AMY KNEHANS MLIS AHIP AKNEHANSHMC PSU EDU Categories

- Slides: 15
AMY KNEHANS, MLIS AHIP AKNEHANS@HMC. PSU. EDU
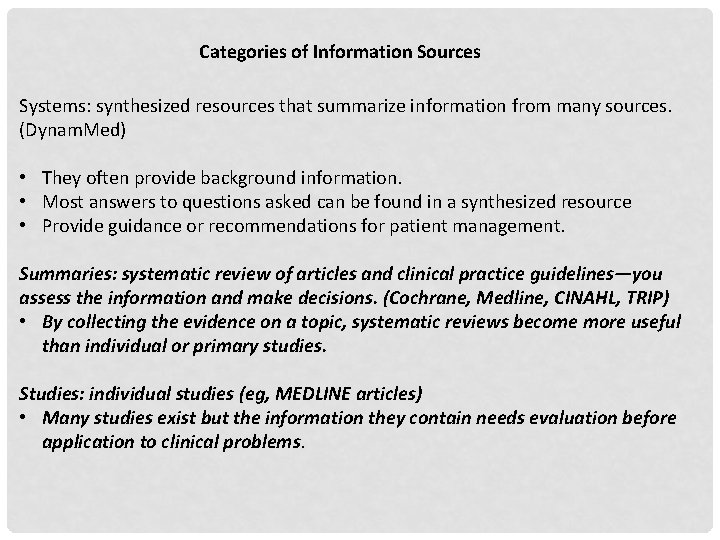
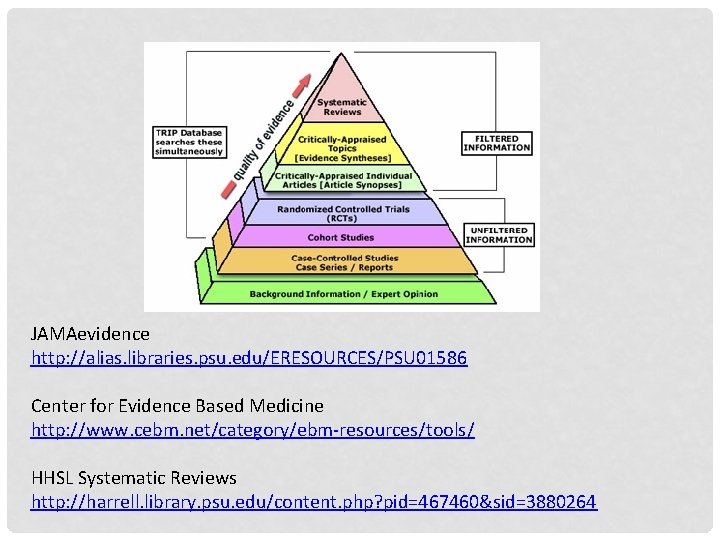
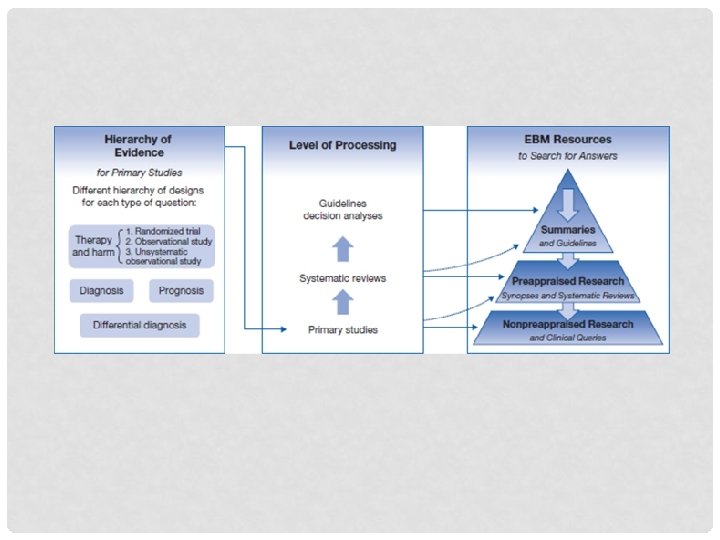
Categories of Information Sources Systems: synthesized resources that summarize information from many sources. (Dynam. Med) • They often provide background information. • Most answers to questions asked can be found in a synthesized resource • Provide guidance or recommendations for patient management. Summaries: systematic review of articles and clinical practice guidelines—you assess the information and make decisions. (Cochrane, Medline, CINAHL, TRIP) • By collecting the evidence on a topic, systematic reviews become more useful than individual or primary studies. Studies: individual studies (eg, MEDLINE articles) • Many studies exist but the information they contain needs evaluation before application to clinical problems.
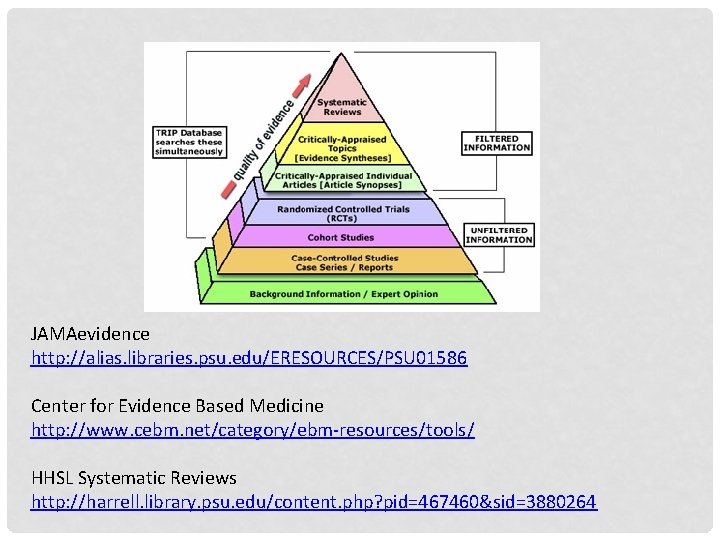
JAMAevidence http: //alias. libraries. psu. edu/ERESOURCES/PSU 01586 Center for Evidence Based Medicine http: //www. cebm. net/category/ebm-resources/tools/ HHSL Systematic Reviews http: //harrell. library. psu. edu/content. php? pid=467460&sid=3880264
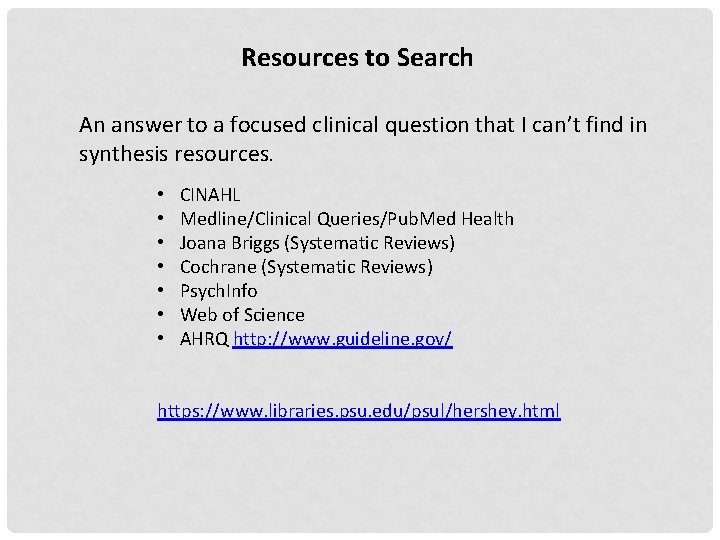
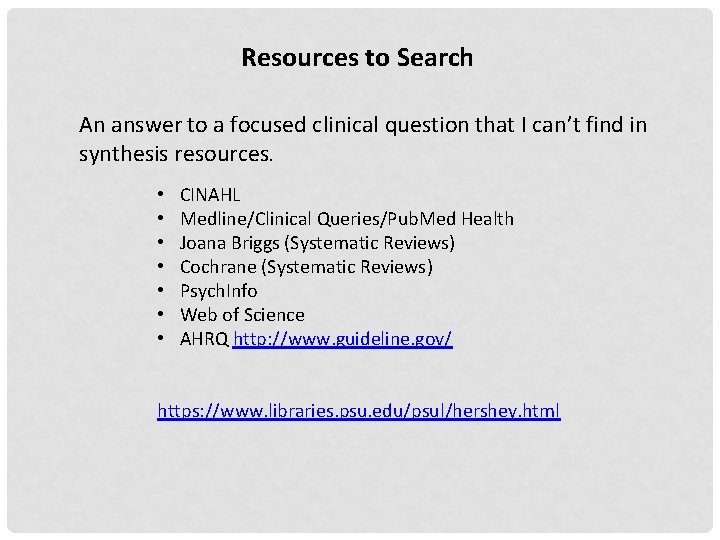
Resources to Search An answer to a focused clinical question that I can’t find in synthesis resources. • • CINAHL Medline/Clinical Queries/Pub. Med Health Joana Briggs (Systematic Reviews) Cochrane (Systematic Reviews) Psych. Info Web of Science AHRQ http: //www. guideline. gov/ https: //www. libraries. psu. edu/psul/hershey. html
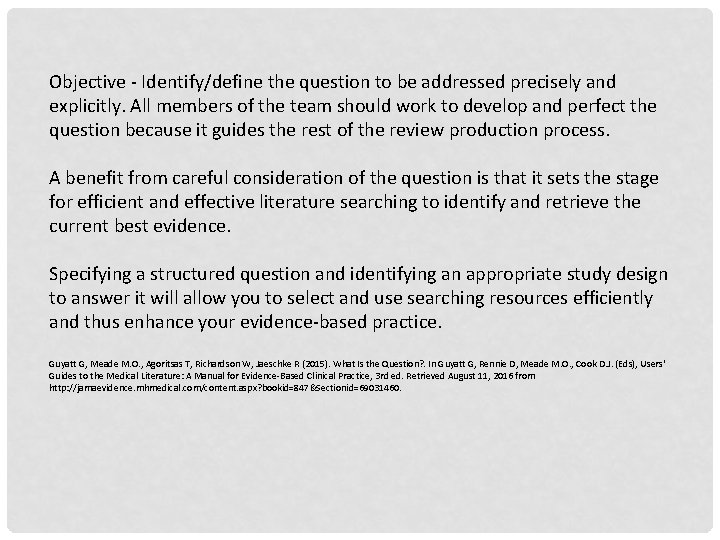
Objective - Identify/define the question to be addressed precisely and explicitly. All members of the team should work to develop and perfect the question because it guides the rest of the review production process. A benefit from careful consideration of the question is that it sets the stage for efficient and effective literature searching to identify and retrieve the current best evidence. Specifying a structured question and identifying an appropriate study design to answer it will allow you to select and use searching resources efficiently and thus enhance your evidence-based practice. Guyatt G, Meade M. O. , Agoritsas T, Richardson W, Jaeschke R (2015). What Is the Question? . In Guyatt G, Rennie D, Meade M. O. , Cook D. J. (Eds), Users' Guides to the Medical Literature: A Manual for Evidence-Based Clinical Practice, 3 rd ed. Retrieved August 11, 2016 from http: //jamaevidence. mhmedical. com/content. aspx? bookid=847&Sectionid=69031460.
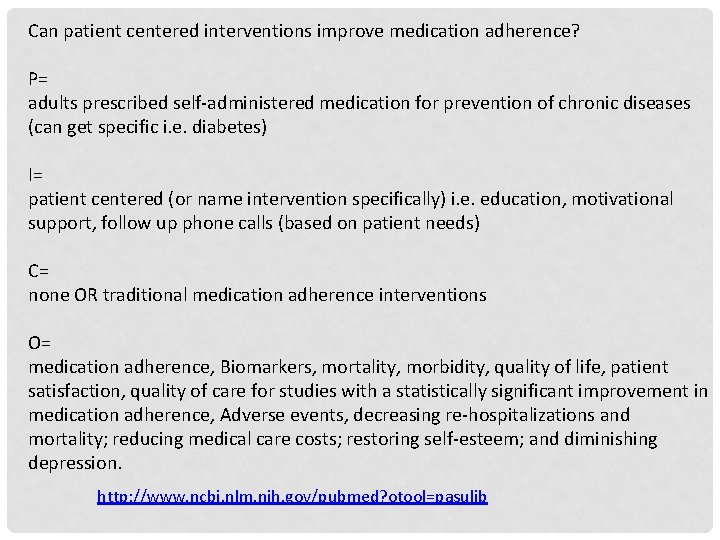
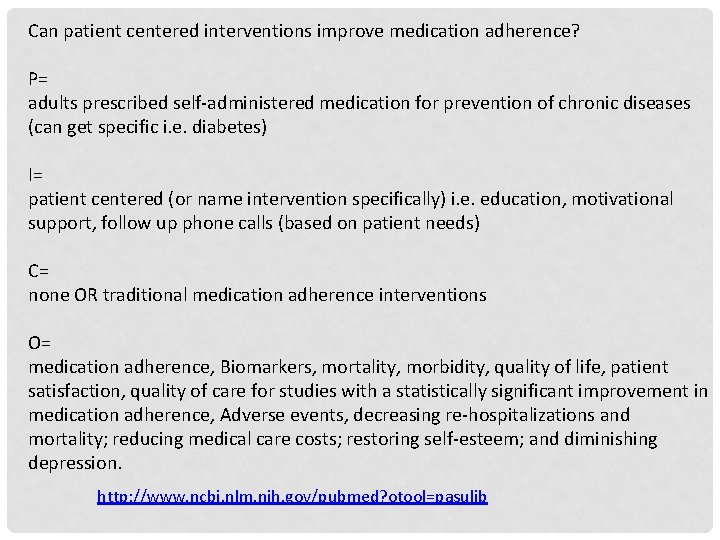
Can patient centered interventions improve medication adherence? P= adults prescribed self-administered medication for prevention of chronic diseases (can get specific i. e. diabetes) I= patient centered (or name intervention specifically) i. e. education, motivational support, follow up phone calls (based on patient needs) C= none OR traditional medication adherence interventions O= medication adherence, Biomarkers, mortality, morbidity, quality of life, patient satisfaction, quality of care for studies with a statistically significant improvement in medication adherence, Adverse events, decreasing re-hospitalizations and mortality; reducing medical care costs; restoring self-esteem; and diminishing depression. http: //www. ncbi. nlm. nih. gov/pubmed? otool=pasulib
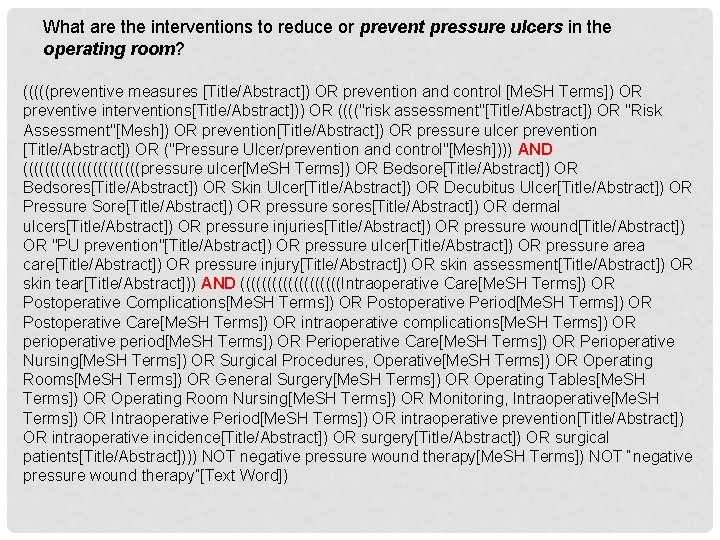
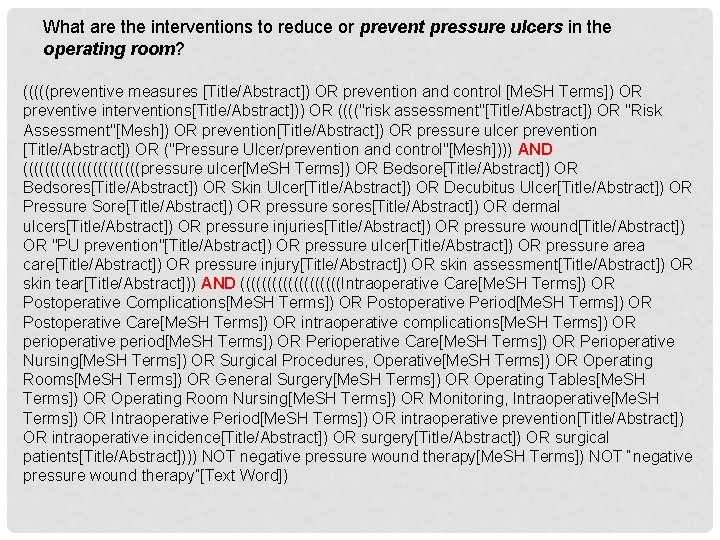
What are the interventions to reduce or prevent pressure ulcers in the operating room? (((((preventive measures [Title/Abstract]) OR prevention and control [Me. SH Terms]) OR preventive interventions[Title/Abstract])) OR (((("risk assessment"[Title/Abstract]) OR "Risk Assessment"[Mesh]) OR prevention[Title/Abstract]) OR pressure ulcer prevention [Title/Abstract]) OR ("Pressure Ulcer/prevention and control"[Mesh]))) AND (((((((((((pressure ulcer[Me. SH Terms]) OR Bedsore[Title/Abstract]) OR Bedsores[Title/Abstract]) OR Skin Ulcer[Title/Abstract]) OR Decubitus Ulcer[Title/Abstract]) OR Pressure Sore[Title/Abstract]) OR pressure sores[Title/Abstract]) OR dermal ulcers[Title/Abstract]) OR pressure injuries[Title/Abstract]) OR pressure wound[Title/Abstract]) OR "PU prevention"[Title/Abstract]) OR pressure ulcer[Title/Abstract]) OR pressure area care[Title/Abstract]) OR pressure injury[Title/Abstract]) OR skin assessment[Title/Abstract]) OR skin tear[Title/Abstract])) AND ((((((((((Intraoperative Care[Me. SH Terms]) OR Postoperative Complications[Me. SH Terms]) OR Postoperative Period[Me. SH Terms]) OR Postoperative Care[Me. SH Terms]) OR intraoperative complications[Me. SH Terms]) OR perioperative period[Me. SH Terms]) OR Perioperative Care[Me. SH Terms]) OR Perioperative Nursing[Me. SH Terms]) OR Surgical Procedures, Operative[Me. SH Terms]) OR Operating Rooms[Me. SH Terms]) OR General Surgery[Me. SH Terms]) OR Operating Tables[Me. SH Terms]) OR Operating Room Nursing[Me. SH Terms]) OR Monitoring, Intraoperative[Me. SH Terms]) OR Intraoperative Period[Me. SH Terms]) OR intraoperative prevention[Title/Abstract]) OR intraoperative incidence[Title/Abstract]) OR surgery[Title/Abstract]) OR surgical patients[Title/Abstract]))) NOT negative pressure wound therapy[Me. SH Terms]) NOT “negative pressure wound therapy”[Text Word])
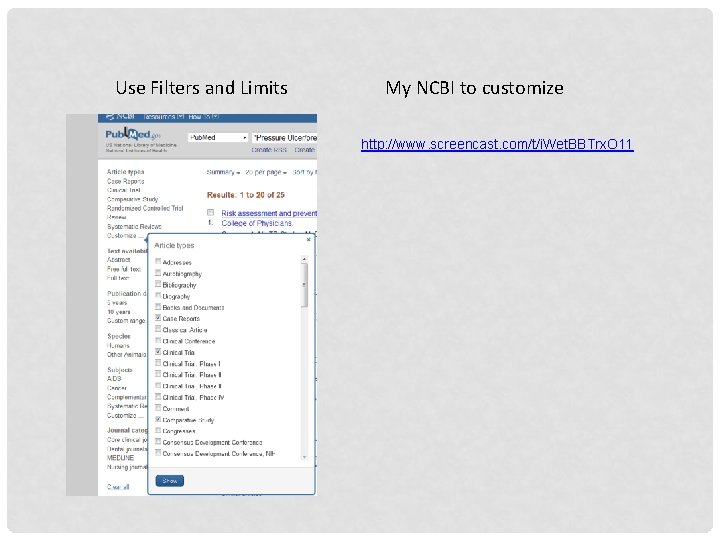
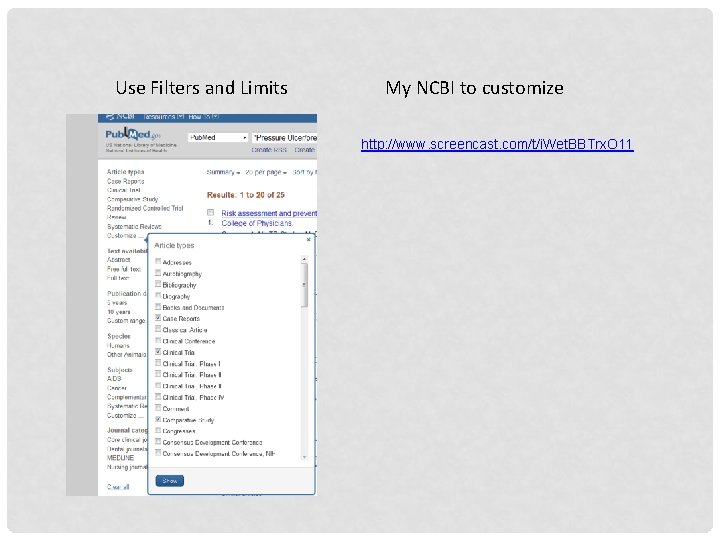
Use Filters and Limits My NCBI to customize http: //www. screencast. com/t/i. Wet. BBTrx. O 11
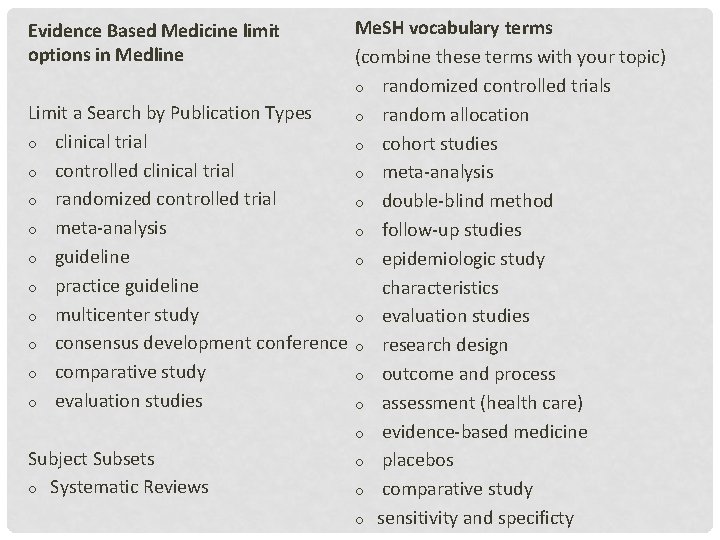
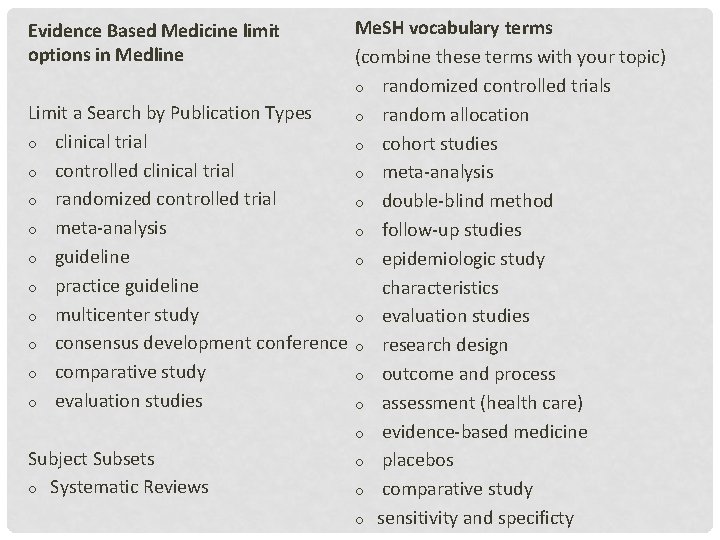
Me. SH vocabulary terms (combine these terms with your topic) o randomized controlled trials Limit a Search by Publication Types o random allocation o clinical trial o cohort studies o controlled clinical trial o meta-analysis o randomized controlled trial o double-blind method o meta-analysis o follow-up studies o guideline o epidemiologic study o practice guideline characteristics o multicenter study o evaluation studies o consensus development conference o research design o comparative study o outcome and process o evaluation studies o assessment (health care) o evidence-based medicine Subject Subsets o placebos o Systematic Reviews o comparative study o sensitivity and specificty Evidence Based Medicine limit options in Medline

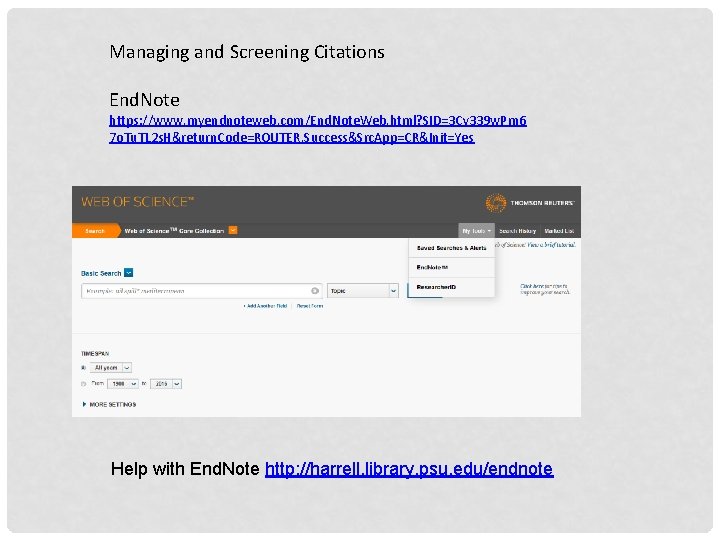
Managing and Screening Citations End. Note https: //www. myendnoteweb. com/End. Note. Web. html? SID=3 Cv 339 w. Pm 6 7 o. Tu. TL 2 s. H&return. Code=ROUTER. Success&Src. App=CR&Init=Yes Help with End. Note http: //harrell. library. psu. edu/endnote
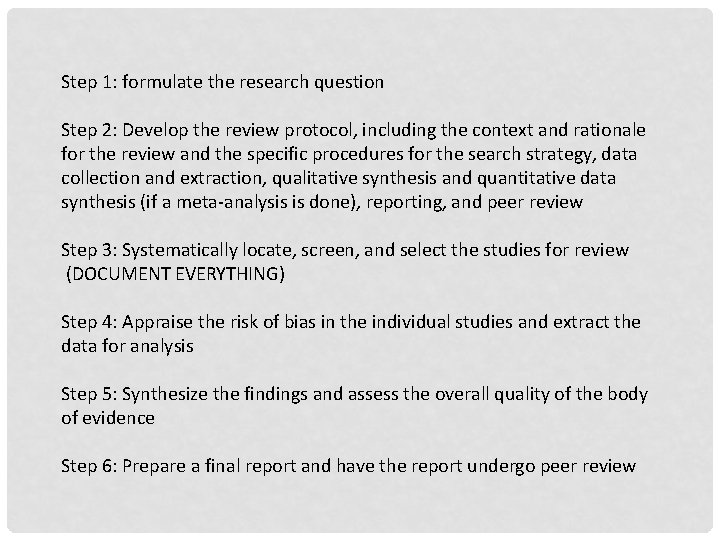
Step 1: formulate the research question Step 2: Develop the review protocol, including the context and rationale for the review and the specific procedures for the search strategy, data collection and extraction, qualitative synthesis and quantitative data synthesis (if a meta-analysis is done), reporting, and peer review Step 3: Systematically locate, screen, and select the studies for review (DOCUMENT EVERYTHING) Step 4: Appraise the risk of bias in the individual studies and extract the data for analysis Step 5: Synthesize the findings and assess the overall quality of the body of evidence Step 6: Prepare a final report and have the report undergo peer review
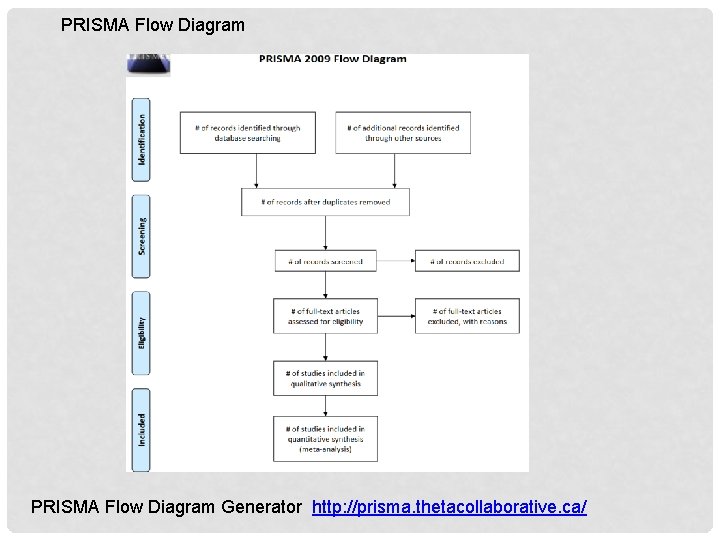
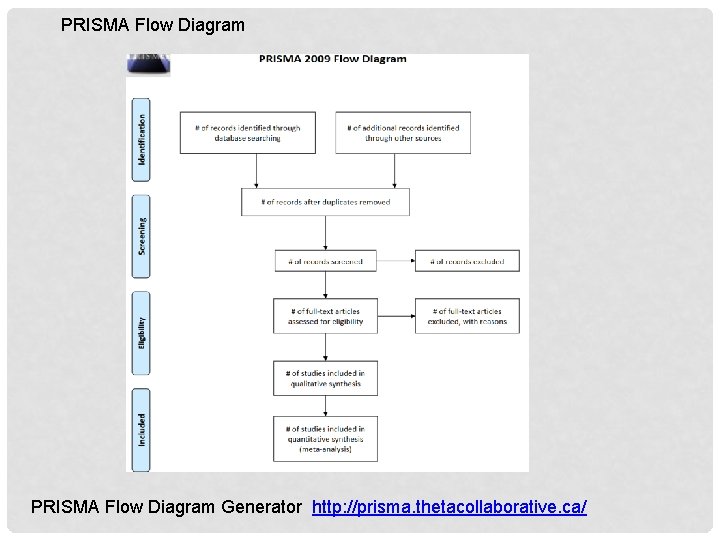
PRISMA Flow Diagram Generator http: //prisma. thetacollaborative. ca/
1. Does RN bedside report improve patient outcomes compared to traditional report outside of the room in hospitalized patients? 2. Will a comprehensive discharge planning and after hospital care intervention reduce readmissions within 30 days? 3. How can organizations raise awareness of nurse work-arounds of unsafe practices? 4. What is the Impact of nurses' uniforms on patient and family perceptions of nurse professionalism? 5. Does hand washing among healthcare workers reduce hospital acquired infections? 6. What is the best available evidence regarding the effectiveness of acute in-hospital falls prevention strategies for adult patients? 7. What are the interventions to reduce or prevent pressure ulcers in the operating room? 8. What is the impact of Early Term Birth (37 0/7 weeks of gestation through 38 6/7 weeks of gestation), on discharge planning and readmission rates? 9. Among patients with ventricular assist devices does a dressing change protocol using a chlorhexidine gluconate impregnated sponge dressing compared to the standard dressing change protocol affect the number of driveline exit site infections?
 Humana ahip medicare training portal
Humana ahip medicare training portal Academic search premier rutgers
Academic search premier rutgers Iva en canada 2018
Iva en canada 2018 Lrn psu training
Lrn psu training Opp.psu.edu timecard
Opp.psu.edu timecard Turnitin.psu
Turnitin.psu Personal.psu
Personal.psu Edu.sharif.edu
Edu.sharif.edu Meteo 3 psu
Meteo 3 psu Huntkey pc case
Huntkey pc case E builder psu
E builder psu Universitas xxi usach
Universitas xxi usach Psu cramer hall
Psu cramer hall Penn state activity insight
Penn state activity insight Forest resources building
Forest resources building Apartments near waupelani drive state college pa
Apartments near waupelani drive state college pa