Cholinergic Antagonists Cholinergic Antagonists Cholinergic antagonist is a
- Slides: 22
Cholinergic Antagonists
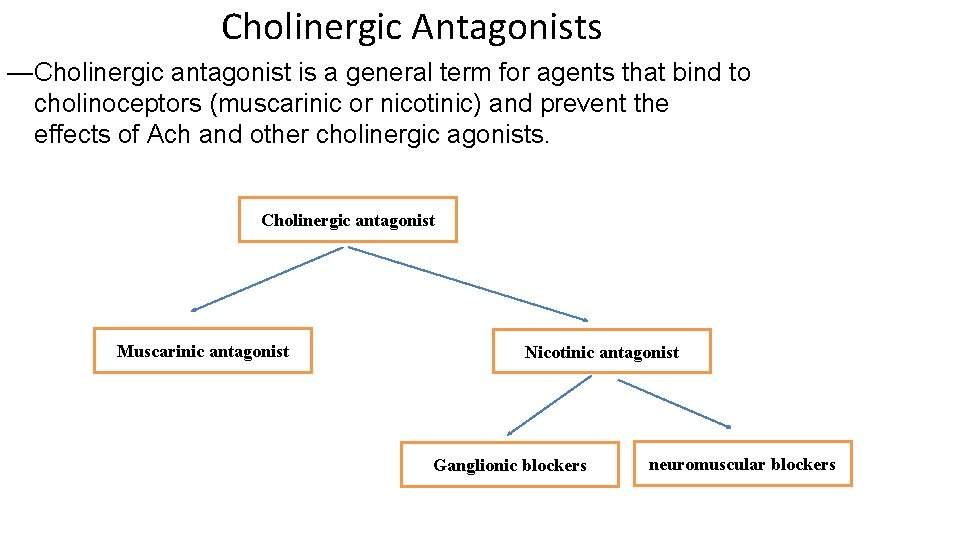
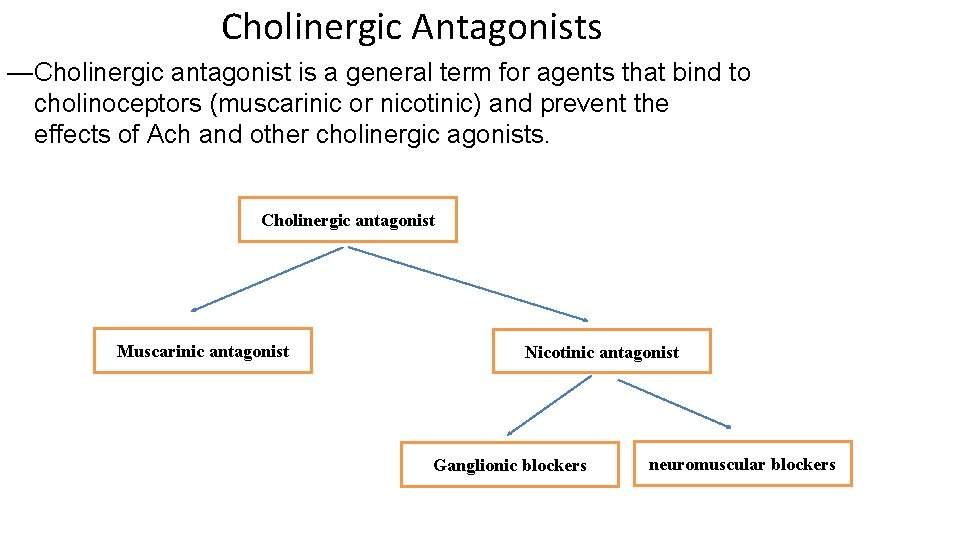
Cholinergic Antagonists —Cholinergic antagonist is a general term for agents that bind to cholinoceptors (muscarinic or nicotinic) and prevent the effects of Ach and other cholinergic agonists. Cholinergic antagonist Muscarinic antagonist Nicotinic antagonist Ganglionic blockers neuromuscular blockers
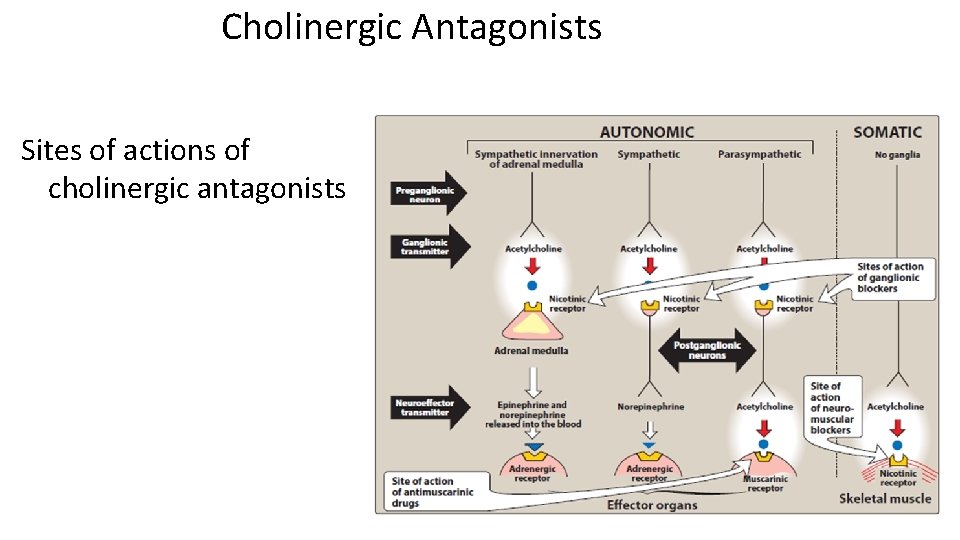
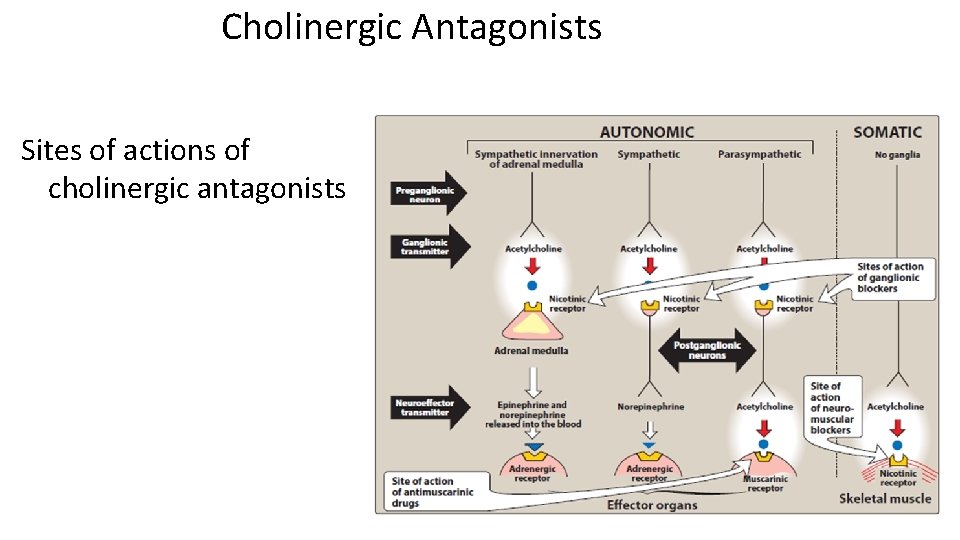
Cholinergic Antagonists Sites of actions of cholinergic antagonists
Muscarinic antagonist • The most clinically useful cholinergic antagonist are selective blockers of muscarinic receptors. • They are commonly known as antimuscarinic agents or parasympatholytics (The effects of parasympathetic innervation are, interrupted, and the actions of sympathetic stimulation are left unopposed). • These drugs block the few exceptional sympathetic neurons that are cholinergic, such the sweat glands. • Because do not block nicotinic receptors, the antimuscarinic drugs have little or no action at skeletal neuromuscular junctions or autonomic ganglia.
Atropine • High affinity for muscarinic receptors. • Binds competitively and prevents ACh from binding to muscarinic receptors. • Acts both centrally (cross blood brain barrier) and peripherally.
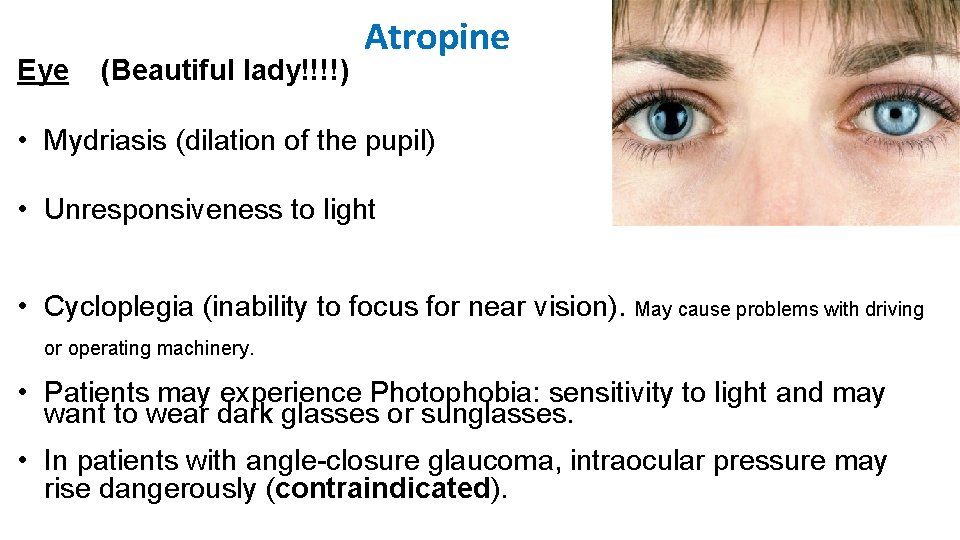
Eye (Beautiful lady!!!!) Atropine • Mydriasis (dilation of the pupil) • Unresponsiveness to light • Cycloplegia (inability to focus for near vision). May cause problems with driving or operating machinery. • Patients may experience Photophobia: sensitivity to light and may want to wear dark glasses or sunglasses. • In patients with angle-closure glaucoma, intraocular pressure may rise dangerously (contraindicated).
Atropine Gastrointestinal (GI) • Antispasmodic to reduce activity of the GI tract. • Most potent antispasmodic drugs available. • Treatment of Irritable bowel disease • Treatment of GI hypersecretory states • May cause constipation Cardiovascular • Causes a progressive increase in heart rate by blocking the M 2 receptors on the sinoatrial node.
Atropine Secretions • Dryness of the mouth (xerostomia). • Decreases sweating and tearing. • Is used as an antisecretory agent to block secretions in the respiratory tract prior to surgery. Genitourinary • Relaxed detrusor muscle • Increased constriction of internal sphincter Result: urinary retention Antidote for cholinergic agonists • Atropine is used for the treatment of organophosphate (insecticides, nerve gases) poisoning, of overdose of clinically used anticholinesterases such as physostigmine.
Atropine Adverse effects • Dry mouth, blurred vision, “sandy eyes dry red irritant eyes, ” tachycardia, urinary retention, and constipation. • Effects on the CNS include restlessness, confusion, hallucinations, and delirium, which may progress to depression, collapse of the circulatory and respiratory systems, and death. • Physostigmine, may be used to overcome atropine toxicity. !!!! Why? ? • The drug may be dangerous in children, because it may dangerously elevate their body temperature. • Anticholinergics may lead to higher risk for heat stroke due to effects on heat-regulating mechanisms.
Scopolamine • Has greater action on the CNS and a longer duration of action as compared to atropine. • Is effective anti–motion sickness. • May produce euphoria and is susceptible to abuse.
Hyoscine • Semi- synthetic derivative of scopolamine. • Works more peripherally on the GI tract than centrally. • Is effective Antispasmodic. Available in Jordan
Ipratropium Available in Jordan • Are quaternary (Charged) derivatives of atropine, do not enter the systemic circulation or the CNS. • Are approved as bronchodilators for maintenance treatment of bronchospasm associated with chronic obstructive pulmonary disease (COPD). • Ipratropium is also used in the acute management of bronchospasm in asthma. • Both agents are delivered via inhalation.
Oxybutynin • These synthetic atropine-like drugs are used to treat overactive bladder. Prifinium • • Is an anticholinergic with selective spasmolytic action on the gastro-intestinal and urinary tracts. It inhibits pain from spasm or hypermotility of these organs. Available in Jordan
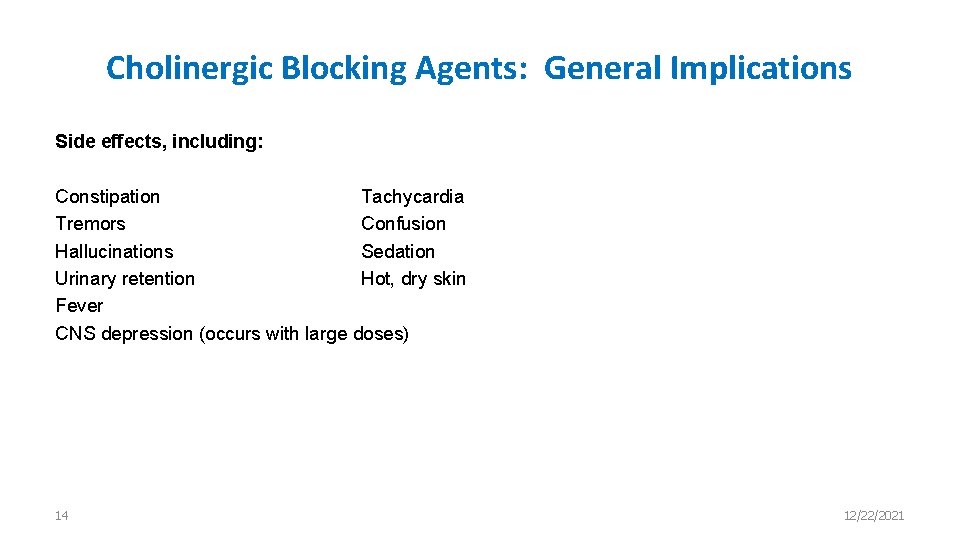
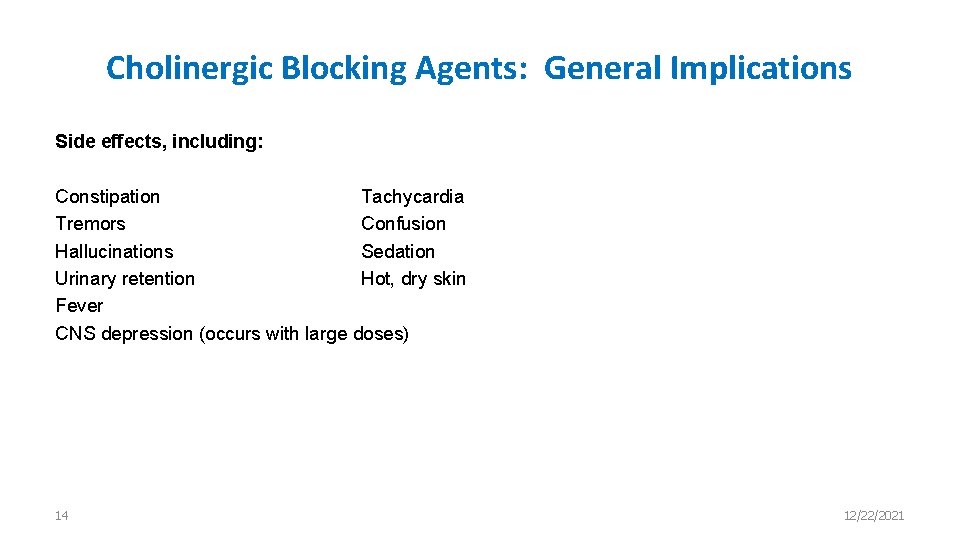
Cholinergic Blocking Agents: General Implications Side effects, including: Constipation Tachycardia Tremors Confusion Hallucinations Sedation Urinary retention Hot, dry skin Fever CNS depression (occurs with large doses) 14 12/22/2021
Neuromuscular Blockers
Neuromuscular-Blocking Agents • Block cholinergic transmission between motor nerve endings and the nicotinic receptors on the skeletal muscle. • Act either as: A) Non- depolarizing type(Antagonists) Or B) Depolarizing type (Agonists) at the receptors on the endplate of the NMJ. • Are clinically useful during surgery to facilitate trachea intubation and provide complete muscle relaxation at lower anesthetic doses (safe).
A. Nondepolarizing blockers • Curare, which native South American hunters used to paralyze prey. • The development of the drug tubocurarine followed. • It has been replaced by safer agents, such as cisatracurium , pancuronium, rocuronium , and vecuronium. • Are injected intravenously or occasionally intramuscularly since they are not effective orally. • They penetrate membranes very poorly and do not enter cells or cross the blood– brain barrier.
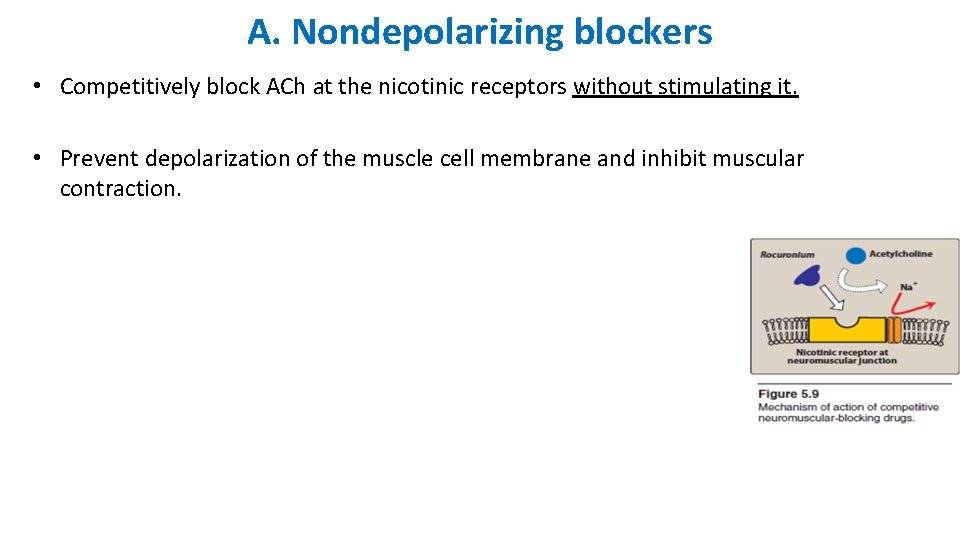
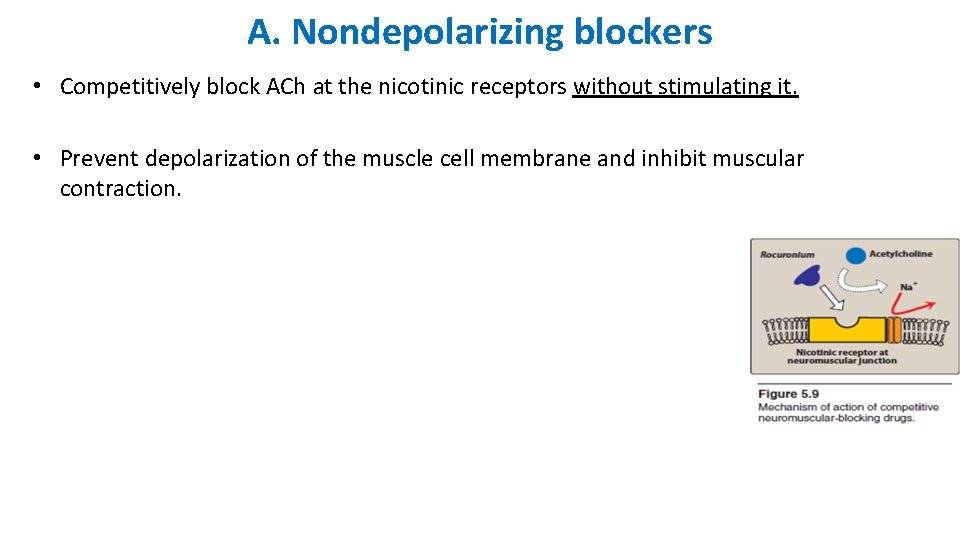
A. Nondepolarizing blockers • Competitively block ACh at the nicotinic receptors without stimulating it. • Prevent depolarization of the muscle cell membrane and inhibit muscular contraction.
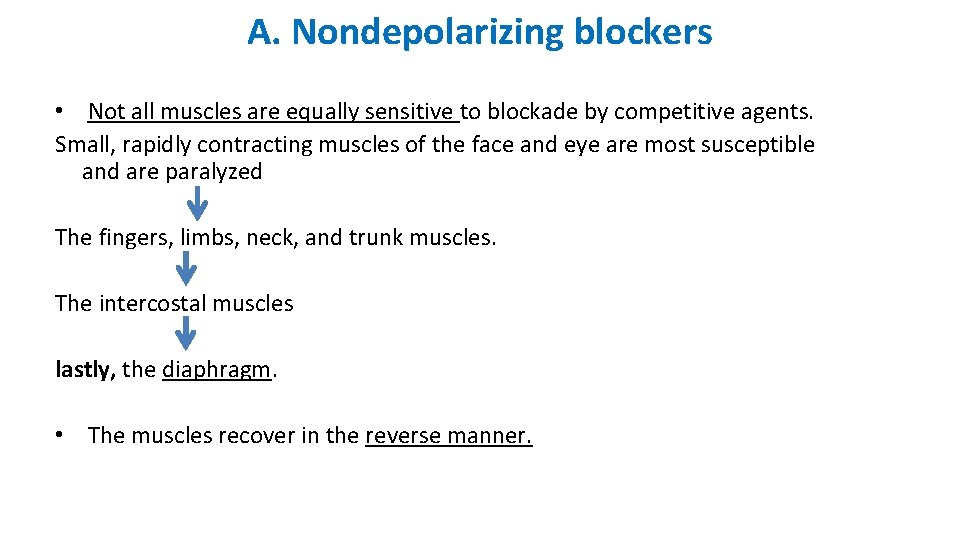
A. Nondepolarizing blockers • Not all muscles are equally sensitive to blockade by competitive agents. Small, rapidly contracting muscles of the face and eye are most susceptible and are paralyzed The fingers, limbs, neck, and trunk muscles. The intercostal muscles lastly, the diaphragm. • The muscles recover in the reverse manner.
B. Depolarizing agents • Work by depolarizing the plasma membrane of the muscle fiber, similar to the action of ACh. • However, these agents are more resistant to degradation by acetylcholinesterase and can thus more persistently depolarize the muscle fibers. • Succinylcholine is the only depolarizing muscle relaxant.
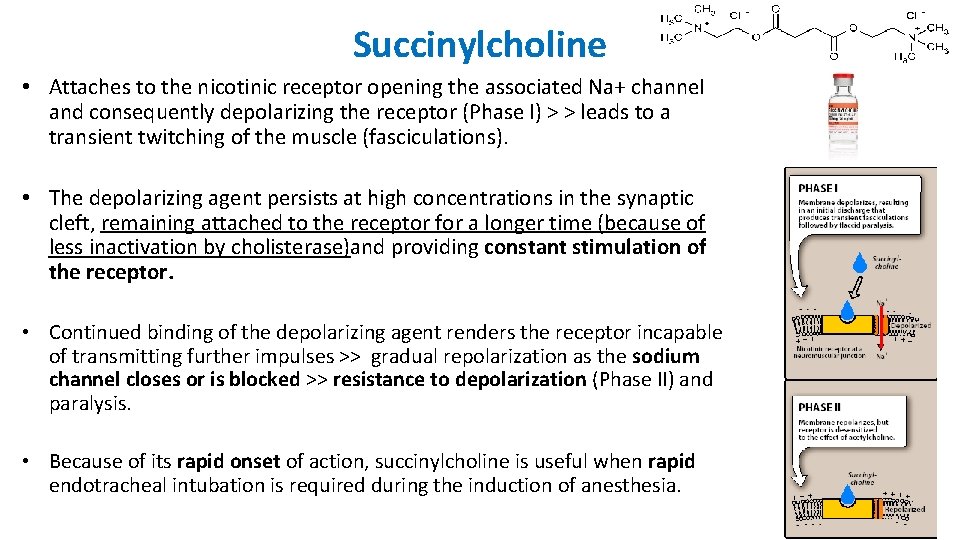
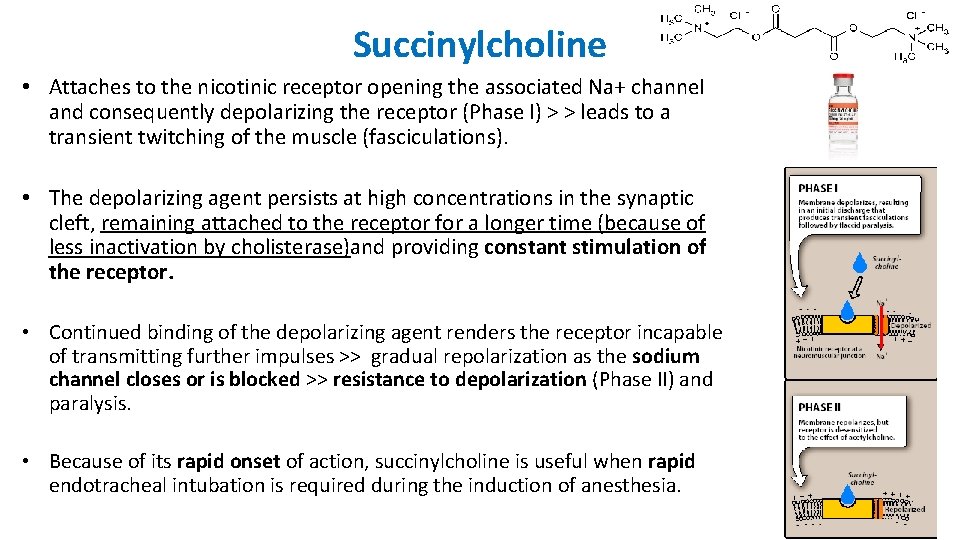
Succinylcholine • Attaches to the nicotinic receptor opening the associated Na+ channel and consequently depolarizing the receptor (Phase I) > > leads to a transient twitching of the muscle (fasciculations). • The depolarizing agent persists at high concentrations in the synaptic cleft, remaining attached to the receptor for a longer time (because of less inactivation by cholisterase)and providing constant stimulation of the receptor. • Continued binding of the depolarizing agent renders the receptor incapable of transmitting further impulses >> gradual repolarization as the sodium channel closes or is blocked >> resistance to depolarization (Phase II) and paralysis. • Because of its rapid onset of action, succinylcholine is useful when rapid endotracheal intubation is required during the induction of anesthesia.
Succinylcholine Adverse effects • 1) Hyperthermia • Is overomed by administration of dantrolene , which blocks release of Ca 2+ from the sarcoplasmic reticulum of muscle cells, thereby reducing heat production and relaxing muscle tone. 2) Apnea (due to paralysis of the diaphragm) 3) Hyperkalemia (increases potassium release from intracellular stores to the plasma)