Womens Health Study WHS Thomas Dayspring MD FACP

- Slides: 41
Women’s Health Study (WHS) Thomas Dayspring, MD, FACP, FNLA Clinical Assistant Professor of Medicine University of Medicine and Dentistry of New Jersey, New Jersey Medical School Diplomate American Board of Clinical Lipidology Fellow of the National Lipid Association Certified Menopause Clinician: North American Menopause Society (NCMP) North Jersey Institute of Menopausal Lipidology Wayne, New Jersey
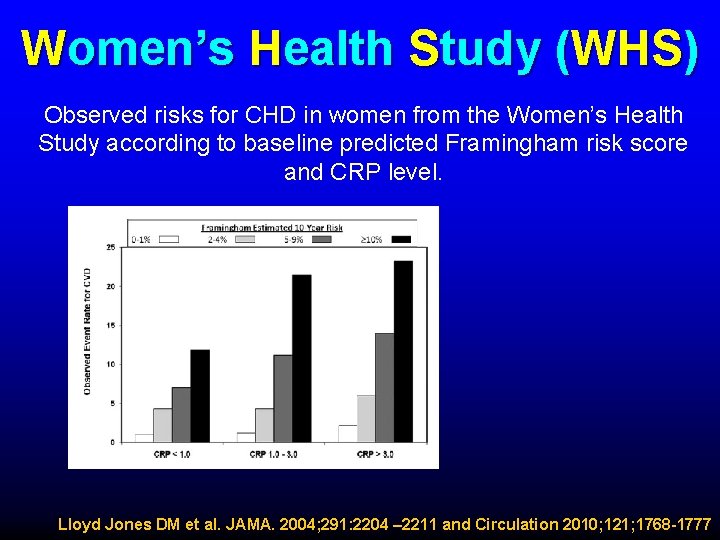
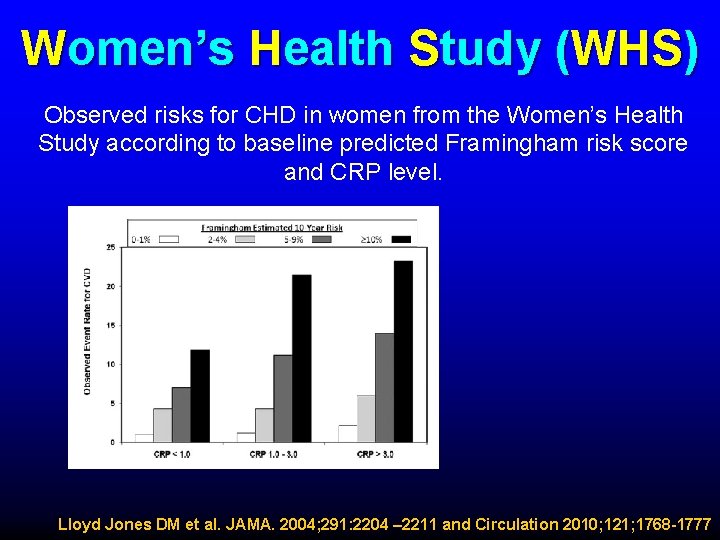
Women’s Health Study (WHS) Observed risks for CHD in women from the Women’s Health Study according to baseline predicted Framingham risk score and CRP level. Lloyd Jones DM et al. JAMA. 2004; 291: 2204 – 2211 and Circulation 2010; 121; 1768 -1777
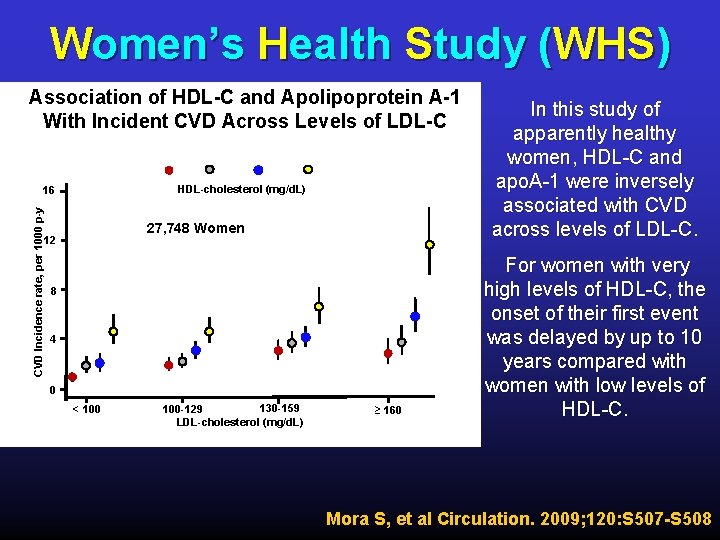
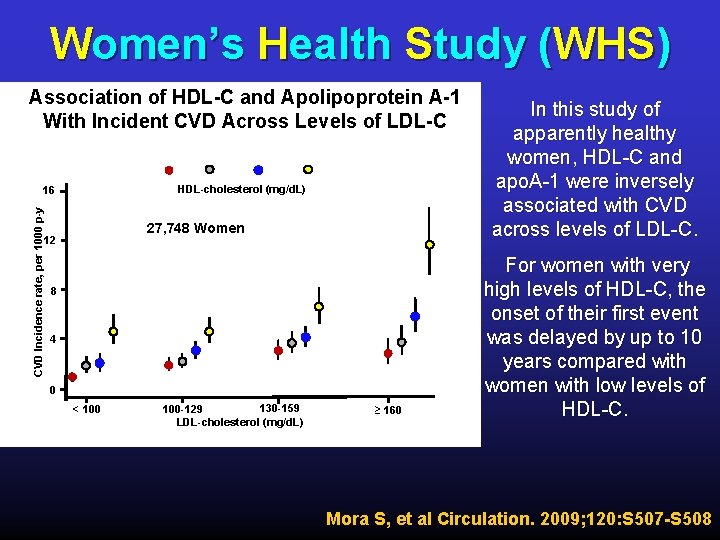
Women’s Health Study (WHS) Association of HDL-C and Apolipoprotein A-1 With Incident CVD Across Levels of LDL-C HDL-cholesterol (mg/d. L) CVD Incidence rate, per 1000 p-y 16 27, 748 Women 12 8 4 0 < 100 130 -159 100 -129 LDL-cholesterol (mg/d. L) ≥ 160 In this study of apparently healthy women, HDL-C and apo. A-1 were inversely associated with CVD across levels of LDL-C. For women with very high levels of HDL-C, the onset of their first event was delayed by up to 10 years compared with women with low levels of HDL-C. Mora S, et al Circulation. 2009; 120: S 507 -S 508
Women’s Health Study (WHS) Fasting versus Nonfasting Triglycerides F F F Prospective study of 26, 509 initially healthy US women (20, 118 fasting and 6391 nonfasting) participating in the Women’s Health Study, enrolled between November 1992 and July 1995 and undergoing follow-up for a median of 11. 4 years. Triglyceride levels were measured in blood samples obtained at time of enrollment. Analyses grouped into tertiles of TG levels • Fasting: ≤ 90 mg/d. L, 91 - 147 mg/d. L and ≥ 148 mg/d. L • Nonfasting: ≤ 104 mg/d. L, 105 -170 mg/d. L, ≥ 171 mg/d. L Bansal, S et al. JAMA. 2007; 298: 309 -316
Women’s Health Study (WHS) Fasting versus Nonfasting Triglycerides F F At baseline, triglyceride levels in fasting as well as nonfasting women correlated with traditional cardiac risk factors and markers of insulin resistance. During a median follow-up of 11. 4 years, 1001 participants experienced an incident cardiovascular event (including 276 nonfatal myocardial infarctions, 265 ischemic strokes, 628 coronary revascularizations, and 163 cardiovascular deaths), for an overall rate of 3. 46 cardiovascular events per 1000 person-years of follow-up. Bansal, S et al. JAMA. 2007; 298: 309 -316
Women’s Health Study (WHS) Fasting versus Nonfasting Triglycerides F F F The use of nonfasting levels of triglycerides in risk assessment provides several potential advantages to clinical practice. • Much of the 24 -hour day is spent in the nonfasting state, especially considering the fact that triglycerides may take up to 12 hours to return to fasting levels after a meal. Postprandial levels are a more robust indicator of cardiovascular risk, perhaps because the greater variability of postprandial levels captures important information about an individual’s metabolism. Previous studies have demonstrated the benefits of several classes of drugs on postprandial elevations in triglyceride levels Bansal, S et al. JAMA. 2007; 298: 309 -316
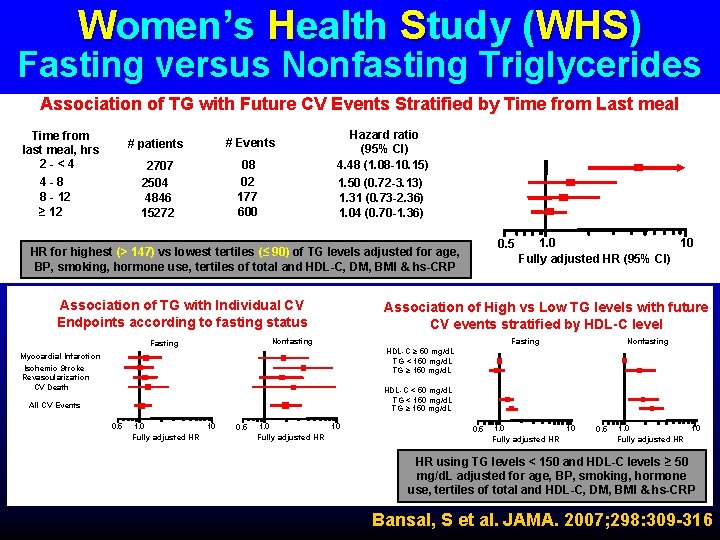
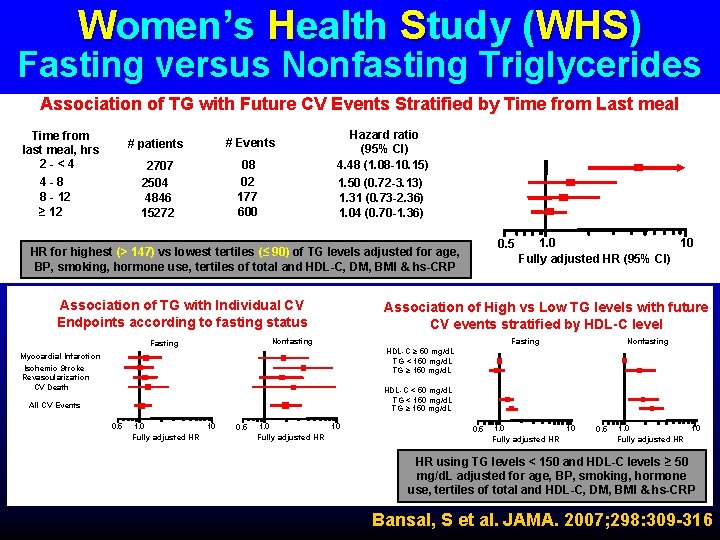
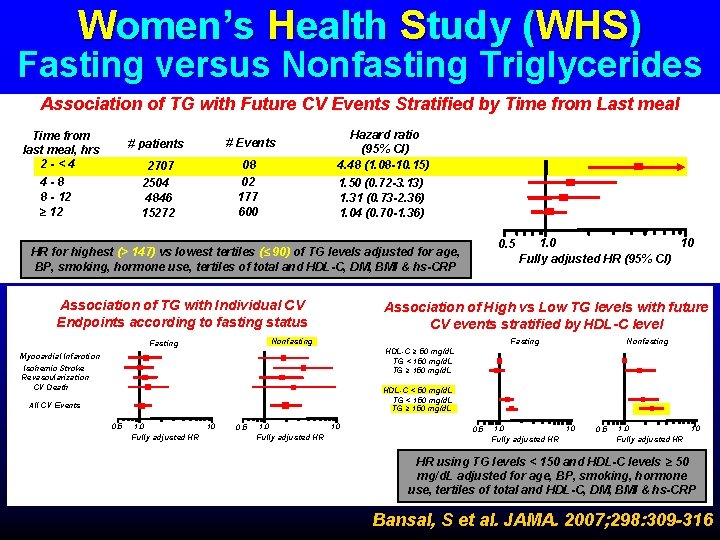
Women’s Health Study (WHS) Fasting versus Nonfasting Triglycerides Association of TG with Future CV Events Stratified by Time from Last meal Time from last meal, hrs 2 -<4 4 -8 8 - 12 ≥ 12 # patients # Events 2707 2504 4846 15272 08 02 177 600 Hazard ratio (95% CI) 4. 48 (1. 08 -10. 15) 1. 50 (0. 72 -3. 13) 1. 31 (0. 73 -2. 36) 1. 04 (0. 70 -1. 36) 0. 5 HR for highest (> 147) vs lowest tertiles (≤ 90) of TG levels adjusted for age, BP, smoking, hormone use, tertiles of total and HDL-C, DM, BMI & hs-CRP Association of TG with Individual CV Endpoints according to fasting status Association of High vs Low TG levels with future CV events stratified by HDL-C level Fasting Nonfasting Fasting 10 1. 0 Fully adjusted HR (95% CI) Nonfasting HDL-C ≥ 50 mg/d. L TG < 150 mg/d. L TG ≥ 150 mg/d. L Myocardial Infarction Ischemic Stroke Revascularization CV Death HDL-C < 50 mg/d. L TG < 150 mg/d. L TG ≥ 150 mg/d. L All CV Events 0. 5 1. 0 10 Fully adjusted HR HR using TG levels < 150 and HDL-C levels ≥ 50 mg/d. L adjusted for age, BP, smoking, hormone use, tertiles of total and HDL-C, DM, BMI & hs-CRP Bansal, S et al. JAMA. 2007; 298: 309 -316
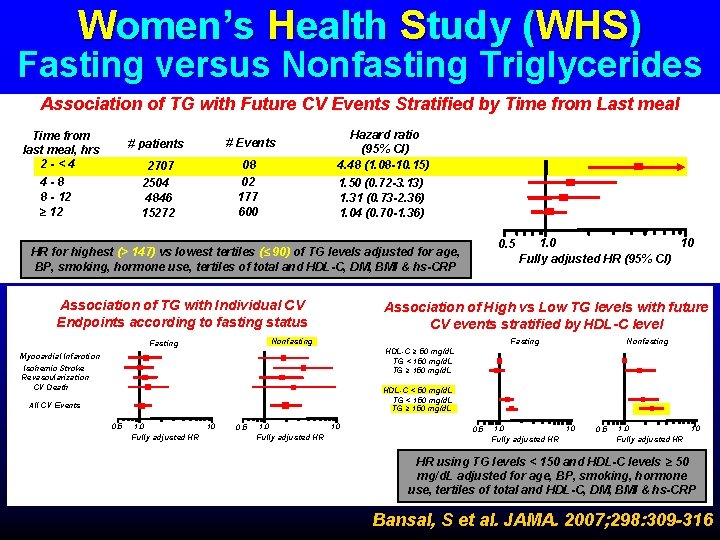
Women’s Health Study (WHS) Fasting versus Nonfasting Triglycerides Association of TG with Future CV Events Stratified by Time from Last meal Time from last meal, hrs 2 -<4 4 -8 8 - 12 ≥ 12 # patients # Events 2707 2504 4846 15272 08 02 177 600 Hazard ratio (95% CI) 4. 48 (1. 08 -10. 15) 1. 50 (0. 72 -3. 13) 1. 31 (0. 73 -2. 36) 1. 04 (0. 70 -1. 36) 0. 5 HR for highest (> 147) vs lowest tertiles (≤ 90) of TG levels adjusted for age, BP, smoking, hormone use, tertiles of total and HDL-C, DM, BMI & hs-CRP Association of TG with Individual CV Endpoints according to fasting status Association of High vs Low TG levels with future CV events stratified by HDL-C level Fasting Nonfasting Fasting 10 1. 0 Fully adjusted HR (95% CI) Nonfasting HDL-C ≥ 50 mg/d. L TG < 150 mg/d. L TG ≥ 150 mg/d. L Myocardial Infarction Ischemic Stroke Revascularization CV Death HDL-C < 50 mg/d. L TG < 150 mg/d. L TG ≥ 150 mg/d. L All CV Events 0. 5 1. 0 10 Fully adjusted HR HR using TG levels < 150 and HDL-C levels ≥ 50 mg/d. L adjusted for age, BP, smoking, hormone use, tertiles of total and HDL-C, DM, BMI & hs-CRP Bansal, S et al. JAMA. 2007; 298: 309 -316
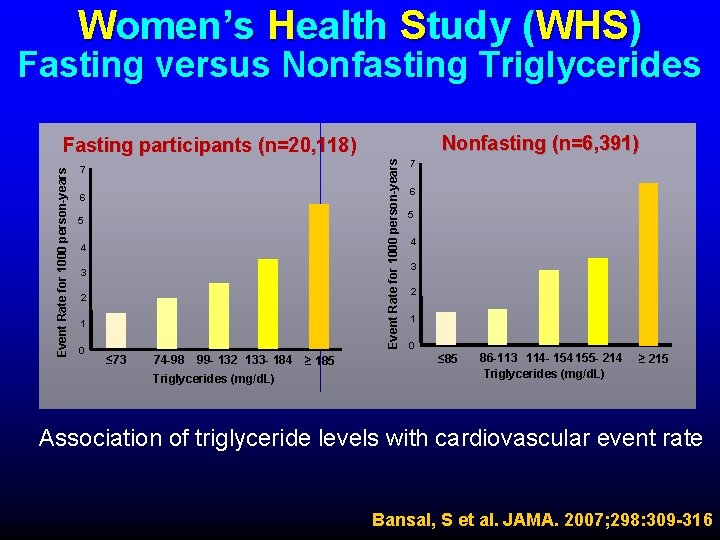
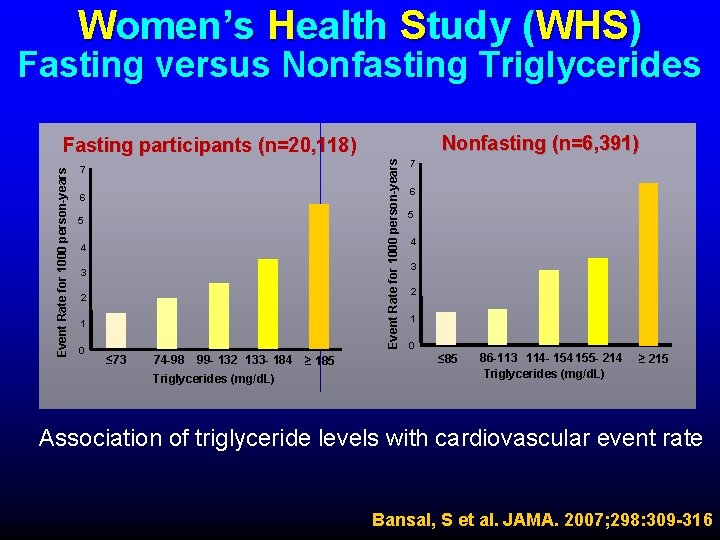
Women’s Health Study (WHS) Fasting versus Nonfasting Triglycerides Nonfasting (n=6, 391) Event Rate for 1000 person-years Fasting participants (n=20, 118) 7 6 5 4 3 2 1 0 ≤ 73 74 -98 99 - 132 133 - 184 Triglycerides (mg/d. L) ≥ 185 7 6 5 4 3 2 1 0 ≤ 85 86 -113 114 - 154 155 - 214 Triglycerides (mg/d. L) ≥ 215 Association of triglyceride levels with cardiovascular event rate Bansal, S et al. JAMA. 2007; 298: 309 -316

Women’s Health Study (WHS) IL-6, CRP and HRT relationship IL-6 (pg/ml hs-CRP mg/dl P trend < 0. 01 P trend < 0. 0002 Never Former Current Hormone Therapy Use Bermudez E et al Arterioscler Thromb Vasc Biol 2002; 22: 1668 -1673
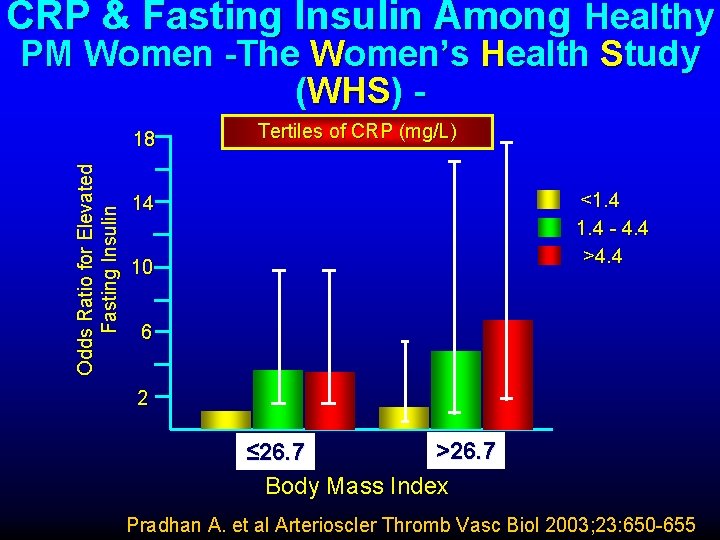
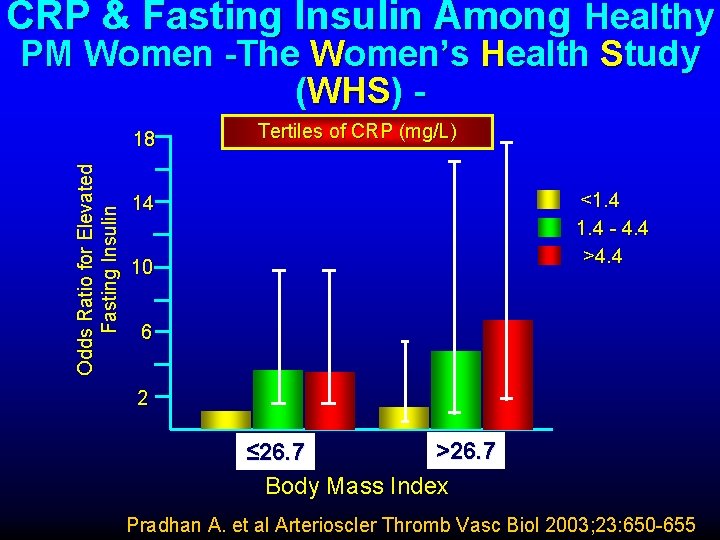
CRP & Fasting Insulin Among Healthy PM Women -The Women’s Health Study (WHS) Odds Ratio for Elevated Fasting Insulin 18 Tertiles of CRP (mg/L) <1. 4 - 4. 4 >4. 4 14 10 6 2 >26. 7 ≤ 26. 7 Body Mass Index Pradhan A. et al Arterioscler Thromb Vasc Biol 2003; 23: 650 -655
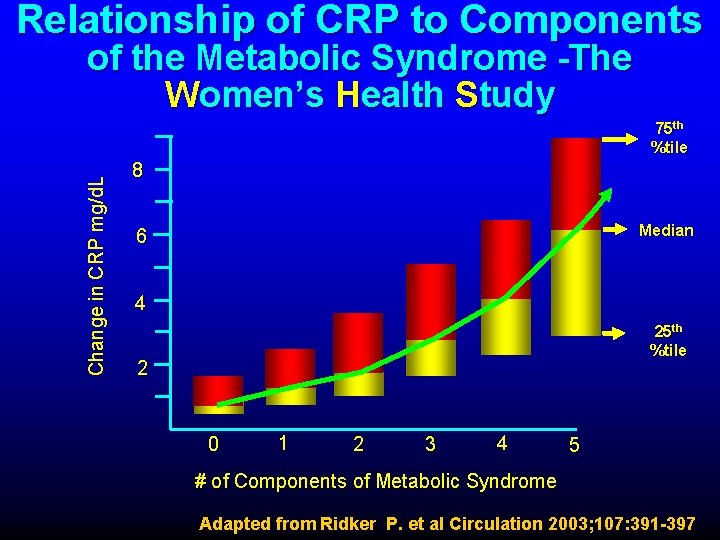
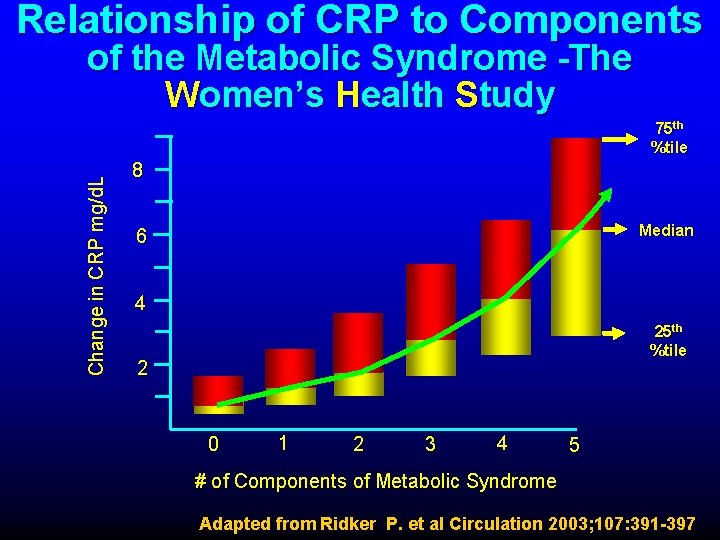
Relationship of CRP to Components of the Metabolic Syndrome -The Women’s Health Study Change in CRP mg/d. L 75 th %tile 8 Median 6 4 25 th %tile 2 0 1 2 3 4 5 # of Components of Metabolic Syndrome Adapted from Ridker P. et al Circulation 2003; 107: 391 -397
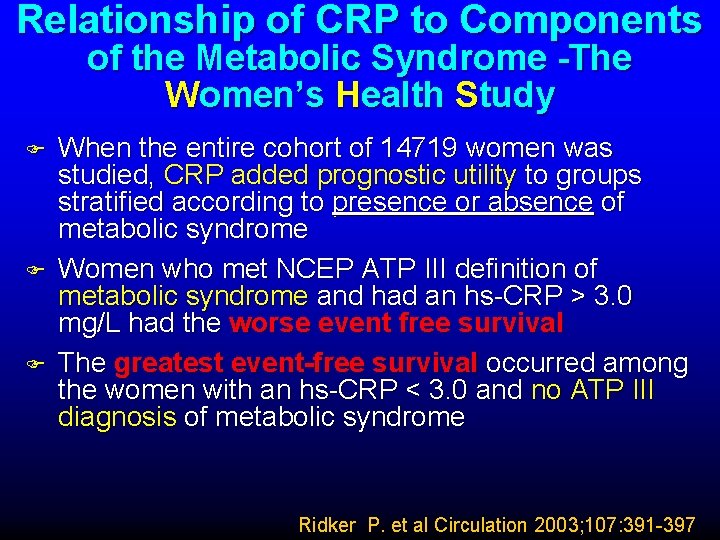
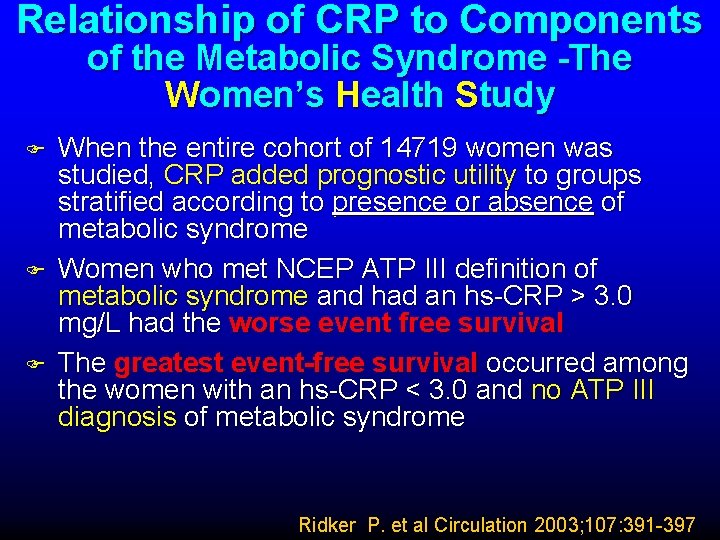
Relationship of CRP to Components of the Metabolic Syndrome -The Women’s Health Study F F F When the entire cohort of 14719 women was studied, CRP added prognostic utility to groups stratified according to presence or absence of metabolic syndrome Women who met NCEP ATP III definition of metabolic syndrome and had an hs-CRP > 3. 0 mg/L had the worse event free survival The greatest event-free survival occurred among the women with an hs-CRP < 3. 0 and no ATP III diagnosis of metabolic syndrome Ridker P. et al Circulation 2003; 107: 391 -397
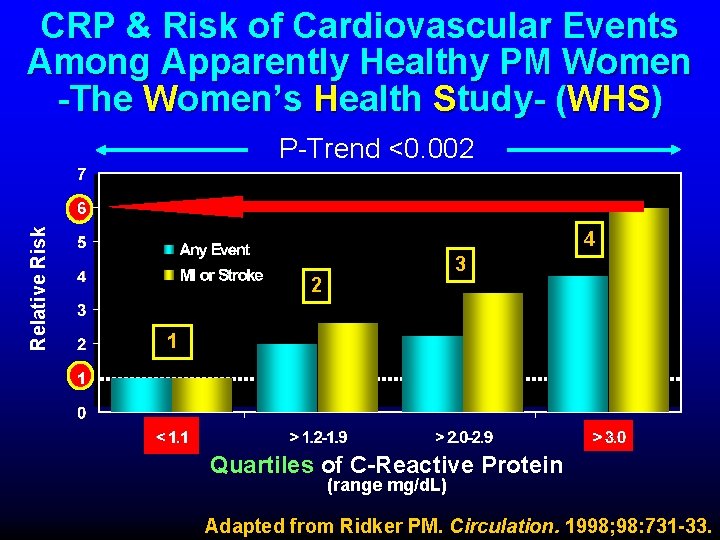
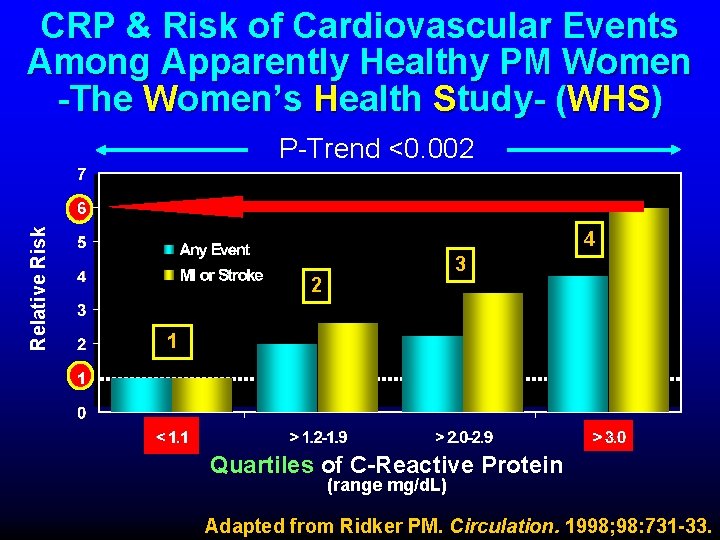
CRP & Risk of Cardiovascular Events Among Apparently Healthy PM Women -The Women’s Health Study- (WHS) Relative Risk P-Trend <0. 002 4 3 2 1 Quartiles of C-Reactive Protein (range mg/d. L) Adapted from Ridker PM. Circulation. 1998; 98: 731 -33.
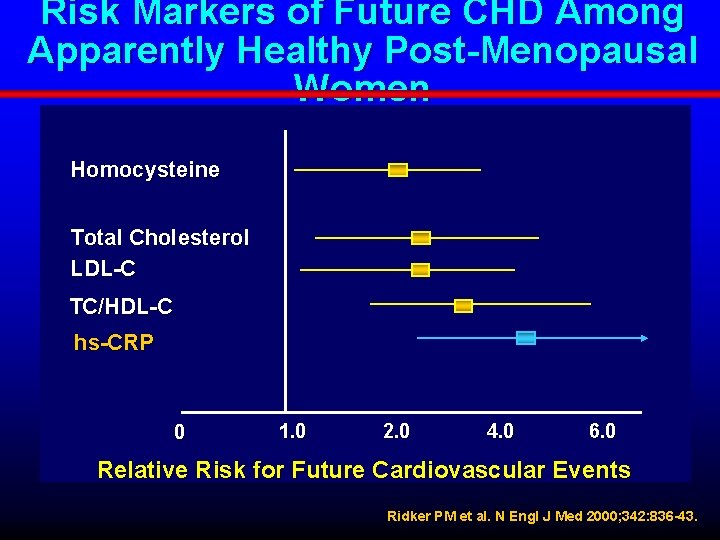
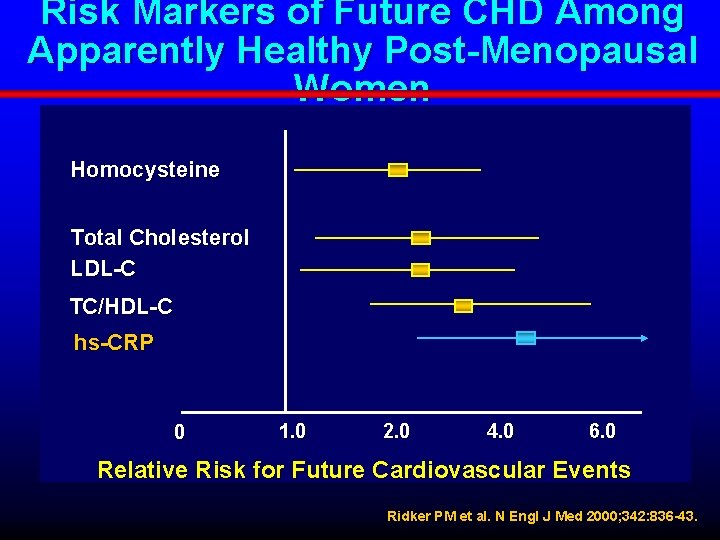
Risk Markers of Future CHD Among Apparently Healthy Post-Menopausal Women Homocysteine Total Cholesterol LDL-C TC/HDL-C hs-CRP 0 1. 0 2. 0 4. 0 6. 0 Relative Risk for Future Cardiovascular Events Ridker PM et al. N Engl J Med 2000; 342: 836 -43.
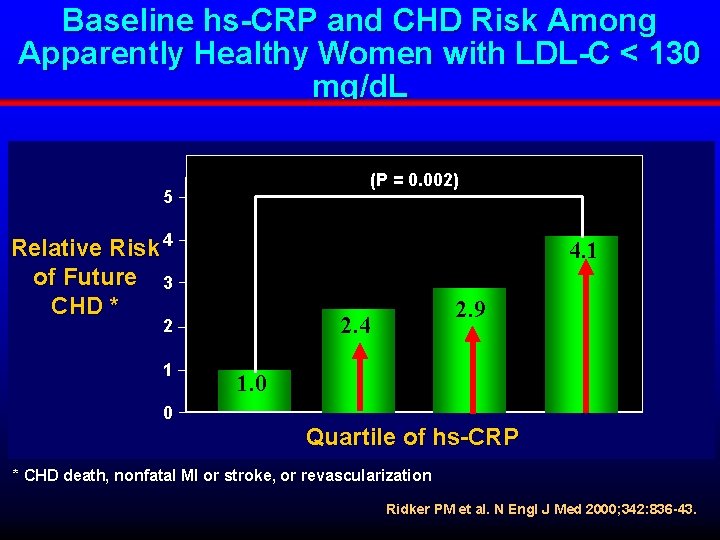
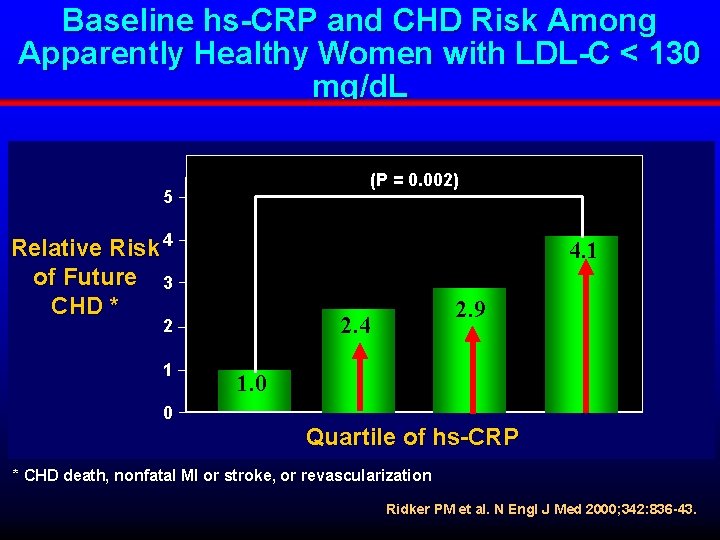
Baseline hs-CRP and CHD Risk Among Apparently Healthy Women with LDL-C < 130 mg/d. L (P = 0. 002) 5 Relative Risk 4 of Future 3 CHD * 4. 1 2. 4 2 1 0 2. 9 1. 0 Quartile of hs-CRP * CHD death, nonfatal MI or stroke, or revascularization Ridker PM et al. N Engl J Med 2000; 342: 836 -43.
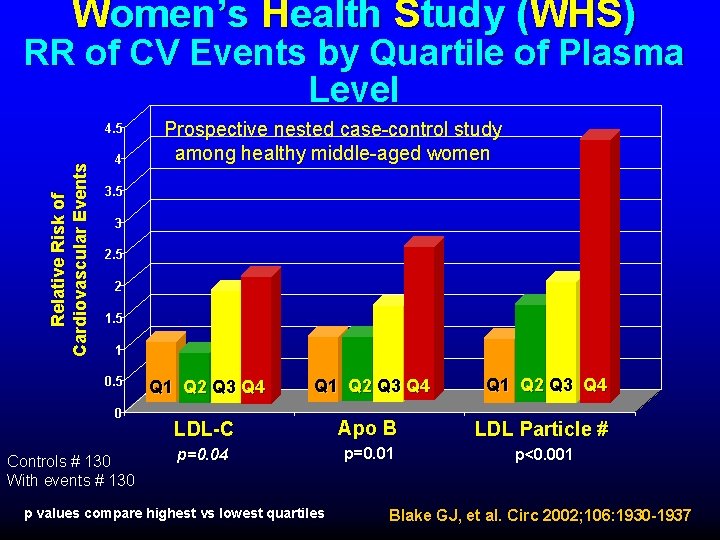
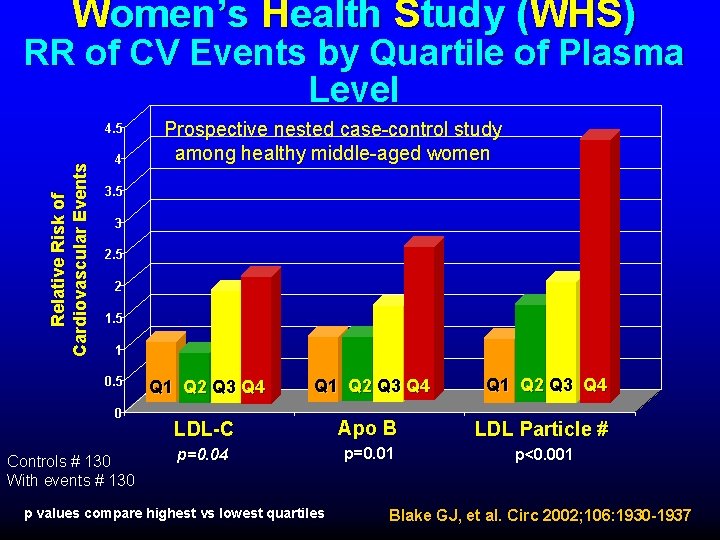
Women’s Health Study (WHS) RR of CV Events by Quartile of Plasma Level Relative Risk of Cardiovascular Events 4. 5 4 Prospective nested case-control study among healthy middle-aged women 3. 5 3 2. 5 2 1. 5 1 0. 5 0 Controls # 130 With events # 130 Q 1 Q 2 Q 3 Q 4 LDL-C Apo B LDL Particle # p=0. 04 p=0. 01 p<0. 001 p values compare highest vs lowest quartiles Blake GJ, et al. Circ 2002; 106: 1930 -1937
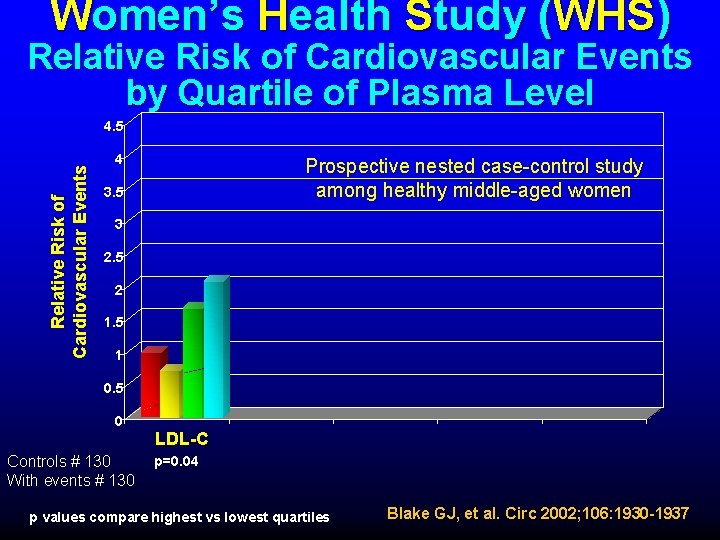
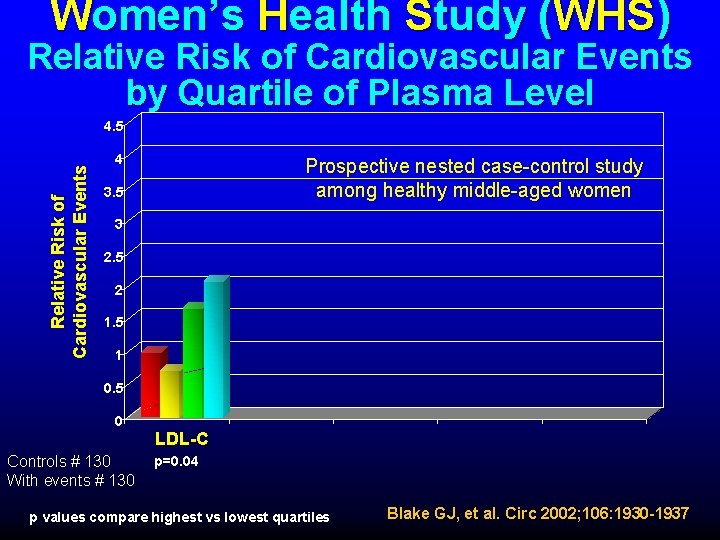
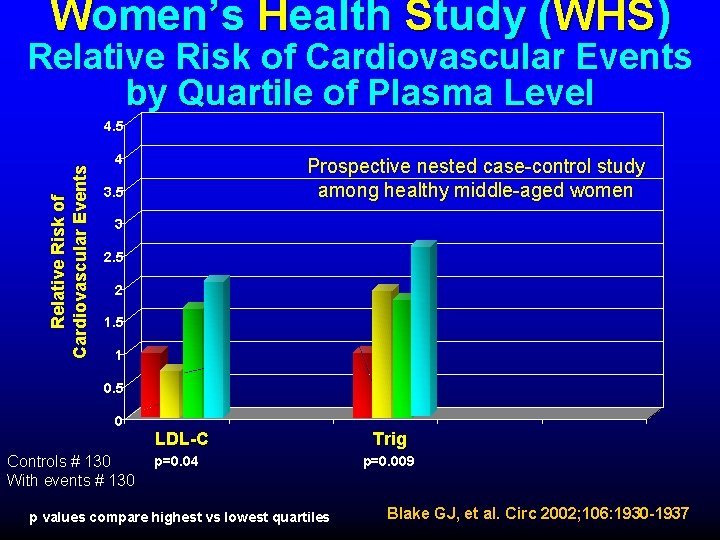
Women’s Health Study (WHS) Relative Risk of Cardiovascular Events by Quartile of Plasma Level Relative Risk of Cardiovascular Events 4. 5 4 Prospective nested case-control study among healthy middle-aged women 3. 5 3 2. 5 2 1. 5 1 0. 5 0 LDL-C Controls # 130 With events # 130 p=0. 04 p values compare highest vs lowest quartiles Blake GJ, et al. Circ 2002; 106: 1930 -1937
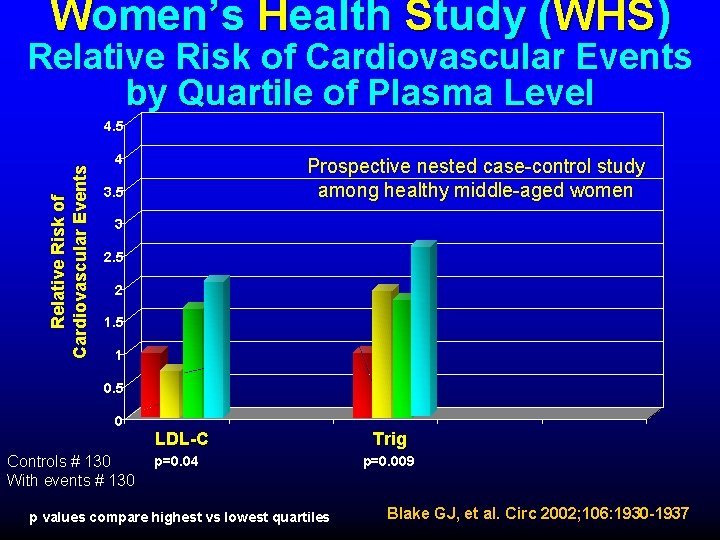
Women’s Health Study (WHS) Relative Risk of Cardiovascular Events by Quartile of Plasma Level Relative Risk of Cardiovascular Events 4. 5 4 Prospective nested case-control study among healthy middle-aged women 3. 5 3 2. 5 2 1. 5 1 0. 5 0 LDL-C Controls # 130 With events # 130 p=0. 04 p values compare highest vs lowest quartiles Trig p=0. 009 Blake GJ, et al. Circ 2002; 106: 1930 -1937
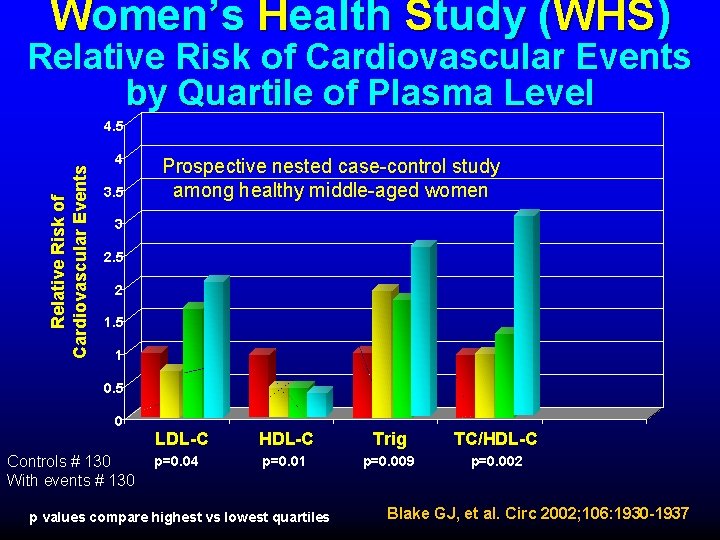
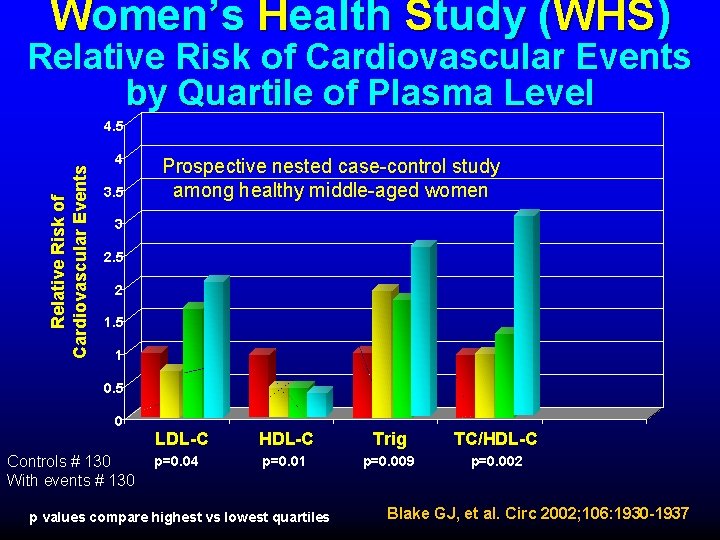
Women’s Health Study (WHS) Relative Risk of Cardiovascular Events by Quartile of Plasma Level Relative Risk of Cardiovascular Events 4. 5 4 3. 5 Prospective nested case-control study among healthy middle-aged women 3 2. 5 2 1. 5 1 0. 5 0 Controls # 130 With events # 130 LDL-C HDL-C Trig TC/HDL-C p=0. 04 p=0. 01 p=0. 009 p=0. 002 p values compare highest vs lowest quartiles Blake GJ, et al. Circ 2002; 106: 1930 -1937
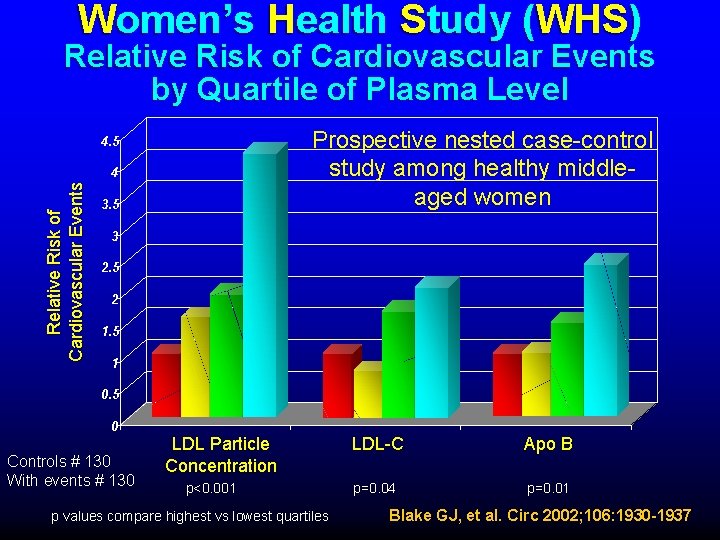
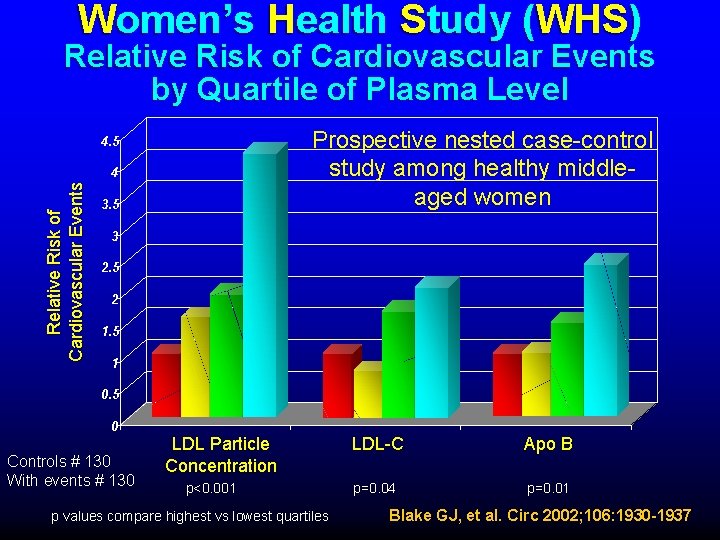
Women’s Health Study (WHS) Relative Risk of Cardiovascular Events by Quartile of Plasma Level Prospective nested case-control study among healthy middleaged women 4. 5 Relative Risk of Cardiovascular Events 4 3. 5 3 2. 5 2 1. 5 1 0. 5 0 Controls # 130 With events # 130 LDL Particle Concentration p<0. 001 p values compare highest vs lowest quartiles LDL-C Apo B p=0. 04 p=0. 01 Blake GJ, et al. Circ 2002; 106: 1930 -1937
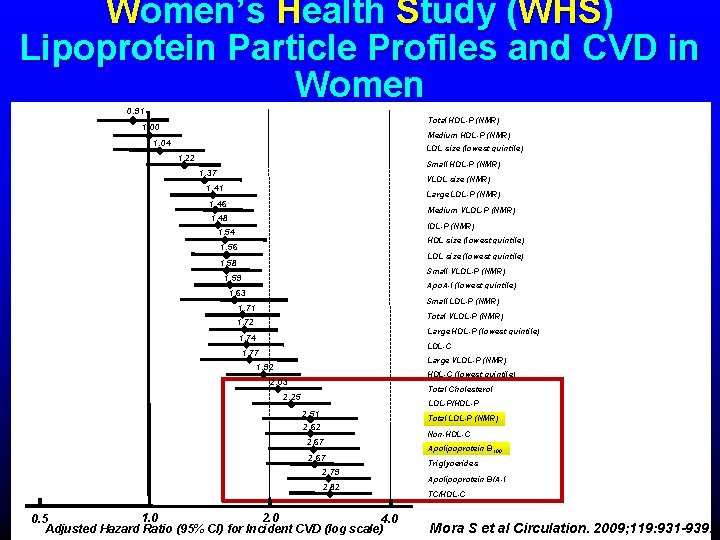
Mora S et al Circulation. 2009; 119: 931 -939.
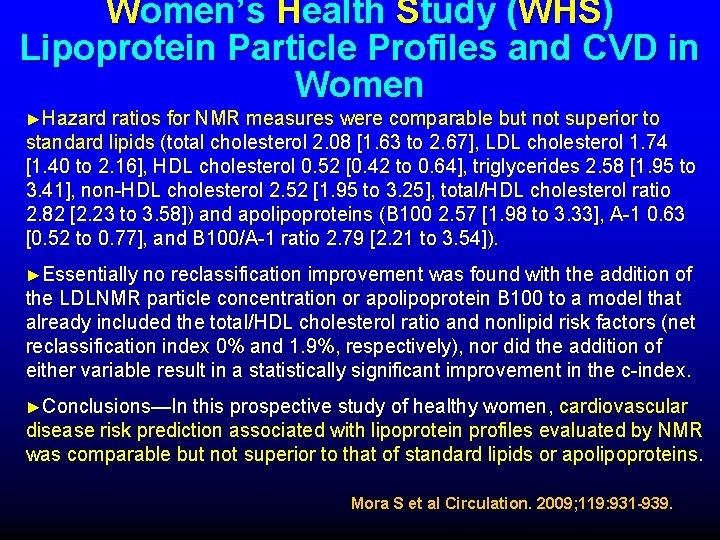
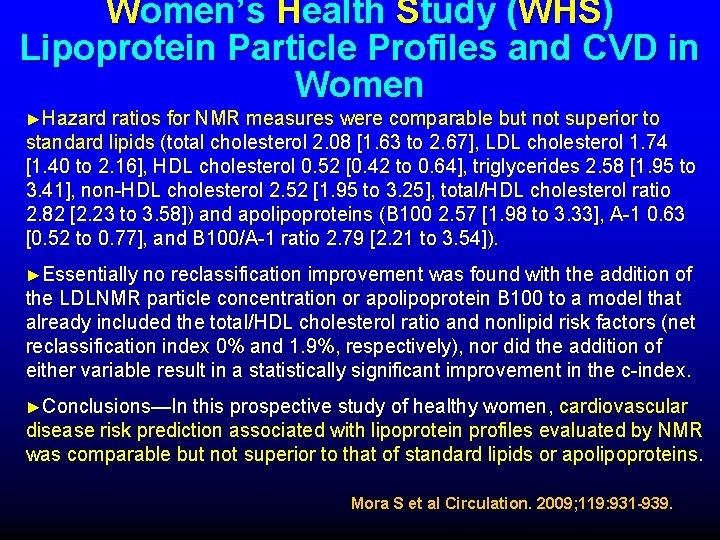
Women’s Health Study (WHS) Lipoprotein Particle Profiles and CVD in Women ►Hazard ratios for NMR measures were comparable but not superior to standard lipids (total cholesterol 2. 08 [1. 63 to 2. 67], LDL cholesterol 1. 74 [1. 40 to 2. 16], HDL cholesterol 0. 52 [0. 42 to 0. 64], triglycerides 2. 58 [1. 95 to 3. 41], non-HDL cholesterol 2. 52 [1. 95 to 3. 25], total/HDL cholesterol ratio 2. 82 [2. 23 to 3. 58]) and apolipoproteins (B 100 2. 57 [1. 98 to 3. 33], A-1 0. 63 [0. 52 to 0. 77], and B 100/A-1 ratio 2. 79 [2. 21 to 3. 54]). ►Essentially no reclassification improvement was found with the addition of the LDLNMR particle concentration or apolipoprotein B 100 to a model that already included the total/HDL cholesterol ratio and nonlipid risk factors (net reclassification index 0% and 1. 9%, respectively), nor did the addition of either variable result in a statistically significant improvement in the c-index. ►Conclusions—In this prospective study of healthy women, cardiovascular disease risk prediction associated with lipoprotein profiles evaluated by NMR was comparable but not superior to that of standard lipids or apolipoproteins. Mora S et al Circulation. 2009; 119: 931 -939.
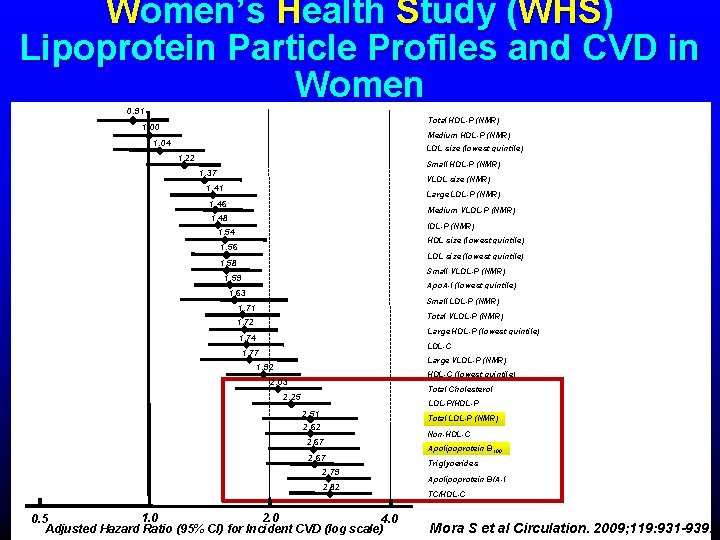
Women’s Health Study (WHS) Lipoprotein Particle Profiles and CVD in Women 0. 91 Total HDL-P (NMR) 1. 00 Medium HDL-P (NMR) 1. 04 LDL size (lowest quintile) 1. 22 Small HDL-P (NMR) 1. 37 VLDL size (NMR) 1. 41 Large LDL-P (NMR) 1. 46 Medium VLDL-P (NMR) 1. 48 IDL-P (NMR) 1. 54 HDL size (lowest quintile) 1. 56 LDL size (lowest quintile) 1. 58 Small VLDL-P (NMR) 1. 59 Apo. A-I (lowest quintile) 1. 63 Small LDL-P (NMR) 1. 71 Total VLDL-P (NMR) 1. 72 Large HDL-P (lowest quintile) 1. 74 LDL-C 1. 77 Large VLDL-P (NMR) 1. 92 HDL-C (lowest quintile) 2. 03 Total Cholesterol 2. 25 LDL-P/HDL-P 2. 51 Total LDL-P (NMR) 2. 62 2. 67 2. 79 2. 82 2. 0 1. 0 0. 5 4. 0 Adjusted Hazard Ratio (95% CI) for Incident CVD (log scale) Non-HDL-C Apolipoprotein B 100 Triglycerides Apolipoprotein B/A-I TC/HDL-C Mora S et al Circulation. 2009; 119: 931 -939.
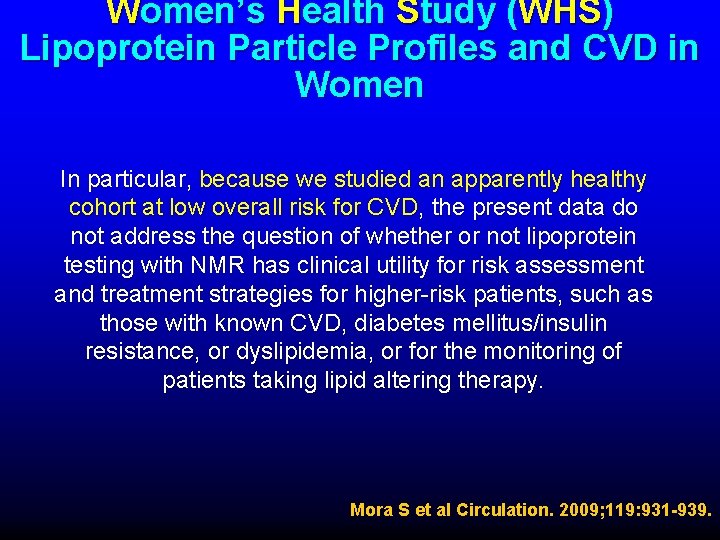
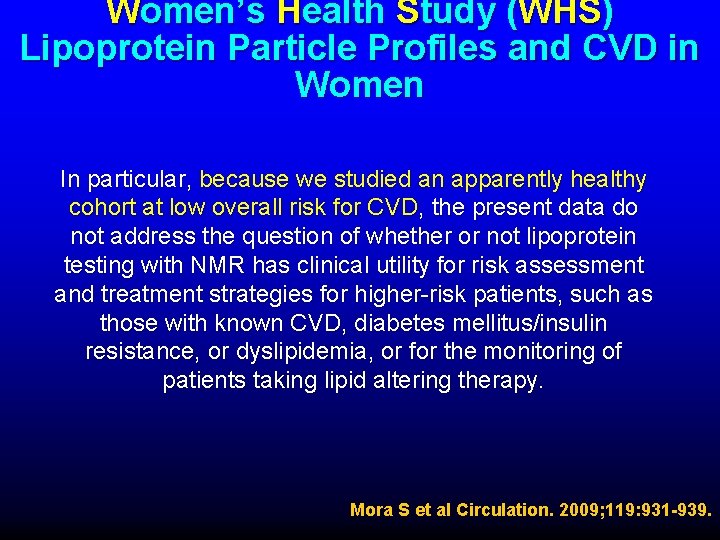
Women’s Health Study (WHS) Lipoprotein Particle Profiles and CVD in Women In particular, because we studied an apparently healthy cohort at low overall risk for CVD, the present data do not address the question of whether or not lipoprotein testing with NMR has clinical utility for risk assessment and treatment strategies for higher-risk patients, such as those with known CVD, diabetes mellitus/insulin resistance, or dyslipidemia, or for the monitoring of patients taking lipid altering therapy. Mora S et al Circulation. 2009; 119: 931 -939.
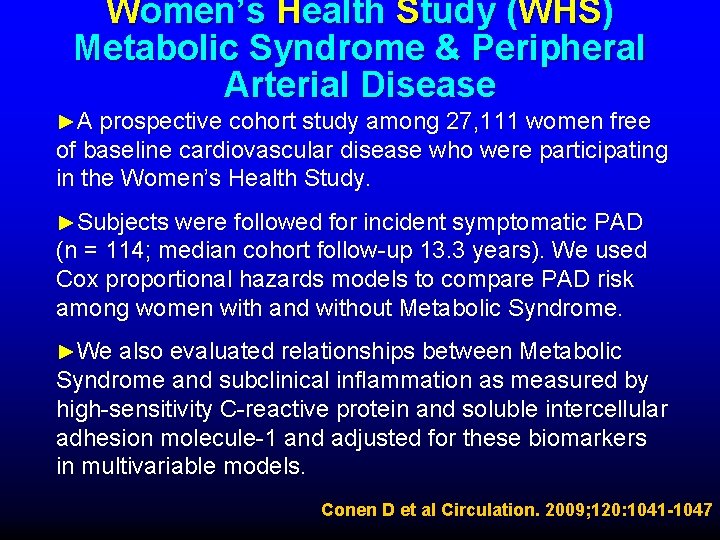
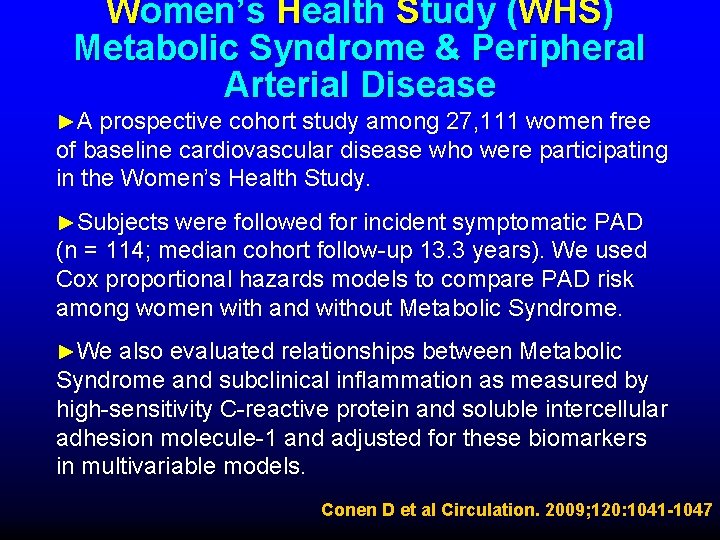
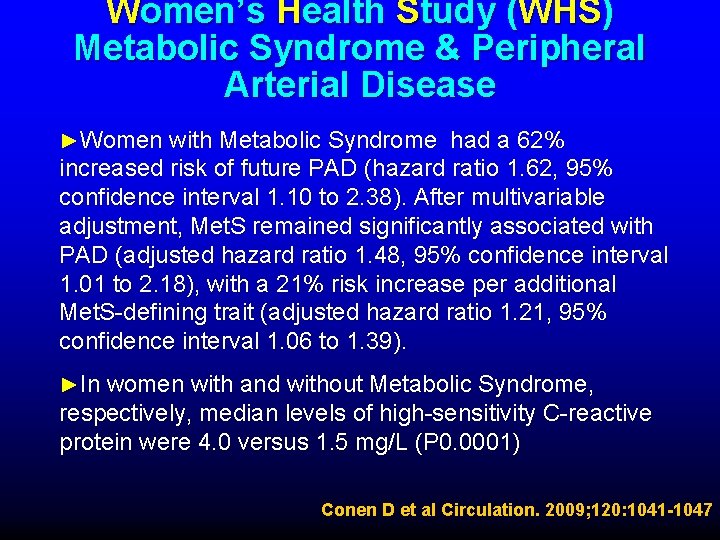
Women’s Health Study (WHS) Metabolic Syndrome & Peripheral Arterial Disease ►A prospective cohort study among 27, 111 women free of baseline cardiovascular disease who were participating in the Women’s Health Study. ►Subjects were followed for incident symptomatic PAD (n = 114; median cohort follow-up 13. 3 years). We used Cox proportional hazards models to compare PAD risk among women with and without Metabolic Syndrome. ►We also evaluated relationships between Metabolic Syndrome and subclinical inflammation as measured by high-sensitivity C-reactive protein and soluble intercellular adhesion molecule-1 and adjusted for these biomarkers in multivariable models. Conen D et al Circulation. 2009; 120: 1041 -1047
Women’s Health Study (WHS) Metabolic Syndrome & Peripheral Arterial Disease ►Women with Metabolic Syndrome had a 62% increased risk of future PAD (hazard ratio 1. 62, 95% confidence interval 1. 10 to 2. 38). After multivariable adjustment, Met. S remained significantly associated with PAD (adjusted hazard ratio 1. 48, 95% confidence interval 1. 01 to 2. 18), with a 21% risk increase per additional Met. S-defining trait (adjusted hazard ratio 1. 21, 95% confidence interval 1. 06 to 1. 39). ►In women with and without Metabolic Syndrome, respectively, median levels of high-sensitivity C-reactive protein were 4. 0 versus 1. 5 mg/L (P 0. 0001) Conen D et al Circulation. 2009; 120: 1041 -1047
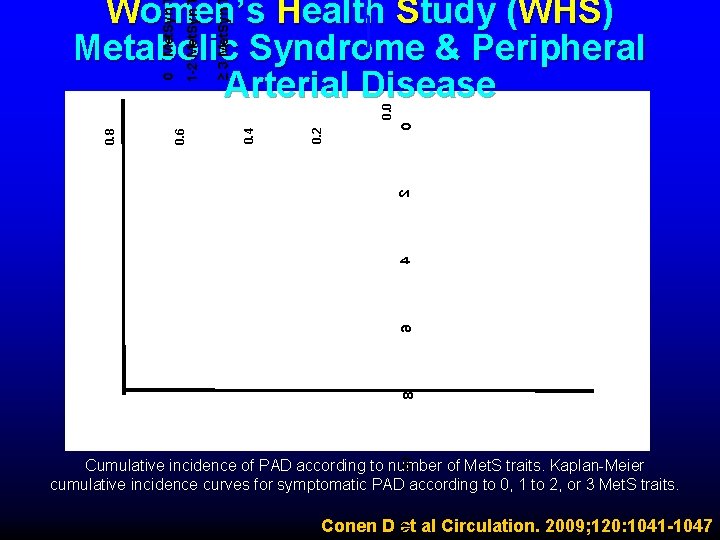
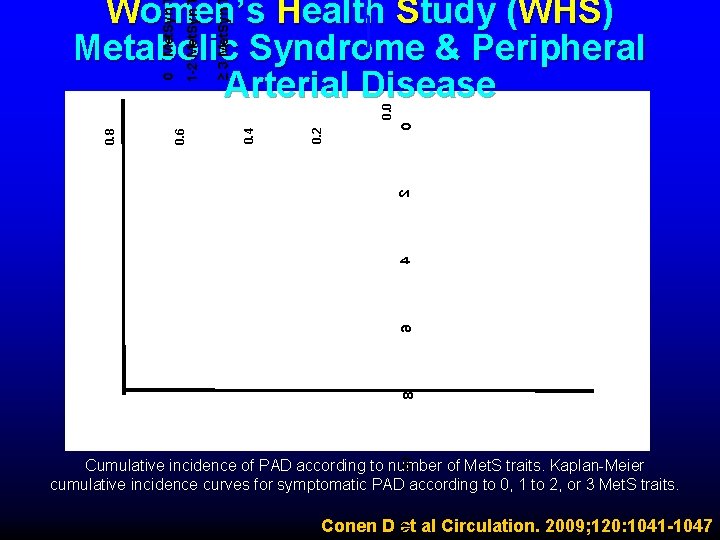
0 01 8 6 4 2 0. 4 0. 6 0. 8 0. 0 ≥ 3 Met. Syn 1 -2 Met. Syn 0 Met. Syn Women’s Health Study (WHS) Metabolic Syndrome & Peripheral Arterial Disease Cumulative incidence of PAD according to number of Met. S traits. Kaplan-Meier cumulative incidence curves for symptomatic PAD according to 0, 1 to 2, or 3 Met. S traits. 21 Conen D et al Circulation. 2009; 120: 1041 -1047
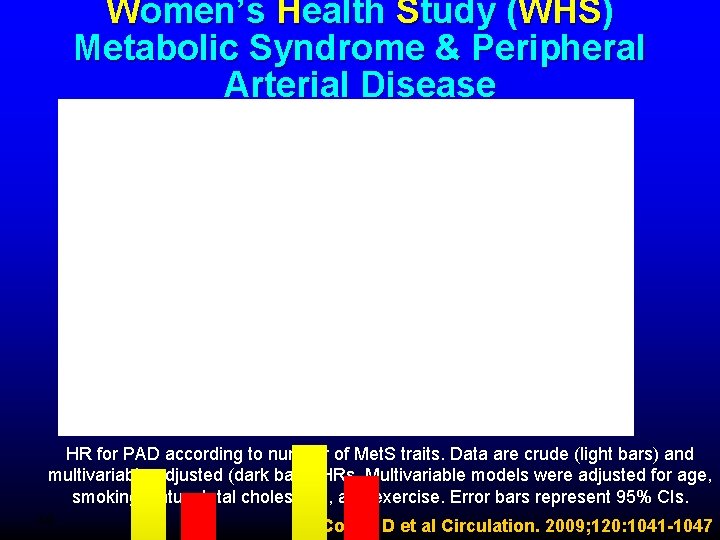
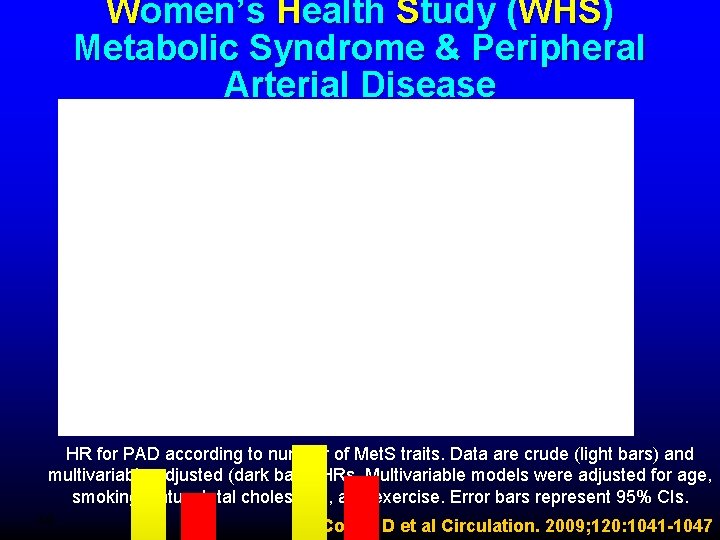
0 Women’s Health Study (WHS) Metabolic Syndrome & Peripheral Arterial Disease HR for PAD according to number of Met. S traits. Data are crude (light bars) and multivariable-adjusted (dark bars) HRs. Multivariable models were adjusted for age, smoking status, total cholesterol, and exercise. Error bars represent 95% CIs. 3. 0 Conen D et al Circulation. 2009; 120: 1041 -1047
Women’s Health Study (WHS) Metabolic Syndrome & Peripheral Arterial Disease Similar to the previously noted relationship between Metabolic Syndrome and incident coronary heart disease and stroke, the present study demonstrated a modest positive association with future PAD in a population of otherwise low-risk women. Substantially increased plasma levels of hs-CRP and s. ICAM-1 were evident in subjects with Met. Syn, and a strong influence of these factors on the relationship between Met. Syn and PAD was noted, suggesting a possible pathophysiological role. Conen D et al Circulation. 2009; 120: 1041 -1047
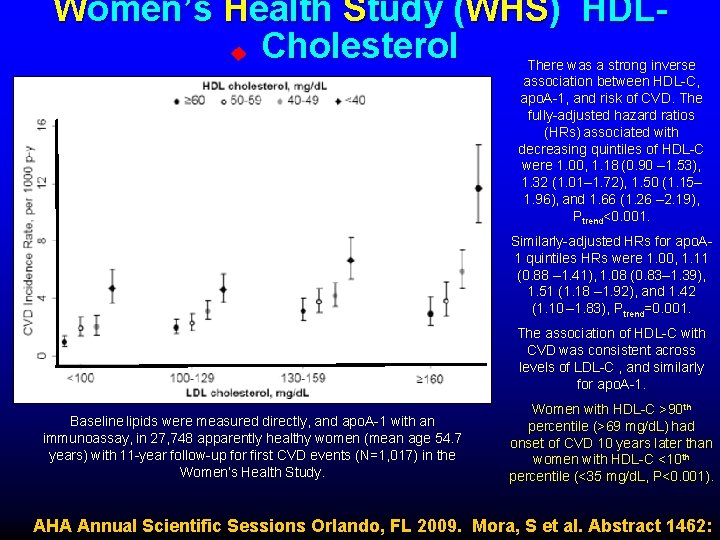
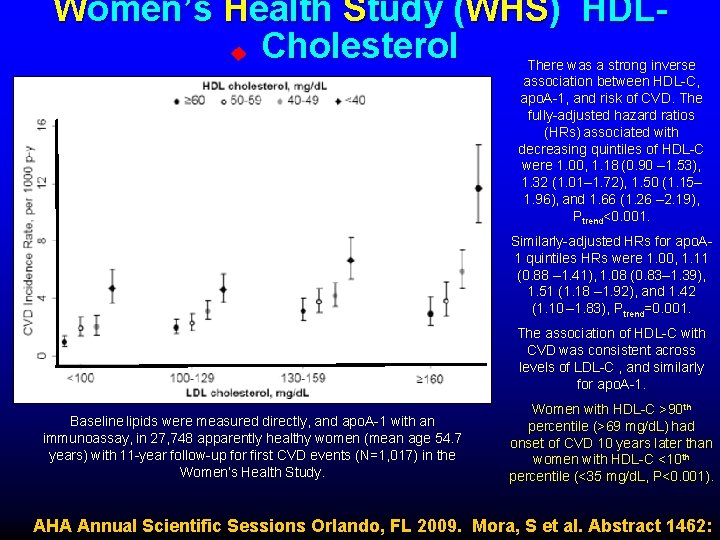
Women’s Health Study (WHS) HDLCholesterol There was a strong inverse association between HDL-C, apo. A-1, and risk of CVD. The fully-adjusted hazard ratios (HRs) associated with decreasing quintiles of HDL-C were 1. 00, 1. 18 (0. 90 – 1. 53), 1. 32 (1. 01– 1. 72), 1. 50 (1. 15– 1. 96), and 1. 66 (1. 26 – 2. 19), Ptrend<0. 001. Similarly-adjusted HRs for apo. A 1 quintiles HRs were 1. 00, 1. 11 (0. 88 – 1. 41), 1. 08 (0. 83– 1. 39), 1. 51 (1. 18 – 1. 92), and 1. 42 (1. 10 – 1. 83), Ptrend=0. 001. The association of HDL-C with CVD was consistent across levels of LDL-C , and similarly for apo. A-1. Baseline lipids were measured directly, and apo. A-1 with an immunoassay, in 27, 748 apparently healthy women (mean age 54. 7 years) with 11 -year follow-up for first CVD events (N=1, 017) in the Women’s Health Study. Women with HDL-C >90 th percentile (>69 mg/d. L) had onset of CVD 10 years later than women with HDL-C <10 th percentile (<35 mg/d. L, P<0. 001). AHA Annual Scientific Sessions Orlando, FL 2009. Mora, S et al. Abstract 1462:
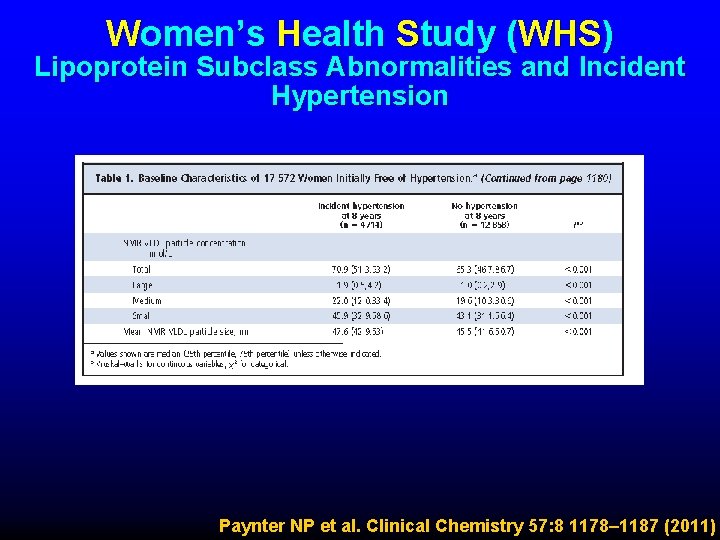
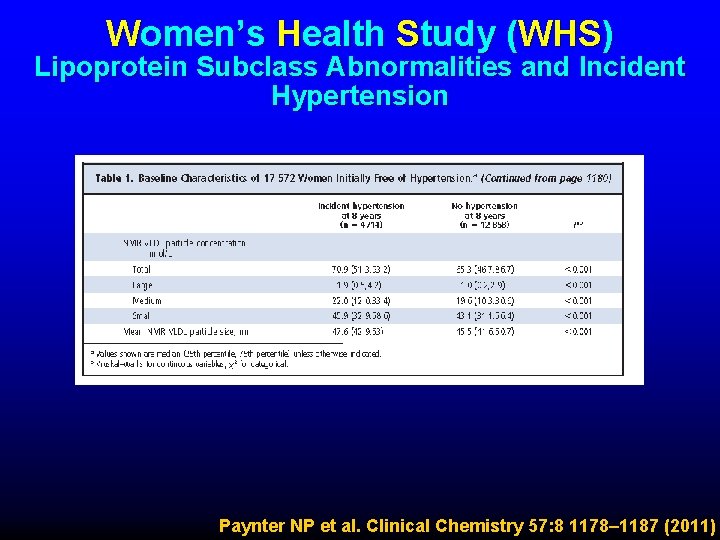
Women’s Health Study (WHS) Lipoprotein Subclass Abnormalities and Incident Hypertension Paynter NP et al. Clinical Chemistry 57: 8 1178– 1187 (2011)
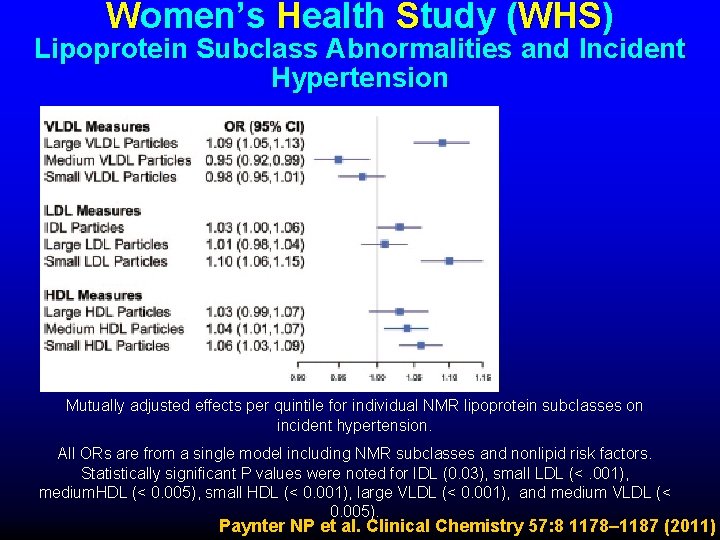
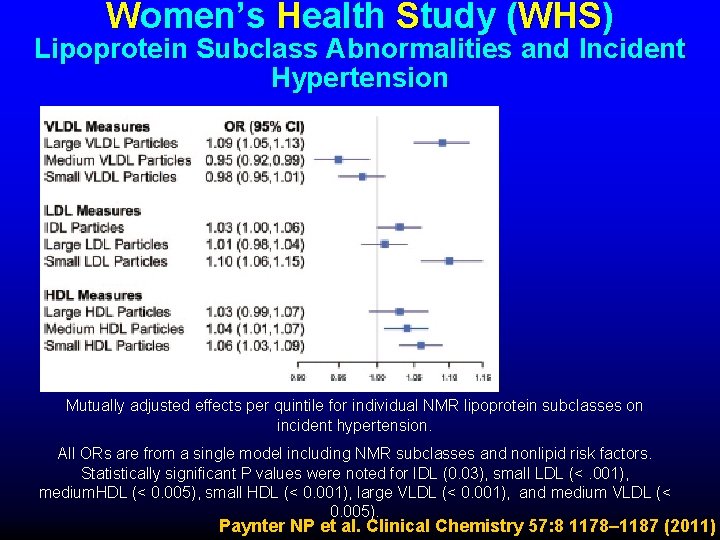
Women’s Health Study (WHS) Lipoprotein Subclass Abnormalities and Incident Hypertension Mutually adjusted effects per quintile for individual NMR lipoprotein subclasses on incident hypertension. All ORs are from a single model including NMR subclasses and nonlipid risk factors. Statistically significant P values were noted for IDL (0. 03), small LDL (<. 001), medium. HDL (< 0. 005), small HDL (< 0. 001), large VLDL (< 0. 001), and medium VLDL (< 0. 005). Paynter NP et al. Clinical Chemistry 57: 8 1178– 1187 (2011)
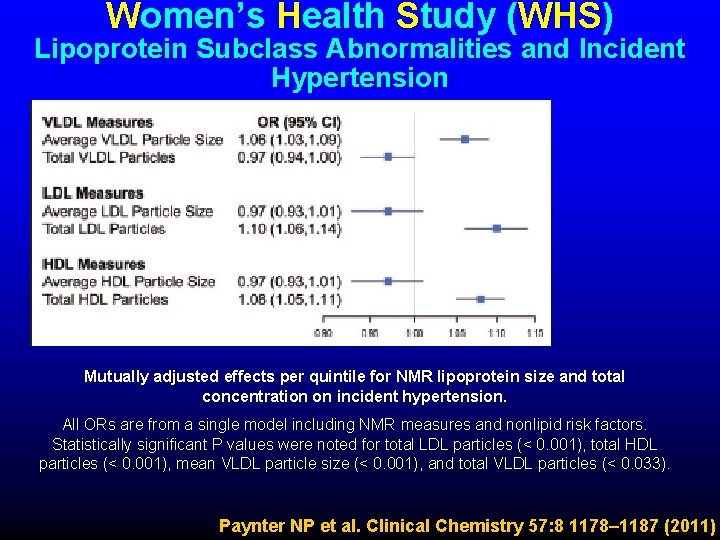
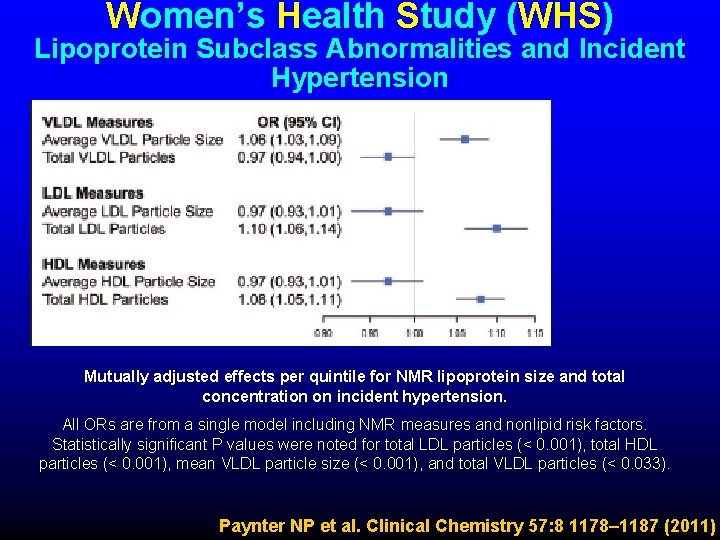
Women’s Health Study (WHS) Lipoprotein Subclass Abnormalities and Incident Hypertension Mutually adjusted effects per quintile for NMR lipoprotein size and total concentration on incident hypertension. All ORs are from a single model including NMR measures and nonlipid risk factors. Statistically significant P values were noted for total LDL particles (< 0. 001), total HDL particles (< 0. 001), mean VLDL particle size (< 0. 001), and total VLDL particles (< 0. 033). Paynter NP et al. Clinical Chemistry 57: 8 1178– 1187 (2011)
Women’s Health Study (WHS) Lipoprotein Subclass Abnormalities and Incident Hypertension ► In summary, among initially healthy women, lipoprotein particle size and subclass concentrations were associated with incident hypertension and provided additive information to traditional lipids and risk factors. ► Greater risk of hypertension was associated with higher total concentrations of LDL and HDL particles, especially small particles, and higher total concentration of VLDL particles, especially large particles. ► In addition, findings suggest that the concentrations and size of lipoprotein particles affect the risk of incident hypertension years before the clinical onset of hypertension, even in women with initially normal blood pressure. Paynter NP et al. Clinical Chemistry 57: 8 1178– 1187 (2011)
Women’s Health Study (WHS) High Density Lipoprotein Cholesterol Conclusion: Consistent inverse associations were found for HDL-C with incident coronary events among women with a range of LDL-C values. Among women with low total atherogenic particle burden (apolipoprotein B 100 level 0. 90 g/L), few events occurred and no associations were seen. Mora S et al. Ann Intern Med. 2011; 155: 742 -750.
Women’s Health Study (WHS) High Density Lipoprotein Cholesterol ► Participants: 26, 861 initially healthy women, aged 45 years or older at study entry (1992– 1995), who were followed for a mean of approximately 11 years. ► In multivariable analyses, HDL-C and apolipoprotein A-I levels were inversely associated with CVD and coronary events but not stroke. Mora S et al. Ann Intern Med. 2011; 155: 742 -750.
Women’s Health Study (WHS) High Density Lipoprotein Cholesterol ► ► Adjusted coronary hazard ratios for decreasing quintiles of HDL-C were 1. 00 (reference), ► 1. 23 (95% CI, 0. 85 to 1. 78), ► 1. 42 (CI, 0. 98 to 2. 06), ► 1. 90 (CI, 1. 33 to 2. 71), and ► 2. 19 (CI, 1. 51 to 3. 19) (P for linear trend 0. 001); Corresponding hazard ratios for apolipoprotein A-I were 1. 00 (reference), ► 0. 98 (CI, 0. 71 to 1. 35), ► 1. 02 (CI, 0. 72 to 1. 44), ► 1. 37 (CI, 0. 98 to 1. 90), and ► 1. 58 (CI, 1. 14 to 2. 20) (P for linear trend 0. 005). Mora S et al. Ann Intern Med. 2011; 155: 742 -750.
Women’s Health Study (WHS) High Density Lipoprotein Cholesterol ► Consistent inverse associations were found for HDL-C with coronary events across a range of LDL-C values, including among women with low LDL-C levels. ► No associations were noted for HDL-C or apolipoprotein A-I among women with low apolipoprotein B 100 values (0. 90 g/L). Mora S et al. Ann Intern Med. 2011; 155: 742 -750.
Women’s Health Study (WHS) High Density Lipoprotein Cholesterol ► Women with very high HDL-C concentrations were not immune to CVD. However, compared with women who had low HDL-C concentrations, they were at lower risk for incident CVD and had first CVD events at older ages. ► In contrast to a study that found increased risk for CVD when HDL-C levels were greater than 80 mg/d. L, we found reduced risk at the highest levels of HDL-C in these healthy women. ► Furthermore, women with very high HDL-C who experienced events had concomitantly higher prevalence of other risk factors that may have overridden the beneficial effects of a high HDL-C value. Mora S et al. Ann Intern Med. 2011; 155: 742 -750.
Women’s Health Study (WHS) High Density Lipoprotein Cholesterol ► HDL-C level can be increased naturally (by as much as 20% to 30%) through nonpharmacologic modifications that include weight loss, aerobic exercise, tobacco cessation, and healthy dietary choices. ► Compared with men, women may sustain even greater HDLC increases by participating in regular exercise programs for extended periods. Mora S et al. Ann Intern Med. 2011; 155: 742 -750.
 Thomas dayspring
Thomas dayspring Thomas dayspring
Thomas dayspring Study whs
Study whs Tom dayspring lipids
Tom dayspring lipids Ian ramsey ce academy
Ian ramsey ce academy Wwusd
Wwusd Confidence interval assumptions
Confidence interval assumptions Model whs act
Model whs act The elements of a swms (safe work method statement)
The elements of a swms (safe work method statement) Needs of adolescence
Needs of adolescence Womens rights
Womens rights Late night womens hour
Late night womens hour Aylesbury womens aid
Aylesbury womens aid Womens right
Womens right Difference between mens and womens soccer
Difference between mens and womens soccer Womens college kumbakonam
Womens college kumbakonam Womens college kumbakonam
Womens college kumbakonam Womens right
Womens right Womens shelter edmonton
Womens shelter edmonton Womens rights
Womens rights Anatomy of woman
Anatomy of woman Womens history month door
Womens history month door Womens community shelters
Womens community shelters Ballybeen womens centre
Ballybeen womens centre Scarborough womens centre
Scarborough womens centre Headgear
Headgear Bristol womens voice
Bristol womens voice Pathologist and anthropologist
Pathologist and anthropologist Thomas snyder mental health
Thomas snyder mental health What is case series
What is case series Retrospective cohort study
Retrospective cohort study Process of method study
Process of method study Marty lobdel
Marty lobdel Phytogeographical zones of india
Phytogeographical zones of india Time study objectives
Time study objectives Distinguish between time study and motion study
Distinguish between time study and motion study Health professionals follow-up study
Health professionals follow-up study Verna and sam case study
Verna and sam case study Role of community health nurse in occupational health
Role of community health nurse in occupational health National programs
National programs Health standards louisiana
Health standards louisiana Differences between health promotion and health education
Differences between health promotion and health education