Autonomic NS 3 Cholinergic Antagonist Drugs Antimuscarinic drug







- Slides: 28
Autonomic NS 3

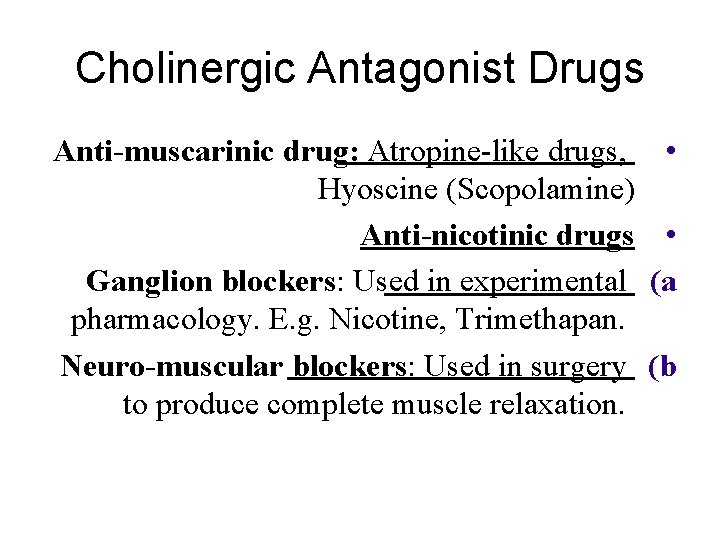
Cholinergic Antagonist Drugs Anti-muscarinic drug: Atropine-like drugs, Hyoscine (Scopolamine) Anti-nicotinic drugs Ganglion blockers: Used in experimental pharmacology. E. g. Nicotine, Trimethapan. Neuro-muscular blockers: Used in surgery to produce complete muscle relaxation. • • (a (b


Anti-muscarinic anti-cholinergic drugs Natural agents: q Atropine, Hyoscine • Semi-synthetic q Homatropine • Synthetic q Ipratropium, Pirenzepine, Propantheline •
Anti-muscarinic Atropine (Hyoscyamine) q Alkaloids obtained from Atropa Belladona, ü Considered as prototype for parasympatolytics ü Hyoscine (Scopolamine) q Obtained from Hyocyamus niger plant (Datura ü Stramonium) Note: Antihistamines, phenothiazides and some antidepressants have anti-muscarinic effects
Clinical pharmacology of antimuscarinic drugs Mechanism of action: Reversible blockade of M receptors Exocrine glands are most sensitive Gastric secretion is the least affected Heart is intermediate • • Note: Atropine blocks all 3 subtypes receptors (M 1, M 2, M 3)
Pharmacokinetics Absorption: q Natural and most tertiary amines: good § Wide distribution and cross BBB § Quaternary amines: poorly absorbed and poor § crossing BBB (Ipratropium) Atropine t½: 2 hrs q Partly metabolized and partly excreted unchanged q
Pharmacodynamics Exocrine glands: at low doses q reduced secretions Salivary • Bronchial • Sweet glands •

CNS Central stimulant effects (Atropine) Some may produce sedation (Hyoscine) Hyoscine blocks M receptors in vomiting centre and has anti-emetic effect Toxic doses: hallucination, convulsion, coma • •
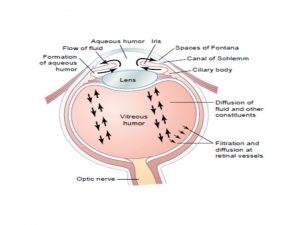
Eye Mydriasis (dilatation of pupil)ü Cycloplegia (relaxation of the ciliary ü muscle) cause: blurred vision and impaired accommodation to near vision Decreased lacrimationü Increase IOPü

CVS Depending in the doses Central effect: • Decrease heart rate § Peripheral effect: • Blockade of vagus nerve and increase heart rate § ABP: • No change §
Respiratory system Bronchodilatation • Reduced bronchial secretion • Ipratropium (quaternary amine derivate of • Atropine) inhalation: Useful in asthma and chronic obstructive pulmonary ü disease (COPD), also in patient who are unable to take adrenergic agonists.

GIT Decrease salivation Decrease acid secretion Decrease motility Delay gastric emptying Prolong intestinal transit time Anti-diarrhoeal and anti-spasmodic effects • • •
Therapeutic uses CNS disorders: Parkinson’s disease • Drug-induced parkinsonism as Phenothiazine (induced acute • dystonias: sustained contraction of muscles leading to twisting, distorted postures) Benztropine, Benzhexol: useful • Motion sickness: Hyoscine oral, injection, trans-dermal patches •
Therapeutic uses Ocular uses: In eye examination (Tropicamide) produce mydriasis and • cycloplegia In iritis (Atropine eye drop) prevent synechia (adhesion of the • iris to the lens) Note: Atropine eye drops effects: 7 days • Tropicamide eye drops effects: 4 -12 hrs •
Therapeutic uses Premedication: Hyoscine and Atropine (use as adjunct in • anaesthetic procedure) Bronchial asthma: Ipratropium inh. (produce • bronchodilatation) Cardiovascular: Bradycardia and heart block following AMI: Atropine •
Therapeutic uses GI disorders: Anti-diarrhoeal � Lomotil= atropine + diphenoxylate • Anti-spasmodics (in intestinal colic, irritable � bowel syndrome) Atropine, hyoscine, clidinium, prifinium. • Urinary disorders: Urinary urgency with UTI � Renal colic �
Therapeutic uses Cholinergic poisoning as: � Irreversible CEI insecticide poisoning • Chemical warfare intoxication. • To counteract muscarinic effects � (nicotinic effects can not be reversed) � Atropine IV �

Adverse effects of anti-muscarinic agents Dry mouth Blurred vision Tachycardia Constipation Hot flushed dry skin & hyperthermia may occur with high doses � � �
Contraindications Glaucoma q Increase IOP • BPH q Bladder wall relaxation & sphincter • contraction
Individual drugs Atropine • Hyoscine • Buscopan • Clidinium • Libraxam • Prifinium Riabal • •
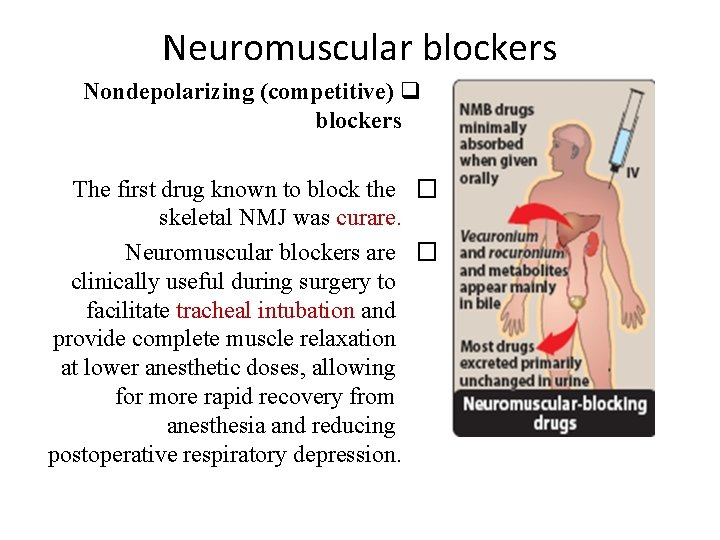
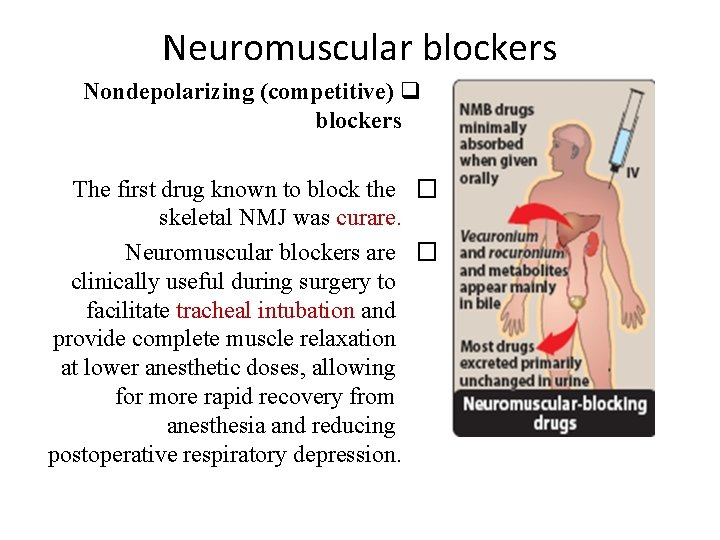
Neuromuscular blockers Nondepolarizing (competitive) q blockers The first drug known to block the � skeletal NMJ was curare. Neuromuscular blockers are � clinically useful during surgery to facilitate tracheal intubation and provide complete muscle relaxation at lower anesthetic doses, allowing for more rapid recovery from anesthesia and reducing postoperative respiratory depression.
Neuromuscular blockers Depolarizing agents � Depolarizing blocking � agents work by depolarizing the plasma membrane of the muscle fiber, similar to the action of ACh.
 Mosby items and derived items
Mosby items and derived items Autonomic drugs
Autonomic drugs Anticholinergic vs antimuscarinic
Anticholinergic vs antimuscarinic Vasicoselective action
Vasicoselective action Parasympathetic drugs classification
Parasympathetic drugs classification Anticholinergic examples
Anticholinergic examples M cholinomimetic drugs examples
M cholinomimetic drugs examples Muscarinic vs nicotinic receptors
Muscarinic vs nicotinic receptors Indirect acting cholinergic agonist
Indirect acting cholinergic agonist Classification of cholinergic drugs
Classification of cholinergic drugs Tropicamaide
Tropicamaide Indirect acting cholinergic drugs
Indirect acting cholinergic drugs Sar of cholinergic agents
Sar of cholinergic agents Adp antagonist drugs
Adp antagonist drugs Antagonist drug
Antagonist drug What is an agonist
What is an agonist Deliberate adulteration definition
Deliberate adulteration definition Somatic vs autonomic nervous system
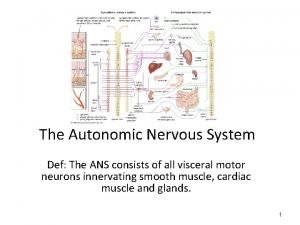
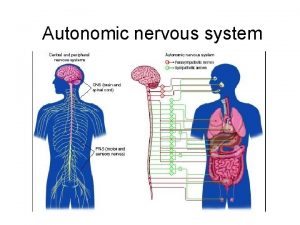
Somatic vs autonomic nervous system Autonomic motor neurons regulate visceral activities by
Autonomic motor neurons regulate visceral activities by Visceral autonomic nervous system
Visceral autonomic nervous system Somatic vs autonomic reflexes
Somatic vs autonomic reflexes Somatic and autonomic nervous system
Somatic and autonomic nervous system Autonomic reflexes
Autonomic reflexes Autonomic nervous system
Autonomic nervous system Autonomic nervous system consists of
Autonomic nervous system consists of Autonomic nerveous system
Autonomic nerveous system Autonomic network management
Autonomic network management Ans
Ans Automatic bladder
Automatic bladder