University Medical Center EMSEC Navigation Program Christi Cargill
- Slides: 17
University Medical Center EMS/EC Navigation Program Christi Cargill MSN, RN, ACM Jill Edge, RN Kyle Galyean, LMSW Katie Noble MSN, RN
Purpose The purpose of this project is to implement an EMS/EC navigation program for University Medical Center (UMC) and reduce overutilization of EMS/EC services.
Navigation Goals � Implement care coordination services for UMC’s EMS and EC “high utilizers” � Hire case manager and social worker to navigate vulnerable, “high utilizers” through the healthcare continuum in Lubbock � Reduce non-emergent EMS and EC use at UMC for the identified “high utilizers” � 50% or 161 patients identified as “high utilizers” will be offered enrollment in the UMC navigation program after one year of implementation � 100 patients of the 161 “high utilizers” identified will enroll in navigation services
Navigation Goals cont. � � 100 patients identified as “high utilizers” will have decreased their EMS/EC visits by 50% after one year of implementation Readmission rates for identified patients enrolled in the navigation program will decrease Focus on managing and coordinating care across the healthcare continuum including chronic disease management, engagement of patients/families in care, creating/supporting patient-centered care, use evidence based care across disciplines, and utilizes technology to ensure measurement and accountability (American Organization of Nurse Executives [AONE], 2010). Coordinate a new delivery model linking the community, UMC, outpatient resources, and the patients to improve patient outcomes.
Background Ø Ø At UMC in 2012, 233 individuals in the Lubbock community accounted for 1, 450 emergency medical services (EMS) calls and transports to local emergency rooms. The EMS cost for these calls were approximately $1. 5 million in charges and approximately $2. 9 million in EC expenses. At UMC in 2013, there were 544 individuals that made an EMS call or an EC visit equal to or over 4 times. One individual had 50 visits in 2013
In 2011, there was one individual that had accumulated a bill over $1 million dollars by utilizing the EMS/EC system in one year.
Organizational Information Ø Ø Ø UMC’s Emergency Center (EC) in Lubbock, Texas averages over 80, 000 visits per year. Patients are seen from all over the region From 2010 to 2014 there was one case manager for the 64 bed EC and one social worker. These two individuals are often in contact with the difficult individuals during an EC visit. Often these “high utilizers” are in need of nonmedical resources. It has been documented that after a case management and/or social work intervention patient’s visits decrease.
With social work and case management intervention at UMC, the patient encounters in 2011 of the patient with $1 million in charges, the visits went from over 50 a year to less than 5 visits per year.
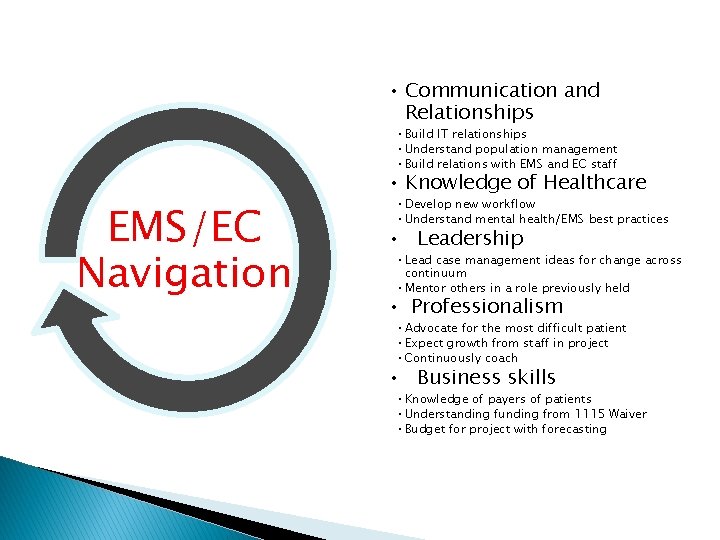
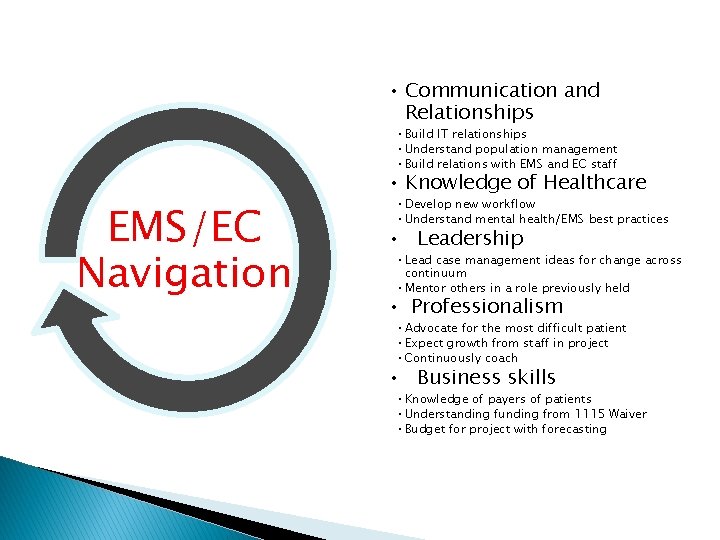
• Communication and Relationships • Build IT relationships • Understand population management • Build relations with EMS and EC staff EMS/EC Navigation • Knowledge of Healthcare • Develop new workflow • Understand mental health/EMS best practices • Leadership • Lead case management ideas for change across continuum • Mentor others in a role previously held • Professionalism • Advocate for the most difficult patient • Expect growth from staff in project • Continuously coach • Business skills • Knowledge of payers of patients • Understanding funding from 1115 Waiver • Budget for project with forecasting
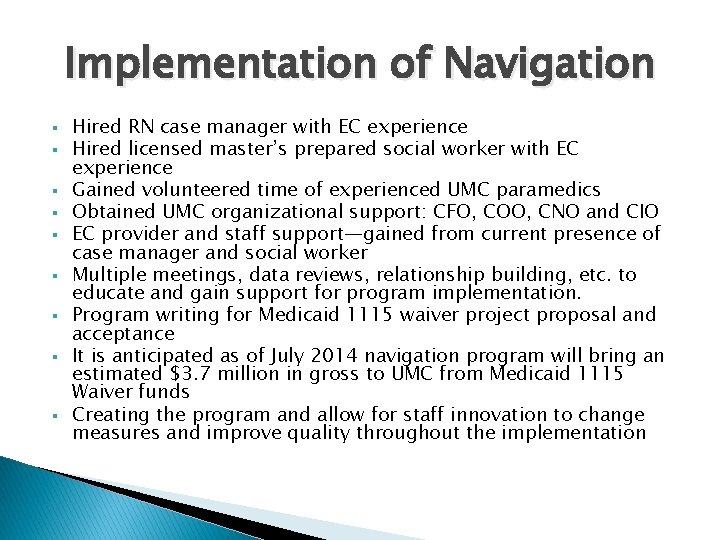
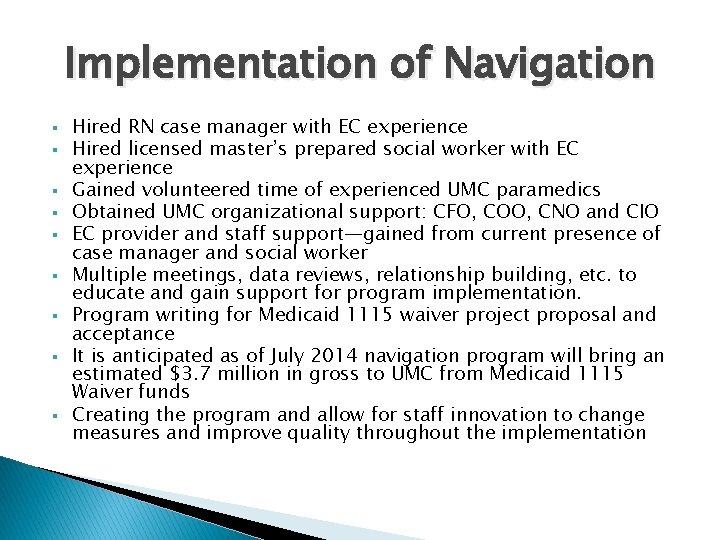
Implementation of Navigation § § § § § Hired RN case manager with EC experience Hired licensed master’s prepared social worker with EC experience Gained volunteered time of experienced UMC paramedics Obtained UMC organizational support: CFO, COO, CNO and CIO EC provider and staff support—gained from current presence of case manager and social worker Multiple meetings, data reviews, relationship building, etc. to educate and gain support for program implementation. Program writing for Medicaid 1115 waiver project proposal and acceptance It is anticipated as of July 2014 navigation program will bring an estimated $3. 7 million in gross to UMC from Medicaid 1115 Waiver funds Creating the program and allow for staff innovation to change measures and improve quality throughout the implementation
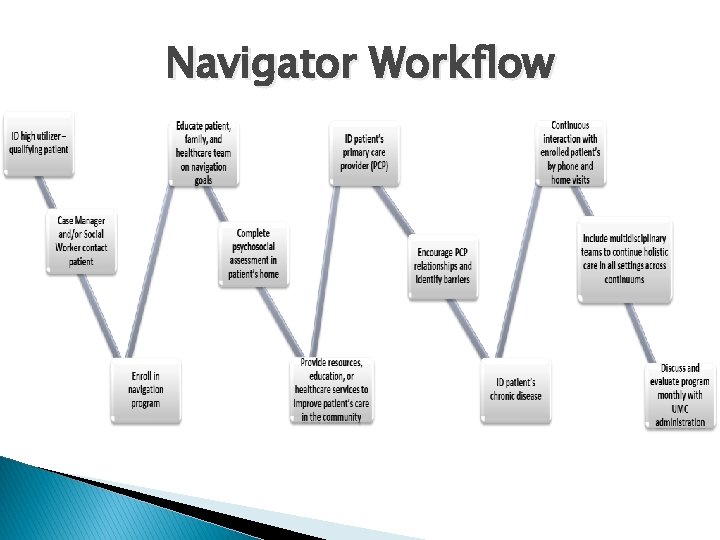
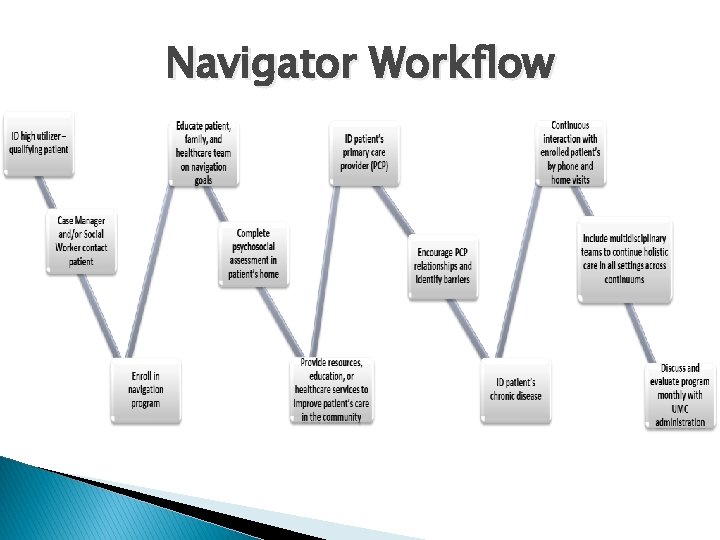
Navigator Workflow
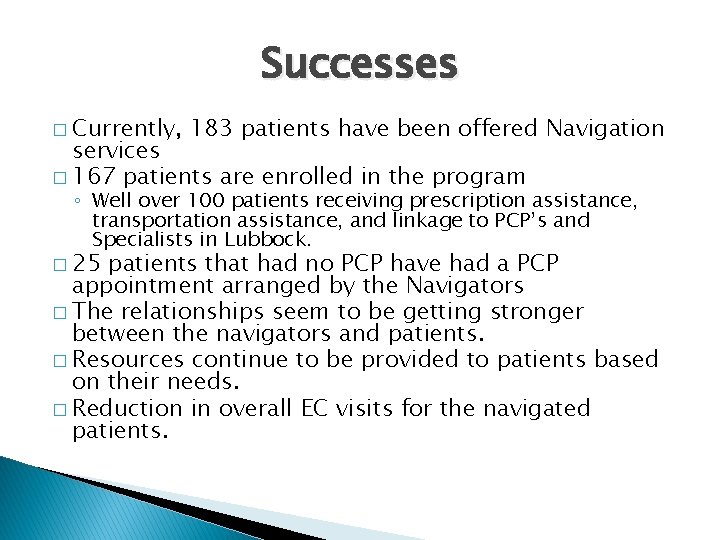
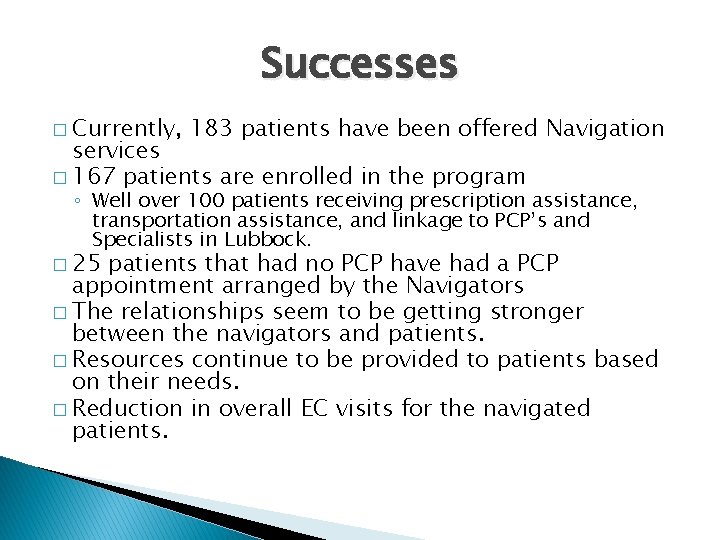
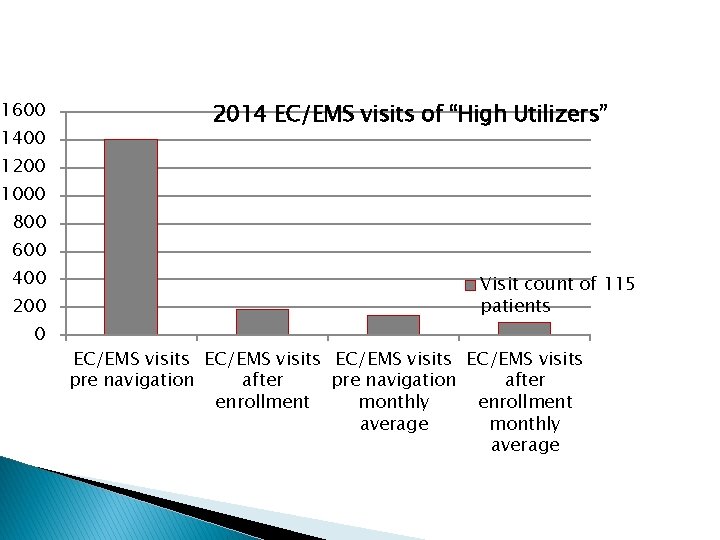
Successes � Currently, 183 patients have been offered Navigation services � 167 patients are enrolled in the program ◦ Well over 100 patients receiving prescription assistance, transportation assistance, and linkage to PCP’s and Specialists in Lubbock. � 25 patients that had no PCP have had a PCP appointment arranged by the Navigators � The relationships seem to be getting stronger between the navigators and patients. � Resources continue to be provided to patients based on their needs. � Reduction in overall EC visits for the navigated patients.
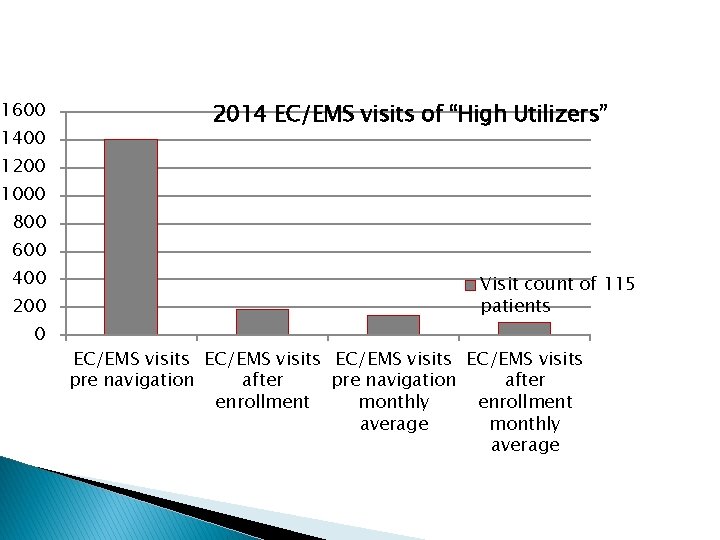
1600 1400 2014 EC/EMS visits of “High Utilizers” 1200 1000 800 600 400 200 0 Visit count of 115 patients EC/EMS visits pre navigation after enrollment monthly enrollment average monthly average
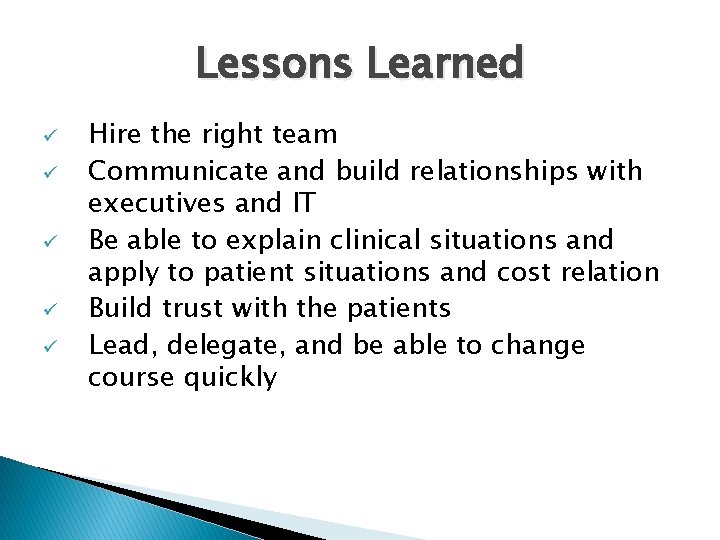
Lessons Learned ü ü ü Hire the right team Communicate and build relationships with executives and IT Be able to explain clinical situations and apply to patient situations and cost relation Build trust with the patients Lead, delegate, and be able to change course quickly
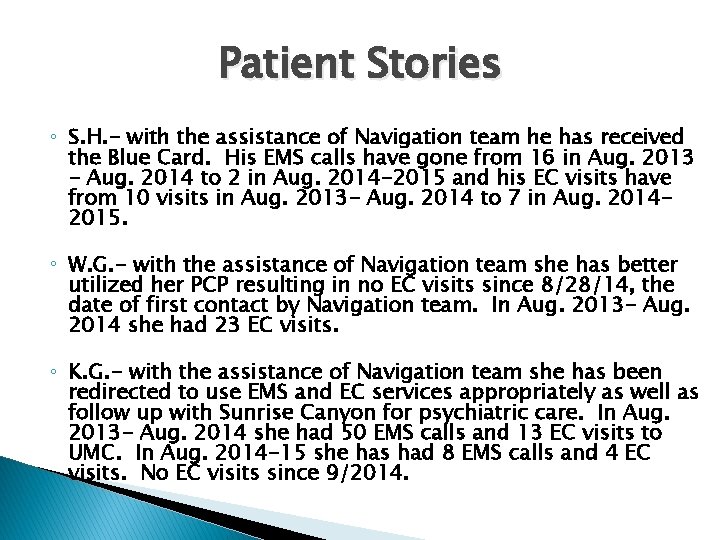
Patient Stories ◦ S. H. - with the assistance of Navigation team he has received the Blue Card. His EMS calls have gone from 16 in Aug. 2013 - Aug. 2014 to 2 in Aug. 2014 -2015 and his EC visits have from 10 visits in Aug. 2013 - Aug. 2014 to 7 in Aug. 20142015. ◦ W. G. - with the assistance of Navigation team she has better utilized her PCP resulting in no EC visits since 8/28/14, the date of first contact by Navigation team. In Aug. 2013 - Aug. 2014 she had 23 EC visits. ◦ K. G. - with the assistance of Navigation team she has been redirected to use EMS and EC services appropriately as well as follow up with Sunrise Canyon for psychiatric care. In Aug. 2013 - Aug. 2014 she had 50 EMS calls and 13 EC visits to UMC. In Aug. 2014 -15 she has had 8 EMS calls and 4 EC visits. No EC visits since 9/2014.
References American Organization of Nurse Executives. (2010). AONE guiding principles for future patient care delivery. Retrieved from http: //www. aone. org/resources/PDFs/AONE_GP_Future_Patie nt_Care_Delivery_2010. pdf
Questions?