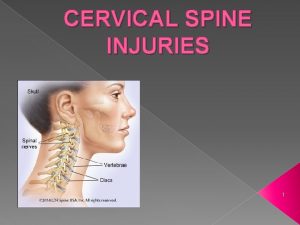
Airway management for patients with cervical spine disorders

- Slides: 19
Airway management for patients with cervical spine disorders Presented by R 3 吳佳展
Case presentation • 30 year-old man • Hyperextension injury • C 4 -5 HIVD • Muscle power: lower extremities 1, upper 3 • HR, BP, vital capacity within normal range • Intubated with light wand under general • anesthesia No neurological deterioration after surgery
Trauma patients • Pathology of cervical spine • Stability • Preoperative neurological deficits • Airway patency • Respiratory function • Cardiovascular compromise • Full stomach
Trauma patients • Other associated injuries • Facial injury: interfere with mask ventilation • 1~2% of trauma patients have cervical spine • • injury 10% of high-risk patients (head-first fall, high speed motor vehicle accidents) Stabilization makes intubation more difficult
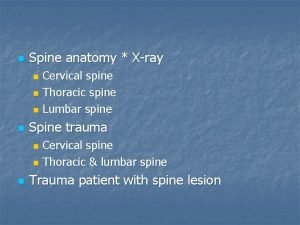
evaluation • Neck pain or tenderness: only valid in alert patients without other painful lesions • Neurological examination • Plain films: lateral, AP, open mouth. Sensitivity~90% • CT scan • MRI
Airway management • No guidelines in this area • Awake or under general anesthesia • Nasal or oral • Blind, larygoscope, fiberoptic bronchoscope, • Bullard scope, Combitube, light wand, LMA, Fastrach, gum elastic bougie, Wu’s scope Surgical airway: tracheostomy, cricothyroitomy
Factors determining methods used • Urgency: most rapid and secure method is preferred • Experience of anesthesiologist • Patients’ cooperation • Airway anatomy • Mechanism of injury: flexion, extension
“standard” • Oral laryngoscope with manual in-line stablization • Blind nasal intubation in awake patients • Nasal fiberoptic intubation
Comparison between methods • Outcome • Radiological study: normal patients, with cervical spine pathology but without instability, cadaver • Upper or lower cervical spine injury
Outcome study • No difference between awake or GA, nasal or oral intubation (retrospective) • few studies comparing other airway management methods based on outcome, possibly because they are not widely used
Effect of airway maneuver • Cadaver study • Unstable C 5 -C 6: chin lift=jaw thrust=oral intubation>nasal intubation in spine movement • Unstable C 1 -C 2: space available for spinal cord oral=nasal>chin lift and jaw thrust
Bullard vs. Macintosh • Patients requiring GA with normal cervical spine • Measured with c-arm • Extension: BUL with ILS (in-line stabilization)< BUL=MAC with ILS<MAC • Intubation time: in reversed order
No neck motion? • Blind nasal • Nasal fiberoptic intubation: may cause the least movement compared other conventional methods • Trachlight • Fastrach • Combitube
Fastrach • Patients with cervical pathology (metastasis, disc prolapse, OPLL) • With light wand guide • Flexion and posterior displacement C 0~C 5
Fastrach • Cadaver • Pressure sensor placed at C 2 -3 • Control: nasal/oral, laryngoscope/ fiberscope • Fastrach produces greater pressure against cervical spine and greater posterior displacement
Fastrach vs. laryngoscope • Flexion vs. extension • Fastrach used in extension injury? • Laryngoscope used in flexion injury?
Trachlight vs. Fastrach Patients with cervical spine pathology Higher success rate at first attempt Less time required No data about cervical spine movement was provided
Thanks for your attention

Thanks for your attention
 Epiglottic
Epiglottic Cervical spine reflexology
Cervical spine reflexology Nursing diagnosis for undescended testis
Nursing diagnosis for undescended testis Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Indikasi intubasi
Indikasi intubasi Chapter 10 airway management
Chapter 10 airway management Supraglotal
Supraglotal Chapter 9 airway management
Chapter 9 airway management Basic airway management equipment
Basic airway management equipment Sandwich manuver adalah
Sandwich manuver adalah Stepwise airway management
Stepwise airway management Lippincott williams & wilkins
Lippincott williams & wilkins Management of patients with neurologic trauma
Management of patients with neurologic trauma Periodontal treatment of medically compromised patients
Periodontal treatment of medically compromised patients Nursing management of sleep disorders
Nursing management of sleep disorders Borborygmi
Borborygmi Lemon moans airway
Lemon moans airway 5 functions of the respiratory system
5 functions of the respiratory system External respiration
External respiration Respiratory airway secretary
Respiratory airway secretary