Acne vulgaris Dr Anwar Issa hasan 15112018 Acne







- Slides: 23
Acne vulgaris Dr. Anwar Issa hasan 15/11/2018
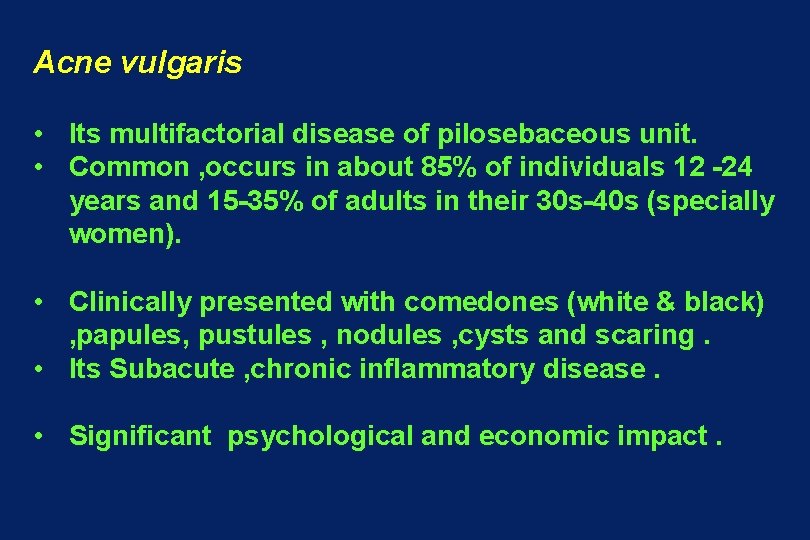
Acne vulgaris • Its multifactorial disease of pilosebaceous unit. • Common , occurs in about 85% of individuals 12 -24 years and 15 -35% of adults in their 30 s-40 s (specially women). • Clinically presented with comedones (white & black) , papules, pustules , nodules , cysts and scaring. • Its Subacute , chronic inflammatory disease. • Significant psychological and economic impact.

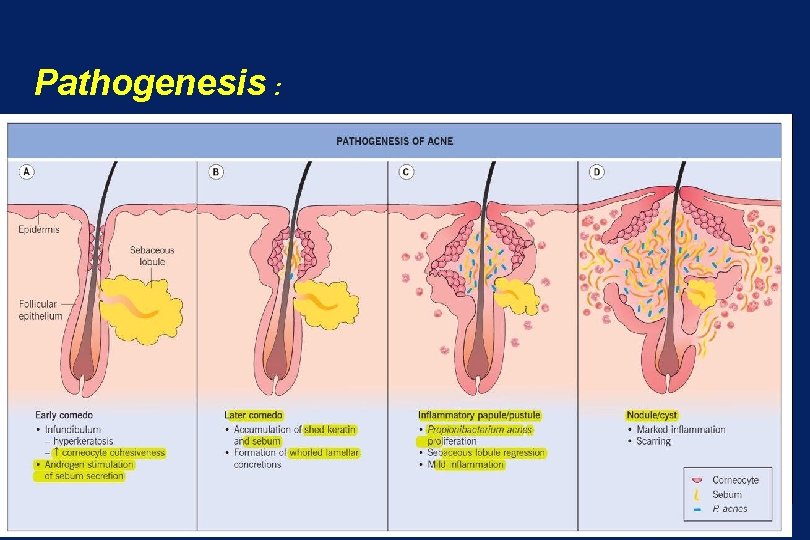
pathogenesis 1. Genetic: the number, size, activity of sebaceous gland are inherited, also sever nodulocystic acne runs in families. 2. Sebum production : increase sebum production due to hormonal factor(androgens) is contributing factor. 3. Comedo formation: 1 st step in acne formation is follicular hyperkeratosis at upper part of hair follicles. (previously) 4. Inflammatory response: early in acne prone sites show increase in number of CD 4 T lymphocytes & IL 1 increase perifollicularly and cause hyperkeratosis. 5. Propionibacterium acne : grame +ve , anaerobic bacterial flora increase in the number & release lipases witch induce inflammatory response.
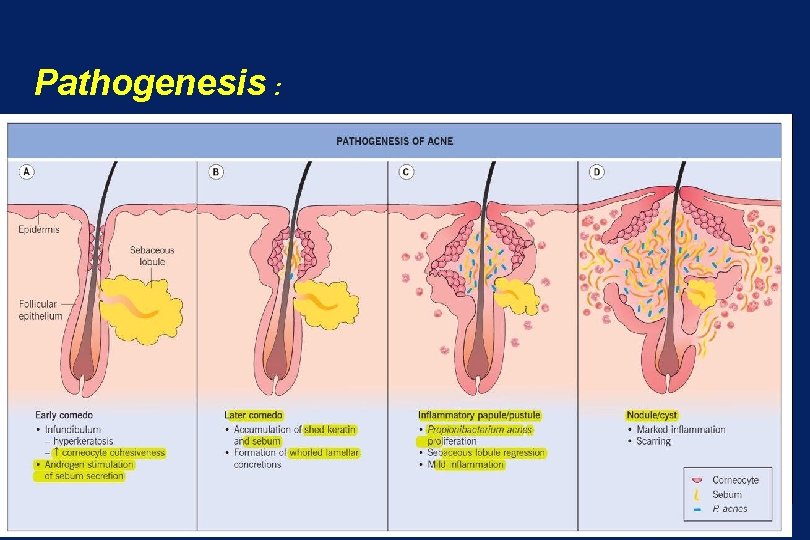
Pathogenesis :
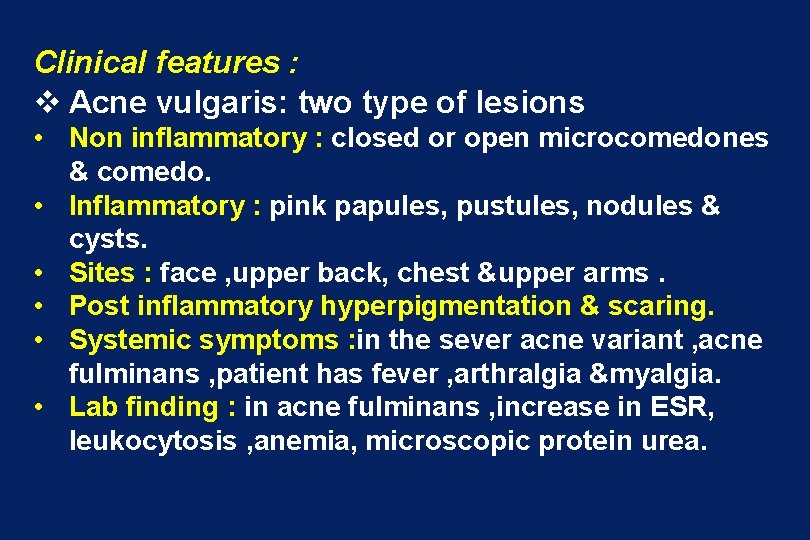
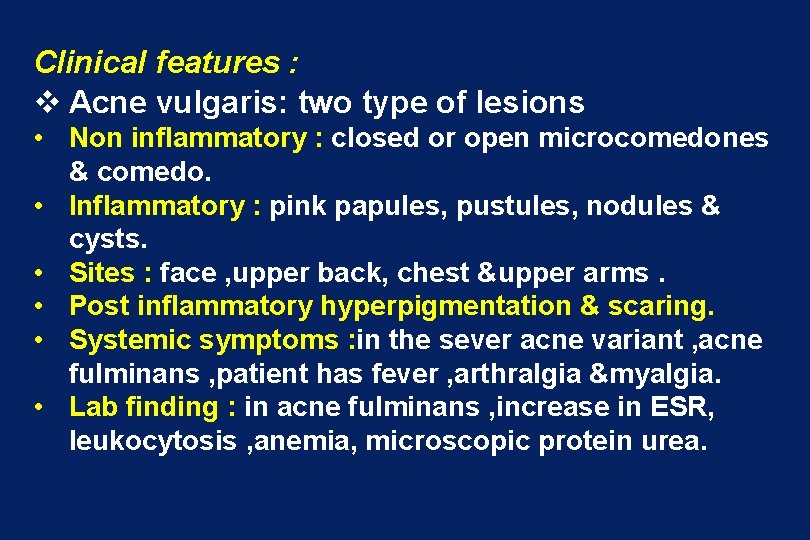
Clinical features : v Acne vulgaris: two type of lesions • Non inflammatory : closed or open microcomedones & comedo. • Inflammatory : pink papules, pustules, nodules & cysts. • Sites : face , upper back, chest &upper arms. • Post inflammatory hyperpigmentation & scaring. • Systemic symptoms : in the sever acne variant , acne fulminans , patient has fever , arthralgia &myalgia. • Lab finding : in acne fulminans , increase in ESR, leukocytosis , anemia, microscopic protein urea.
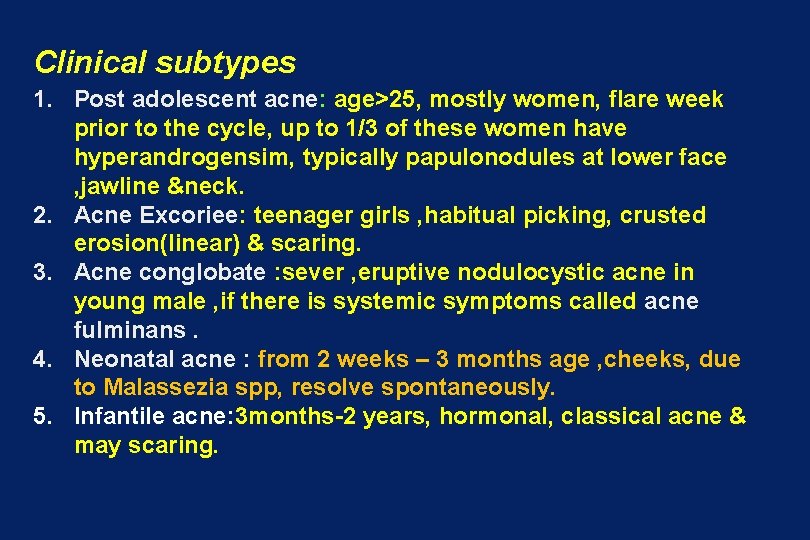
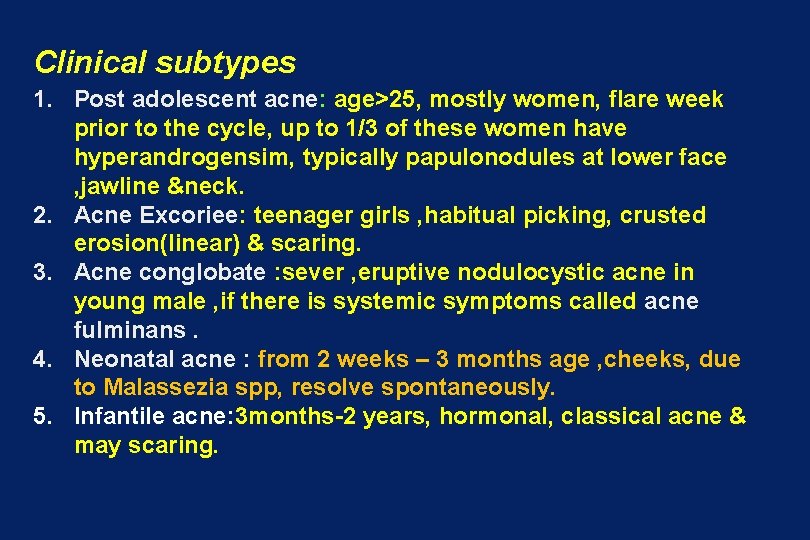
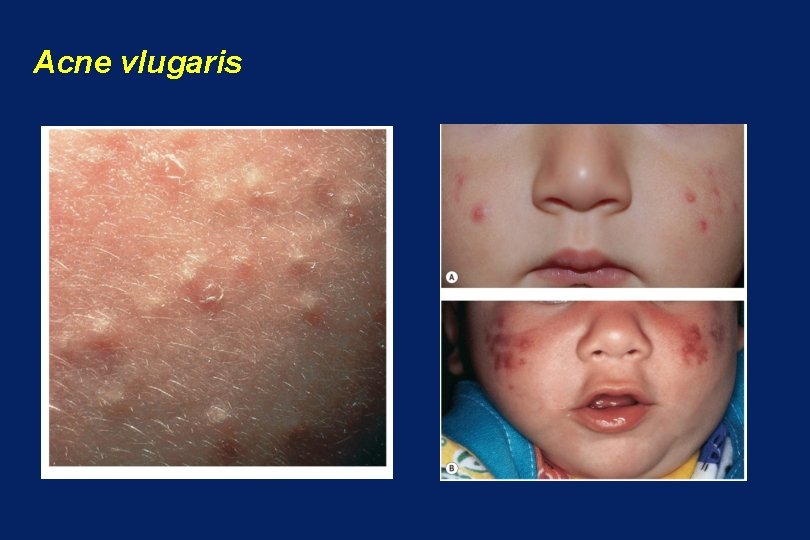
Clinical subtypes 1. Post adolescent acne: age>25, mostly women, flare week prior to the cycle, up to 1/3 of these women have hyperandrogensim, typically papulonodules at lower face , jawline &neck. 2. Acne Excoriee: teenager girls , habitual picking, crusted erosion(linear) & scaring. 3. Acne conglobate : sever , eruptive nodulocystic acne in young male , if there is systemic symptoms called acne fulminans. 4. Neonatal acne : from 2 weeks – 3 months age , cheeks, due to Malassezia spp, resolve spontaneously. 5. Infantile acne: 3 months-2 years, hormonal, classical acne & may scaring.
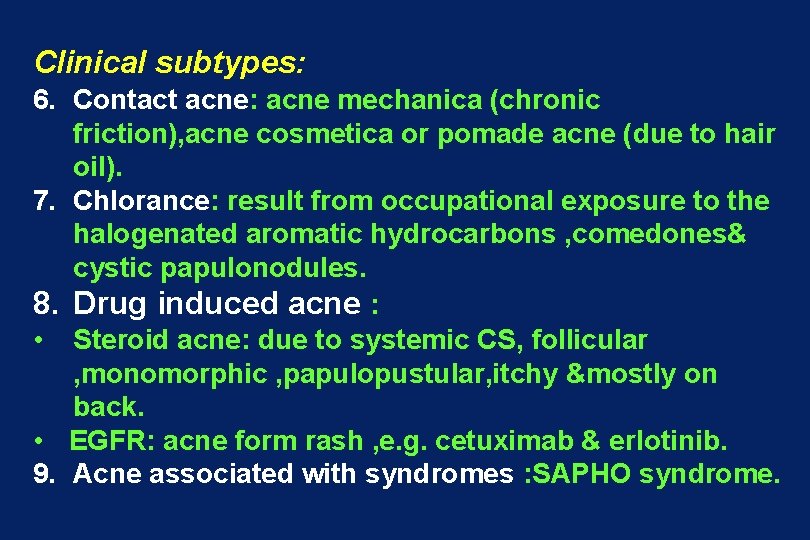
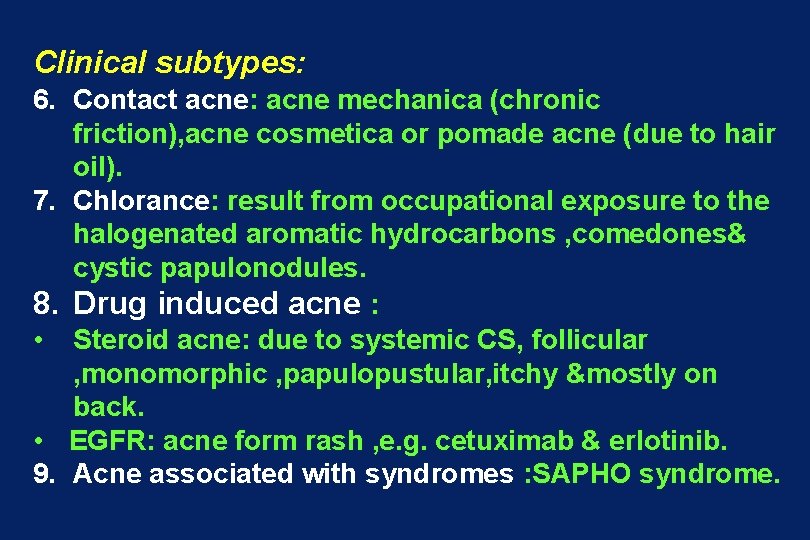
Clinical subtypes: 6. Contact acne: acne mechanica (chronic friction), acne cosmetica or pomade acne (due to hair oil). 7. Chlorance: result from occupational exposure to the halogenated aromatic hydrocarbons , comedones& cystic papulonodules. 8. Drug induced acne : • Steroid acne: due to systemic CS, follicular , monomorphic , papulopustular, itchy &mostly on back. • EGFR: acne form rash , e. g. cetuximab & erlotinib. 9. Acne associated with syndromes : SAPHO syndrome.

clinical variant of acne

Acne vulgaris
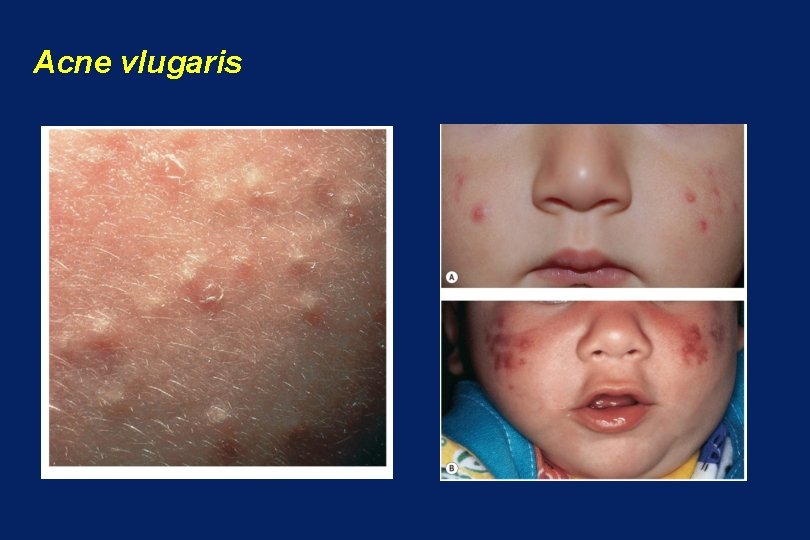
Acne vlugaris
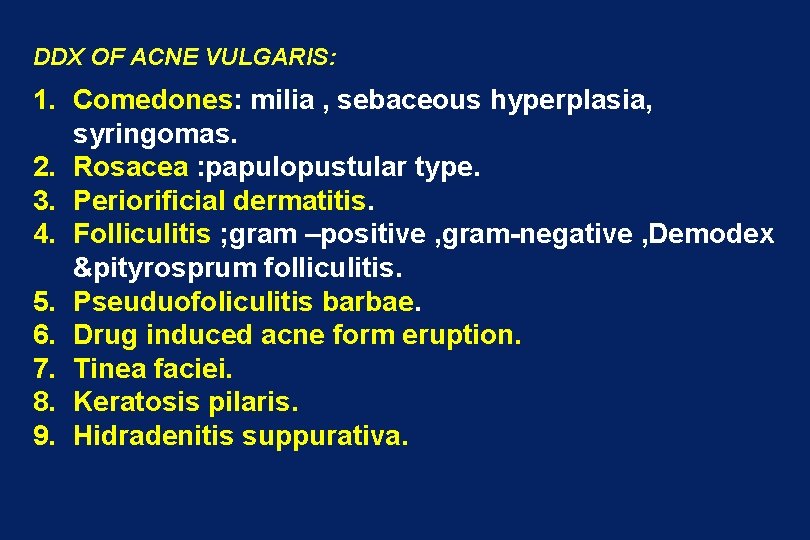
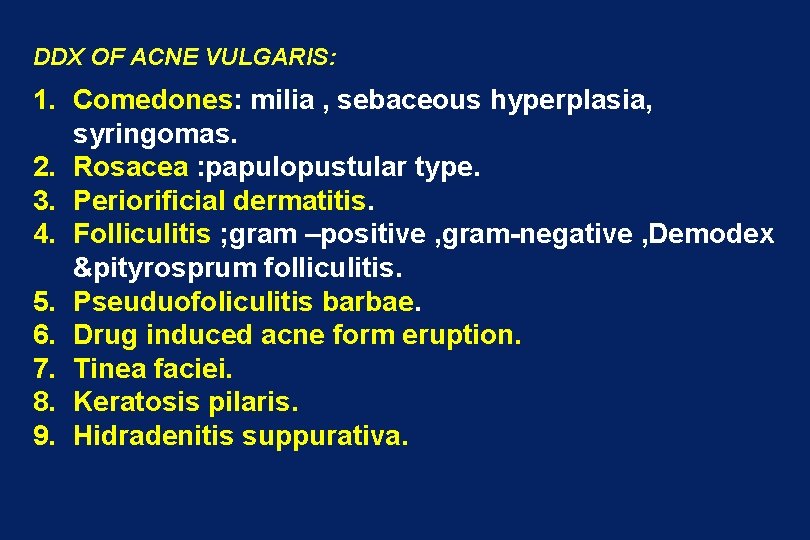
DDX OF ACNE VULGARIS: 1. Comedones: milia , sebaceous hyperplasia, syringomas. 2. Rosacea : papulopustular type. 3. Periorificial dermatitis. 4. Folliculitis ; gram –positive , gram-negative , Demodex &pityrosprum folliculitis. 5. Pseuduofoliculitis barbae. 6. Drug induced acne form eruption. 7. Tinea faciei. 8. Keratosis pilaris. 9. Hidradenitis suppurativa.
Management of acne: Avoidance: oily make up , sunblock's , pomade , harsh soap, psychological stress & skim milk. 1. Topical retinoid ; comedolytic>anti-inflammatory effects, tretinion, adapalene &tazorotene • Initial response 3 -4 weeks , use small amount & treat all acne prone areas. • Causes irritation, so use small amount in alternate night. 1. Topical antimicrobials: benzoyl peroxide and/or antibiotic(clindamycin , erythromycin). 2. Oral antibiotic: 1 st line tetracycline(Doxycycline , minocycline), alt e. g. azithromycin, trimethoprimsulfamethoxazole for 3 -6 months.
Management of acne 3. OCPs: for hormonal acne e. g. Estrostep( ethinyl estradiol 20/30/35 Microgram, norethindrone 1000 Mg) , for 6 months &up to 2 years. 4. Anti androgens: spironolactone 50 -200 mg. 5. Oral isotretinion: systemic retiniods, 0. 5 -1 mg/kg for 4 -6 months. 6. Treatment of acne &scaring : chemical peels, physical treatment e. g. , laser, lights IPL, microneedling radiofrequency.

Treatment of acne Sebum production • • • P. acnes ➢ Hormonal therapy ➢ Antibiotics ➢ Sebum correction ➢ Benzoyl peroxide ➢ isotretinoin ➢ Isotretinoin Follicular hyperkeratinization • Inflammation ➢ Topical retinoids ➢ Antibiotics ➢ Topical tazarotene ➢ Benzoyl peroxide (receptor selective) ➢ Hormonal therapy Isotretinoin ➢
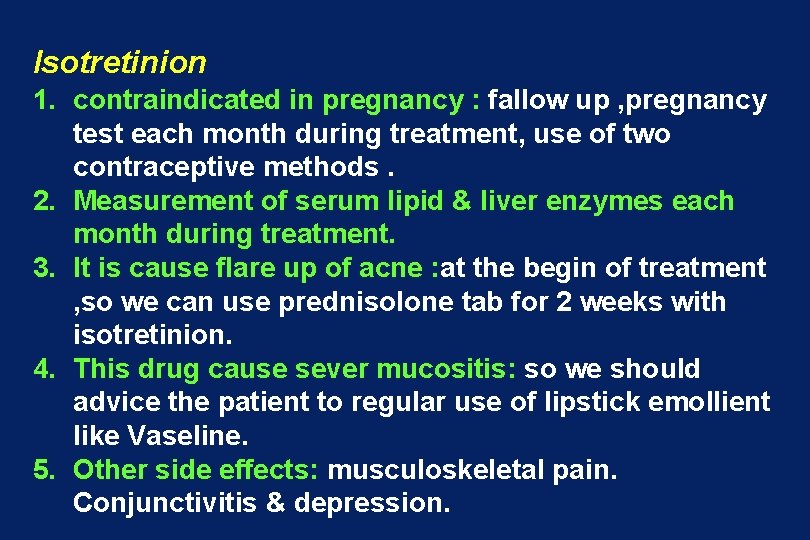
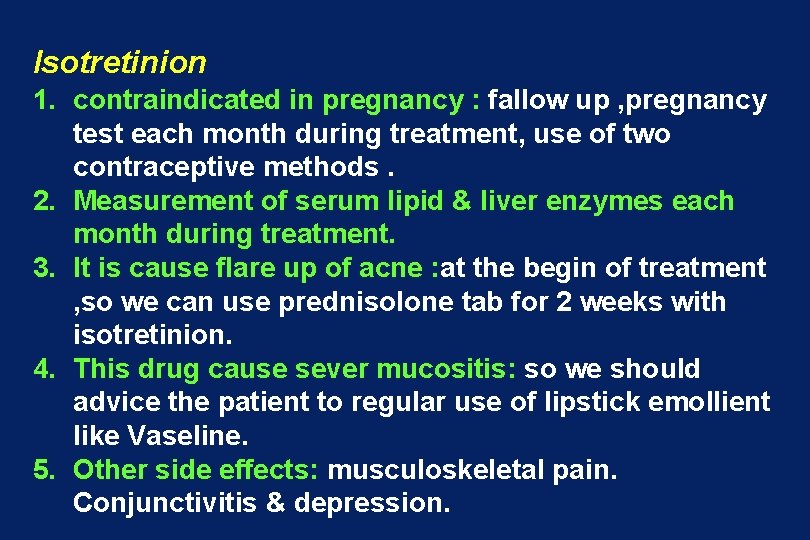
Isotretinion 1. contraindicated in pregnancy : fallow up , pregnancy test each month during treatment, use of two contraceptive methods. 2. Measurement of serum lipid & liver enzymes each month during treatment. 3. It is cause flare up of acne : at the begin of treatment , so we can use prednisolone tab for 2 weeks with isotretinion. 4. This drug cause sever mucositis: so we should advice the patient to regular use of lipstick emollient like Vaseline. 5. Other side effects: musculoskeletal pain. Conjunctivitis & depression.
Rosacea • its chronic, vascular inflammatory disorder, usually limited to the center of face and characterized by recurrent flushing, persistent erythema, telangiectasia, papules and pustules. • Age between 30 -50 years. • Sex: more in females& more in white peoples.
Rosacea Etiology and exacerbating factors • • GIT disturbances. Reaction to the follicular mite, Demodex follilculorum. Climatic (sun). Vasomotor instability. Psychic factors. Role of helicobacter pylori. Rosacea has been reported as a manifestation of HIV infection.
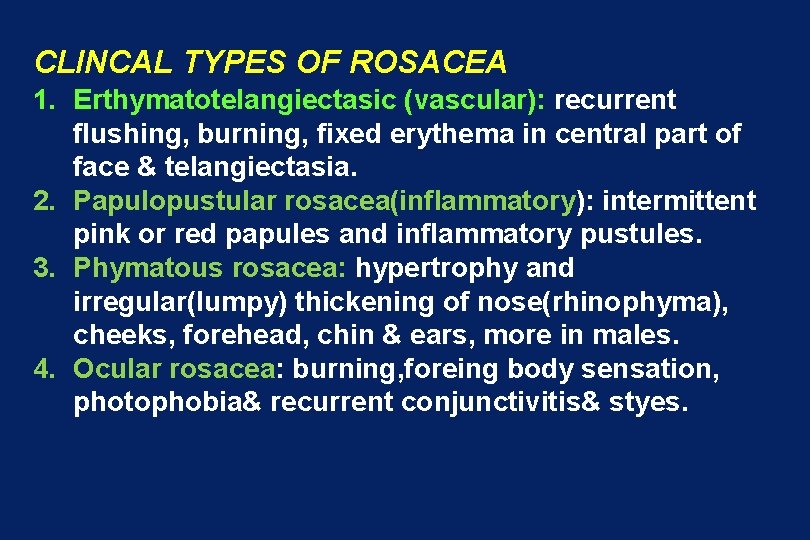
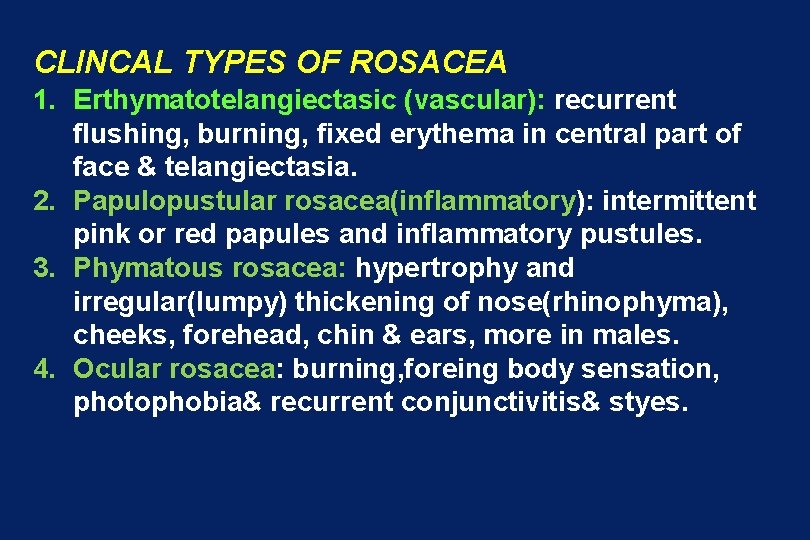
CLINCAL TYPES OF ROSACEA 1. Erthymatotelangiectasic (vascular): recurrent flushing, burning, fixed erythema in central part of face & telangiectasia. 2. Papulopustular rosacea(inflammatory): intermittent pink or red papules and inflammatory pustules. 3. Phymatous rosacea: hypertrophy and irregular(lumpy) thickening of nose(rhinophyma), cheeks, forehead, chin & ears, more in males. 4. Ocular rosacea: burning, foreing body sensation, photophobia& recurrent conjunctivitis& styes.


Rosacea

Rosacea Treatment Avoid extremes of heat & cold, excessive sunlight, spices, hot liquids & alcohols. I) Systemic treatment • Tetracyclines: 250 mg 3 times daily. • Metronidazole (Flagyl®) 200 mg twice daily. • Isotretinion.
Rosacea - Treatment (Cont’d) II) Topically • Bland emollient • Anti-acne agents • Topical metronidazole 0. 75% gel (Metrogel) III)Plastic surgery for rhinophyma&co 2 laser.
Thank you
 Acne vulgaris histology
Acne vulgaris histology Carotenmia
Carotenmia Equine large intestine
Equine large intestine Strongylus vulgaris patogenia
Strongylus vulgaris patogenia Strongylus vulgaris
Strongylus vulgaris Matchstick sign lupus vulgaris
Matchstick sign lupus vulgaris Hydnora plant
Hydnora plant Pemfigus vulgaris büllöz pemfigoid farkı
Pemfigus vulgaris büllöz pemfigoid farkı Pemphigus vulgaris
Pemphigus vulgaris Pemphigus vulgaris vs bullous pemphigoid
Pemphigus vulgaris vs bullous pemphigoid Faba vulgaris
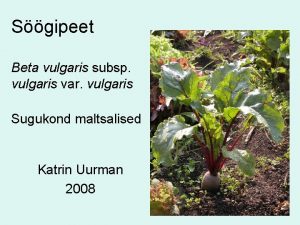
Faba vulgaris Nitrate reduction test for pseudomonas aeruginosa
Nitrate reduction test for pseudomonas aeruginosa Knops salt solution
Knops salt solution Pemphigus vulgaris tombstone
Pemphigus vulgaris tombstone Free verse poem examples for students
Free verse poem examples for students Issa raleigh
Issa raleigh Issa tb 109
Issa tb 109 Issa ottawa
Issa ottawa Ghassan issa
Ghassan issa Amanda issa
Amanda issa Rmf process
Rmf process Dr nabil khouri
Dr nabil khouri Issa associates degree
Issa associates degree Notre dame opt
Notre dame opt