Assessing Suicide Risk with the QPRT SUICIDE AND




- Slides: 28
Assessing Suicide Risk with the QPRT
SUICIDE AND RISK ¨ Personally humiliating events. ¨ The greater the number of losses, the greater the risk. ¨ No good evidence for sexual orientation as an independent risk factor for suicide. ¨ Treatment prevents suicide. Eve Morscicki, NIMH, 1997
SUICIDE AND RISK ¨ Necessary condition + trigger(s) push suicide threshold. ¨ Distal vs. Proximal & Trait vs. State. ¨ Halt (hungry, angry, lonely, tired). ¨ Mental illness and suicide connection (90+%). ¨ Comorbidity is the single greatest risk.
STATUS OF SUICIDE RISK ASSESSMENT ¨ National Survey: Almost all clinicians rely on clinical interview (Jobes, Eyman & Yufi, 1995). ¨ No known method to identify those few who complete suicide. ¨ Beck Hopelessness Scale. ¨ Current methods produce large numbers of false positives. ¨ Risk detection is job one.
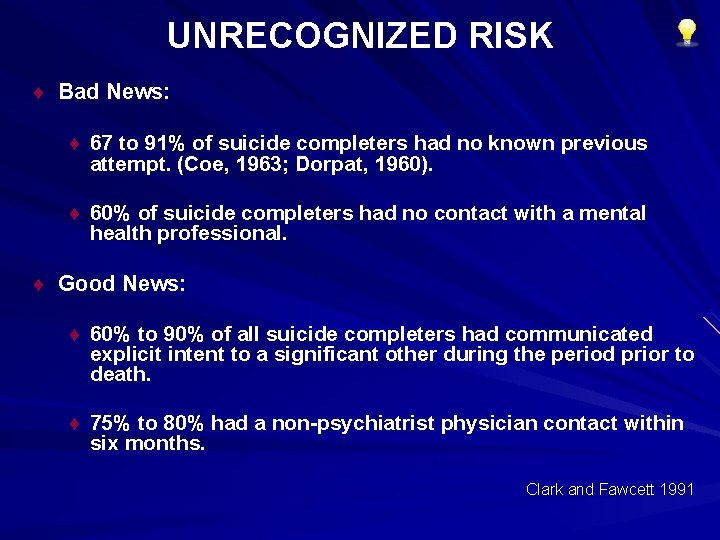
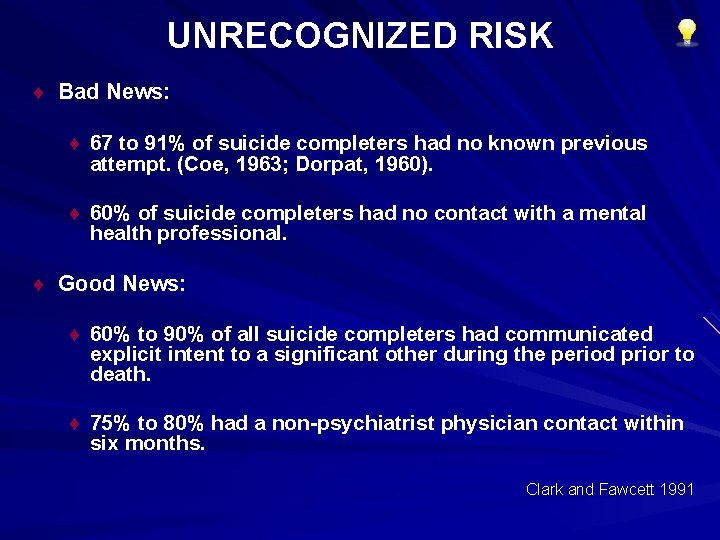
UNRECOGNIZED RISK ¨ Bad News: ¨ 67 to 91% of suicide completers had no known previous attempt. (Coe, 1963; Dorpat, 1960). ¨ 60% of suicide completers had no contact with a mental health professional. ¨ Good News: ¨ 60% to 90% of all suicide completers had communicated explicit intent to a significant other during the period prior to death. ¨ 75% to 80% had a non-psychiatrist physician contact within six months. Clark and Fawcett 1991
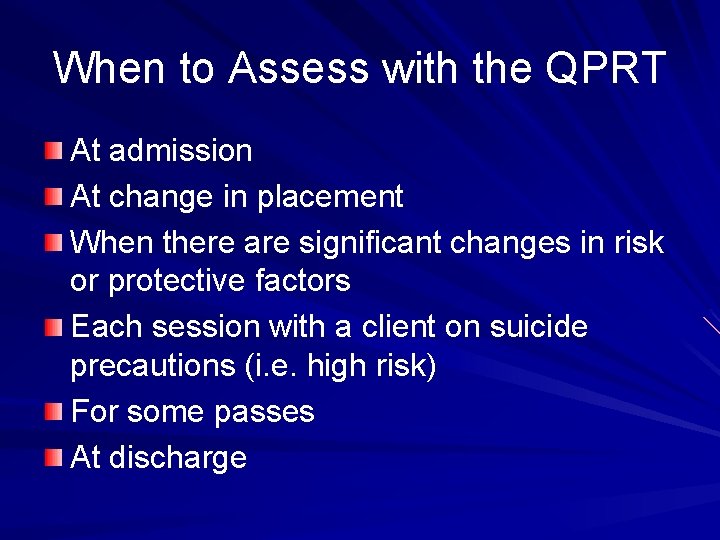
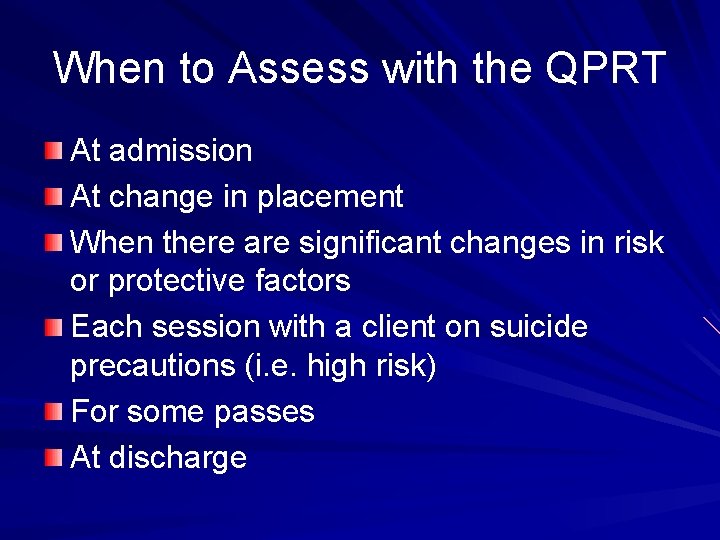
When to Assess with the QPRT At admission At change in placement When there are significant changes in risk or protective factors Each session with a client on suicide precautions (i. e. high risk) For some passes At discharge
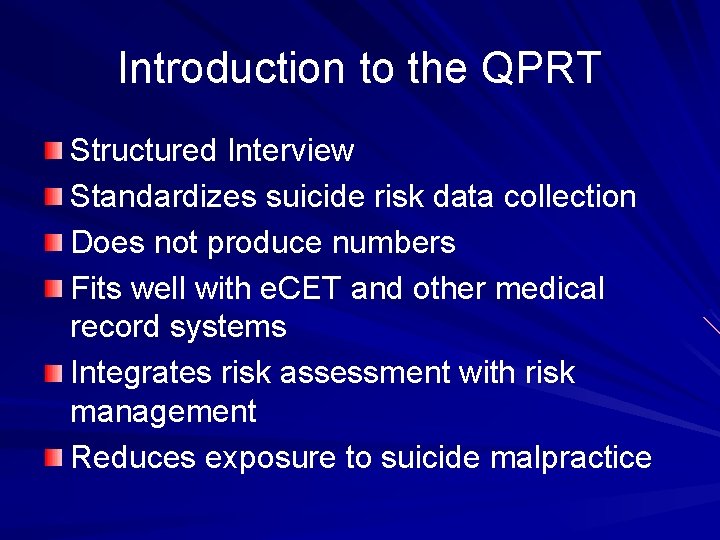
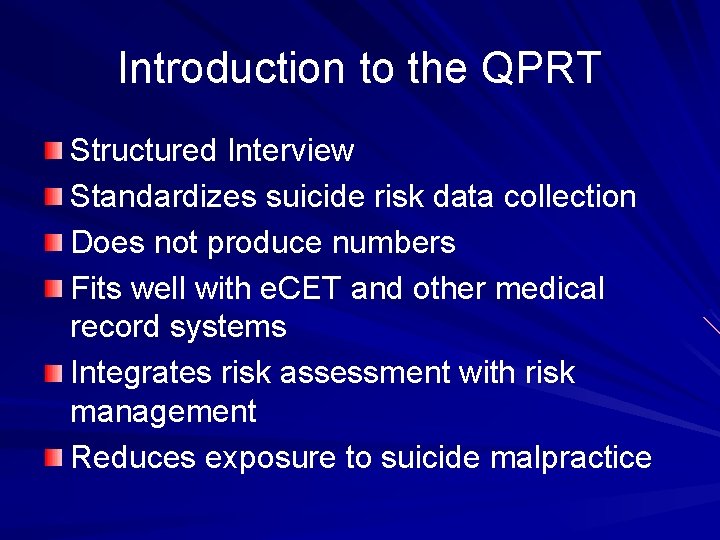
Introduction to the QPRT Structured Interview Standardizes suicide risk data collection Does not produce numbers Fits well with e. CET and other medical record systems Integrates risk assessment with risk management Reduces exposure to suicide malpractice

QPRT Intake Forms Pediatric (up to 18 yrs. ) One Manual Adult Inpatient & outpatient manuals Inpatient (RTC, Hospital, Group Homes) Outpatient (O/P Clinics Foster Care) X X
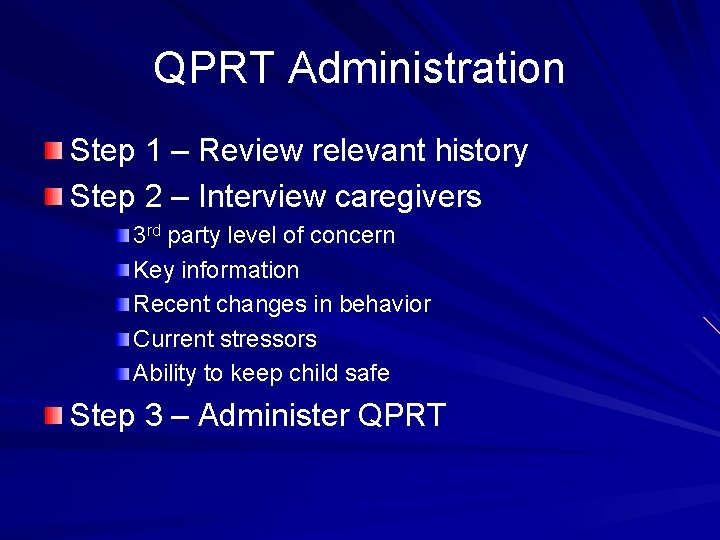
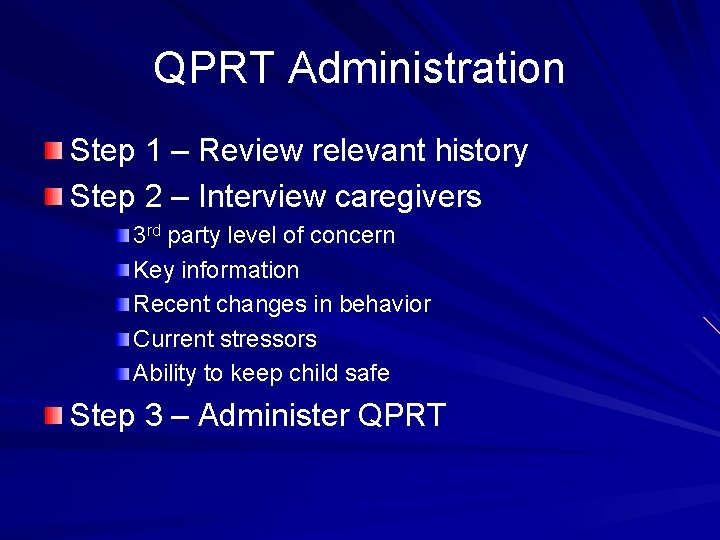
QPRT Administration Step 1 – Review relevant history Step 2 – Interview caregivers 3 rd party level of concern Key information Recent changes in behavior Current stressors Ability to keep child safe Step 3 – Administer QPRT
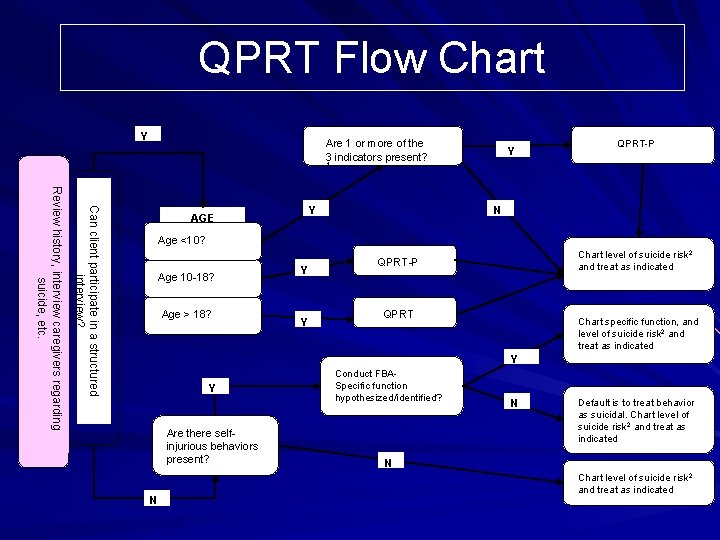
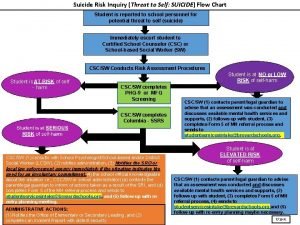
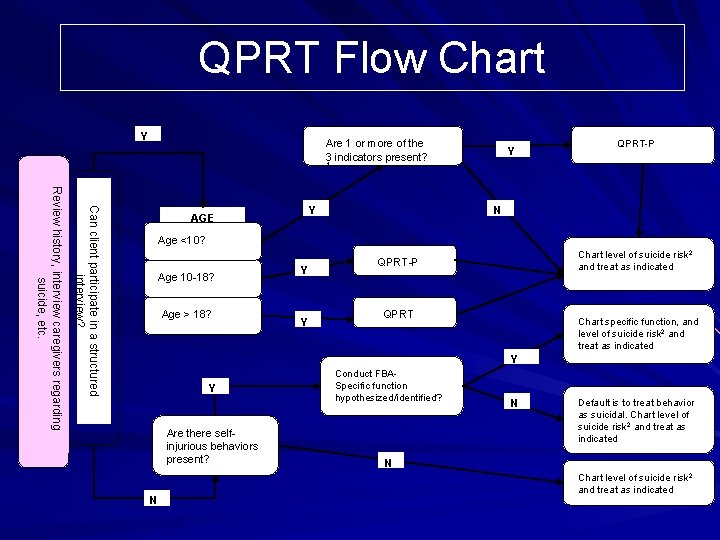
QPRT Flow Chart Y Are 1 or more of the 3 indicators present? Y QPRT-P 1 Can client participate in a structured interview? Review history, interview caregivers regarding suicide, etc. N Y AGE Age <10? Ages 10 -18? 10 -18 Age > 18? Y Y Chart level of suicide risk 2 and treat as indicated QPRT-P QPRT Chart specific function, and level of suicide risk 2 and treat as indicated Y Y Are there selfinjurious behaviors present? N Conduct FBASpecific function hypothesized/identified? N Default is to treat behavior as suicidal. Chart level of suicide risk 2 and treat as indicated N Chart level of suicide risk 2 and treat as indicated
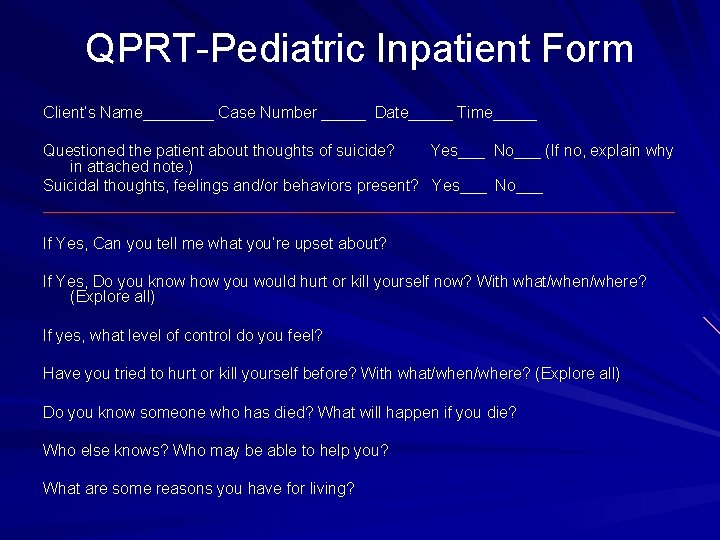
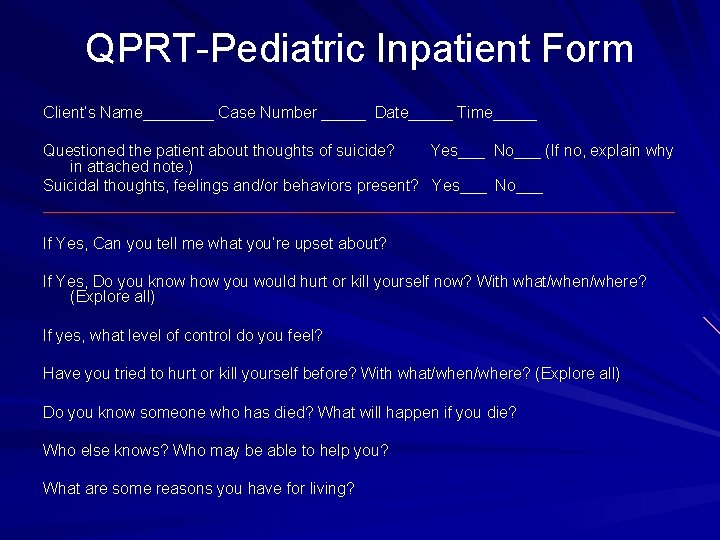
QPRT-Pediatric Inpatient Form Client’s Name____ Case Number _____ Date_____ Time_____ Questioned the patient about thoughts of suicide? Yes___ No___ (If no, explain why in attached note. ) Suicidal thoughts, feelings and/or behaviors present? Yes___ No___ ____________________________________ If Yes, Can you tell me what you’re upset about? If Yes, Do you know how you would hurt or kill yourself now? With what/when/where? (Explore all) If yes, what level of control do you feel? Have you tried to hurt or kill yourself before? With what/when/where? (Explore all) Do you know someone who has died? What will happen if you die? Who else knows? Who may be able to help you? What are some reasons you have for living?
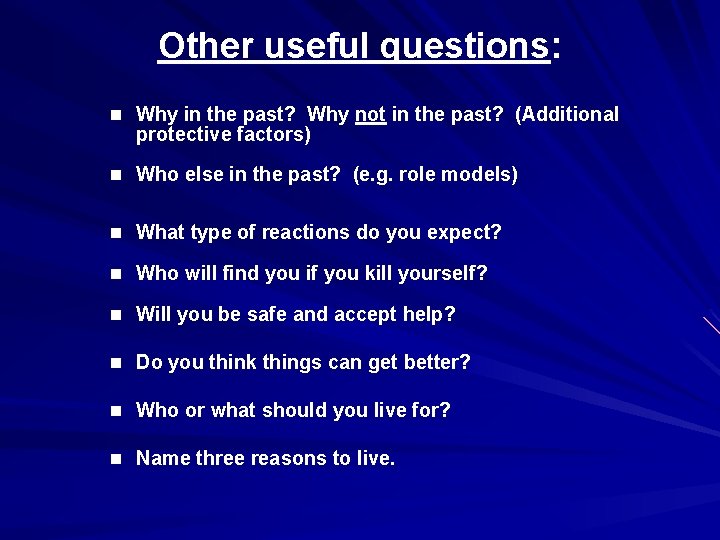
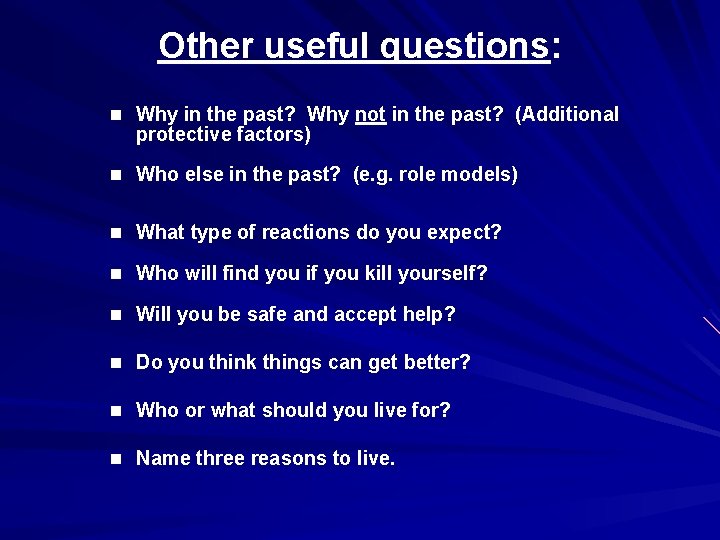
Other useful questions: n Why in the past? Why not in the past? (Additional protective factors) n Who else in the past? (e. g. role models) n What type of reactions do you expect? n Who will find you if you kill yourself? n Will you be safe and accept help? n Do you think things can get better? n Who or what should you live for? n Name three reasons to live.
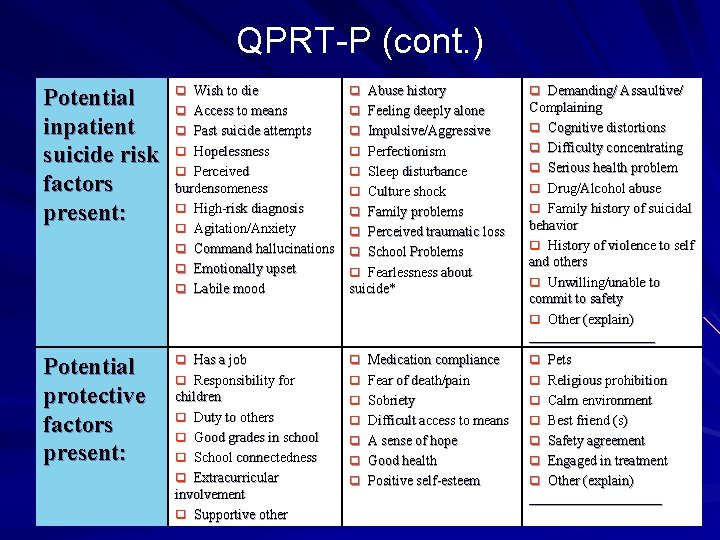
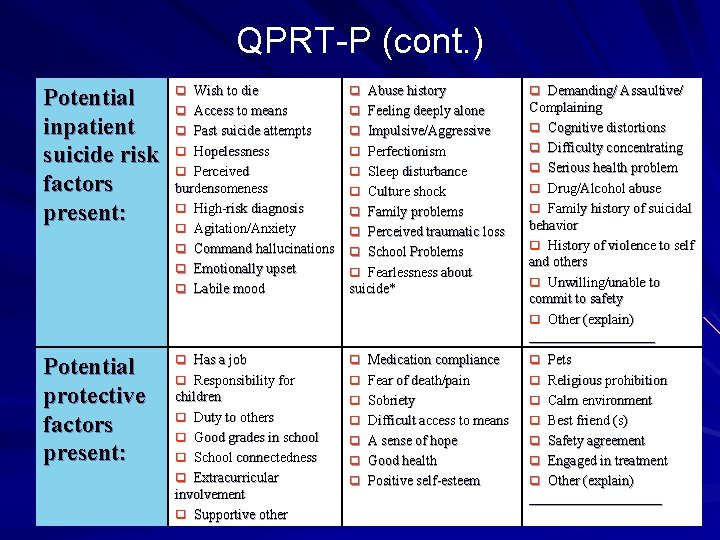
QPRT-P (cont. ) Potential inpatient suicide risk factors present: q Wish to die q Access to means q Abuse history q Feeling deeply alone q q Past suicide attempts Hopelessness q Perceived burdensomeness q High-risk diagnosis q Agitation/Anxiety q Command hallucinations q Emotionally upset q Labile mood q q Potential protective factors present: q Has a job q Responsibility for q Medication compliance q Fear of death/pain q Pets q Religious prohibition children q Duty to others q Good grades in school q School connectedness q Extracurricular involvement q Supportive other q Sobriety q Difficult access to means q Calm environment q Best friend (s) q A sense of hope q Good health q Safety agreement q Engaged in treatment q Positive self-esteem q Other (explain) Impulsive/Aggressive Perfectionism q Sleep disturbance q Culture shock q Family problems q Perceived traumatic loss q School Problems q Fearlessness about suicide* q Demanding/ Assaultive/ Complaining q Cognitive distortions q Difficulty concentrating q Serious health problem q Drug/Alcohol abuse q Family history of suicidal behavior q History of violence to self and others q Unwilling/unable to commit to safety q Other (explain) ___________________

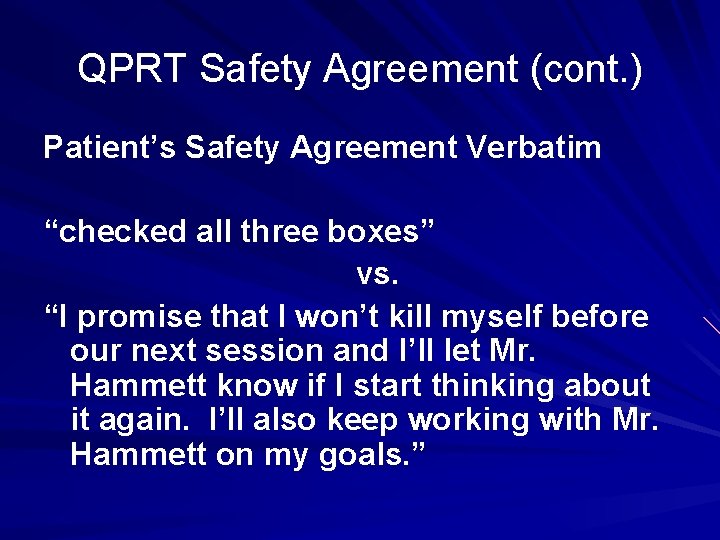
QPRT Safety Agreement. Patient/Family agrees to: 1. Not hurt or kill self accidentally or on purpose. 2. Notify staff of urge to harm/kill self. 3. Agrees to share in the development and implementation of a treatment plan. OR Unwilling/Unable to commit to safety
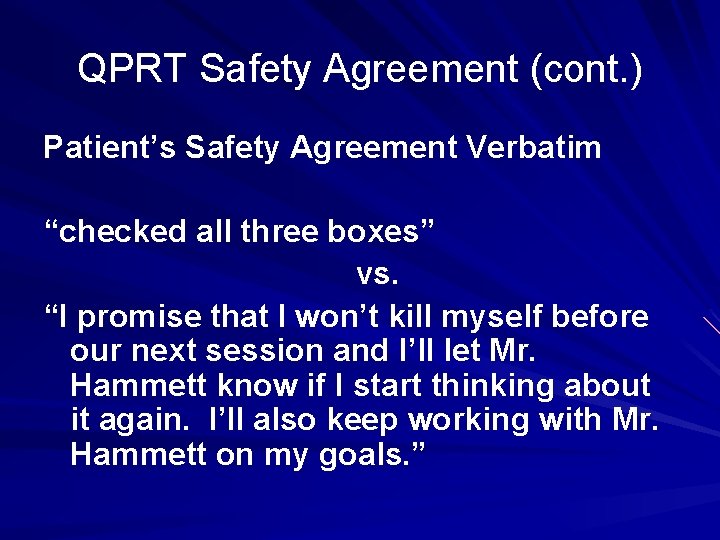
QPRT Safety Agreement (cont. ) Patient’s Safety Agreement Verbatim “checked all three boxes” vs. “I promise that I won’t kill myself before our next session and I’ll let Mr. Hammett know if I start thinking about it again. I’ll also keep working with Mr. Hammett on my goals. ”
The advantages of having a Safety Agreement: Good basic clinical management Clarifies that both you and the client share a common goal Good faith agreement Appeals to the patient’s code of honor May help in prescribing a plan of action Increases the client’s belief that help is available Decreases gatekeeper or provider anxiety Refusal to agree provides important information!
Assigning Level of Risk Based on risk and protective factors and willingness to commit to safety, assign a level of risk. High Moderate Low No Known Risk Document in e. CET Guidelines from New Zealand

Assigning Level of Risk High: – Taking into account current risk and protective factors, it can reasonably be foreseen that this individual is likely to make a suicide attempt in the near future Moderate: – Suicide risk factors are present, yet suicide appear unlikely in the near future. Any significant change in risk or protective factors could result in immediate elevation to high risk Low: – Given current risk and protective factors, a suicide attempt is viewed as unlikely. The client and family actively engage in treatment No Known Risk
Risk Management Plan 1. Assign level of supervision 2. More is not always better 3. Other interventions/precautions 4. Document in e. CET treatment plan

Justification for Risk Management Plan Documentation of your reasoning One of the “twin pillars” of malpractice avoidance. Show that you did a thorough assessment. Be concrete, specific and detailed. Consider protective factors as well as risk factors. If in doubt, over do your documentation.
Consultation with Clinical Team The other “twin pillar” When do we need to consult the most?
Risk rating exercise Compare yourself with other judges Adapted from work done by Steckelmeyer Rate each of the following on a scale of 1 - 7 (1 = no risk; 7 = high risk)
A 39 -year-old white male was referred from the Emergency Room. The patient was in the process of overdosing when he was called by a friend, who arranged for the ambulance to bring the patient to the Crisis Intervention Center (CIC). The patient took 10 or 15 aspirin tablets and 72 over-the-counter sleeping pills. He had written along suicide note bequeathing belongings, expressing guilt about not doing well on his job and feeling hopeless about a “hereditary thinking disorder. ” He feels that no one can help him and suffers from low self-esteem (“I’m a misfit”). Three nights ago he had also made a suicide attempt with Navane and aspirin but woke up by himself in the morning. He lives by himself. There was no obvious immediate precipitant, but the patient’s mother had died six months ago. He is currently in therapy and has a psychiatrist.
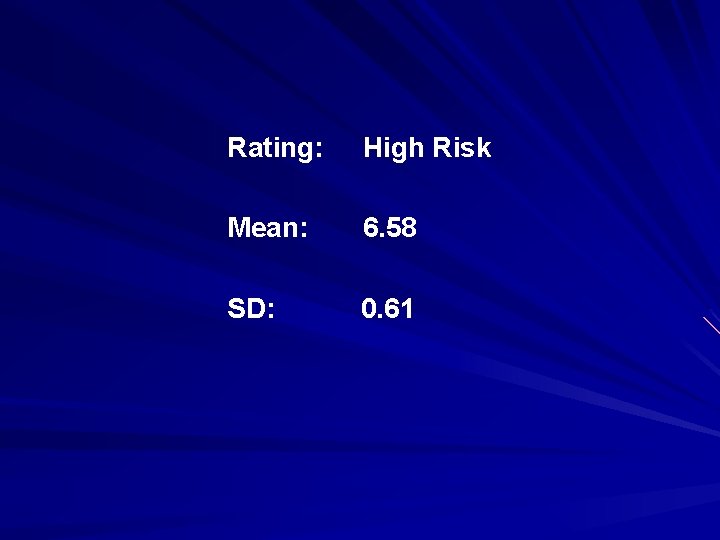
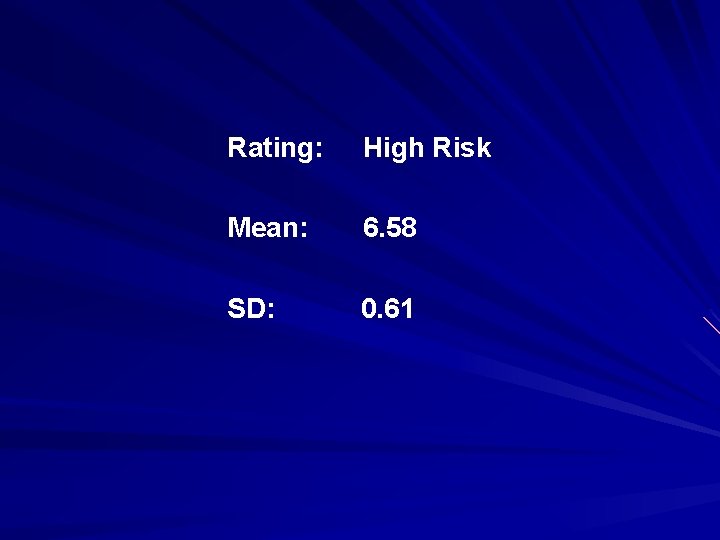
Rating: High Risk Mean: 6. 58 SD: 0. 61
A 16 -year-old Native American female presented as a selfreferral following an overdose of 12 aspirin tablets. Patient reports that she could not tolerate the rumors at school that she and another girl are sharing the same boyfriend. The patient denies being suicidal at this time (“I won’t do it again; I learned my lesson”). She reports that she has always had difficulty expressing her feelings. In the interview she is quiet, guarded and initially quite reluctant to talk.
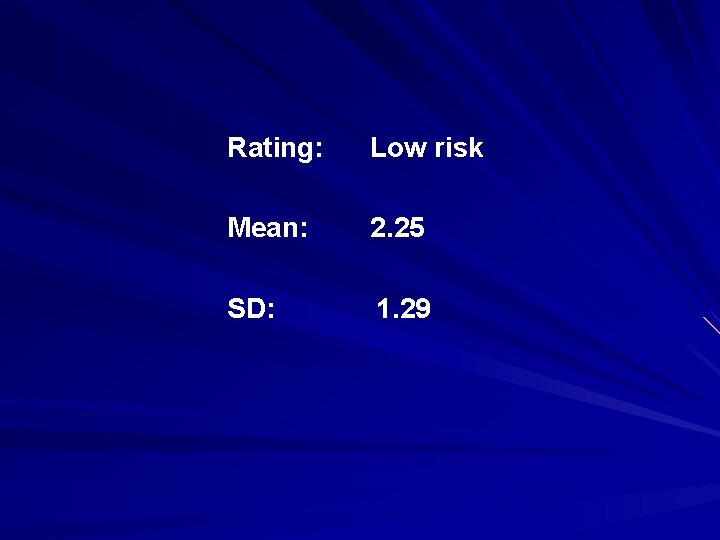
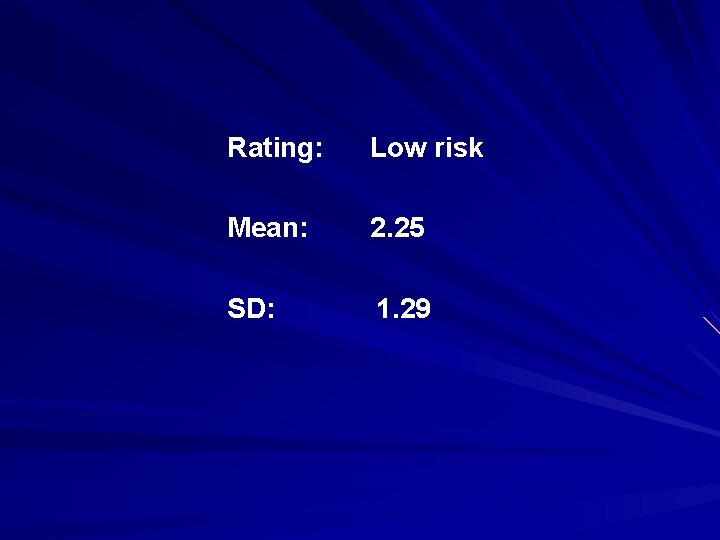
Rating: Low risk Mean: 2. 25 SD: 1. 29
Charting for Low Levels of Risk If client/patient is assessed to be at low or no known risk only, review this section for accuracy and initial here _____. “Client denies desire to hurt or kill himself or herself, and there are no substantial suicide risk factors present. The client is oriented to person, time, and place, sober, non-psychotic, attentive, and cooperative. The client and/or caregiver were advised to inform me or ______ should this change. The client and/or caregiver were assessed to have the capacity to assess the risk and benefits of treatment and/or recommendations for same, and know(s) what to do in the event of worsening distress and the need to seek additional help. ”
QPRT AS A RISK ASSESSMENT TOOL The QPRT is not a substitute for: n A proper diagnostic work-up n A thorough mental status exam n A comprehensive psychological exam n A detailed social or medical history OR n Good clinical judgment QPRT effectiveness depends upon the quality of therapeutic relationship The QPRT inventory can help build rapport, understanding and trust
 Module 4 topic 1 assessing and managing risk
Module 4 topic 1 assessing and managing risk Module 4 topic 1 assessing and managing risk
Module 4 topic 1 assessing and managing risk Assessing risk in sport regulatory bodies
Assessing risk in sport regulatory bodies Market risk credit risk operational risk
Market risk credit risk operational risk Ways to address grammar in the writing classroom ppt
Ways to address grammar in the writing classroom ppt Professional standard strand
Professional standard strand Benefits of informal assessment
Benefits of informal assessment Assessing a new venture's financial strength and viability
Assessing a new venture's financial strength and viability Assessing leadership and measuring its effects
Assessing leadership and measuring its effects Residual risk and secondary risk pmp
Residual risk and secondary risk pmp Business vs financial risk
Business vs financial risk Relative risk calculation
Relative risk calculation Relative risk
Relative risk Unit 18 assessing children's development support needs
Unit 18 assessing children's development support needs Assessing need for hrd
Assessing need for hrd Aashto manual for assessing safety hardware
Aashto manual for assessing safety hardware Chapter 4 cultural dynamics in assessing global markets
Chapter 4 cultural dynamics in assessing global markets Assessing cardiorespiratory fitness
Assessing cardiorespiratory fitness A nine box matrix requires assessing employees on ________.
A nine box matrix requires assessing employees on ________. Methodology for assessing procurement systems
Methodology for assessing procurement systems Core graded high-frequency word survey
Core graded high-frequency word survey Ar = ir x cr x dr
Ar = ir x cr x dr Amc orange county
Amc orange county Chapter 22 assessing health status
Chapter 22 assessing health status Assessing motivation to change
Assessing motivation to change Assessing opportunity cost involves
Assessing opportunity cost involves Hazard communication quiz answers
Hazard communication quiz answers Cultural dynamics in assessing global markets
Cultural dynamics in assessing global markets Assessing value for money
Assessing value for money