Cardiac Output Monitoring Monica Morosan Typical value l





- Slides: 22
Cardiac Output Monitoring Monica Morosan
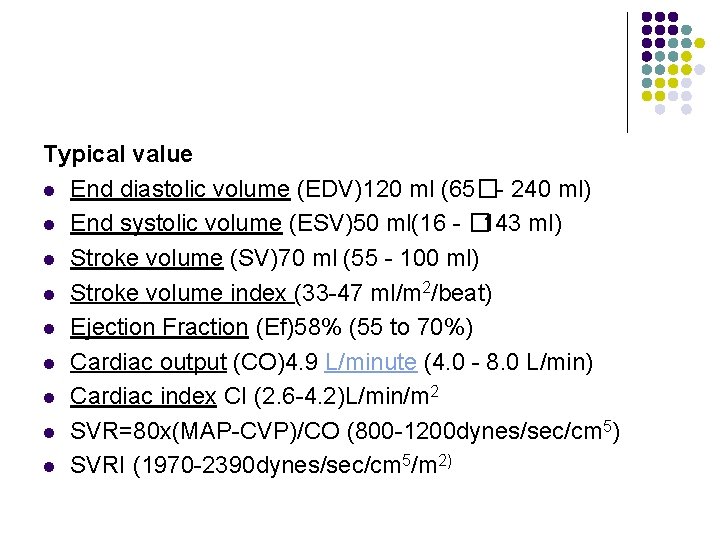
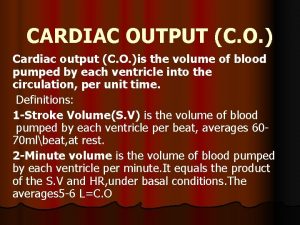
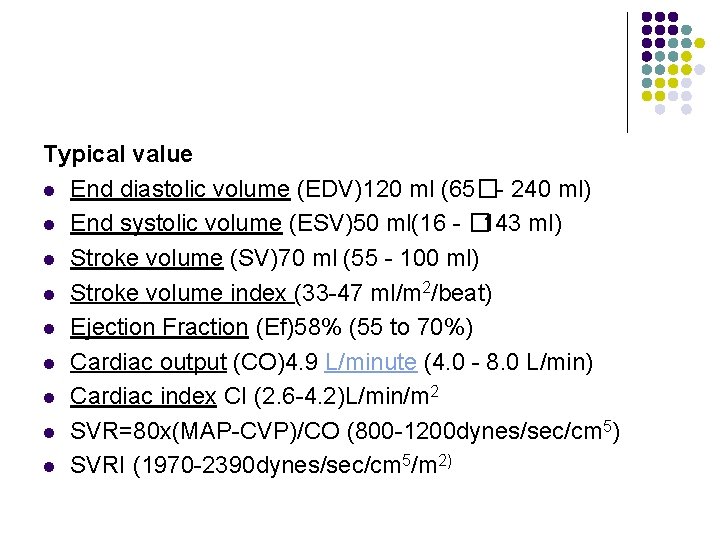
Typical value l End diastolic volume (EDV)120 ml (65�- 240 ml) l End systolic volume (ESV)50 ml(16 - � 143 ml) l Stroke volume (SV)70 ml (55 - 100 ml) l Stroke volume index (33 -47 ml/m 2/beat) l Ejection Fraction (Ef)58% (55 to 70%) l Cardiac output (CO)4. 9 L/minute (4. 0 - 8. 0 L/min) l Cardiac index CI (2. 6 -4. 2)L/min/m 2 l SVR=80 x(MAP-CVP)/CO (800 -1200 dynes/sec/cm 5) l SVRI (1970 -2390 dynes/sec/cm 5/m 2)

Cardiac output monitoring Invasive PA catheter l Non invasive TOE, Echo Oesophageal Doppler Transthoracic impedance Arterial pulse contour analysis (Pi. CCO) Arterial pulse power analysis (Li. DCO) l
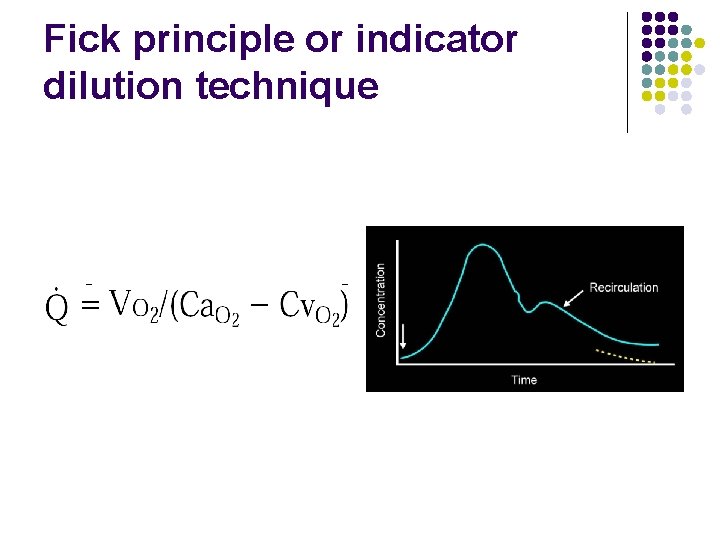
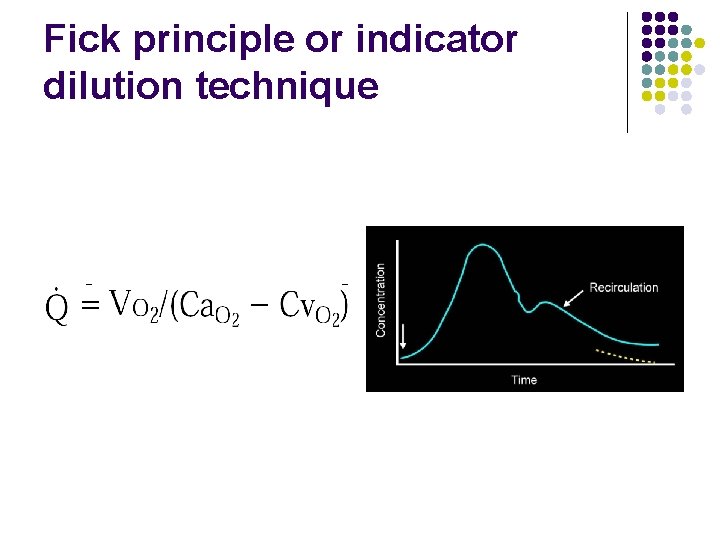
Fick principle or indicator dilution technique

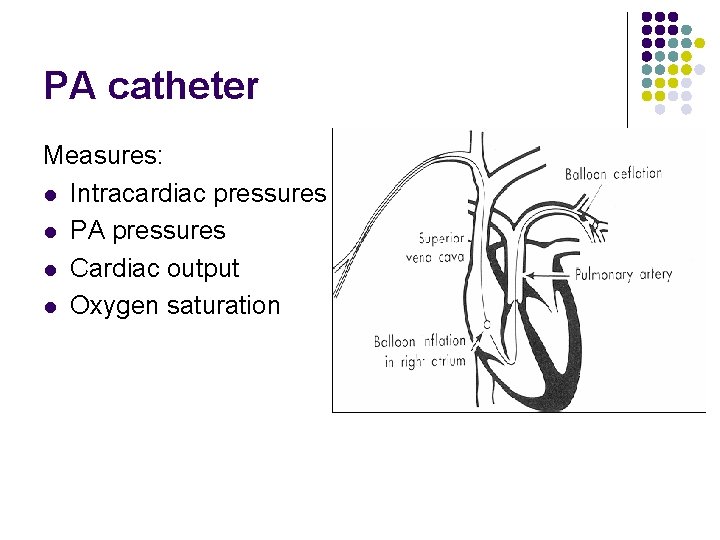
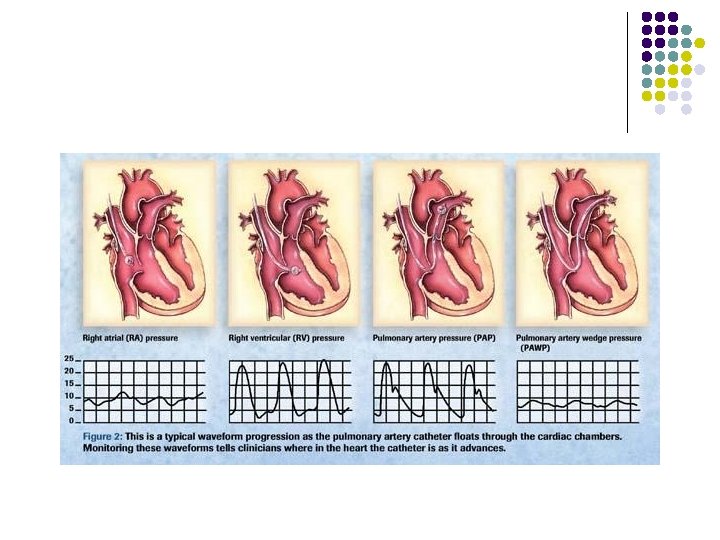
PA catheter
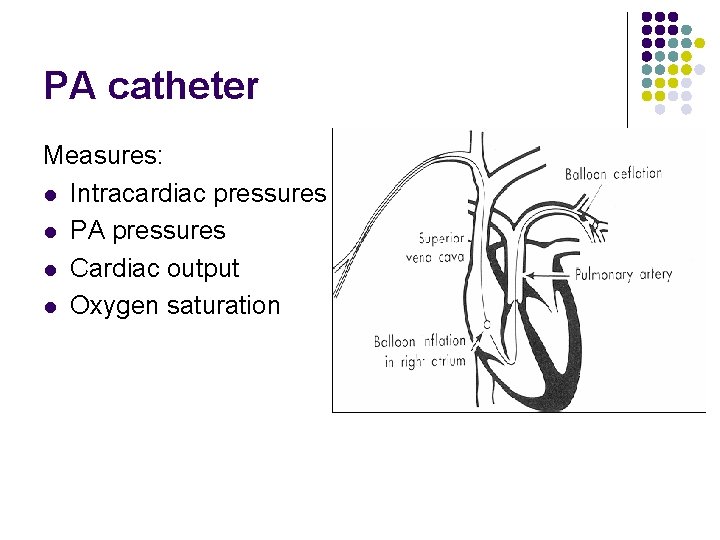
PA catheter Measures: l Intracardiac pressures l PA pressures l Cardiac output l Oxygen saturation

Indications: Contraindications: l IHD, Cardiogenic shock l Tricuspid or pulm valve mechanical prosthesis l RV failure l Right heart mass l Septic shock (Tumour or thrombus) l ARDS l Tricuspid or pulmonary l Periop: high risk cardiac endocarditis surgery or neurosurgery
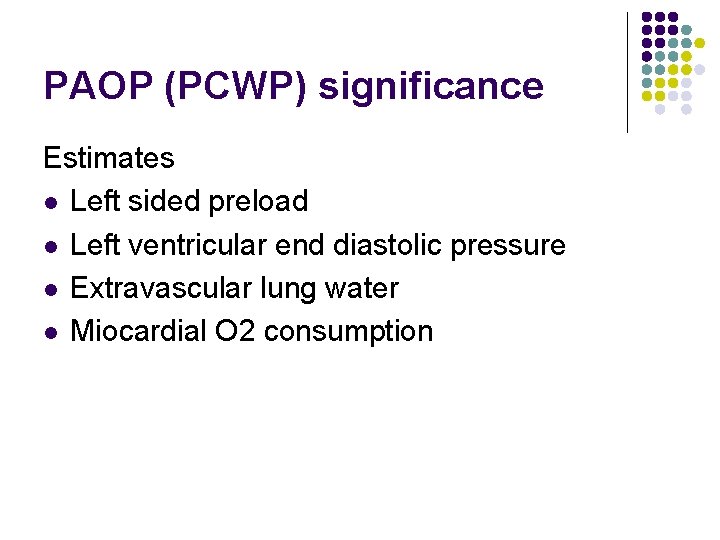
PAOP (PCWP) significance Estimates l Left sided preload l Left ventricular end diastolic pressure l Extravascular lung water l Miocardial O 2 consumption
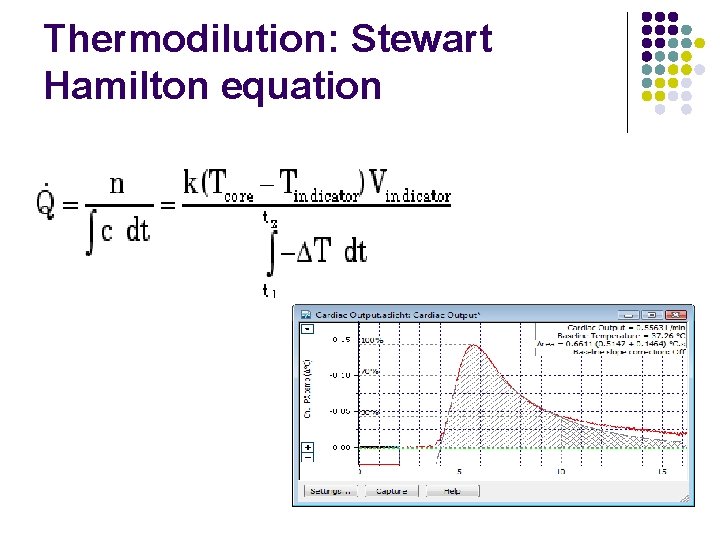
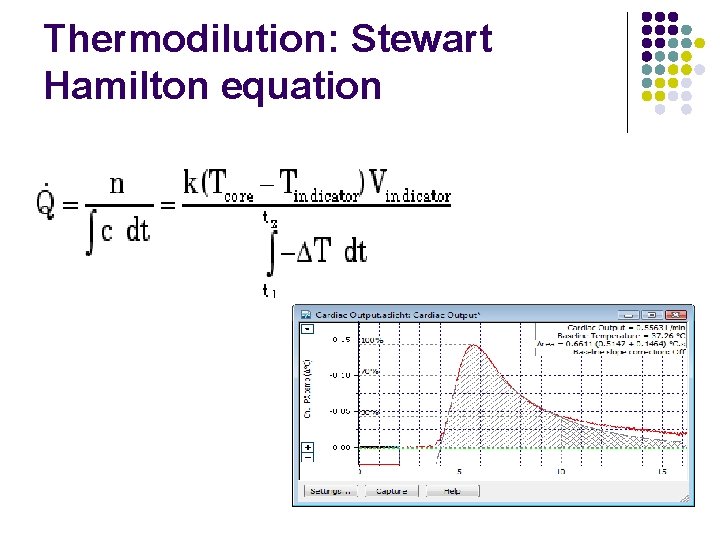
Thermodilution: Stewart Hamilton equation
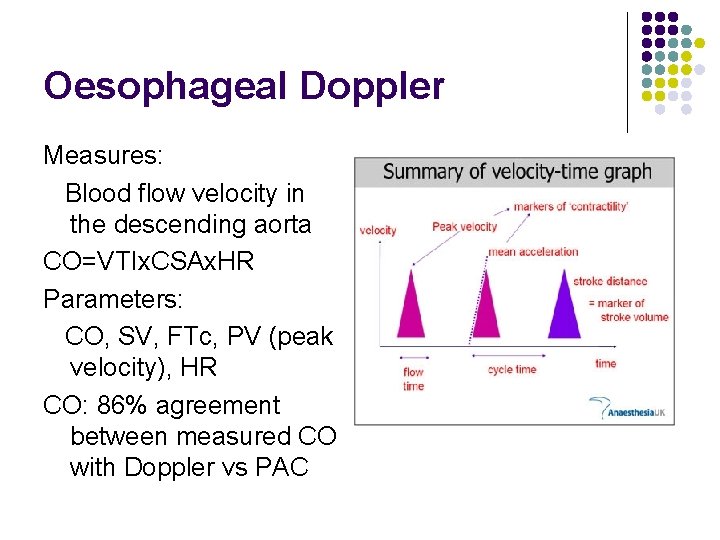
Oesophageal Doppler
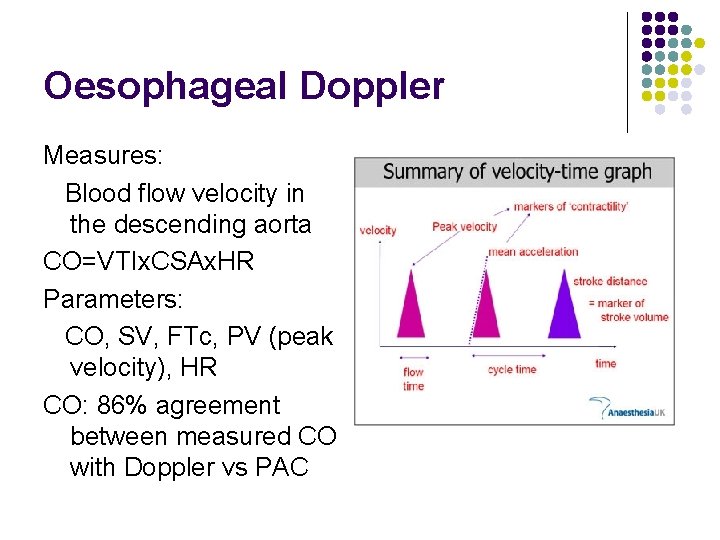
Oesophageal Doppler Measures: Blood flow velocity in the descending aorta CO=VTIx. CSAx. HR Parameters: CO, SV, FTc, PV (peak velocity), HR CO: 86% agreement between measured CO with Doppler vs PAC
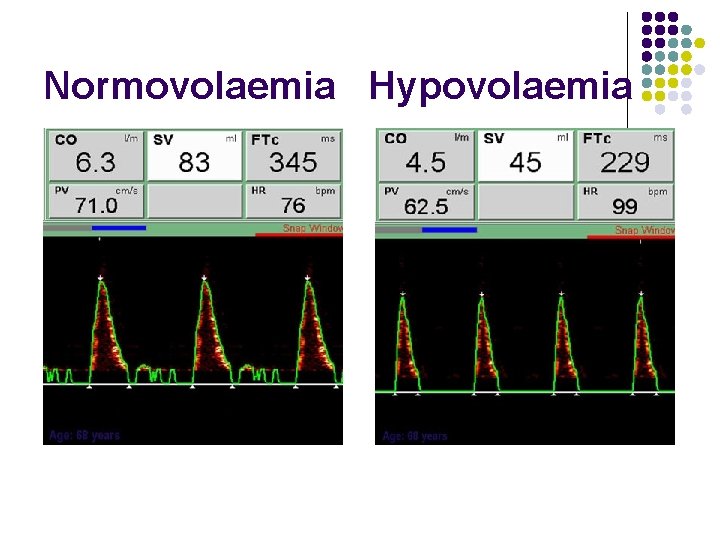
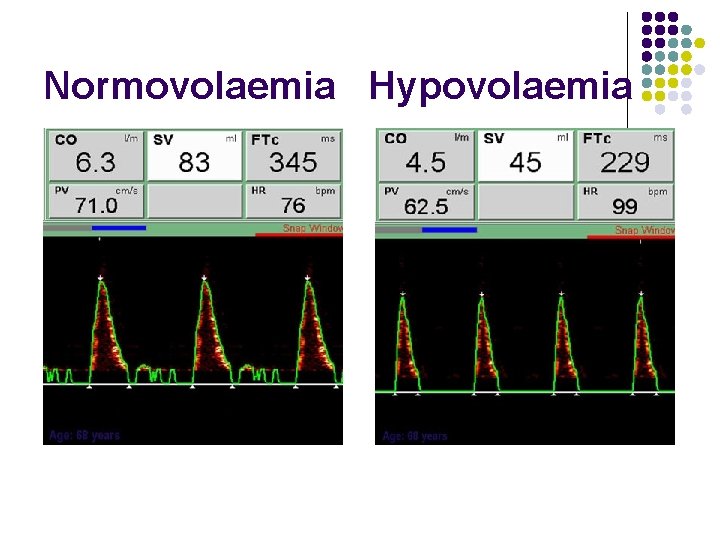
Normovolaemia Hypovolaemia
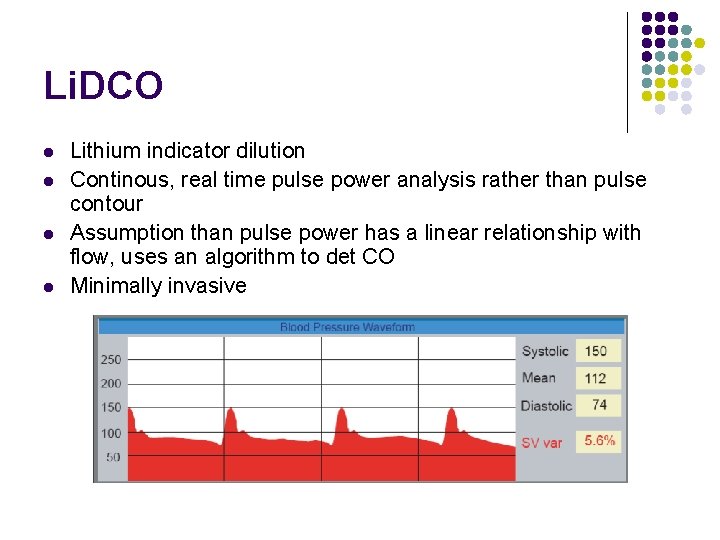
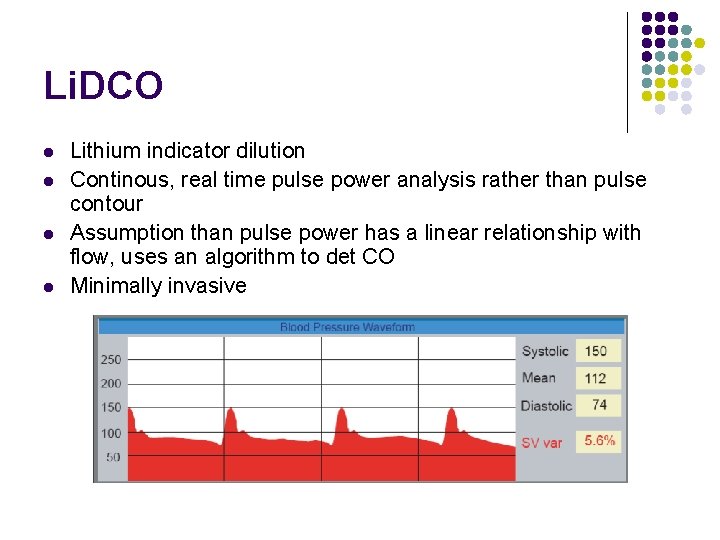
Li. DCO l l Lithium indicator dilution Continous, real time pulse power analysis rather than pulse contour Assumption than pulse power has a linear relationship with flow, uses an algorithm to det CO Minimally invasive

Safe l Uses the CVP catheter and A line l Injectate 0. 15 -0. 3 mmol Lithium Chloride Contraindications -If already on Lithium -Muscle relaxant drugs -Weight less then 40 kg -First 3 months pregnancy l
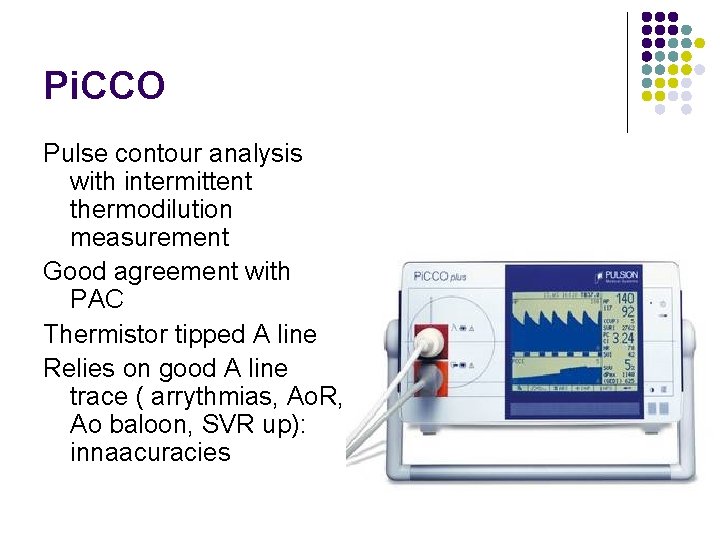
Pi. CCO Pulse contour analysis with intermittent thermodilution measurement Good agreement with PAC Thermistor tipped A line Relies on good A line trace ( arrythmias, Ao. R, Ao baloon, SVR up): innaacuracies
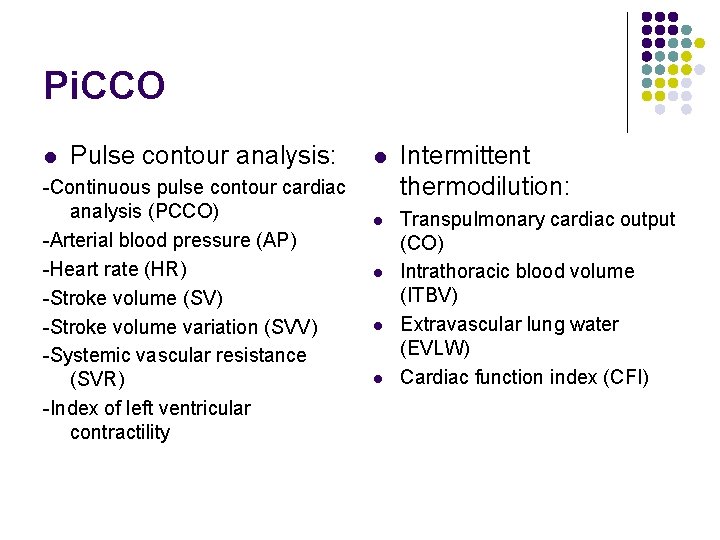
Pi. CCO l Pulse contour analysis: -Continuous pulse contour cardiac analysis (PCCO) -Arterial blood pressure (AP) -Heart rate (HR) -Stroke volume (SV) -Stroke volume variation (SVV) -Systemic vascular resistance (SVR) -Index of left ventricular contractility l Intermittent thermodilution: l Transpulmonary cardiac output (CO) Intrathoracic blood volume (ITBV) Extravascular lung water (EVLW) Cardiac function index (CFI) l l l
Impedance plethysmography l l l 2 sets circular wire electrodes around chest and neck Current passed between outer two( high frec, low magnitude), with measurement of potential difference between the inner two Maximal rate of change of impedance occurs with peak Ao flow Movement, arrythmias and diathermy: innacuracies More evidence in haemodynamically unstable
Thoracic bioreactance NICOM l l l Modification of impedance technology To improve the signal to noise ratio Phase shift in voltage across thorax 4 electrodes across thorax CO for L and R side and then averages Also averages over 60 s
Penaz technique l l l Continous pulse contour analysis of NIBP ( also known as vascular unloading technique) Finger cuff applies pressure Infrared light assesses the light absorbtion (artery diameter) Alters the pressure in the cuff to keep the diameter constant (this pressure=BP) Trace compared to oscillometric derived systolic and diastolic values Limitations: oedema or hypeperfusion, low CO, low SVR
Others l l Pulse wave transit time: continous, derived from ECG, sats probe trace and Art pressure Radial artery tonometry ECHO: LVEF, IVC collapsibility index All might have a place in low/intermediate risk patients, non-invasive haemodyn optimisation, ED department and diagnostic procedures

 Liceul tehnologic nicanor morosan
Liceul tehnologic nicanor morosan Homometric regulation of cardiac output
Homometric regulation of cardiac output Gittata sistolica
Gittata sistolica Map tpr x co
Map tpr x co Acute responses to training definition
Acute responses to training definition Cardiac output trained vs untrained
Cardiac output trained vs untrained Heart wall
Heart wall Heart rate during exercise
Heart rate during exercise Cardiac output trained vs untrained
Cardiac output trained vs untrained Cardiac output fick principle
Cardiac output fick principle Intrinsic conduction system
Intrinsic conduction system Fick principle cardiac output
Fick principle cardiac output Indicator dilution principle
Indicator dilution principle Co = hr x sv
Co = hr x sv Events of cardiac cycle class 11
Events of cardiac cycle class 11 Cardiac output stroke volume
Cardiac output stroke volume Heart sounds and murmurs
Heart sounds and murmurs Fick principle cardiac output
Fick principle cardiac output Cardiac muscle is
Cardiac muscle is End-diastolic volume vs end-systolic volume
End-diastolic volume vs end-systolic volume Cardiac output
Cardiac output Cardiac output
Cardiac output Cardiac output
Cardiac output