Xlinked and mitochondrial inheritance pattern Dr Eva Masiero


- Slides: 42
X-linked and mitochondrial inheritance pattern Dr Eva Masiero 4 th Feb 2020
Learning objectives • Review of the phenomenon of X-inactivation (Lyonisation) • Describe the inheritance characteristics of a X-linked disorder • Draw out a Punnett square to show the inheritance pattern of X-linked disorder • Give examples of X-linked conditions and their clinical symptoms
Learning objectives • Understand the inheritance of disorders where the disease gene is on the mitochondrial genome • Give examples of disorders demonstrating these phenomena
X-linked disorders
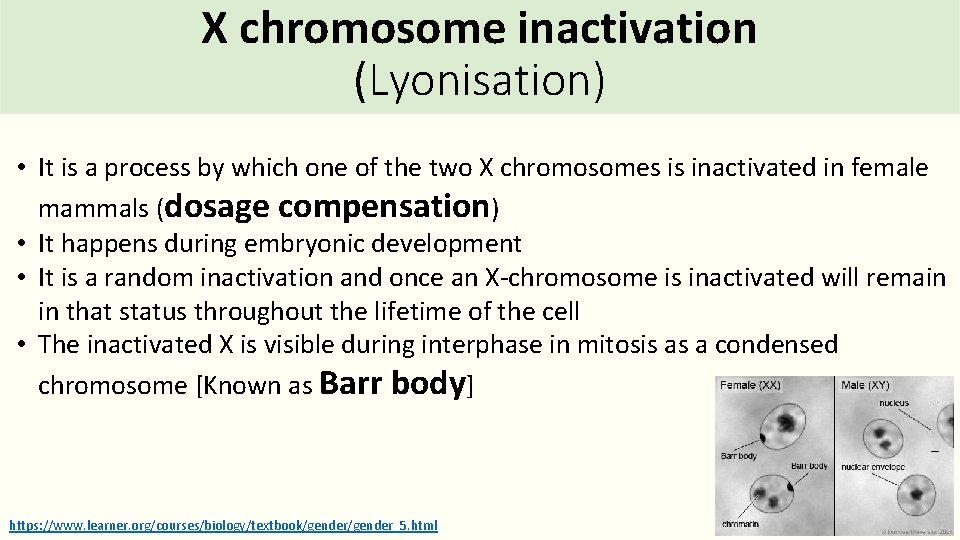
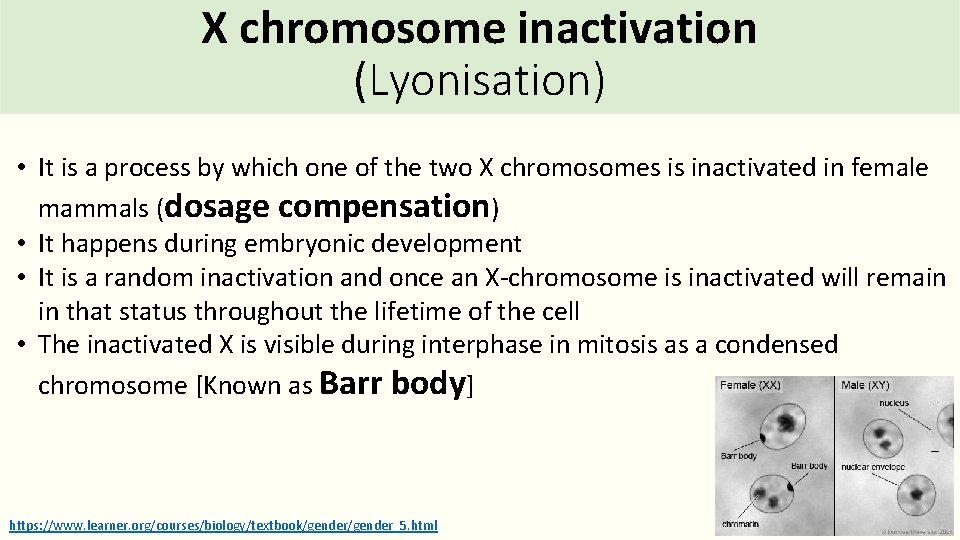
X chromosome inactivation (Lyonisation) • It is a process by which one of the two X chromosomes is inactivated in female mammals (dosage compensation) • It happens during embryonic development • It is a random inactivation and once an X-chromosome is inactivated will remain in that status throughout the lifetime of the cell • The inactivated X is visible during interphase in mitosis as a condensed chromosome [Known as Barr body] https: //www. learner. org/courses/biology/textbook/gender_5. html
X- inactivation is an epigenetic process Ø Methylation of Histone H 3 at Lys K 27 Ø Hypoacetylation of Histone H 3 and H 4 Ø Methylation of Cp. G islands
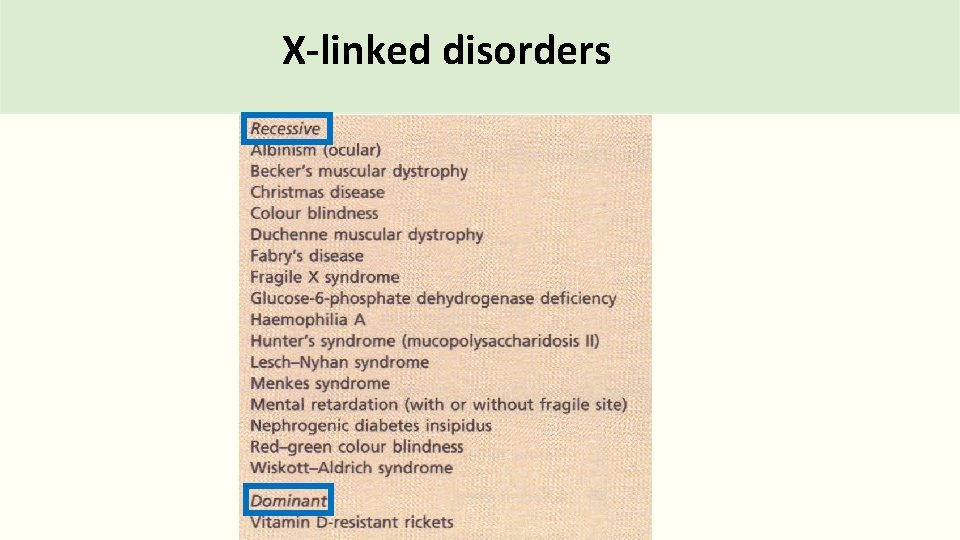
X-linked disorders
X-linked disorders Faulty gene is present on X chromosome
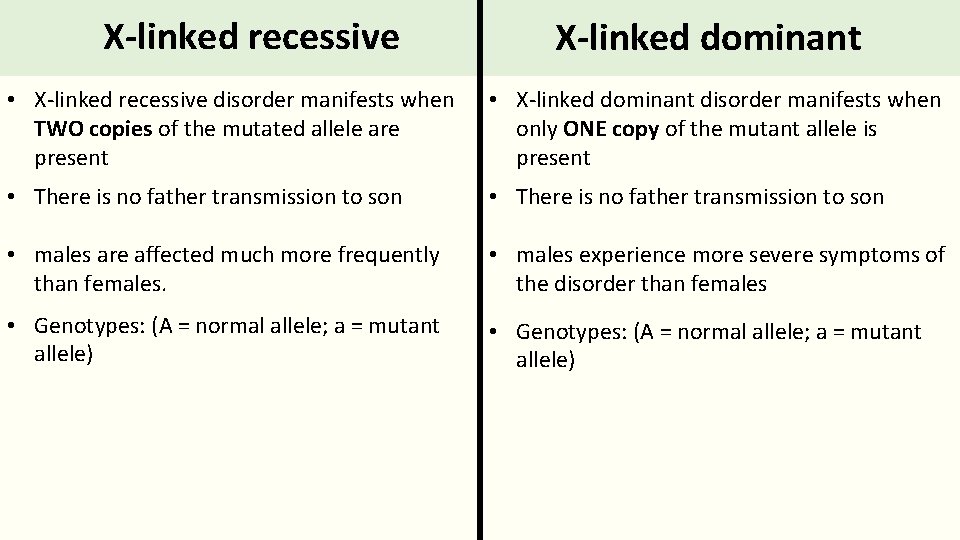
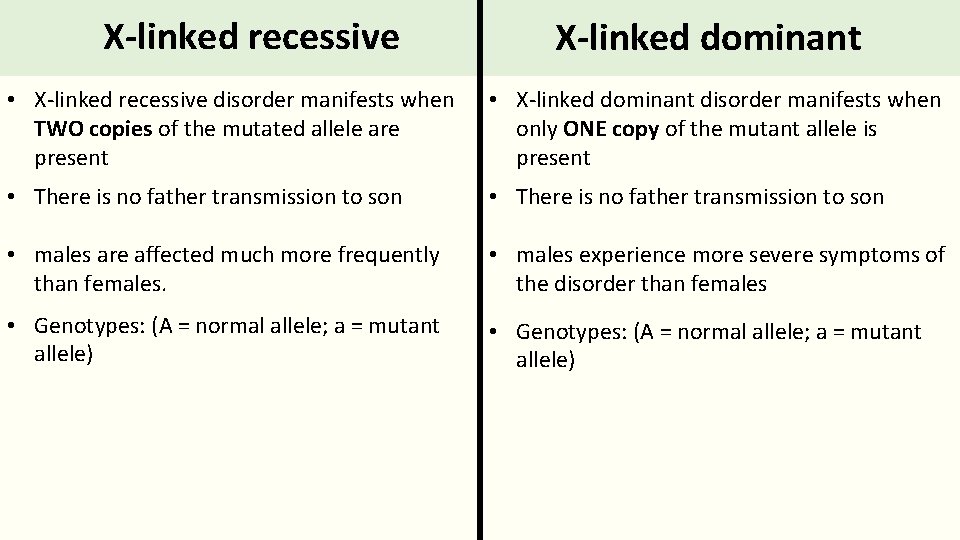
X-linked recessive X-linked dominant • X-linked recessive disorder manifests when TWO copies of the mutated allele are present • X-linked dominant disorder manifests when only ONE copy of the mutant allele is present • There is no father transmission to son • males are affected much more frequently than females. • males experience more severe symptoms of the disorder than females • Genotypes: (A = normal allele; a = mutant allele)
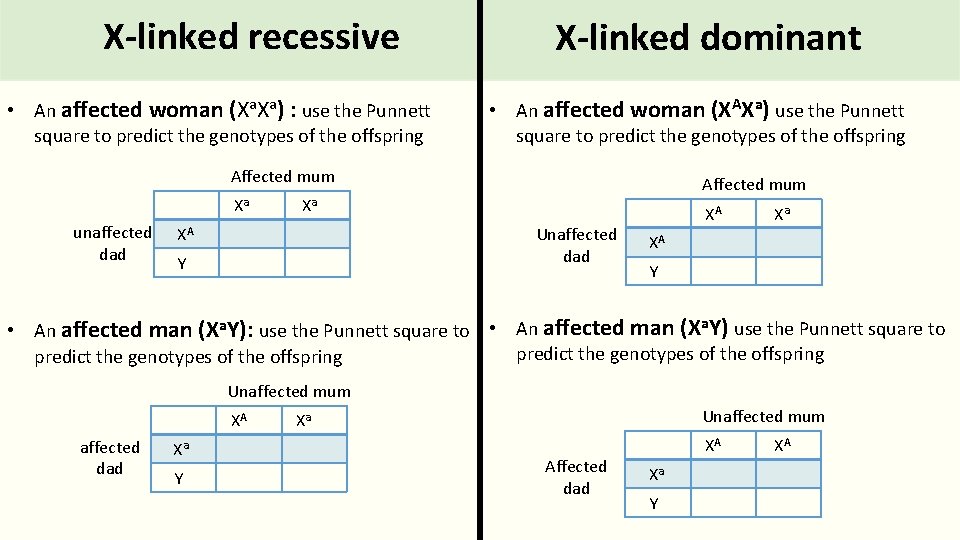
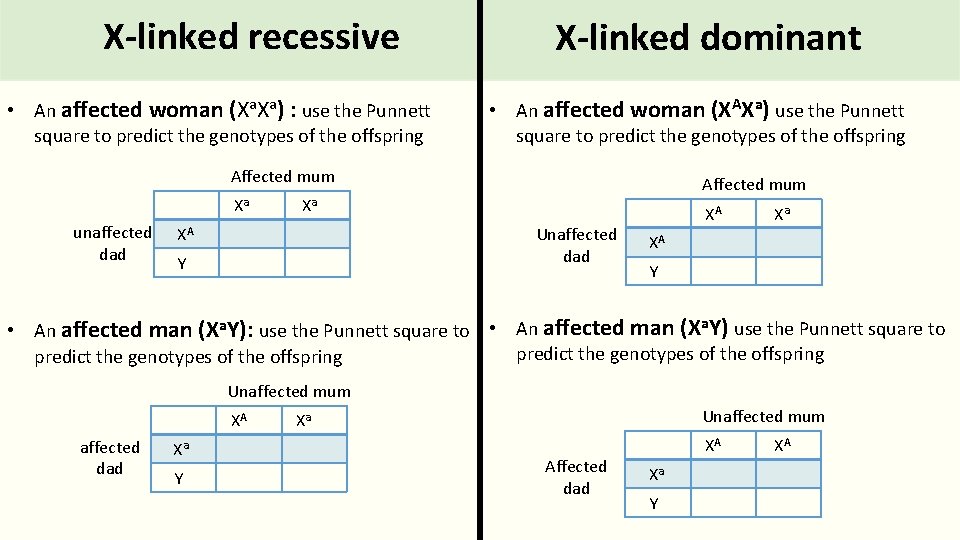
X-linked recessive • An affected woman (Xa. Xa) : use the Punnett square to predict the genotypes of the offspring X-linked dominant • An affected woman (XAXa) use the Punnett square to predict the genotypes of the offspring Affected mum Xa unaffected dad Affected mum Xa XA Unaffected dad Y XA Xa XA Y • An affected man (Xa. Y): use the Punnett square to • An affected man (Xa. Y) use the Punnett square to predict the genotypes of the offspring Unaffected mum XA affected dad Xa Y Unaffected mum Xa Affected dad XA Xa Y XA
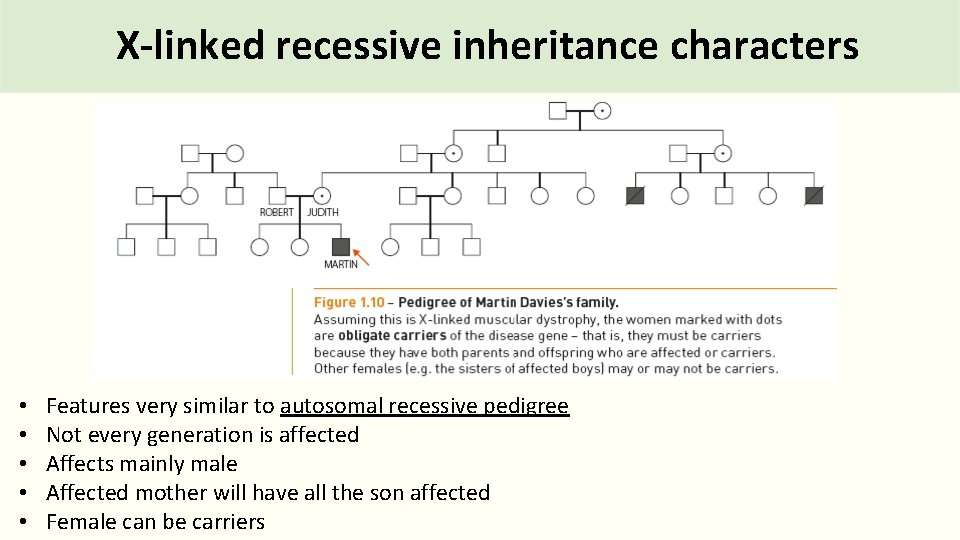
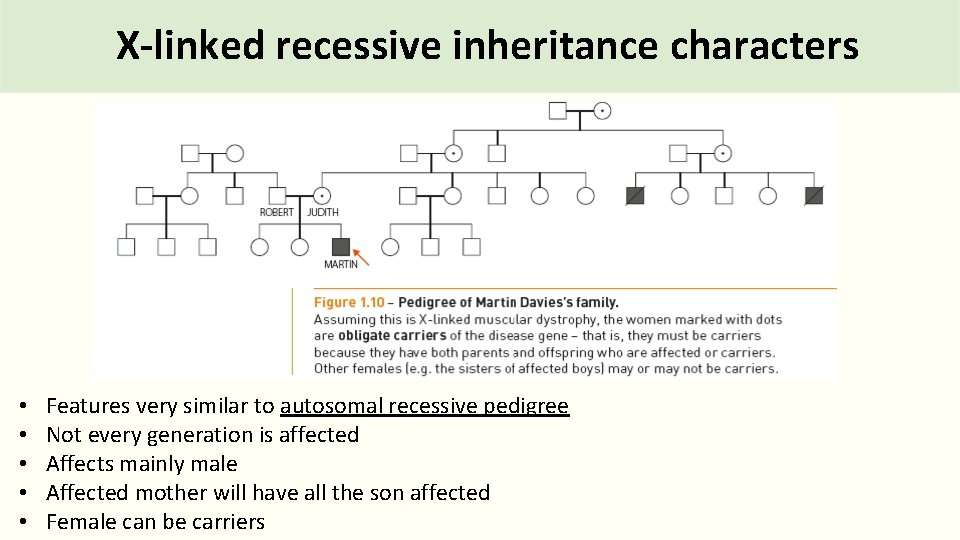
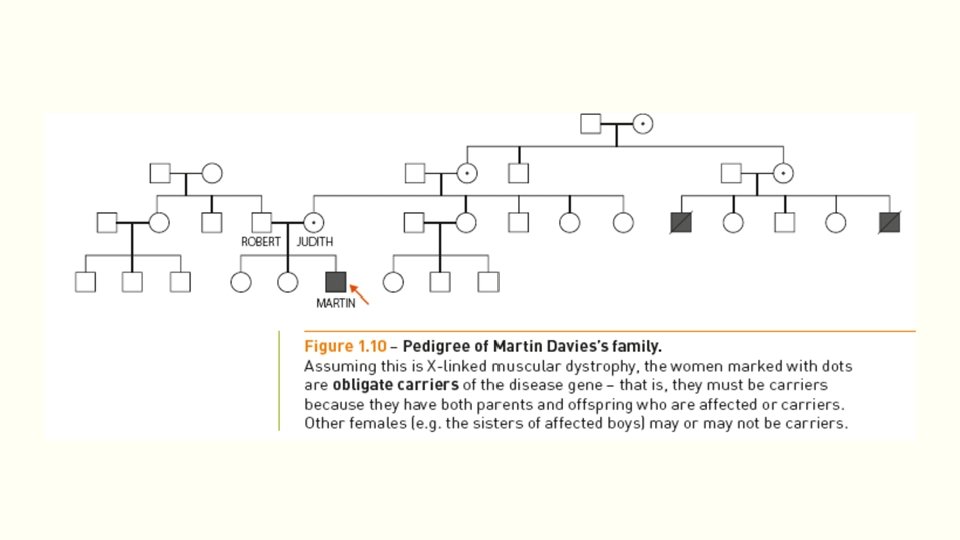
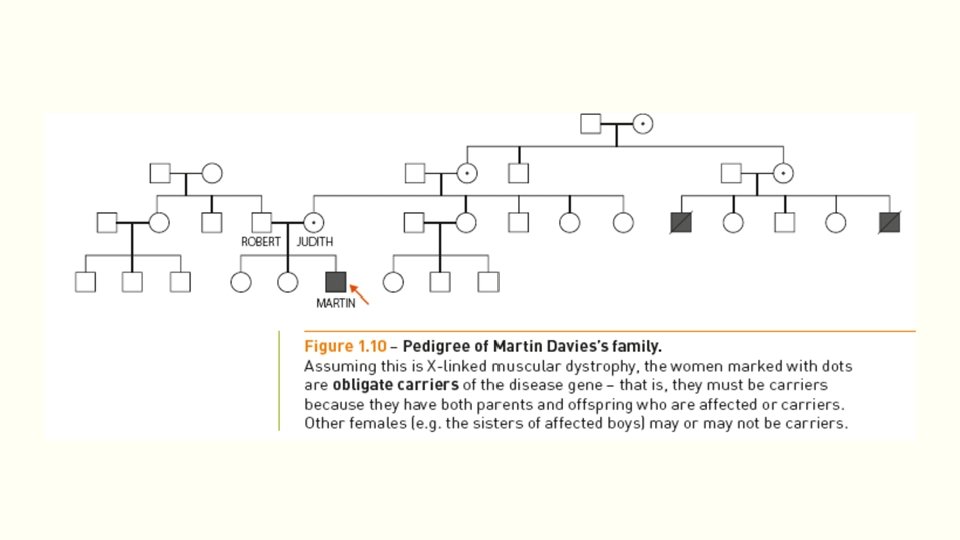
X-linked recessive inheritance characters • • • Features very similar to autosomal recessive pedigree Not every generation is affected Affects mainly male Affected mother will have all the son affected Female can be carriers
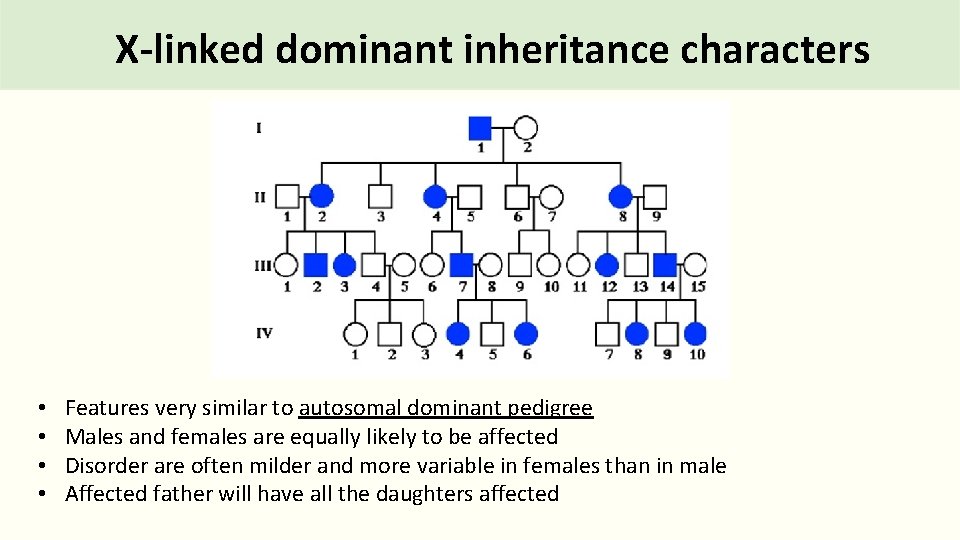
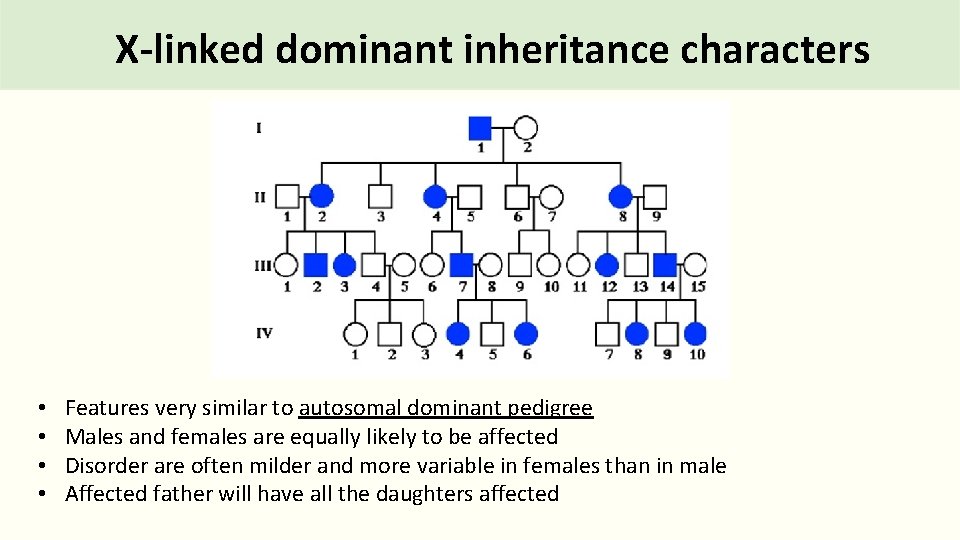
X-linked dominant inheritance characters • • Features very similar to autosomal dominant pedigree Males and females are equally likely to be affected Disorder are often milder and more variable in females than in male Affected father will have all the daughters affected
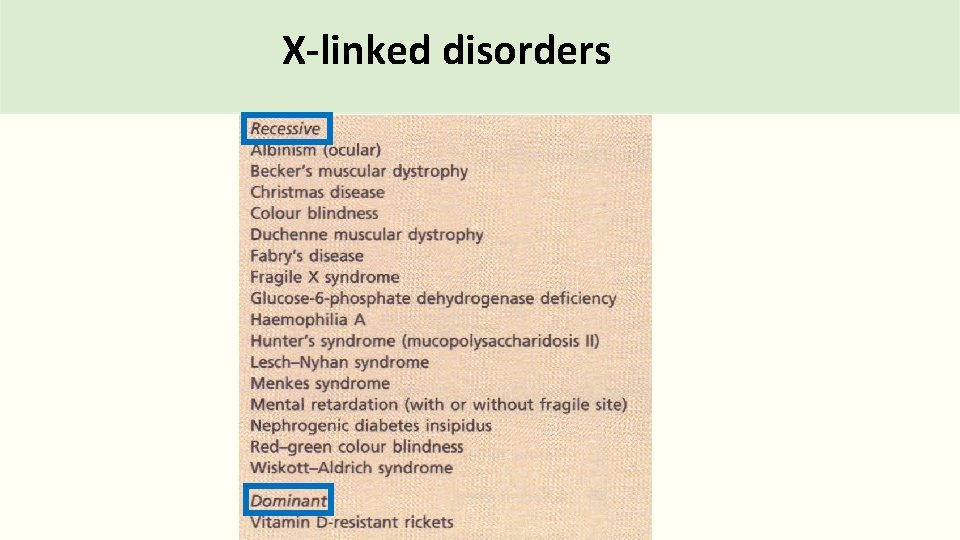
X-linked disorders
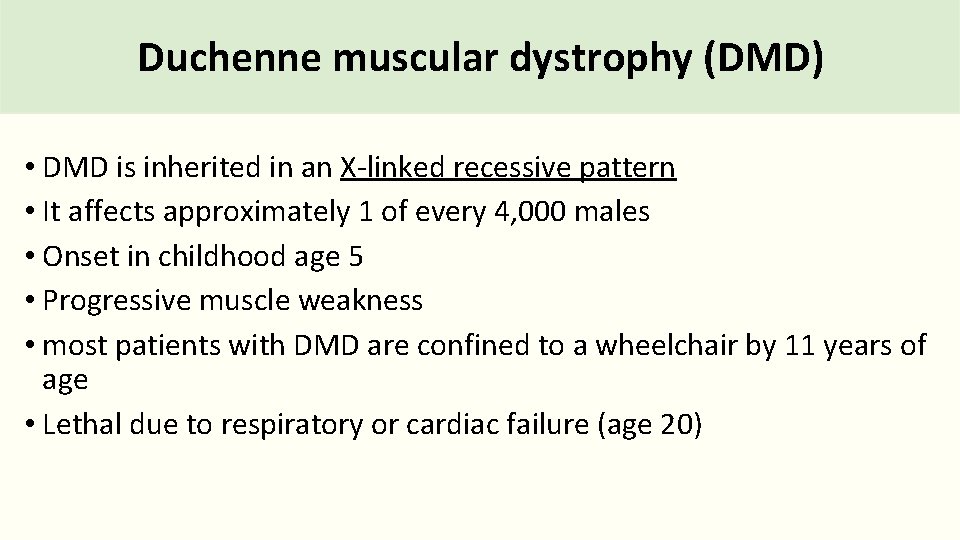
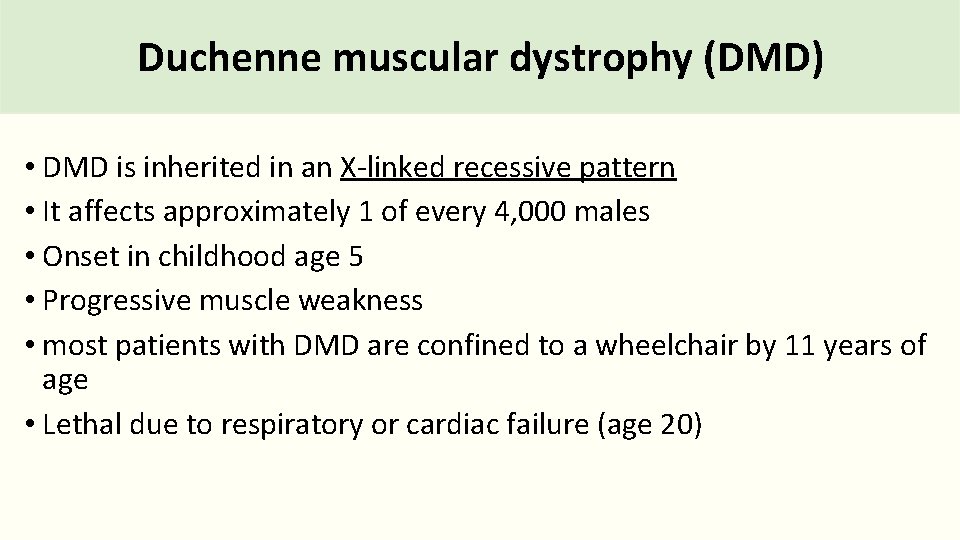
Duchenne muscular dystrophy (DMD) • DMD is inherited in an X-linked recessive pattern • It affects approximately 1 of every 4, 000 males • Onset in childhood age 5 • Progressive muscle weakness • most patients with DMD are confined to a wheelchair by 11 years of age • Lethal due to respiratory or cardiac failure (age 20)
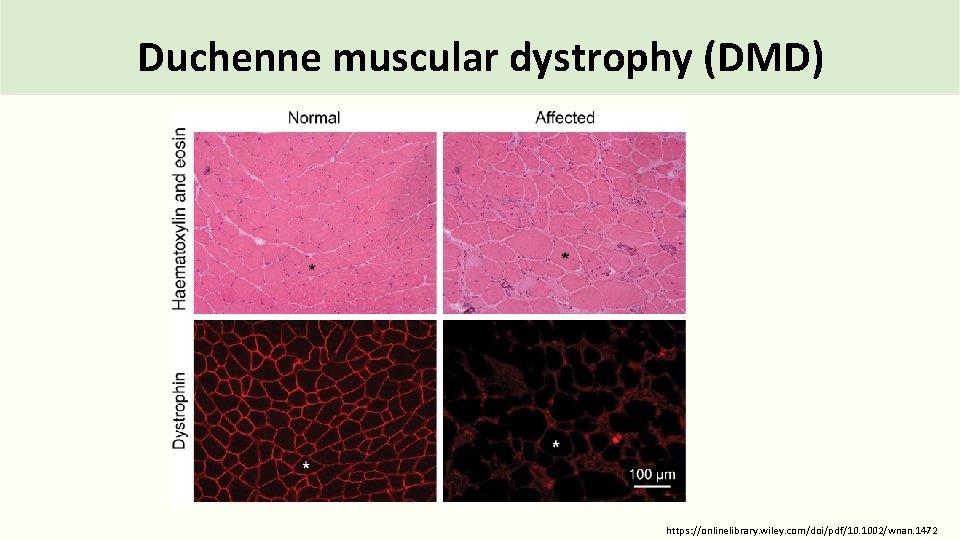
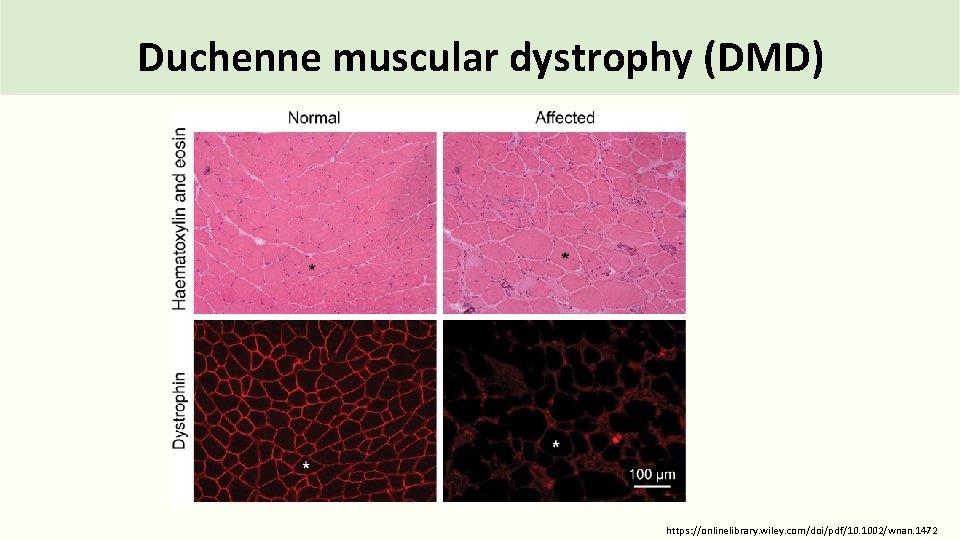
Duchenne muscular dystrophy (DMD) https: //onlinelibrary. wiley. com/doi/pdf/10. 1002/wnan. 1472
Duchenne Muscular Dystrophy • Mutations in the DMD gene cause the Duchenne muscular dystrophy • The DMD gene is the largest known human gene • It contains 79 exons • Cytogenetic Location: Xp 21. 2 -p 21. 1 • DMD gene encodes for a protein called dystrophin
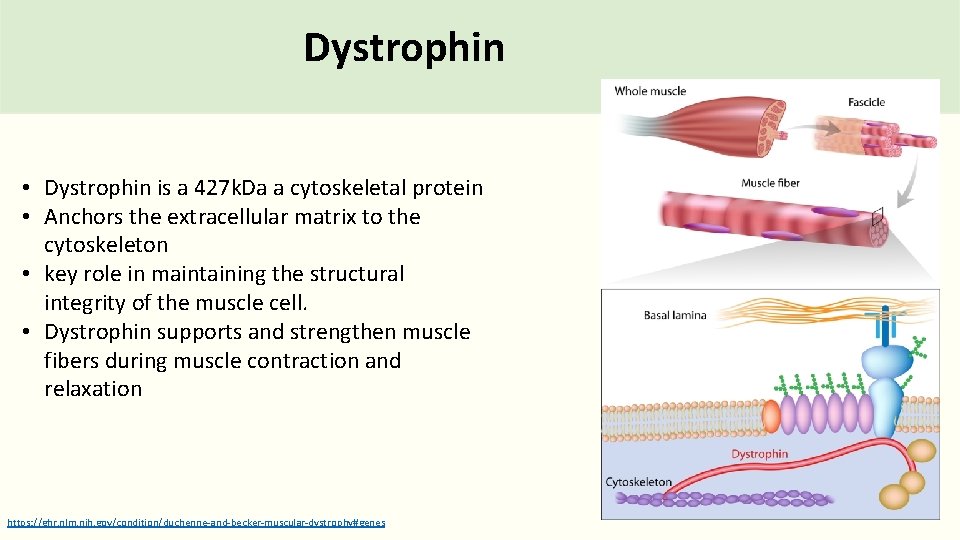
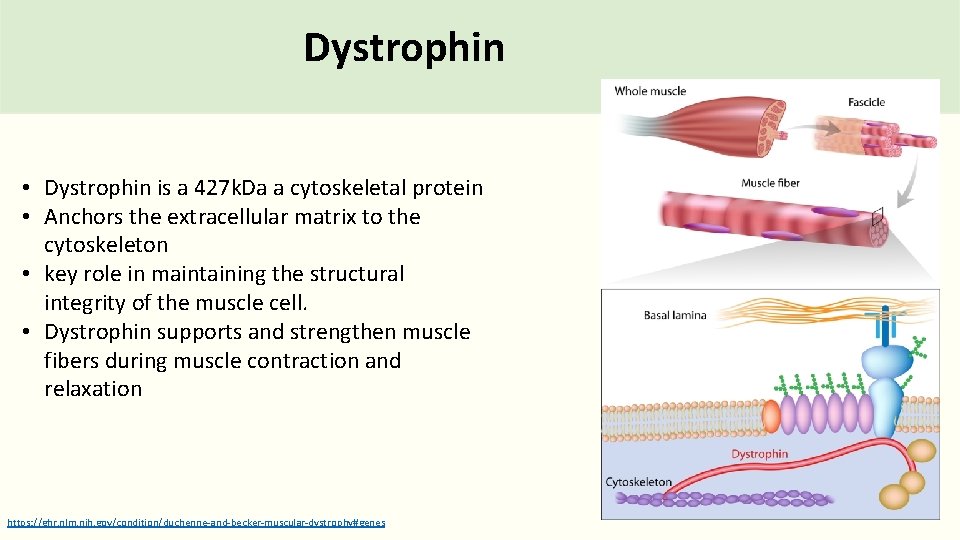
Dystrophin • Dystrophin is a 427 k. Da a cytoskeletal protein • Anchors the extracellular matrix to the cytoskeleton • key role in maintaining the structural integrity of the muscle cell. • Dystrophin supports and strengthen muscle fibers during muscle contraction and relaxation https: //ghr. nlm. nih. gov/condition/duchenne-and-becker-muscular-dystrophy#genes
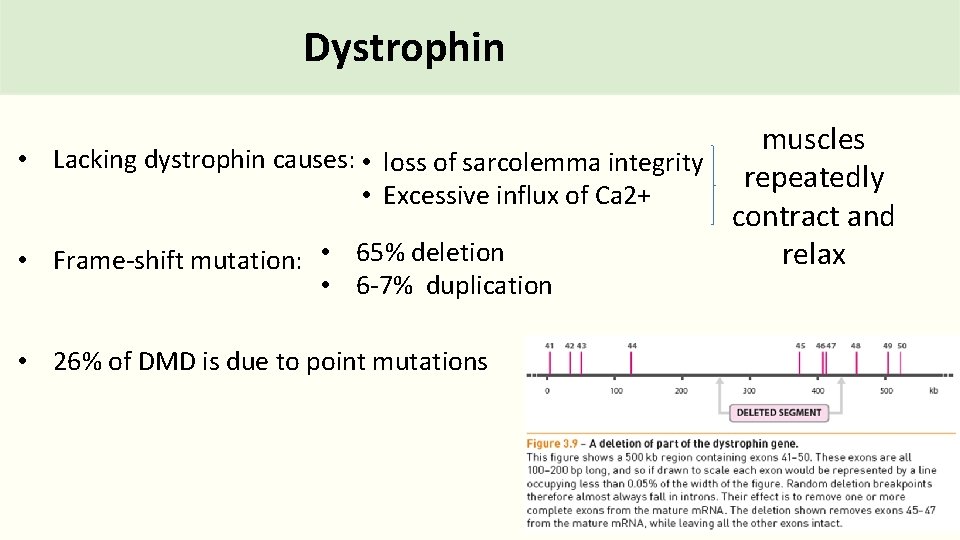
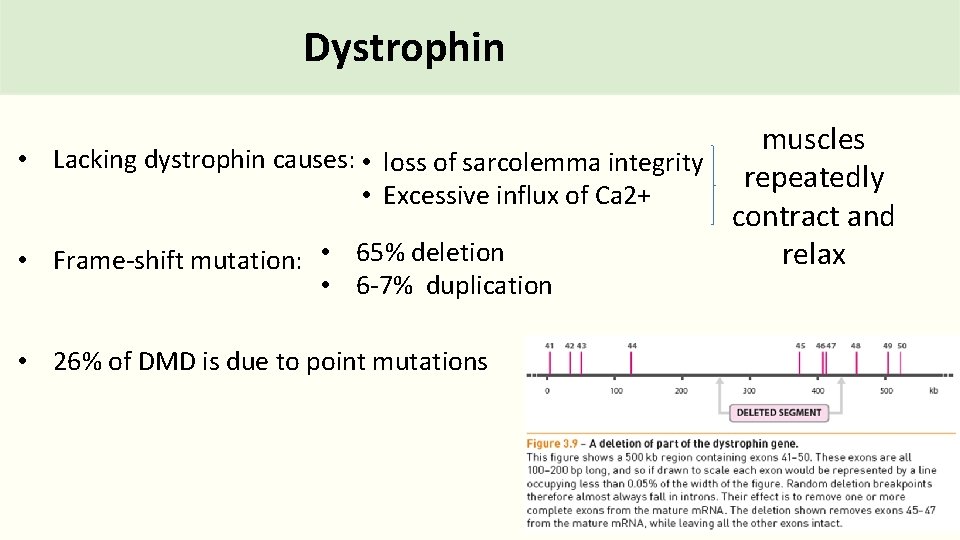
Dystrophin muscles • Lacking dystrophin causes: • loss of sarcolemma integrity repeatedly • Excessive influx of Ca 2+ contract and relax • Frame-shift mutation: • 65% deletion • 6 -7% duplication • 26% of DMD is due to point mutations
Duchenne Muscular Dystrophy Which molecular technique can be used to detect the mutations on the DMD gene?
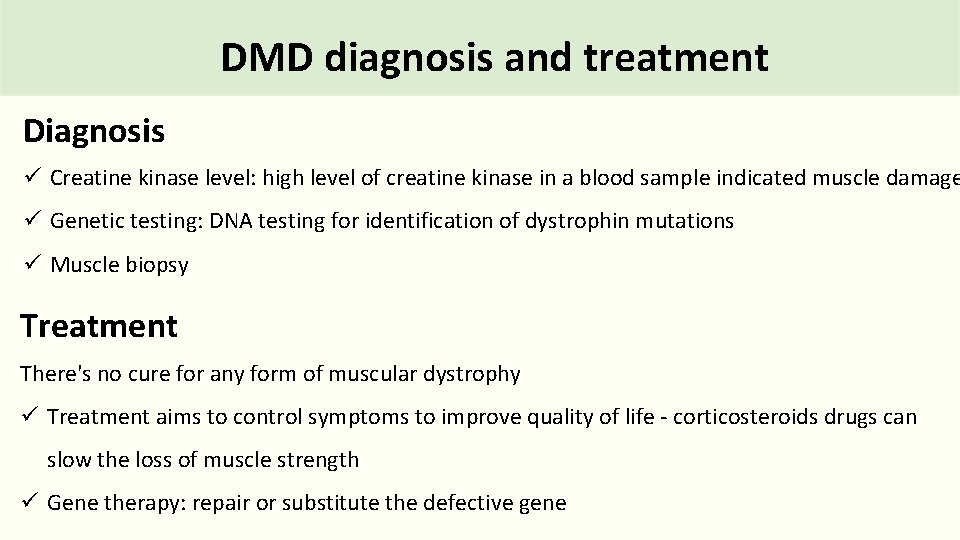
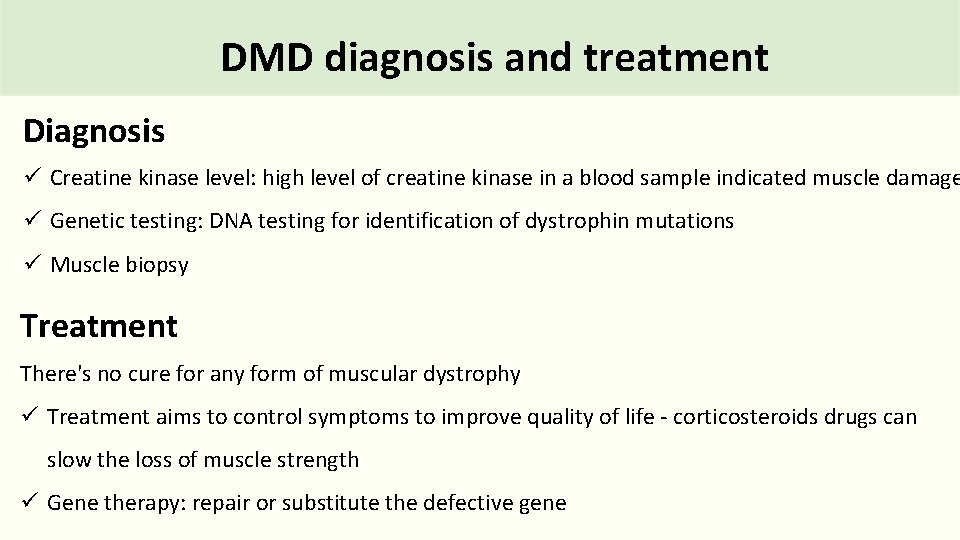
DMD diagnosis and treatment Diagnosis ü Creatine kinase level: high level of creatine kinase in a blood sample indicated muscle damage ü Genetic testing: DNA testing for identification of dystrophin mutations ü Muscle biopsy Treatment There's no cure for any form of muscular dystrophy ü Treatment aims to control symptoms to improve quality of life - corticosteroids drugs can slow the loss of muscle strength ü Gene therapy: repair or substitute the defective gene
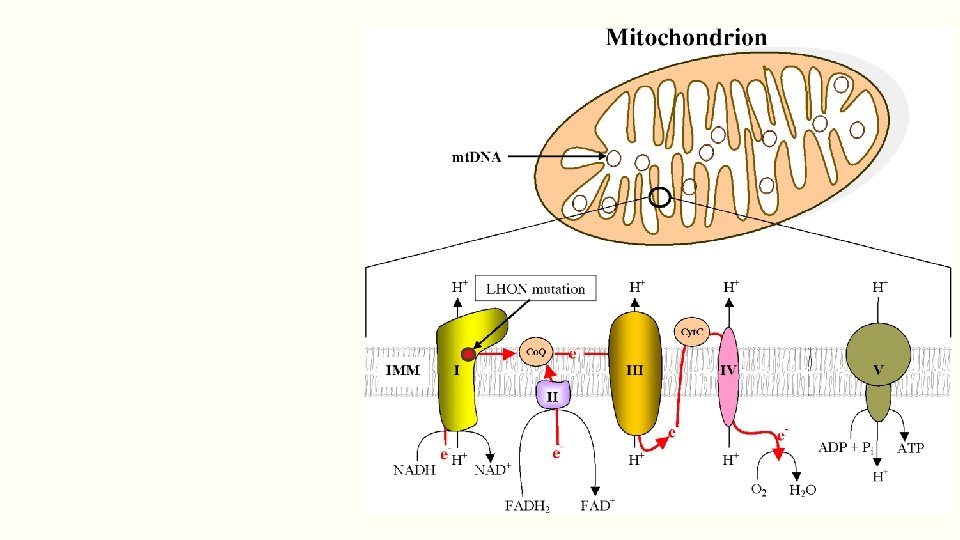
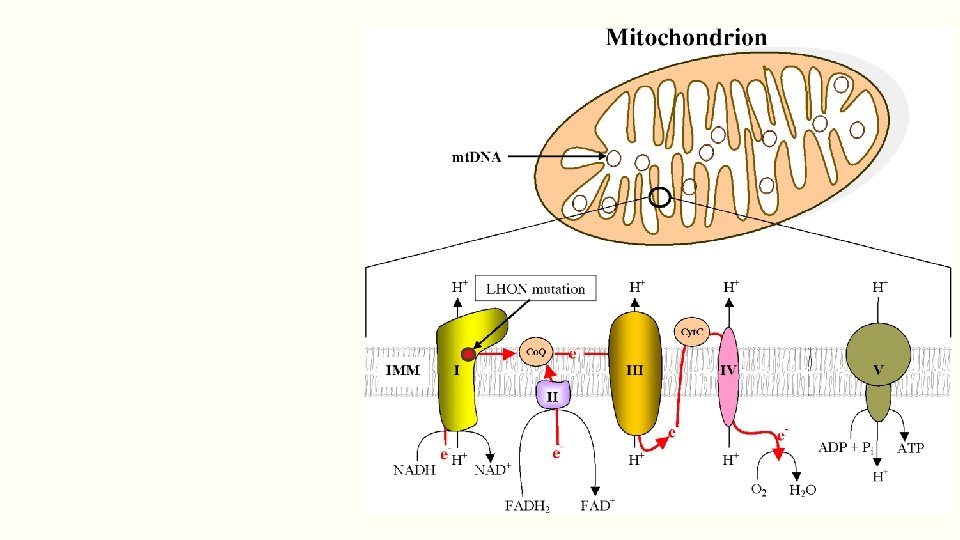
Mitochondrial DNA inheritance
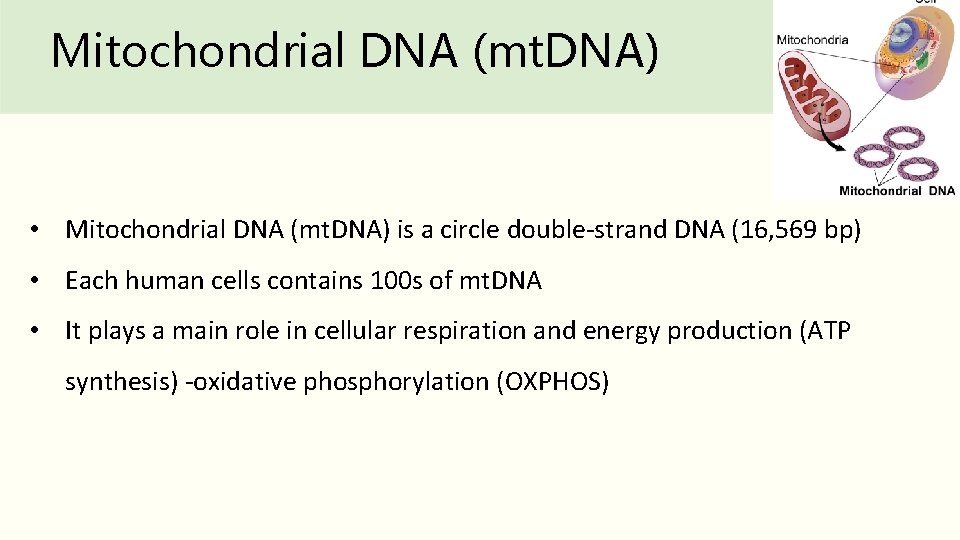
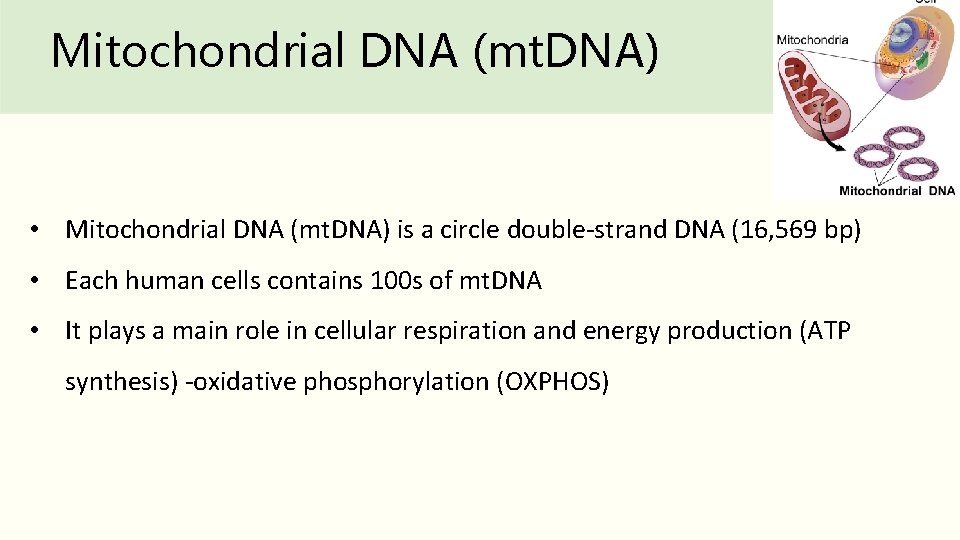
Mitochondrial DNA (mt. DNA) • Mitochondrial DNA (mt. DNA) is a circle double-strand DNA (16, 569 bp) • Each human cells contains 100 s of mt. DNA • It plays a main role in cellular respiration and energy production (ATP synthesis) -oxidative phosphorylation (OXPHOS)
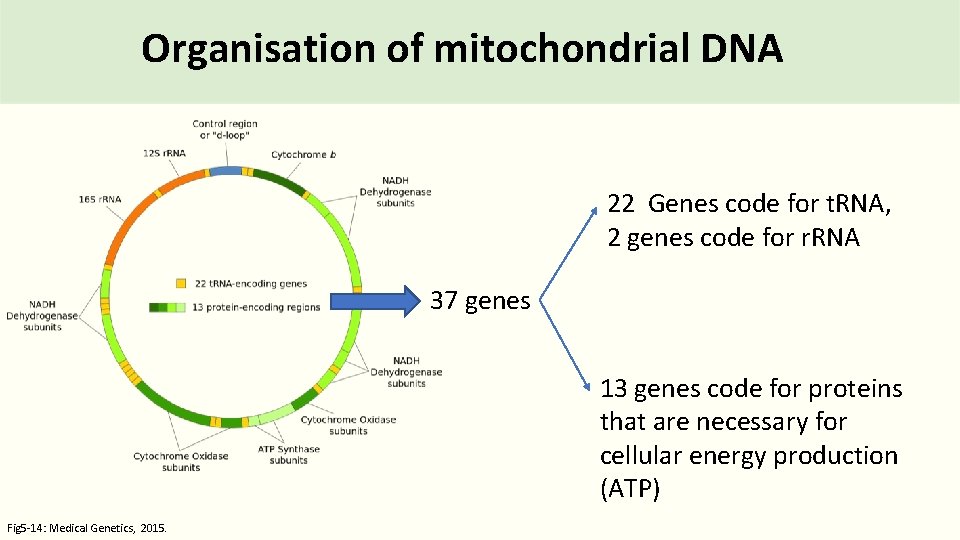
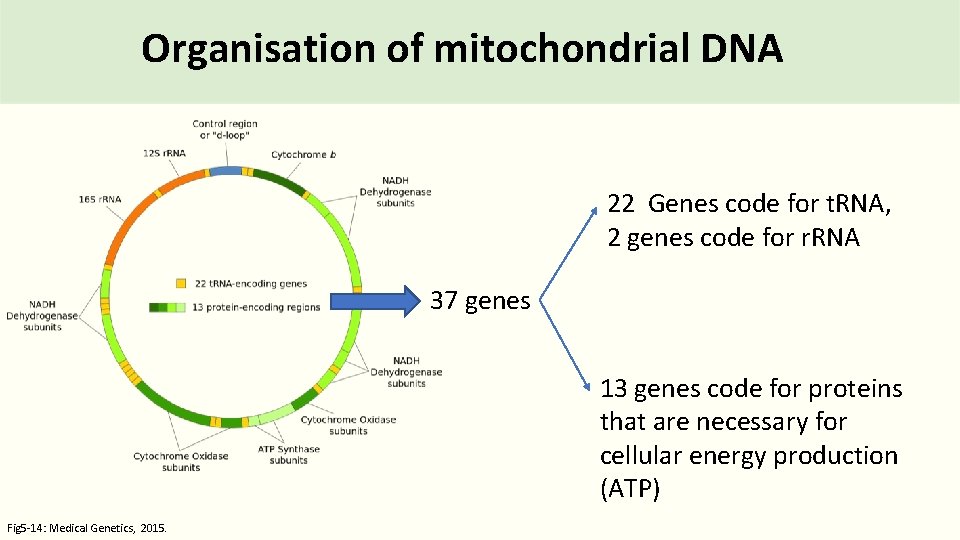
Organisation of mitochondrial DNA 22 Genes code for t. RNA, 2 genes code for r. RNA 37 genes 13 genes code for proteins that are necessary for cellular energy production (ATP) Fig 5 -14: Medical Genetics, 2015.
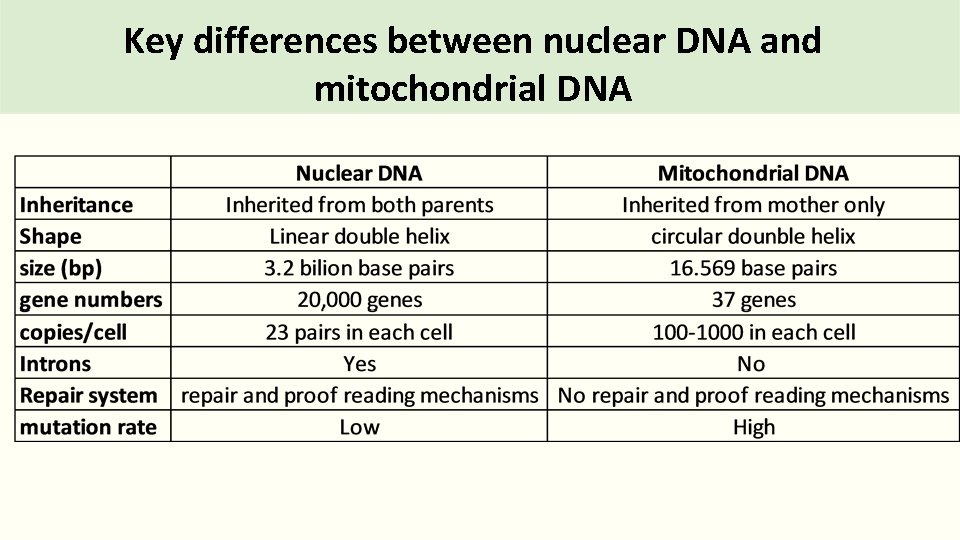
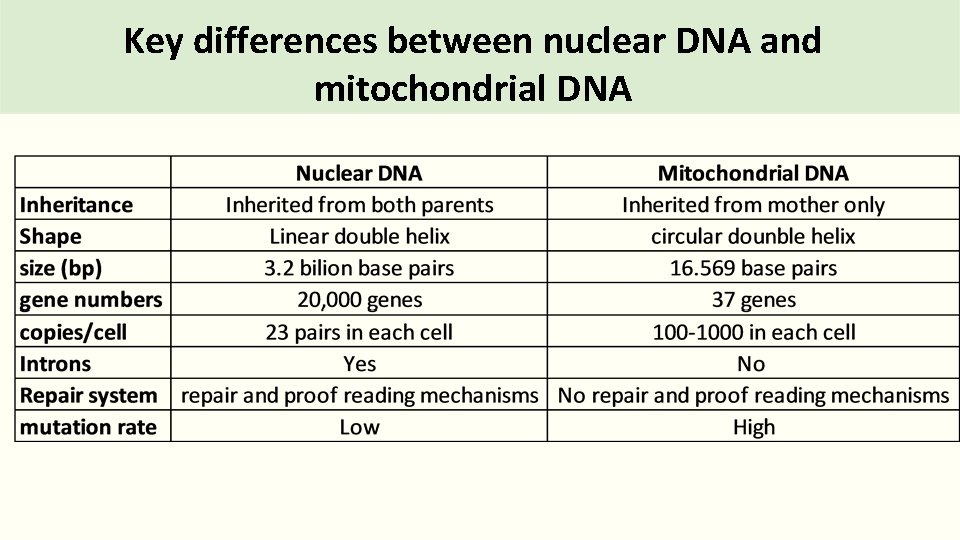
Key differences between nuclear DNA and mitochondrial DNA
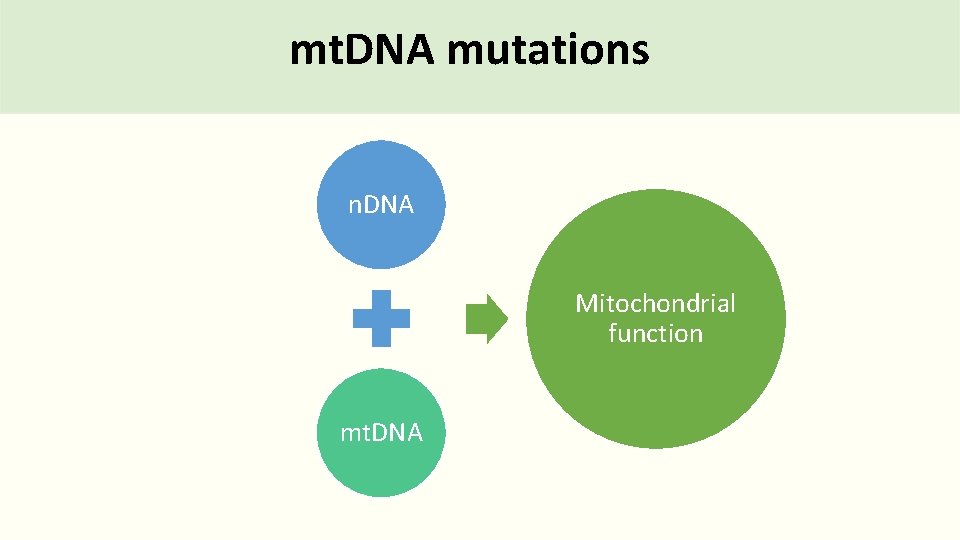
mt. DNA mutations n. DNA Mitochondrial function mt. DNA
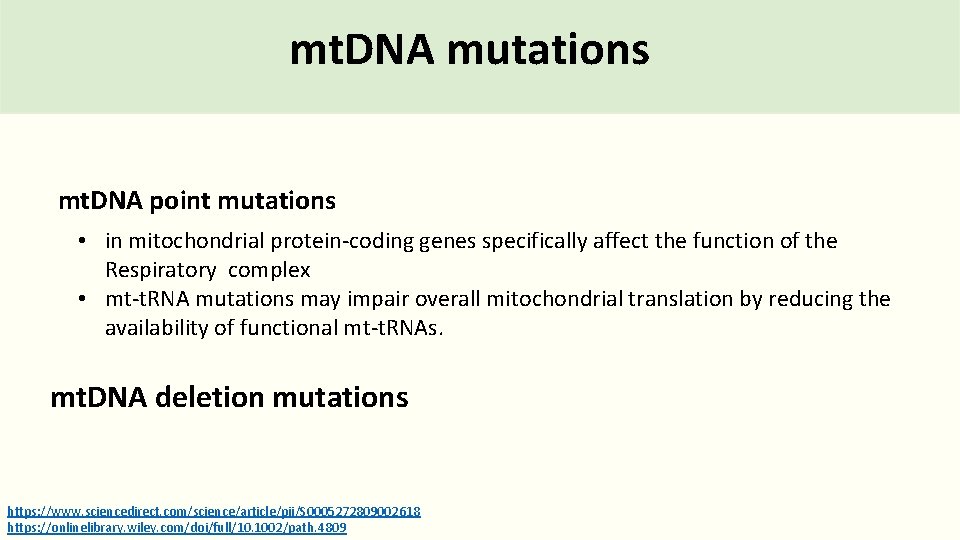
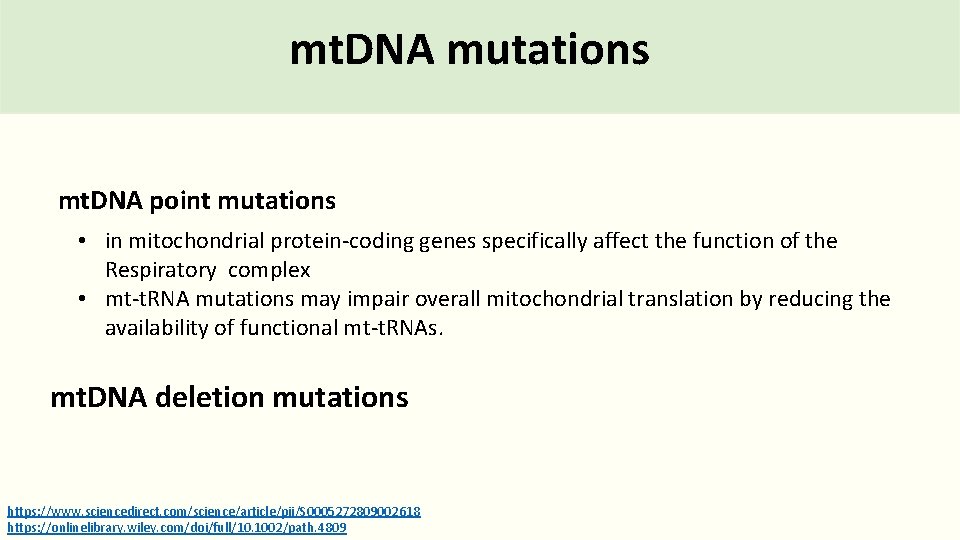
mt. DNA mutations mt. DNA point mutations • in mitochondrial protein-coding genes specifically affect the function of the Respiratory complex • mt-t. RNA mutations may impair overall mitochondrial translation by reducing the availability of functional mt-t. RNAs. mt. DNA deletion mutations https: //www. sciencedirect. com/science/article/pii/S 0005272809002618 https: //onlinelibrary. wiley. com/doi/full/10. 1002/path. 4809
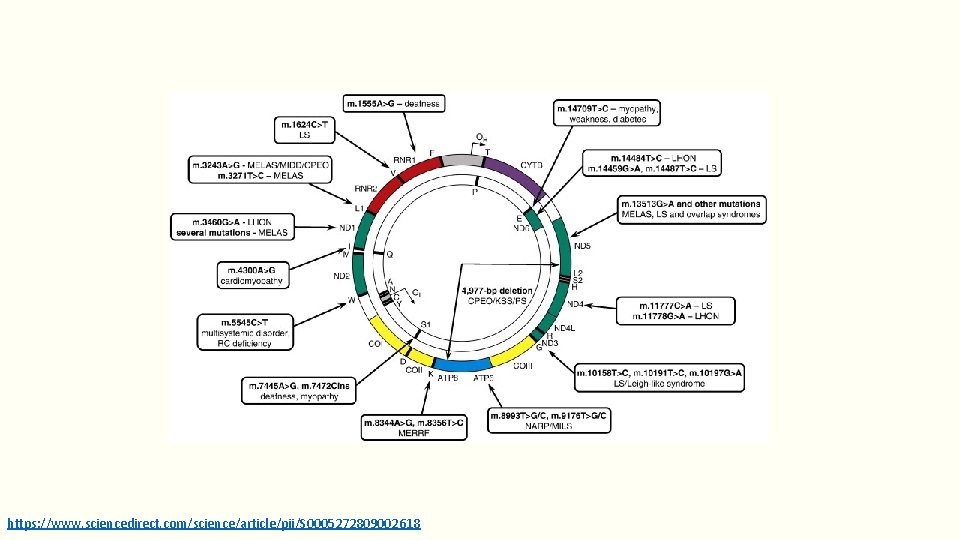
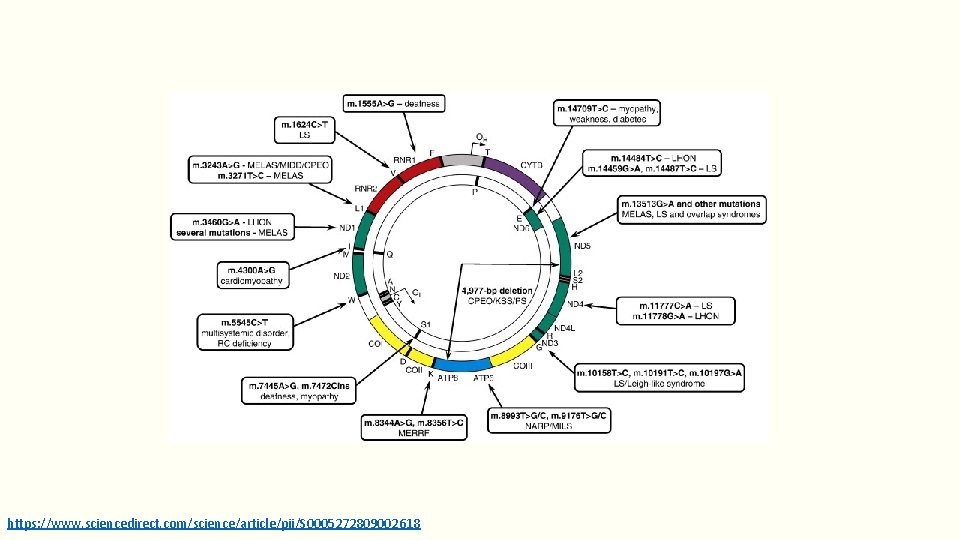
https: //www. sciencedirect. com/science/article/pii/S 0005272809002618
mt. DNA mutations Which molecular technique can be used to detect the mt. DNA mutations?
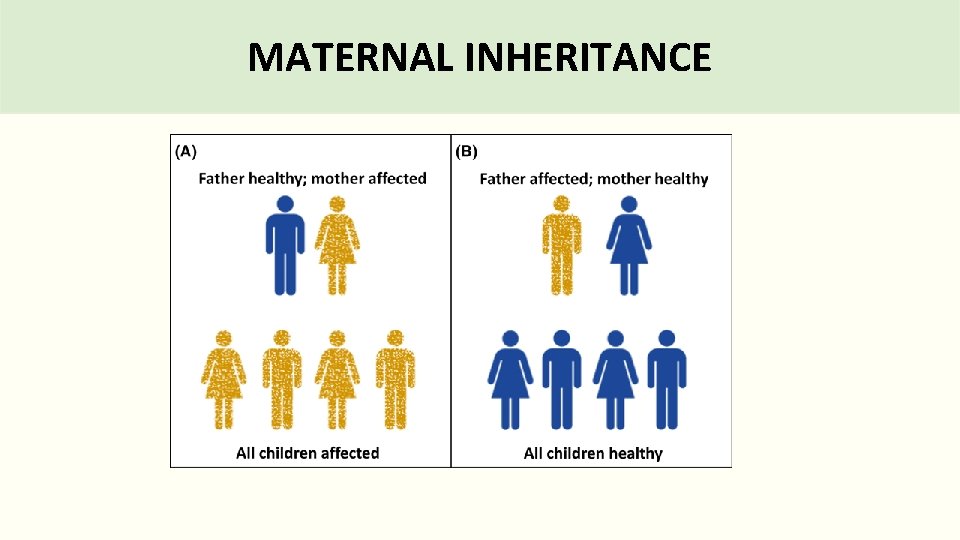
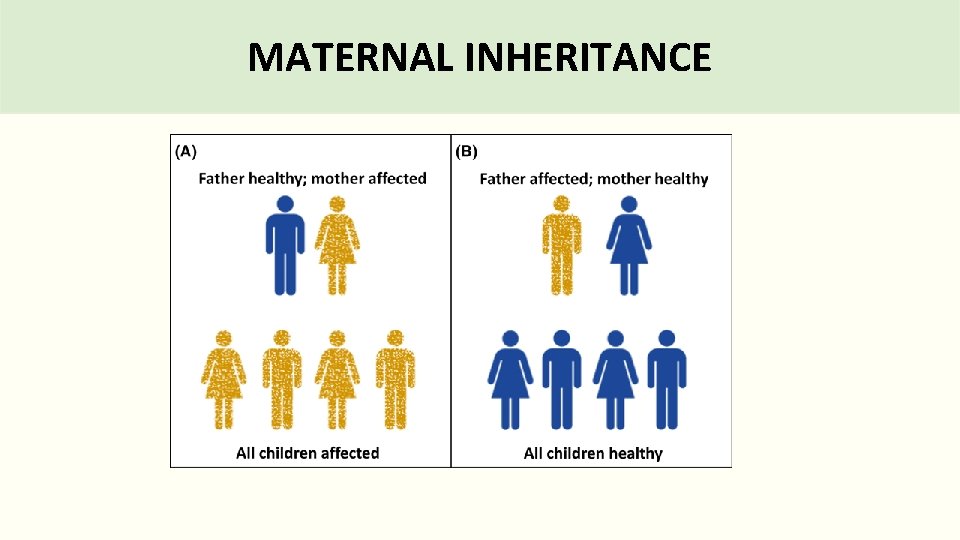
MATERNAL INHERITANCE

mt. DNA inheritance tree • Mothers pass the disease to ALL their offspring (males and females affected)
Mitochondrial disease phenotype Location of mutation type of mutation number of mitochondrial involved
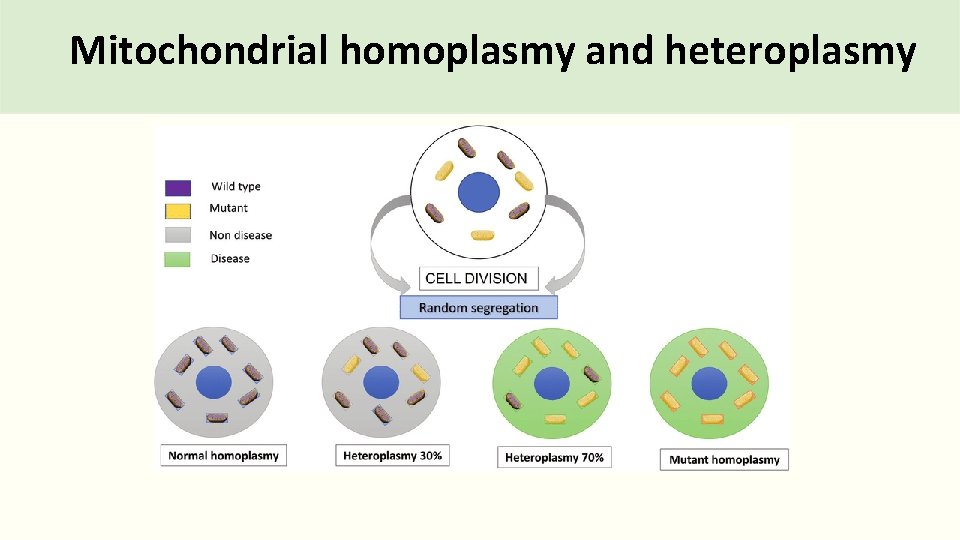
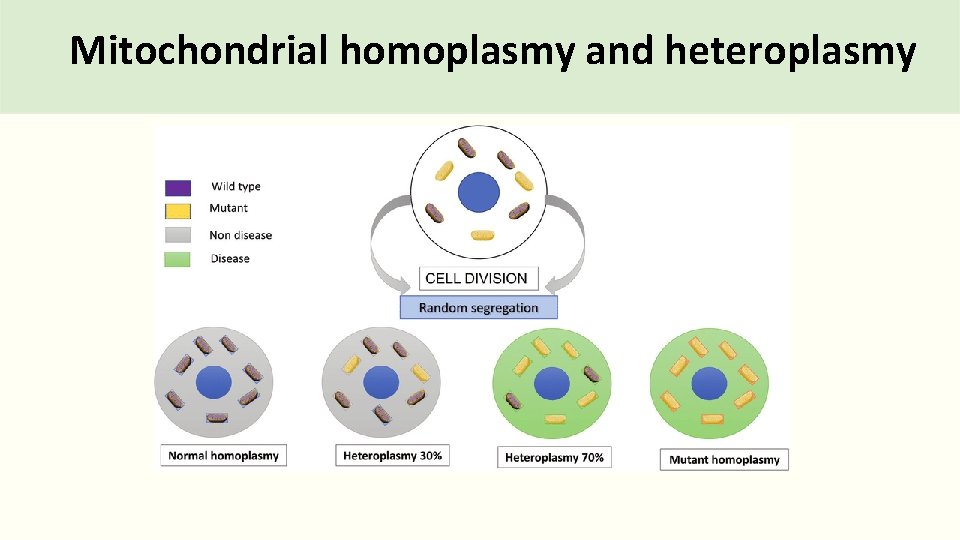
Mitochondrial homoplasmy and heteroplasmy
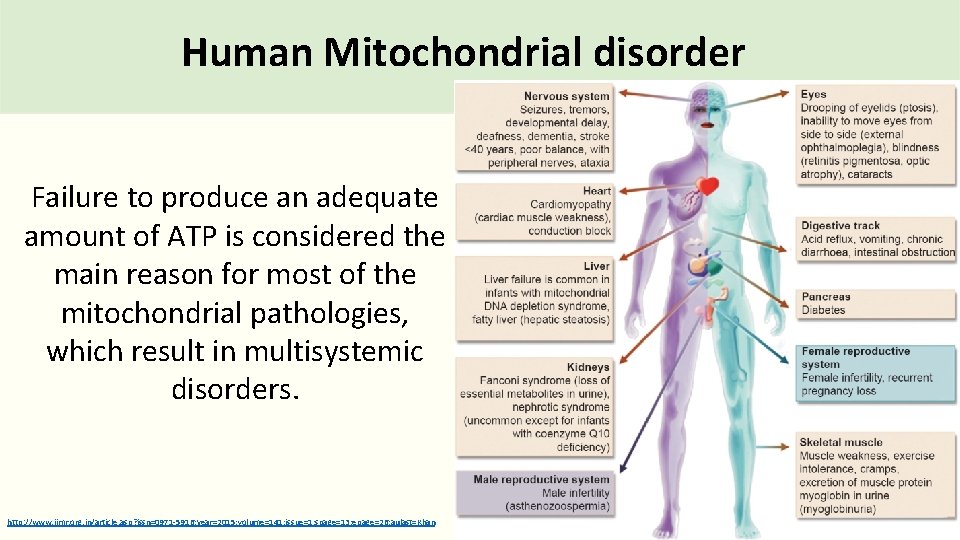
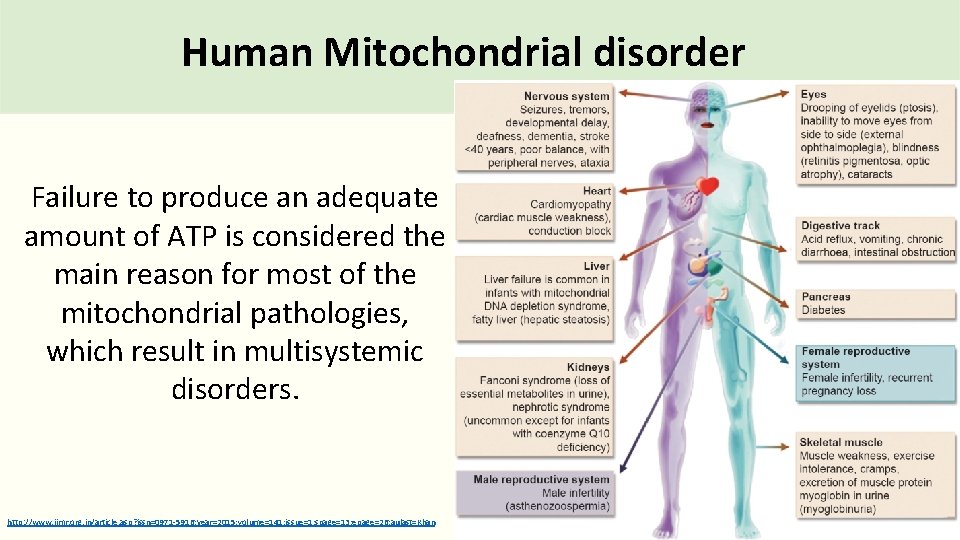
Human Mitochondrial disorder Failure to produce an adequate amount of ATP is considered the main reason for most of the mitochondrial pathologies, which result in multisystemic disorders. http: //www. ijmr. org. in/article. asp? issn=0971 -5916; year=2015; volume=141; issue=1; spage=13; epage=26; aulast=Khan
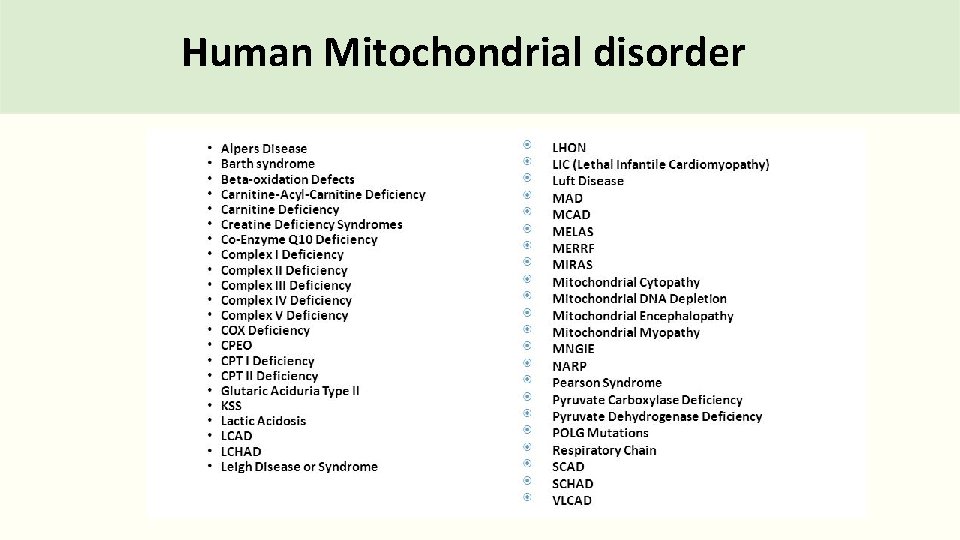
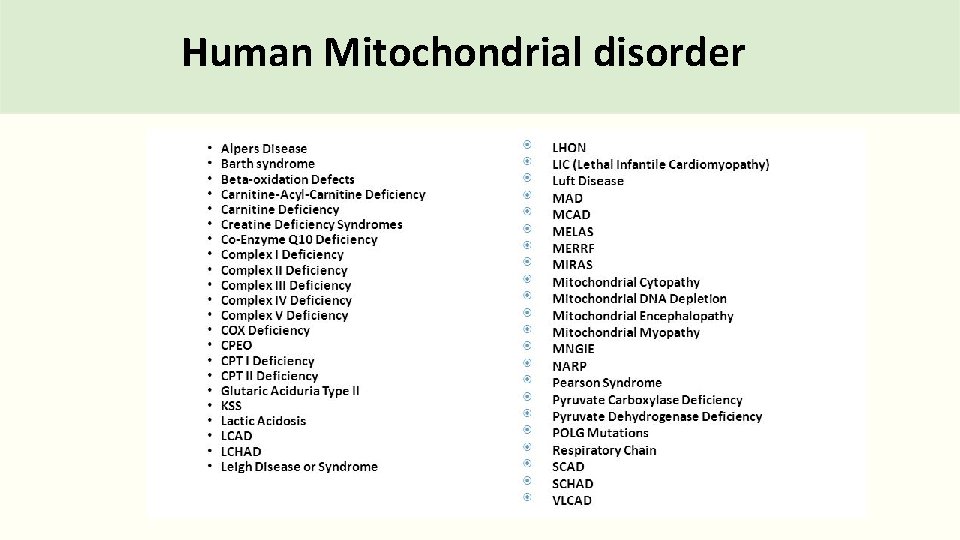
Human Mitochondrial disorder
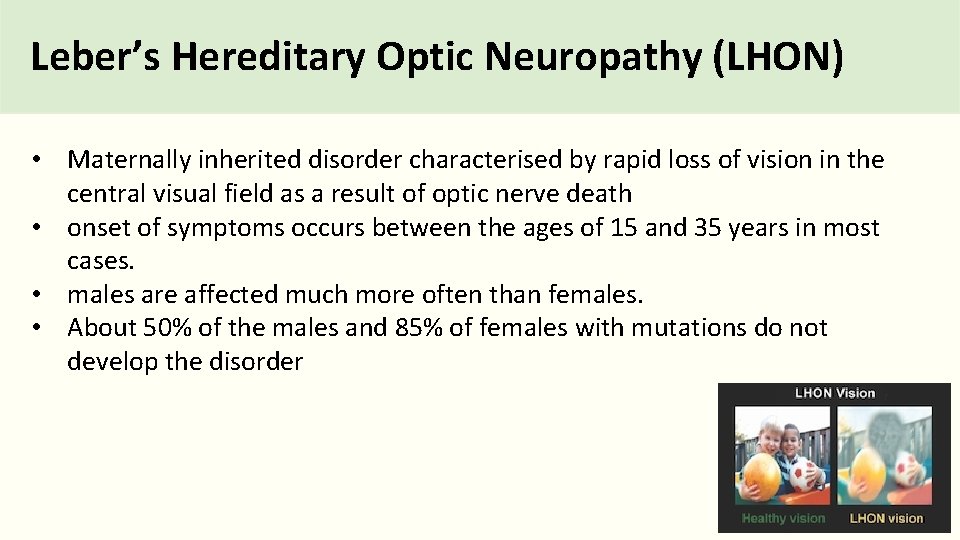
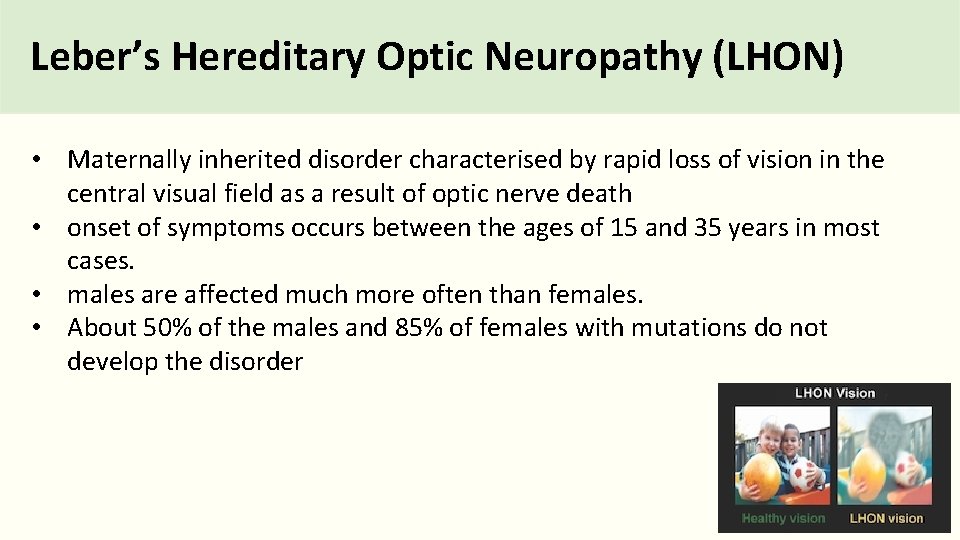
Leber’s Hereditary Optic Neuropathy (LHON) • Maternally inherited disorder characterised by rapid loss of vision in the central visual field as a result of optic nerve death • onset of symptoms occurs between the ages of 15 and 35 years in most cases. • males are affected much more often than females. • About 50% of the males and 85% of females with mutations do not develop the disorder
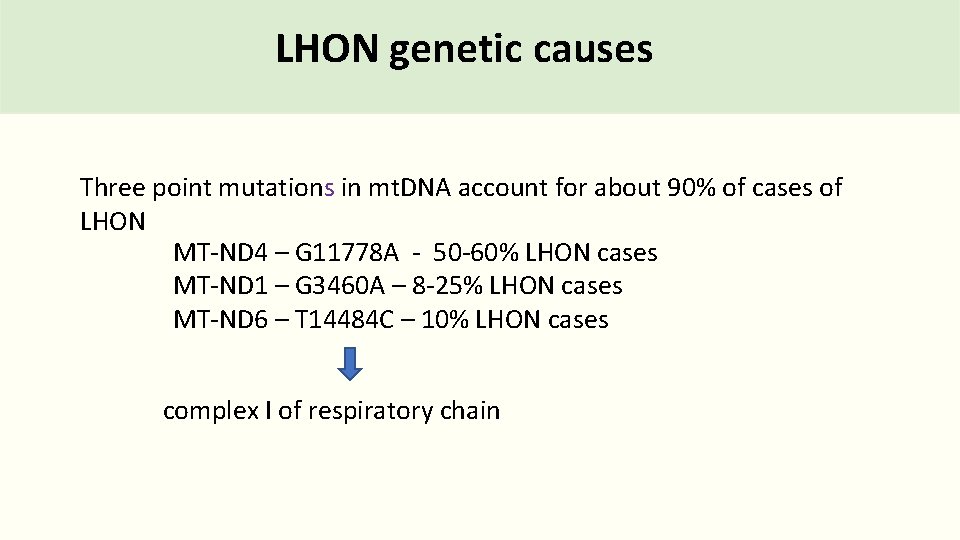
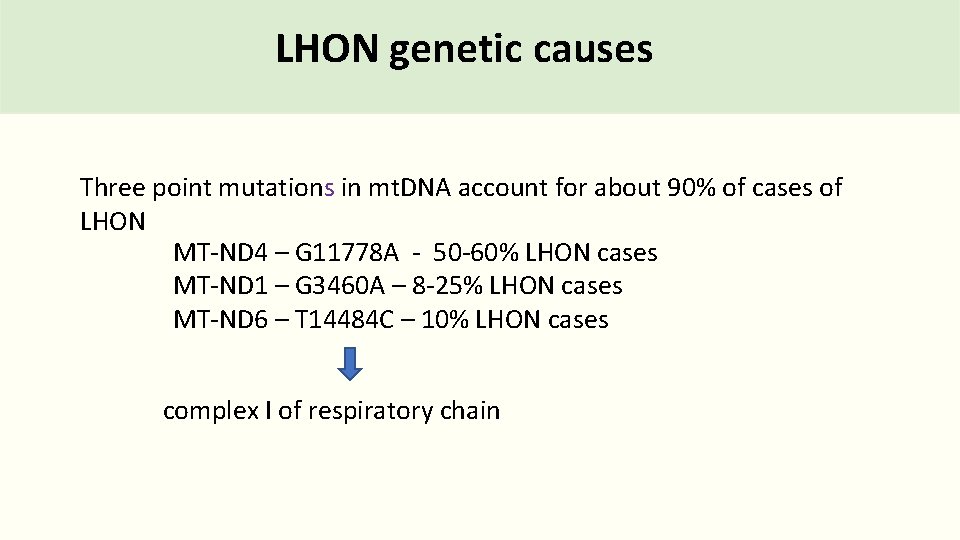
LHON genetic causes Three point mutations in mt. DNA account for about 90% of cases of LHON MT-ND 4 – G 11778 A - 50 -60% LHON cases MT-ND 1 – G 3460 A – 8 -25% LHON cases MT-ND 6 – T 14484 C – 10% LHON cases complex I of respiratory chain
LHON diagnosis and treatment Diagnosis neuro-ophthalmology examination Genetic Testing Treatment Currently, there is no cure for this disease Antioxidant drugs may protect the nerve cells from free radicals
X-inactivation • Where does it occur? X-linked disorders Possible genotypes (affected/carrier/unaffected): • When does it occur? • Is the paternal or maternal X chromosome inactivated? Example Punnett square • How are inactive X chromosomes viewed? • What is the consequence of X-inactivation for heterozygous females? • Other information Example pedigree (family tree) Example disorder(s):
Mitochondrial genome Explanation Mitochondrial genome Disorder:
