Advance Care Planning What do you plan to



- Slides: 42
Advance Care Planning “What do you plan to do with your one wild and precious life? Mary Oliver Chris Ward
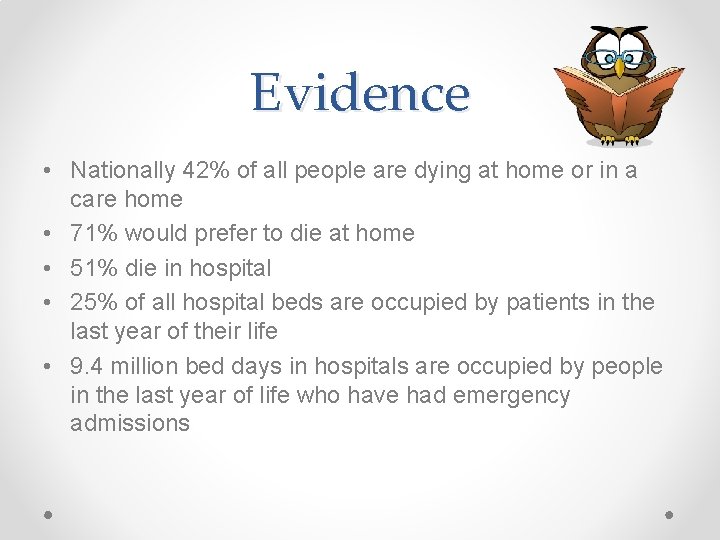
Evidence • Nationally 42% of all people are dying at home or in a care home • 71% would prefer to die at home • 51% die in hospital • 25% of all hospital beds are occupied by patients in the last year of their life • 9. 4 million bed days in hospitals are occupied by people in the last year of life who have had emergency admissions
“ACP is a voluntary process of discussion and review to help an individual who has capacity to anticipate how their condition may affect them in the future and , if they wish, set on record choices about their care and treatment in specific circumstances, so that these can be referred to by those responsible for their care or treatment in the event they loose capacity to decide once their illness progresses”.

• 52% reduction in hospitalised admissions/length of stay • Increased DNACPR status from 8 to 71% • Increase in explicit decision making in care homes from 4% to 55% • Reduction in residents dying in acute hospitals from the previous year (Hockley et al 2010) • Preplanning encourages deeper conversations at an important time (Detering 2010)
http: //www. youtube. com/watch? v=b. Yy 4 q 8 R 9 kro
• Advance care planning should be accessible for patients, as a choice, not a ‘must do’ • Timely introduction • Advance care planning is a process in supporting patient preference and not a tick box exercise • Lack of educational support and/or time provision for education • Place of care and death preferences important • Will highlight patient concerns part of holistic care • Documentation and sharing vital
www. theclinicalnetwork. org Deciding right An integrated approach to making care decisions in advance with children, young people and adults
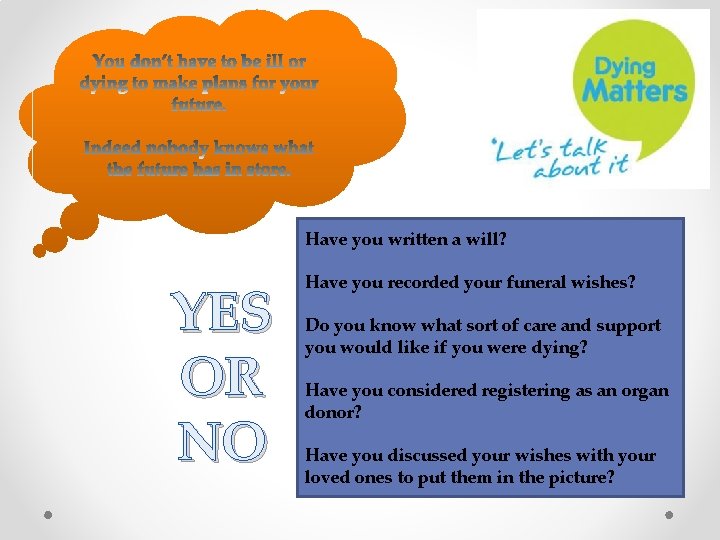
Have you written a will? YES OR NO Have you recorded your funeral wishes? Do you know what sort of care and support you would like if you were dying? Have you considered registering as an organ donor? Have you discussed your wishes with your loved ones to put them in the picture?
How did you score? Score 0 – 1 Its time to get some plans in place Score 2 – 3 Not bad, still a little way to go. Score 4 – 5 Fabulous, but remember to update your plans if things change.

Deciding right - a new north east initiative for making care decisions in advance
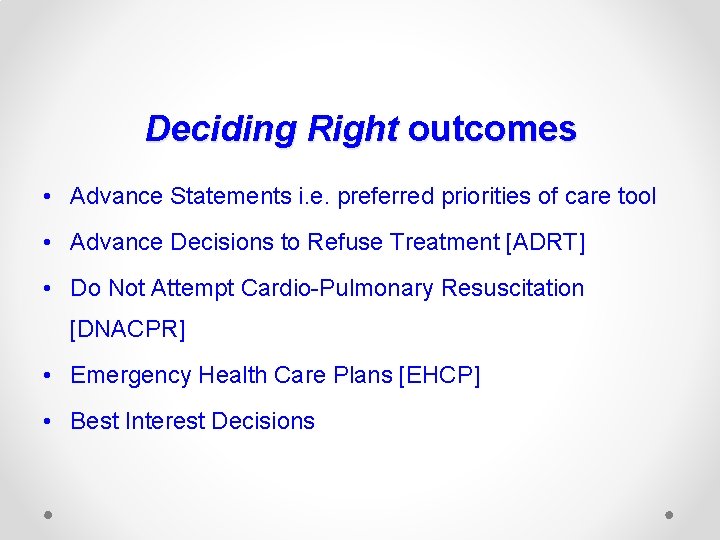
Deciding Right outcomes • Advance Statements i. e. preferred priorities of care tool • Advance Decisions to Refuse Treatment [ADRT] • Do Not Attempt Cardio-Pulmonary Resuscitation [DNACPR] • Emergency Health Care Plans [EHCP] • Best Interest Decisions
Outcomes of ACP Advance Statement this can be verbal or written and must be made when the individual has capacity for those care decisions. It is a record of an individual’s wishes and feelings, beliefs and values. It is not legally binding, but once the individual loses capacity for those care decisions all carers are legally bound to take it into account when making decisions in the patient’s best interests.
Outcomes of ACP cont… Advance Decision to Refuse Treatment (ADRT) this can be verbal or written, but must be written to refuse life-sustaining treatment. It must be made when the individual has capacity for those care decisions. It is legally binding on all carers if it is valid and applicable to the situation Some patients choose not to make a formal document, but may agree to setting limits on their treatment in an Emergency Health Care Plan or a Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) order.
Outcomes of ACP cont… • Lasting Power of Attorney (LPA) this is a legal authority made by a patient when they have capacity to nominate another person to make decisions on their behalf should the patient lose capacity in the future. A Property and Affairs LPA has no authority to make health care decisions; these can only be made by a personal welfare LPA (also known as a Health & welfare LPA) who must have specific authorisation in the order if the patient wishes them to make life-sustaining decisions.
Outcomes of ACP cont… Emergency Health Care Plans This is a document that makes communication easier in the event of a healthcare emergency for infants, children, young people and adults (i. e. . any individual) with complex healthcare needs, so that they can have the right treatment, as promptly as possible and with the right experts involved in their care. EHCPs make up for the deficiencies of singledecision DNACPR forms.
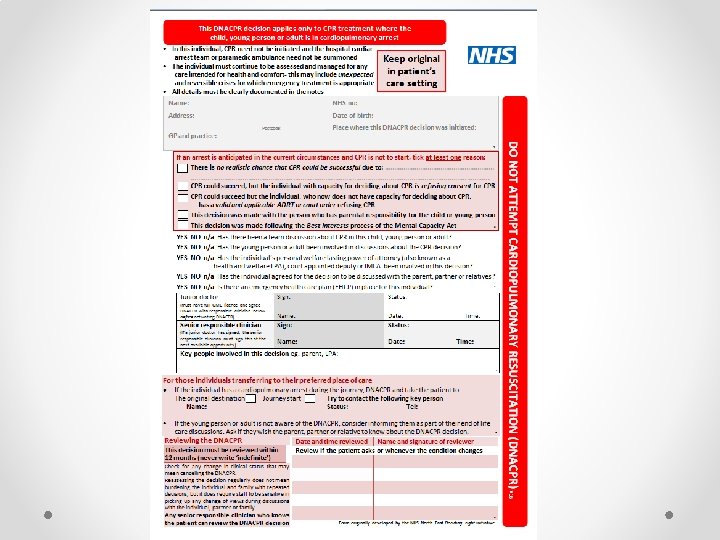
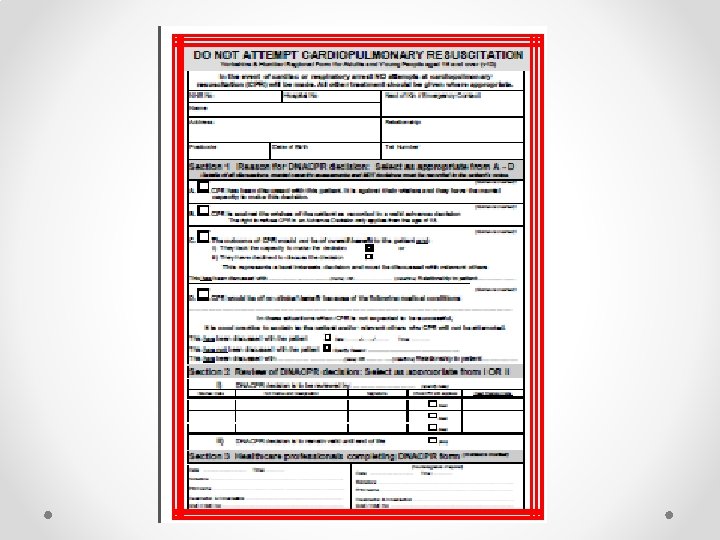
Outcomes of ACP • Do Not Attempt Cardiopulmonary resuscitation (DNACPR) A written, valid and applicable advance decision to refuse treatment (ADRT) is legally binding but, if CPR is being refused, a DNACPR is also needed. DNACPR forms are advisory only. A DNACPR document decision can be overridden if it is clear that an unexpected event could be successfully treated with CPR. A single DNACPR document should be used across the region When individuals cross boundaries into different settings, their DNACPR form should be recognised and accepted by all health care professionals in all settings.
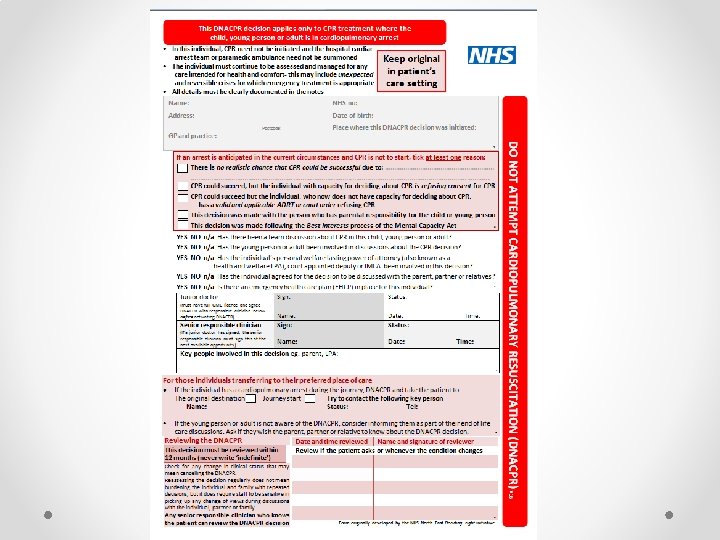
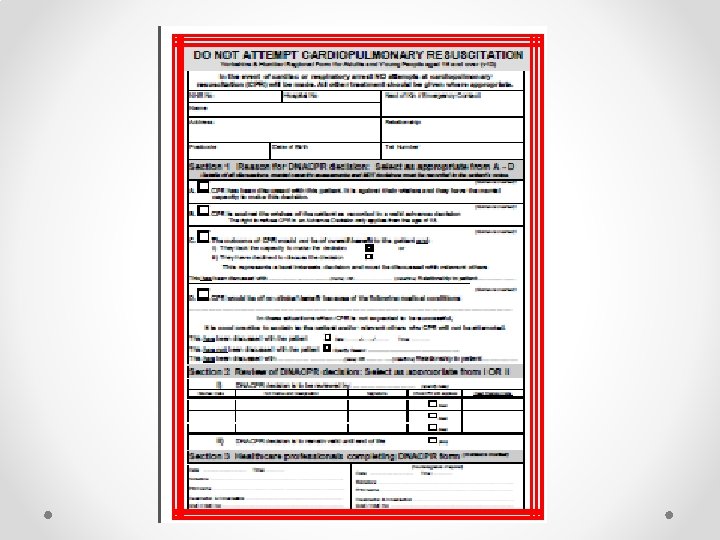
Yorkshire Ambulance Services will recognise the North East DNACPR forms in use by the Trust upon transfer of patients from Trust services based within Yorkshire or if they are called to a patient’s home and one is in place. Patients transferred home with a North East DNACPR form will need it to be converted to a Yorkshire and Humber form by the appropriate community staff as soon as practicable.
Outcomes of ACP Best Interest Decision • Any act done for, or any decision made on behalf of a person who lacks capacity must be done, or made, in that person’s best interests. To do this, it is recommended to use the checklist from Deciding Right. • The intention is not to decide for the individual, but to estimate what decision they would have made if they still had capacity for this decision.
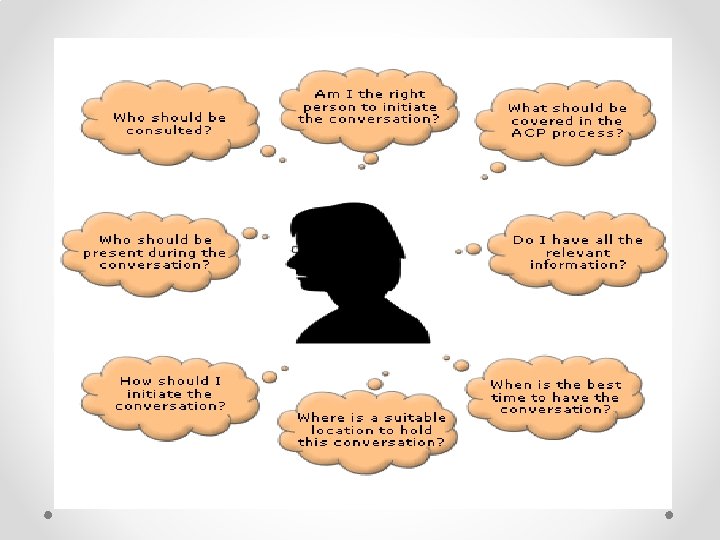
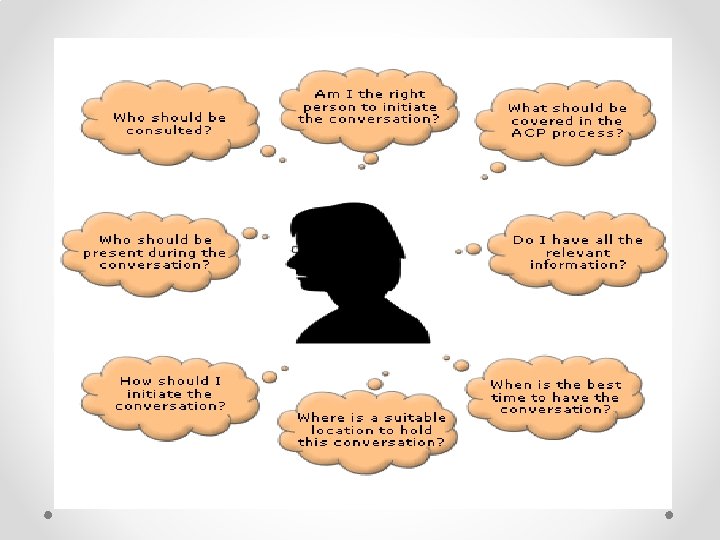
Initiation of an ACP discussion • The discussion should be introduced sensitively • The process is voluntary • Staff must be skilled practitioners • Realistic account of choices to be given • Families and carers may be part of the discussion if the patient wishes
Direct cues Indirect Cues

• What do you see happening with your illness over the next few months? • It is important that you think about any preferences that you may have, so we can discuss these and perhaps help you make decisions. • It would be good to discuss what kind of medical care you would want if you should get sick again. How do you feel about talking about this? • It is important that you think about any preferences that you may have, so we can discuss these and perhaps help you make decisions.
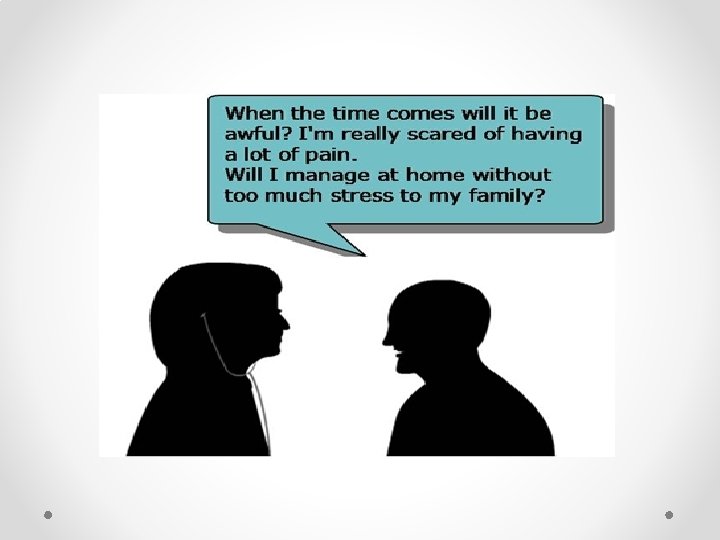
Sensitive discussions • Within the assessment look for cues which will enable you to explore end of life issues ‘ As we were talking you mentioned the fact that you knew things were getting worse…’ • Use those cues to help empathise, negotiate to ask about the patient’s wishes and priorities It seems as if things are hard for you. Is it OK if I ask you more about that? • If no cues are given about end of life, ask about their views of the future You have told me about your current difficulties and we clearly need to address those, but before we do, is it OK if I ask you how you see things going in the future? • Acknowledge, empathise and clarify the elements which are unclear • Take time and this can be a work in progress • Go prepared with information to leave for the patient to read
How might I know if timing is wrong…. • When the patient is symptomatic. They will be unable to focus and may feel the future is more short term • If the patient is angry or upset. They may lack concentration and the ability to think about the future • If the patient has not been informed of their situation or if they lack information. Therefore the need to plan ahead has never been considered • If the patient and/or their family are in denial • The patient is not in denial but is simply not ready to think about, or plan for, the future
Non verbal cues that the timing isn't right…. • A patient can demonstrate that they are uncomfortable with the conversation by using non-verbal cues. For example: • Using body posture to indicate they are less open to communication e. g. folding arms, turning away from you • Becoming fidgety e. g. tapping foot, fiddling with fingers or blanket etc. • Changing facial expression e. g. looking glazed, tearful or frowning • Removing eye contact by looking away or down at lap • Showing signs of heightened emotion e. g. with flushed face, tears or gritted teeth
General inability to complete the conversation • Watch for signs that the person is overwhelmed or confused by the conversation. • Discuss your observations with the carer or colleague. • Decide whether any action needs to be taken to improve the patient's ability to participate in this conversation, e. g. alleviating symptoms, clarifying doubts, answering questions and giving the patient more time and space to think things over.
Tiredness • Ask the patient at appropriate intervals how they are feeling. Discuss your observations and check if they wish to continue the conversation. If the patient has slower speech or drooping eyelids, this can indicate that the patient is tired or fatigued. Offer to come back later and agree when that should be.
Benefits of ACP • For the patient the unknown can be scary, reduces anxiety, addresses loss of control, decide what they want and when, relax when choices fulfilled, encourages dialogue with family and professionals, receive care that the patient wants • Easier for those left behind • Reduces unnecessary hospital admissions, increases DNACPR decisions, reduces crises • Empowers and enables patient and family • Family, carers don’t know everything about the person, promotes important discussions, help avoid anxiety and disagreement about decisions, better bereavement outcomes, can help to carry out wishes • Health professionals better job satisfaction support a good death • Good communication and sharing of information is the key to success
It can be hard for us too…
Suggested on going learning and support ……. Network website http: //www. nescn. nhs. uk/common-themes/deciding-right/ CLIP Worksheets http: //www. stoswaldsuk. org/how-we-help/weeducate/resources/current-learning-in-palliative-care-(clip)/clipworkshops-adult-version. aspx Download the App
Thank you and any questions?