincidence of two or more: § Classical manifestations: o Optic neuritis o NMO/SD-typical CNS lesions o LETM cord lesion on MRI § No more compelling alternative dx § Frequent relapses (e. g. q 2 -6 mos) § Severe relapse phenotype © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 8
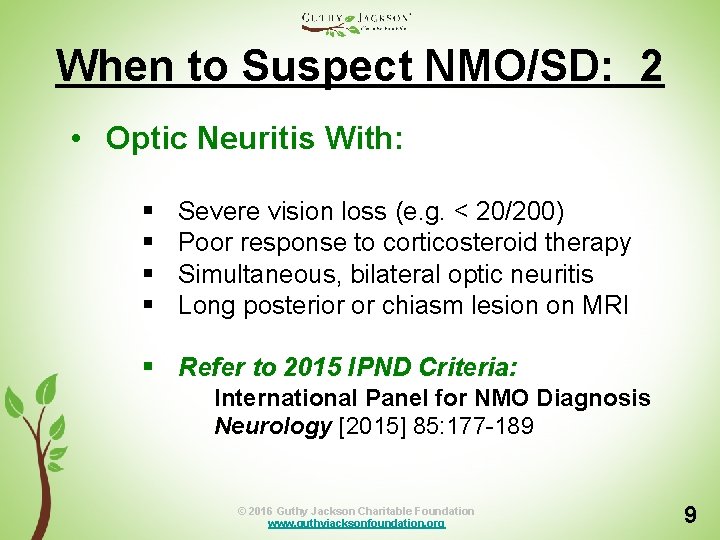
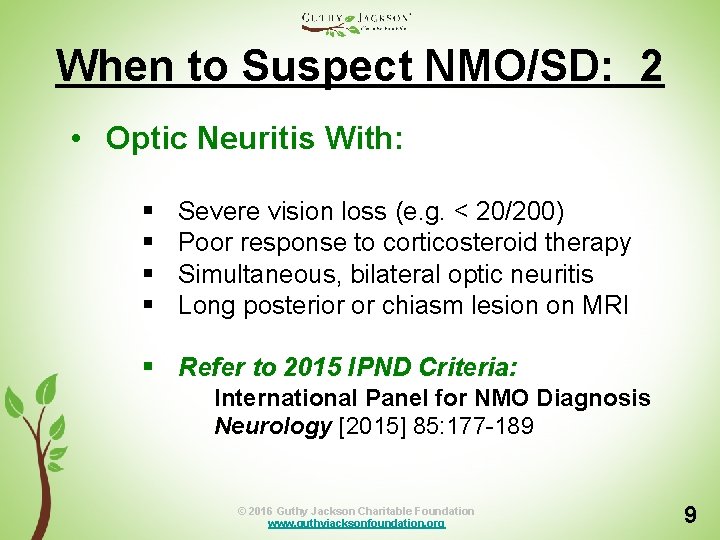
When to Suspect NMO/SD: 2 • Optic Neuritis With: § § Severe vision loss (e. g. < 20/200) Poor response to corticosteroid therapy Simultaneous, bilateral optic neuritis Long posterior or chiasm lesion on MRI § Refer to 2015 IPND Criteria: International Panel for NMO Diagnosis Neurology [2015] 85: 177 -189 © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 9
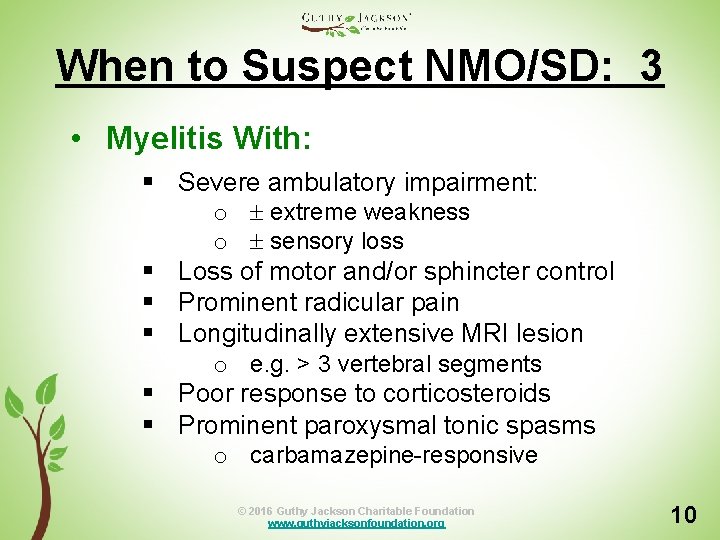
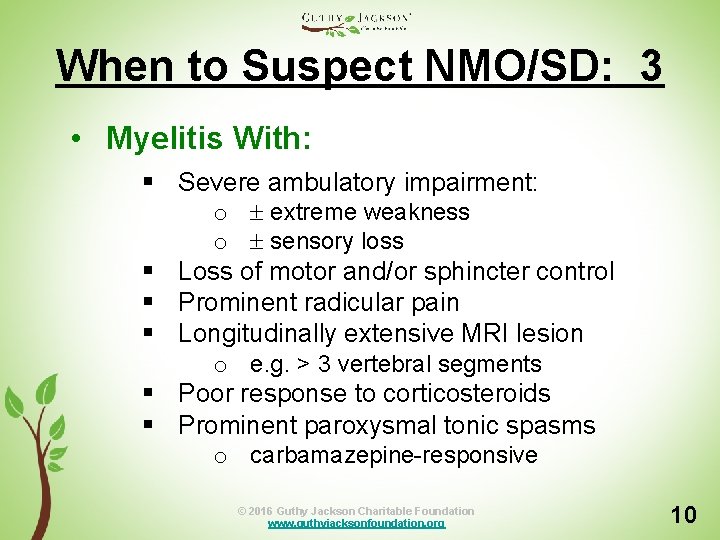
When to Suspect NMO/SD: 3 • Myelitis With: § Severe ambulatory impairment: o extreme weakness o sensory loss § Loss of motor and/or sphincter control § Prominent radicular pain § Longitudinally extensive MRI lesion o e. g. > 3 vertebral segments § Poor response to corticosteroids § Prominent paroxysmal tonic spasms o carbamazepine-responsive © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 10
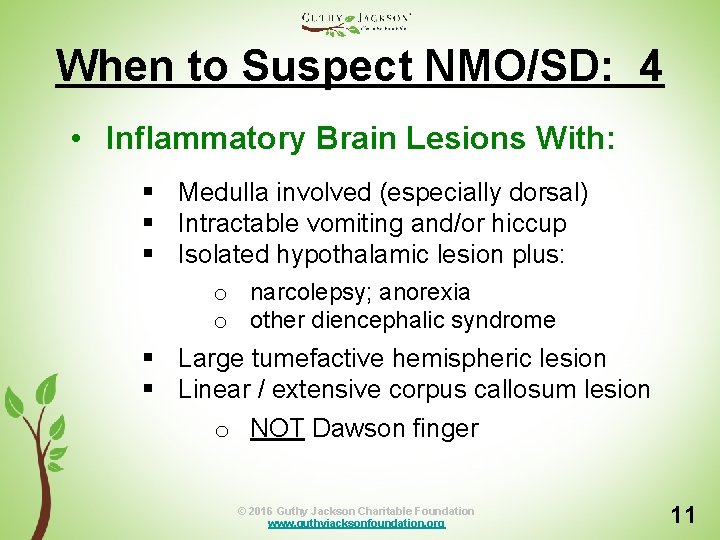
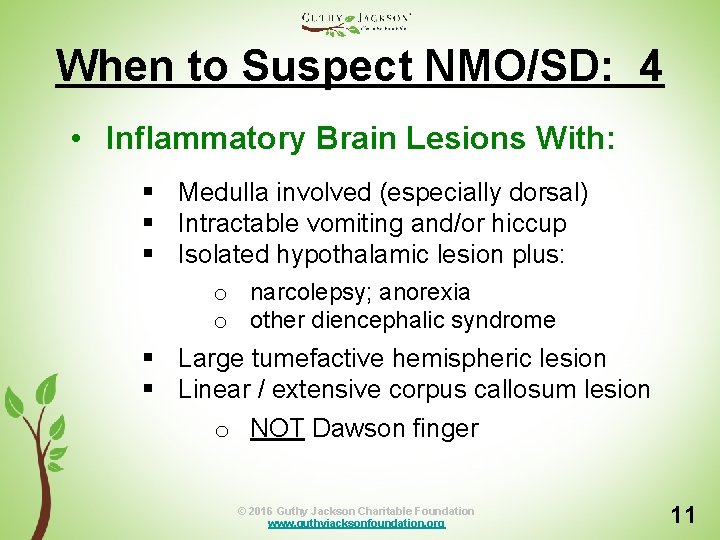
When to Suspect NMO/SD: 4 • Inflammatory Brain Lesions With: § Medulla involved (especially dorsal) § Intractable vomiting and/or hiccup § Isolated hypothalamic lesion plus: o narcolepsy; anorexia o other diencephalic syndrome § Large tumefactive hemispheric lesion § Linear / extensive corpus callosum lesion o NOT Dawson finger © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 11
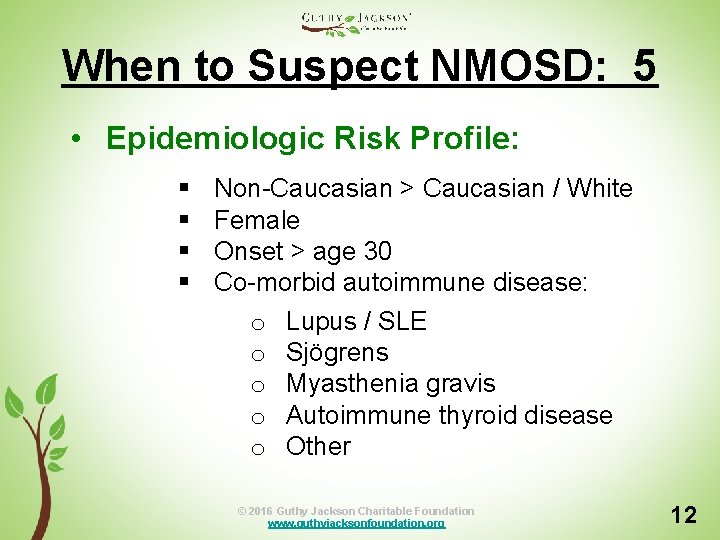
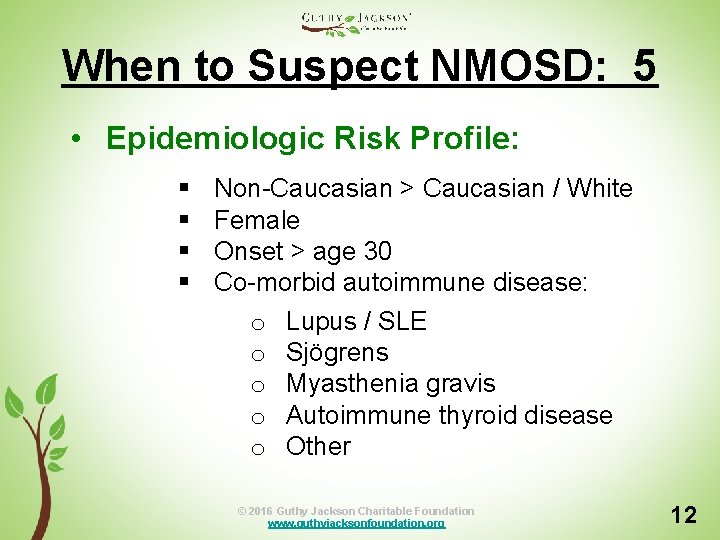
When to Suspect NMOSD: 5 • Epidemiologic Risk Profile: § § Non-Caucasian > Caucasian / White Female Onset > age 30 Co-morbid autoimmune disease: o Lupus / SLE o Sjögrens o Myasthenia gravis o Autoimmune thyroid disease o Other © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 12
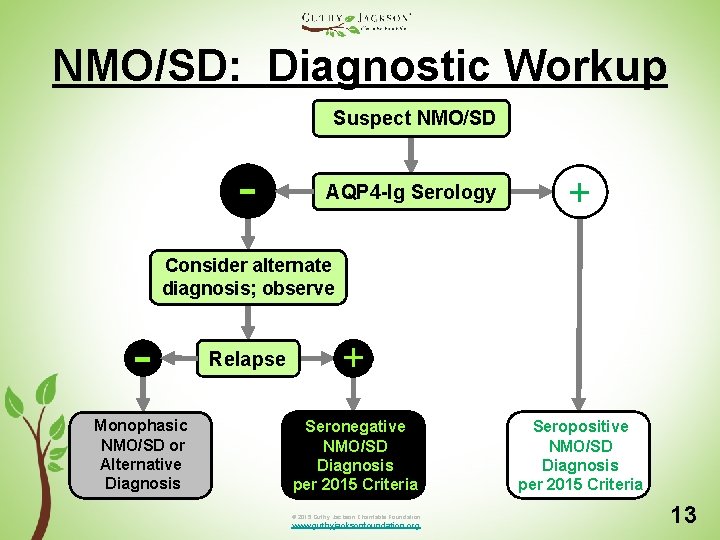
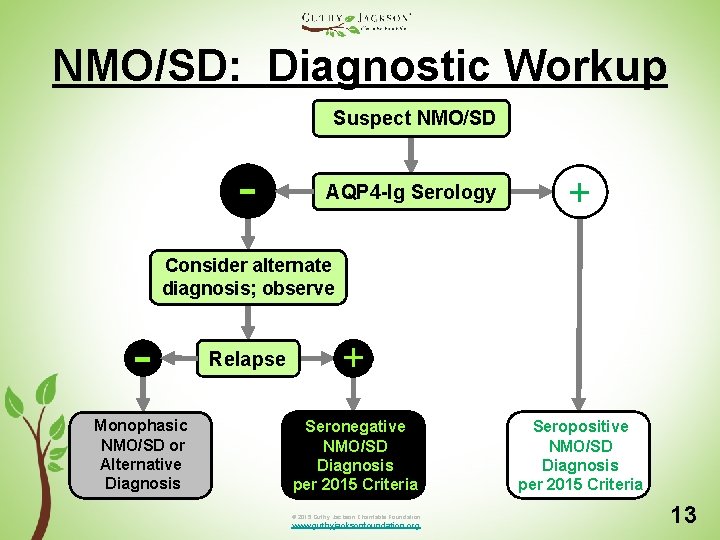
NMO/SD: Diagnostic Workup Suspect NMO/SD - AQP 4 -Ig Serology + Consider alternate diagnosis; observe Monophasic NMO/SD or Alternative Diagnosis Relapse + Seronegative NMO/SD Diagnosis per 2015 Criteria © 2015 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org Seropositive NMO/SD Diagnosis per 2015 Criteria 13
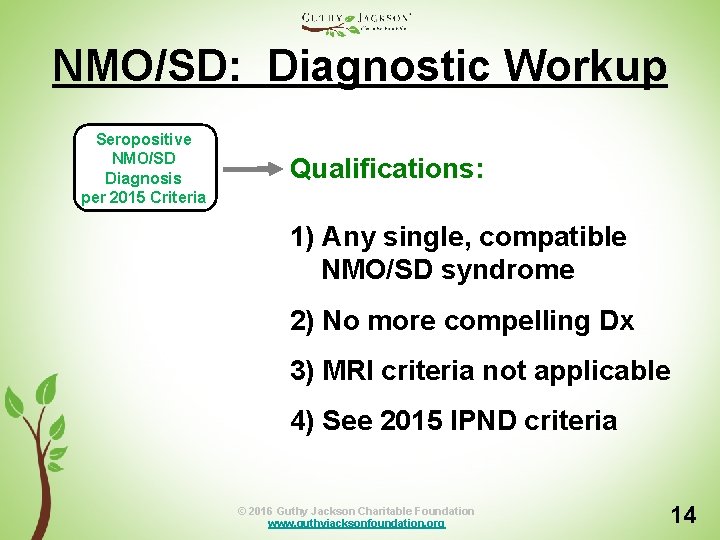
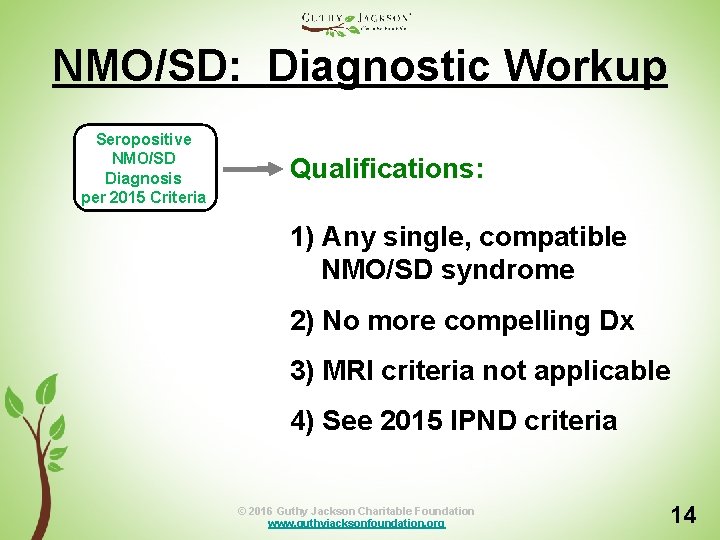
NMO/SD: Diagnostic Workup Seropositive NMO/SD Diagnosis per 2015 Criteria Qualifications: 1) Any single, compatible NMO/SD syndrome 2) No more compelling Dx 3) MRI criteria not applicable 4) See 2015 IPND criteria © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 14
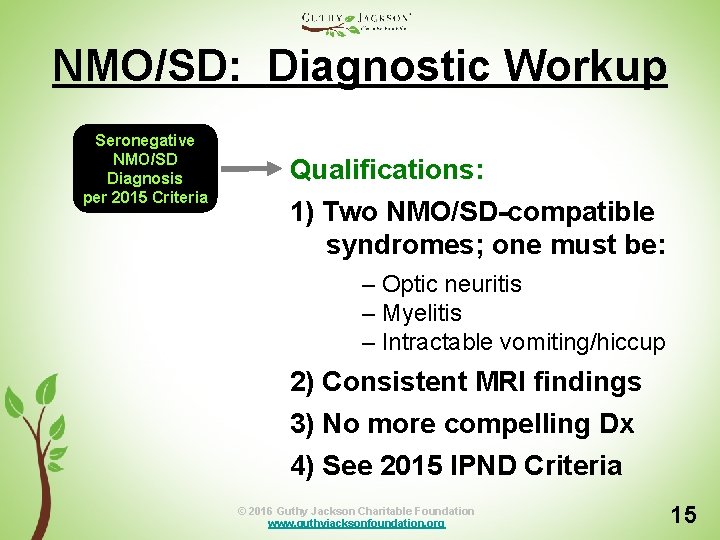
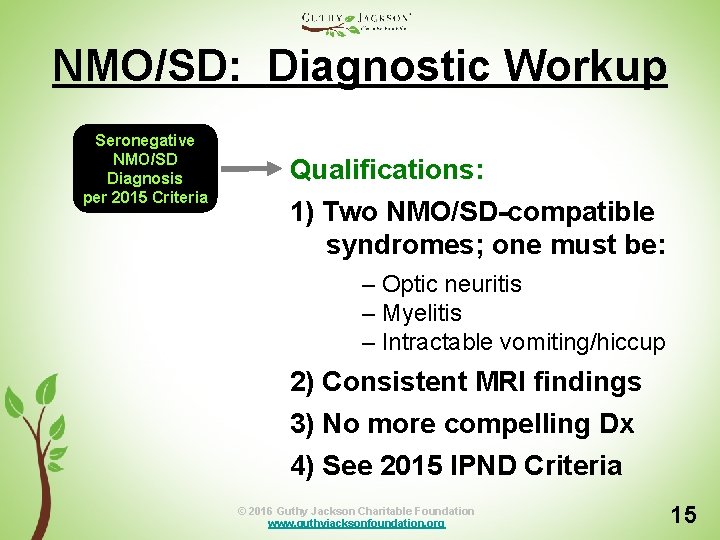
NMO/SD: Diagnostic Workup Seronegative NMO/SD Diagnosis per 2015 Criteria Qualifications: 1) Two NMO/SD-compatible syndromes; one must be: – Optic neuritis – Myelitis – Intractable vomiting/hiccup 2) Consistent MRI findings 3) No more compelling Dx 4) See 2015 IPND Criteria © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 15
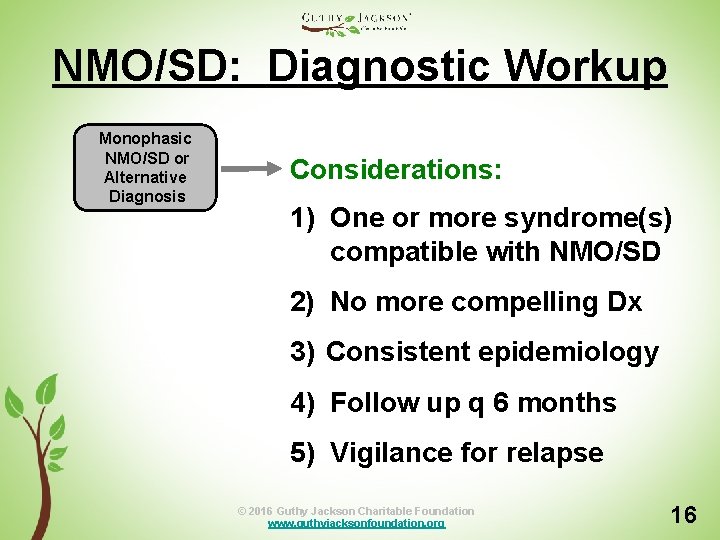
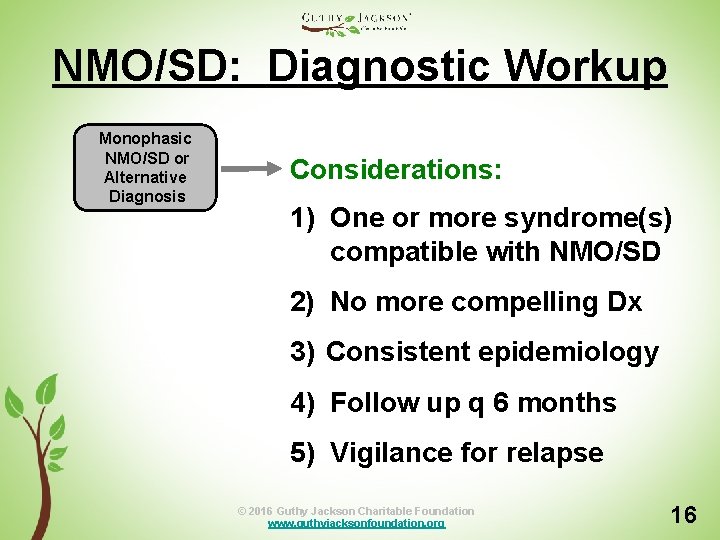
NMO/SD: Diagnostic Workup Monophasic NMO/SD or Alternative Diagnosis Considerations: 1) One or more syndrome(s) compatible with NMO/SD 2) No more compelling Dx 3) Consistent epidemiology 4) Follow up q 6 months 5) Vigilance for relapse © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 16
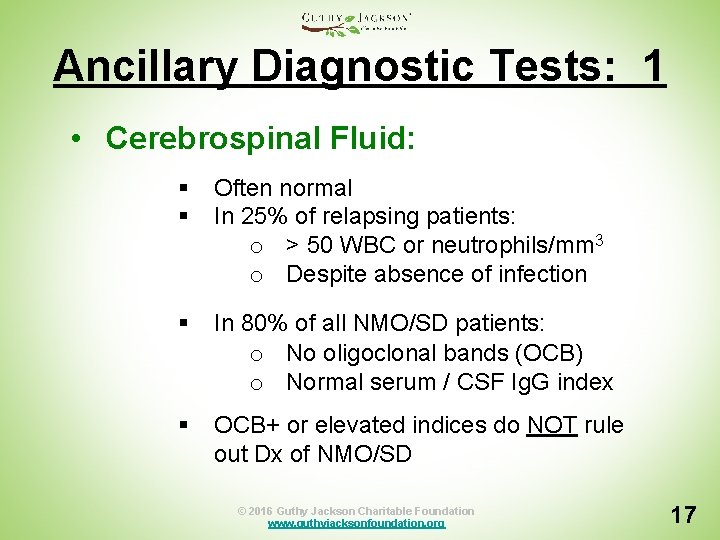
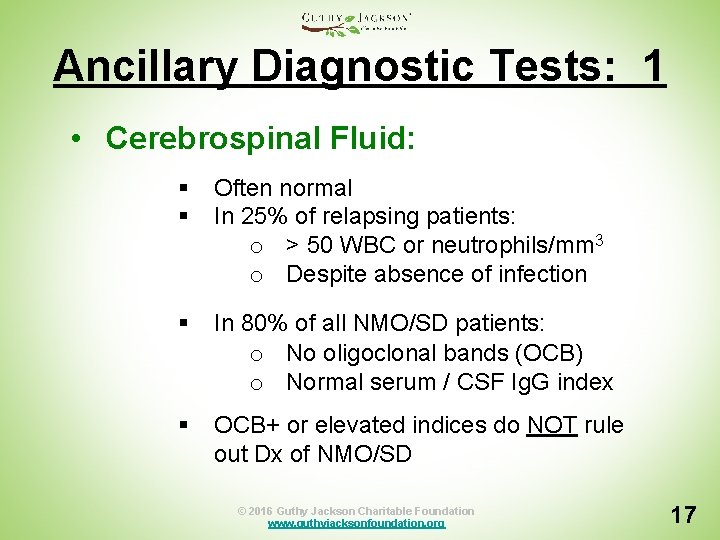
Ancillary Diagnostic Tests: 1 • Cerebrospinal Fluid: § § Often normal In 25% of relapsing patients: o > 50 WBC or neutrophils/mm 3 o Despite absence of infection § In 80% of all NMO/SD patients: o No oligoclonal bands (OCB) o Normal serum / CSF Ig. G index § OCB+ or elevated indices do NOT rule out Dx of NMO/SD © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 17
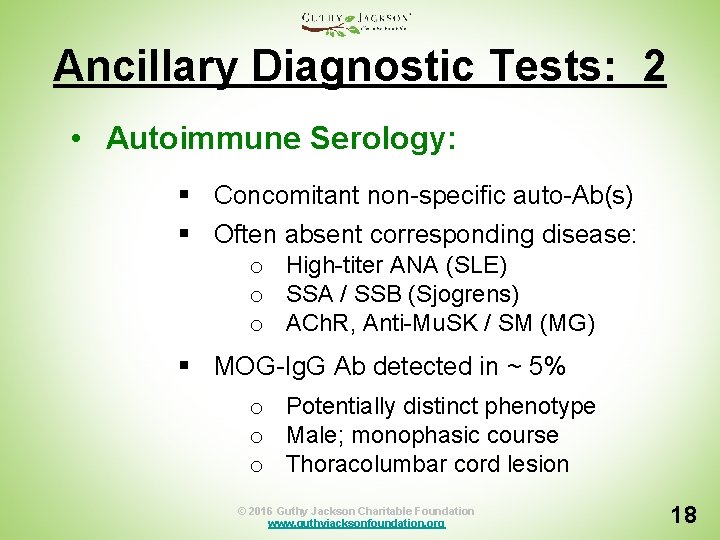
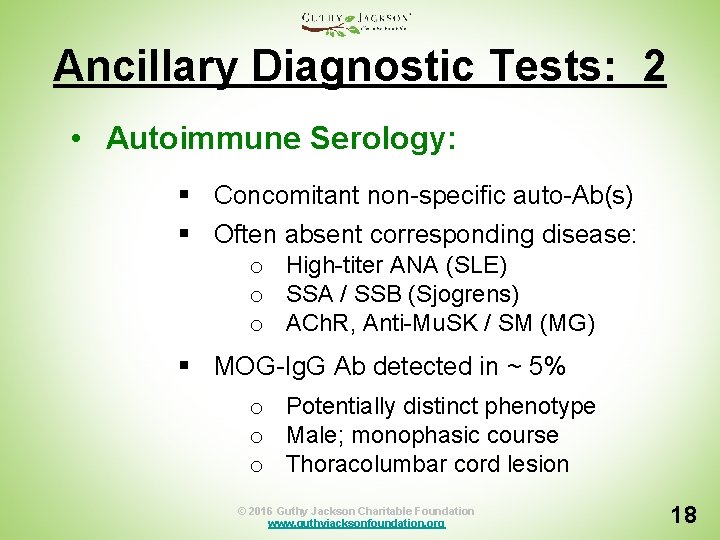
Ancillary Diagnostic Tests: 2 • Autoimmune Serology: § Concomitant non-specific auto-Ab(s) § Often absent corresponding disease: o High-titer ANA (SLE) o SSA / SSB (Sjogrens) o ACh. R, Anti-Mu. SK / SM (MG) § MOG-Ig. G Ab detected in ~ 5% o Potentially distinct phenotype o Male; monophasic course o Thoracolumbar cord lesion © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 18
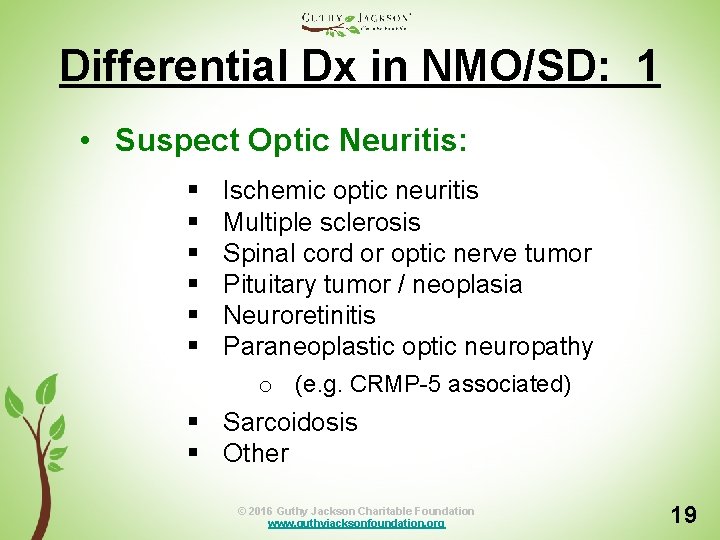
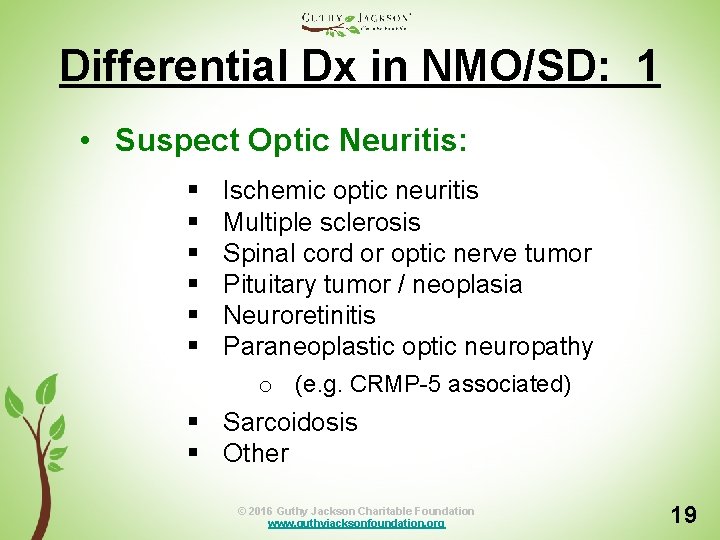
Differential Dx in NMO/SD: 1 • Suspect Optic Neuritis: § § § Ischemic optic neuritis Multiple sclerosis Spinal cord or optic nerve tumor Pituitary tumor / neoplasia Neuroretinitis Paraneoplastic optic neuropathy o (e. g. CRMP-5 associated) § Sarcoidosis § Other © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 19
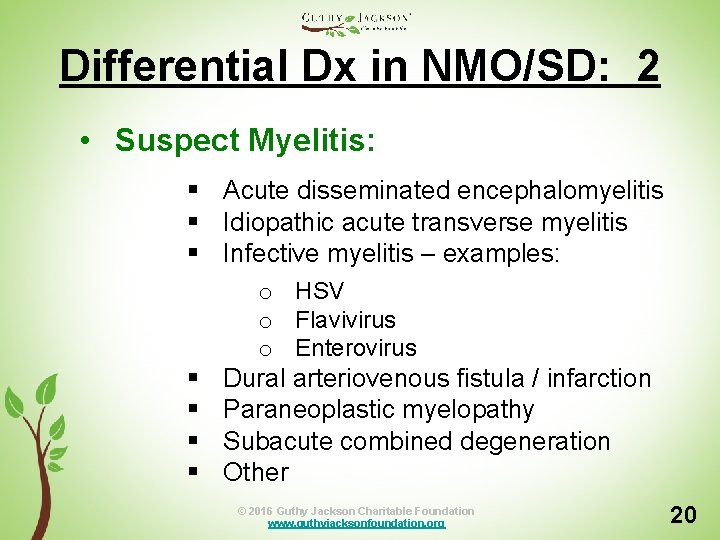
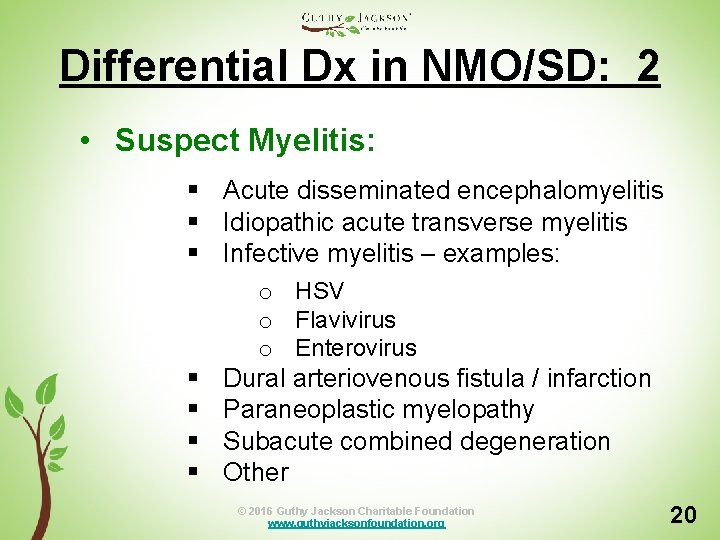
Differential Dx in NMO/SD: 2 • Suspect Myelitis: § Acute disseminated encephalomyelitis § Idiopathic acute transverse myelitis § Infective myelitis – examples: § § o HSV o Flavivirus o Enterovirus Dural arteriovenous fistula / infarction Paraneoplastic myelopathy Subacute combined degeneration Other © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 20
Module 1: Summary Consider NMO/SD Diagnosis Suspect NMO/SD Diagnosis Diagnostic Workup Schema Ancillary Diagnostic Tests Differential Diagnosis © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 3
![Module 1 References Wingerchuk DM et al with IPND 2015 International consensus diagnostic criteria Module 1: References Wingerchuk DM et al with IPND [2015] International consensus diagnostic criteria](https://slidetodoc.com/presentation_image/3106a3c4a68440e53690c69cecc0083e/image-22.jpg)
Module 1: References Wingerchuk DM et al with IPND [2015] International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85: 177 -189. Kim HJ et al with GJCF ICC&BR [2015] MRI characteristics of neuromyelitis optica spectrum disorder: an international update. Neurology 84: 1165 -1173. Kremer S et al with GJCF ICC&BR [2015] Use of advanced magnetic resonance imaging techniques in neuromyelitis optica spectrum disorder. JAMA Neurology 72: 815 -822. Sato DK et al [2014] Seronegative neuromyelitis spectrum – the challenges of disease definition and pathogenesis. Arq Neuropsiquiatr 72: 445 -450. Jarius S et al [2014] Neuromyelitis optica: clinical features, immunopathogenesis and treatment. Clin Exp Immunol 176: 149 -160. Papadopoulos MC et al [2014] Treatment of neuromyelitis optica: state-of-the-art and emerging therapies. Nature Rev Neurol 10: 493 -506. Weinshenker BG et al with GJCF ICC&BR [2015] Challenges and opportunities in designing clinical trials for neuromyelitis optica. Neurology 84: 1805 -1815. Melamed E et al with GJCF ICC&BR [2015] Update on biomarkers in neuromyelitis optica. Neurology Neuroimmunol Neuroinflamm 2(4): e 134. © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 22
NMO/SD Resources 2015 IPND Diagnostic Card / Toolkit NMOtion Patient & Advocate Gateway Searchable NMO/SD Biomedical Library The NMO Story Video & NMO TV NMO Resources Downloadable App © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 23
Clinical Evaluation of Neuromyelitis Optica Spectrum Disorder Module 1: Basic Diagnosis Authorship Team: Brian Weinshenker, M. D. Jacinta Behne, M. A. Terry Smith, M. D. Michael Yeaman, Ph. D. © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 24
Clinical Evaluation of Neuromyelitis Optica Spectrum Disorder Module 1: Basic Diagnosis © 2016 Guthy Jackson Charitable Foundation www. guthyjacksonfoundation. org 25
 Factitious disorder vs somatic symptom disorder
Factitious disorder vs somatic symptom disorder Added authorization in autism spectrum disorders
Added authorization in autism spectrum disorders Sensory processing disorder dsm
Sensory processing disorder dsm Are there different types of autism
Are there different types of autism Fetal alcohol spectrum disorder
Fetal alcohol spectrum disorder Autism spectrum disorder
Autism spectrum disorder Autism spectrum disorder adhd
Autism spectrum disorder adhd Spectrum disorder
Spectrum disorder Spectrum disorder
Spectrum disorder Orbital diagram for cu
Orbital diagram for cu Absorption spectrum
Absorption spectrum Celf 5 record form
Celf 5 record form Cuerpo geniculado lateral
Cuerpo geniculado lateral Estereoisómeros
Estereoisómeros Cabecera fibra optica
Cabecera fibra optica Hemianopsia bitemporal causas
Hemianopsia bitemporal causas Zeni optica
Zeni optica Luneta
Luneta Isomeria optica
Isomeria optica Enantiomeros
Enantiomeros Instrumente optice
Instrumente optice Conclusion de fibra optica
Conclusion de fibra optica Diagrama unifilar fibra optica
Diagrama unifilar fibra optica Colores de fibra optica
Colores de fibra optica Dispersia anormala
Dispersia anormala Sticla optica
Sticla optica