Vaginal Hysterectomy Modified Safe Technique Professor Galal Lotfi








- Slides: 34
Vaginal Hysterectomy: Modified Safe Technique Professor Galal Lotfi, MD, MRCOG Obstetrics & Gynecology Suez Canal University Egypt

Suez Canal University Hospital
Aim? • This is not a comparison between vaginal and abdominal Hyst. • This is not a comparison between vaginal and laparoscopic Hyst.
Aim Of That Work • Reviving, a Well Known Technique for Hysterectomy. • Implementing a Technique, Safe Without the Tragic Vault prolapse.
Material and Methods • Women for hysterectomy. • No prolapse. • No contraindication for vaginal hyst.
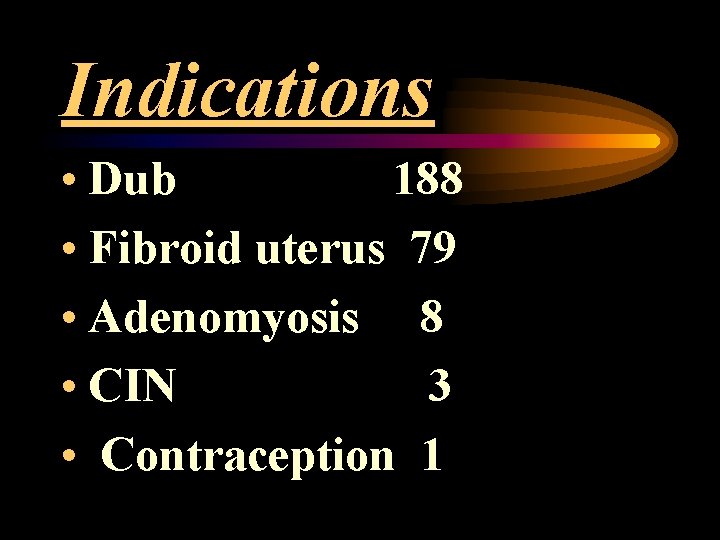
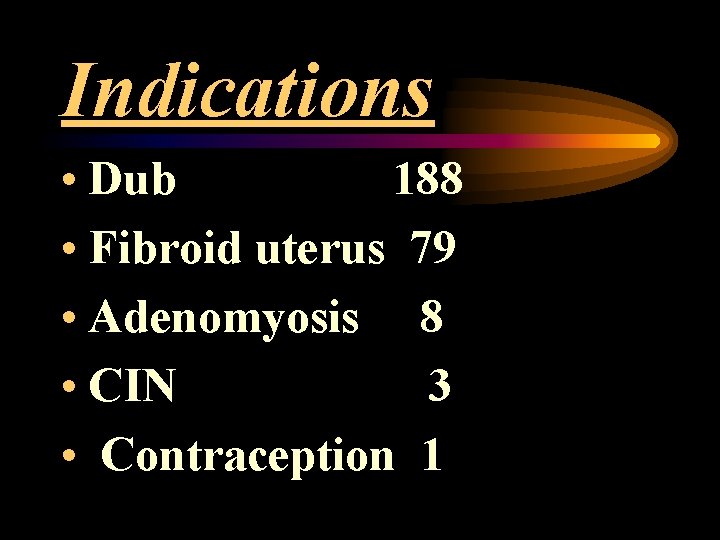
Indications • Dub 188 • Fibroid uterus 79 • Adenomyosis 8 • CIN 3 • Contraception 1
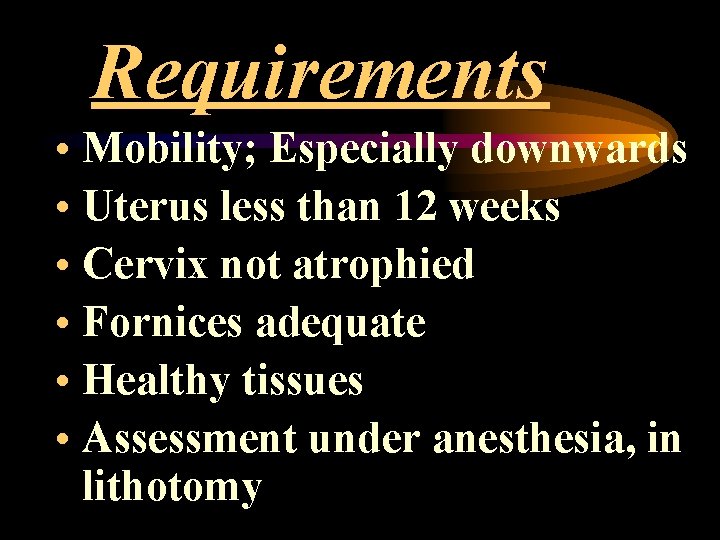
Requirements • Mobility; Especially downwards • Uterus less than 12 weeks • Cervix not atrophied • Fornices adequate • Healthy tissues • Assessment under anesthesia, in lithotomy
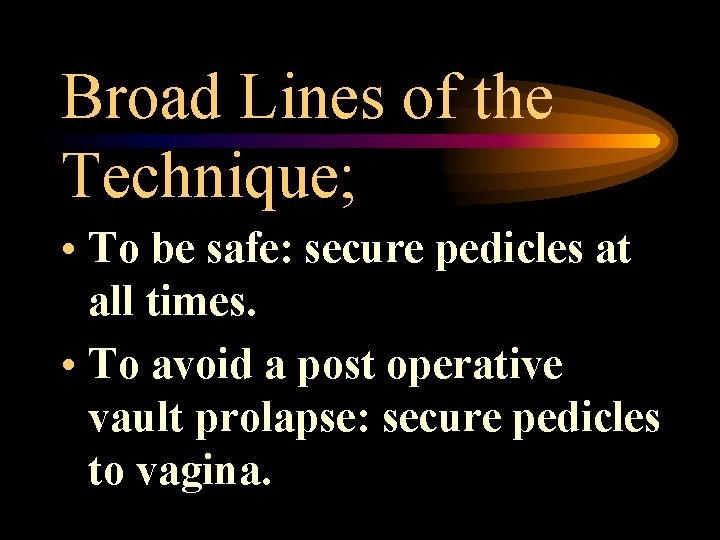
Broad Lines of the Technique; • To be safe: secure pedicles at all times. • To avoid a post operative vault prolapse: secure pedicles to vagina.
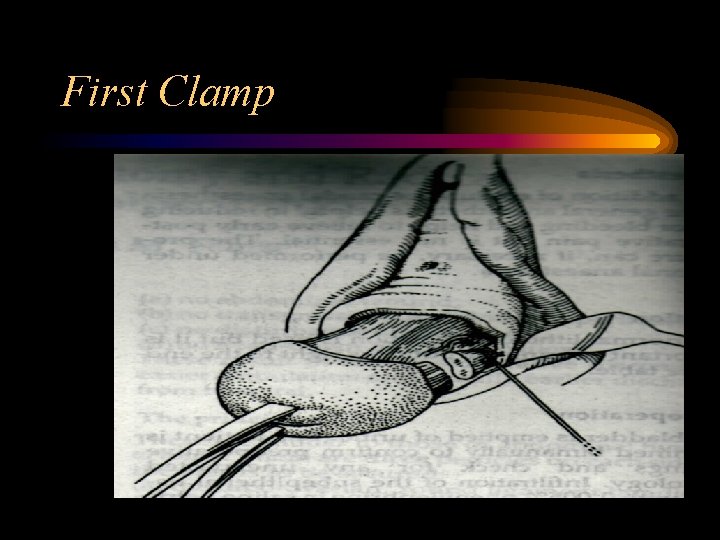
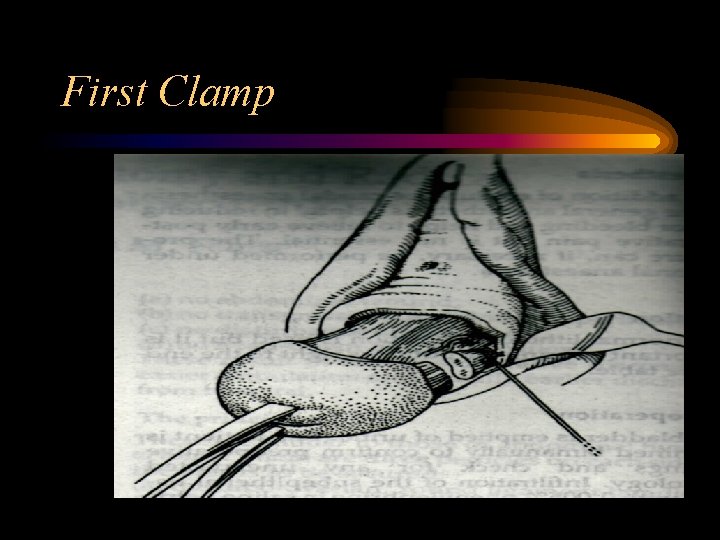
First Clamp
First Clamp • After pushing up the bladder and opening the pouch of Douglas (POD), 1 st clamp is applied to uterosacral ligament as close to the uterus as possible; Confirming that the inside blade is inside the peritoneal cavity to include the small vessels between the peritoneum and the base of the pelvis
Ligatures. • First ligatures is left with long threads, one with needle will be used to have a bite in the lateral vaginal angle so: – Support the vaginal vault by ligating it to the main supporting structures of the pelvis – Shares in the homeostasis of that vascular area

Stitching First Pedicle to Vaginal Angle • Occlusion of the space in between • Closure of small vessels • Fixing uterosacral to vagina

nd 2 Ligatures, Step ladder • Almost always the 2 nd bite will not reach the level of uterine vessels and we don’t intend to do so. • The long thread of the 1 st bite is tied with one of the threads of the next ligature so the whole uterosacral was at the end taken to the vaginal angle.
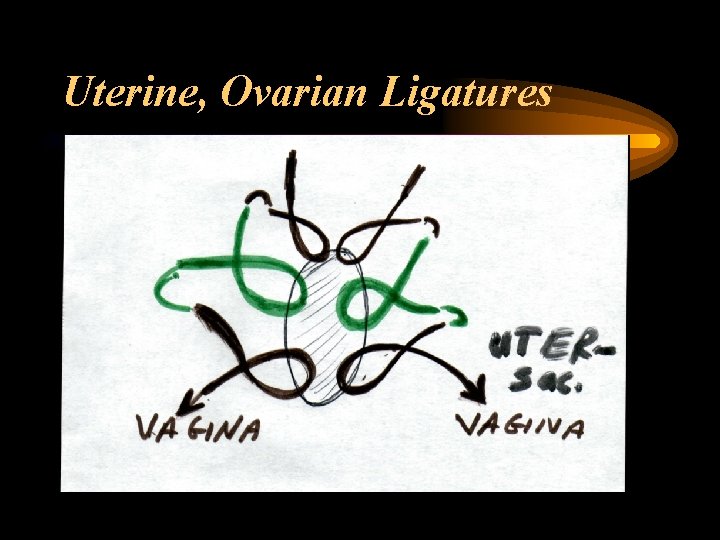
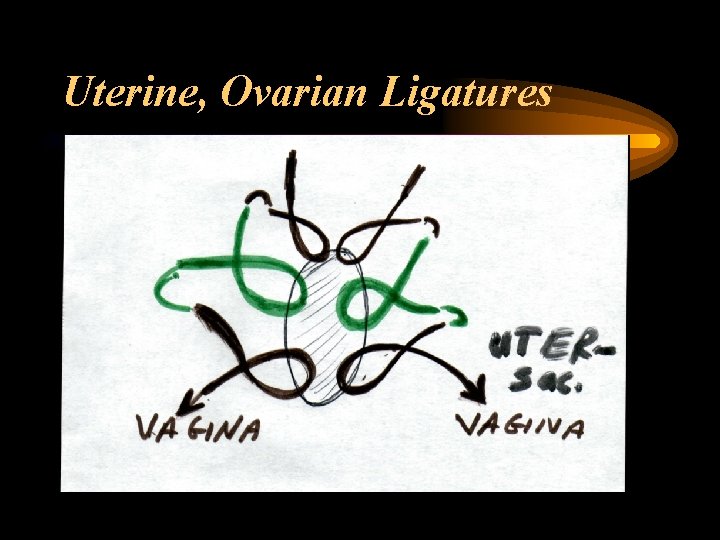
Uterine, Ovarian Ligatures


So, At the End. . • The whole three pedicles are ligated together on one side with marked stitch. During peritonization, one thread from round ligament was tied to its counterpart on the other side and peritoneum was approximated
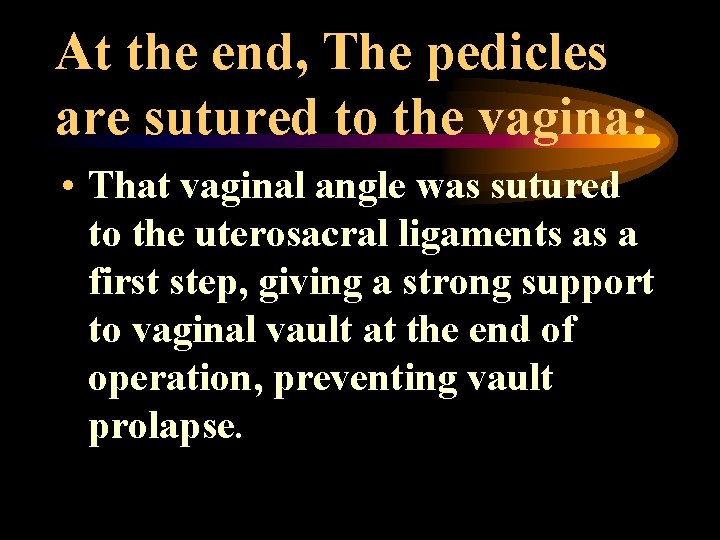
At the end, The pedicles are sutured to the vagina: • That vaginal angle was sutured to the uterosacral ligaments as a first step, giving a strong support to vaginal vault at the end of operation, preventing vault prolapse.
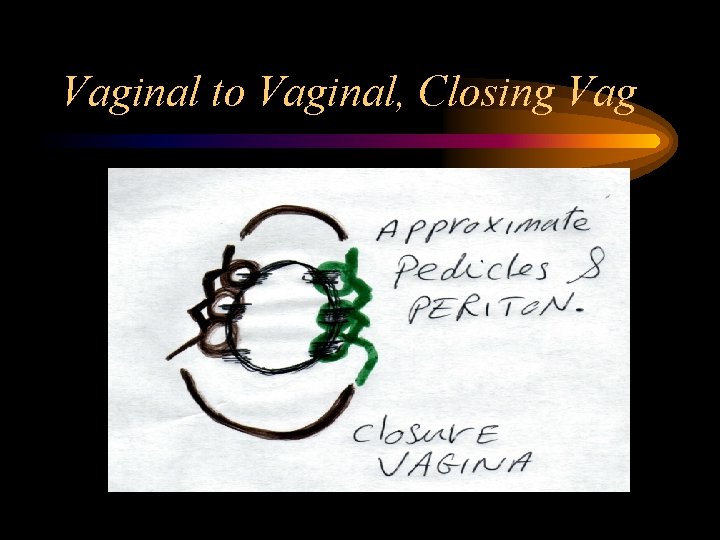
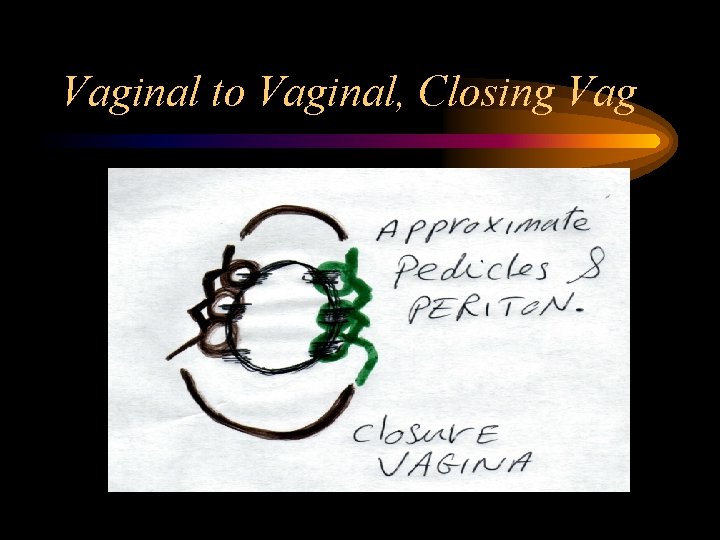
Vaginal to Vaginal, Closing Vag
Approximating Pedicles: • The marker stitch can help in pulling down any part of any pedicle when bleeding has to be secured. • Ligaturing the pedicles together will occlude the small vessels in between making good hemostasis. • These structures give good support to the vagina preventing posthysterectomy vaginal vault prolapse.
Results. • Median opertive time 60 min. • Post operative analgesics 33%. • Hospital stay 2. 1 days.
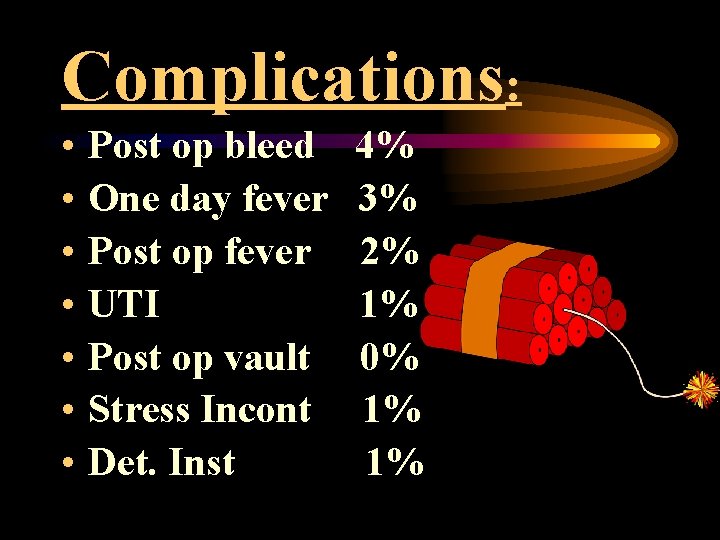
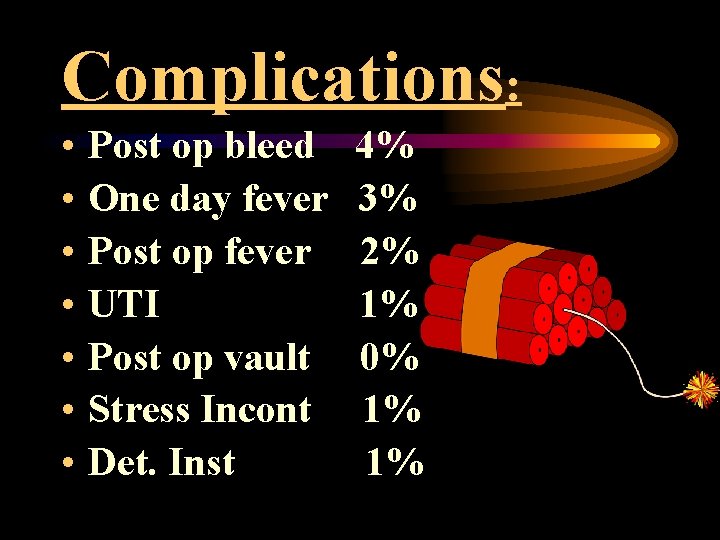
Complications: • • Post op bleed One day fever Post op fever UTI Post op vault Stress Incont Det. Inst 4% 3% 2% 1% 0% 1% 1%
Cost. • In 1998, the average charge for a laparoscopically-assisted vaginal hysterectomy in the united states was $14, 500; An abdominal hysterectomy was $12, 500: that for a vaginal hysterectomy was $10, 380; And that for (stat bull Metrop Insur co 2000). • Vaginal hysterectomy resulted in better quality -of-life outcomes and lower costs compared with laparoscopically assisted vaginal or abdominal hysterectomy (van den Eeden 1998).
Conclusion. . • Vaginal hysterectomy should be considered whethere is associated prolapse or not. • With proper selection, continued training, its rate will increase in front of abdominal or laparoscopic route. • Good access and assessment of uterosacrals. • Good support to the vagina.
Step Ladder • Easy access to all pedicles at any time. • Good inspection of the pedicles at the conclusion of surgery. • Minimizing oozing vessels inbetween pedicles.
Advantages of Technique: • Minimize well known postoperative vault prolapse, good support to vaginal vault. • Minimize intraoperative bleeding. • Minimize postoperative hematoma. • Easy and versatile access to ligature.
Advantages of Vaginal Approach • Time of operation • Exposure and Traumatization • Good for high risk patients • Post operative stay • Cost



Rules • Opening the POD in proper plane • Don’t dissect the bladder from fascia • In clamping uterosacral, inner blade includes the peritoneum • Clamping the pedicle in two steps is better than a big sizeable pedicle • First pedicle to be fixed to vaginal angle • Keep your clamps adjacent to the uterus • Step ladder procedure
Epilog • Abdominal route: Surgery • Laparoscopic: Technological surgery • Vaginal: Art surgery
Thank You
 Most common site of ureteric injury during hysterectomy
Most common site of ureteric injury during hysterectomy Hysterectomy
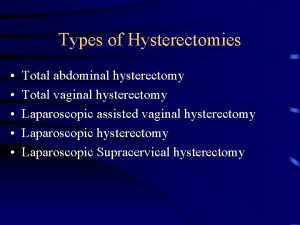
Hysterectomy Indications for hysterectomy
Indications for hysterectomy Cesarean hysterectomy steps
Cesarean hysterectomy steps Myotectomy
Myotectomy Promotion from assistant to associate professor
Promotion from assistant to associate professor Safe people safe places
Safe people safe places Safe feed safe food
Safe feed safe food Lotfi gaafar
Lotfi gaafar Lotfi lazaare
Lotfi lazaare Kimi zadeh
Kimi zadeh Lotfi zad
Lotfi zad Lotfi zad
Lotfi zad Lotfi zad
Lotfi zad Lotfi zad
Lotfi zad Lotfi gaafar
Lotfi gaafar System theory lotfi a. zadeh
System theory lotfi a. zadeh Lotfi gaafar
Lotfi gaafar Lotfi zad
Lotfi zad Lotfi zadeh
Lotfi zadeh Modified double flare technique
Modified double flare technique Modified stoll-egg counting technique
Modified stoll-egg counting technique Modified brandt andrews method
Modified brandt andrews method Modified stillman technique indication
Modified stillman technique indication Modified stillman technique
Modified stillman technique Actual and apparent position of gingiva
Actual and apparent position of gingiva Charters method of toothbrushing
Charters method of toothbrushing Www youtube com
Www youtube com Stages of labor
Stages of labor Site:slidetodoc.com
Site:slidetodoc.com Método del calendario
Método del calendario Jonction squamo cylindrique
Jonction squamo cylindrique Tipos de himem
Tipos de himem Sims speculum exam
Sims speculum exam Dt56a side effects
Dt56a side effects