The Culture of Healthcare Quality Measurement and Improvement

- Slides: 22
The Culture of Healthcare Quality Measurement and Improvement Lecture a This material (Comp 2_Unit 7 a) was developed by Oregon Health and Science University, funded by the Department of Health and Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU 24 OC 000015.
Quality Measurement and Improvement Learning Objectives • Define healthcare quality and the major types of quality measures: structural, process, and outcome measures (Lecture a) • Describe the current state of healthcare quality in the United States (Lecture a) • Discuss the current healthcare quality measures used in various healthcare settings in the US, including those required for the HITECH meaningful use program (Lecture b) • Describe the role of information technology in measuring and improving healthcare quality (Lecture c) • Describe the results of current healthcare quality efforts in the US (Lecture c) Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 2
Definitions and Operationalization • What is healthcare quality? Different views… • From Blumenthal (1996) – Donabedian, 1988: “That kind of care which is expected to maximize an inclusive measure of patient welfare, after one has taken account of the balance of expected gains and losses that attend the process of care in all its parts. ” – Lohr, IOM, 1990: The “degree to which health services for individuals and populations increase the likelihood of desired outcomes and are consistent with current professional knowledge. ” • In era of rising costs and concerns about quality, physicians and healthcare system must have public accountability (Chassin, 2010; Chassin, 2011) Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 3
Donabedian Model of Quality (2002) • Three categories – Structural–factors that make it easier or harder to deliver high-quality care, e. g. , hospital location, volume, association with teaching hospital – Process–factors describing healthcare content and activities, e. g. , adherence to screening, guidelines, etc. – Outcomes–changes attributable to care, e. g. , mortality, morbidity, functional status • Implemented and measured at different levels at an institution, e. g. , individual, department, organization Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 4
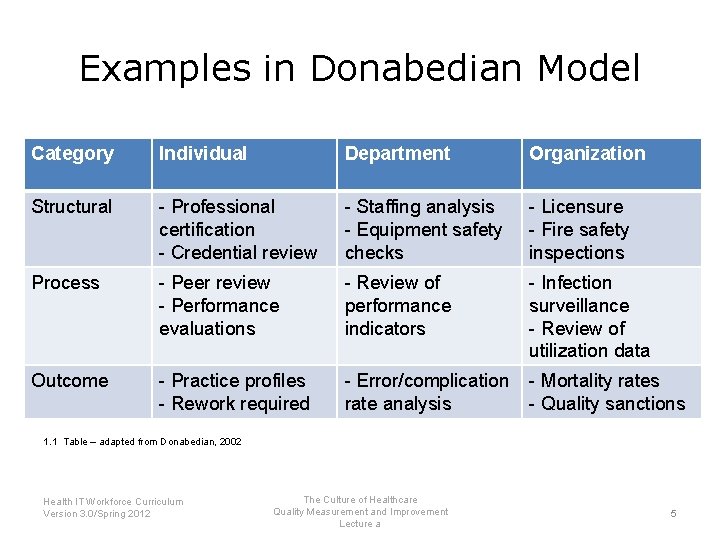
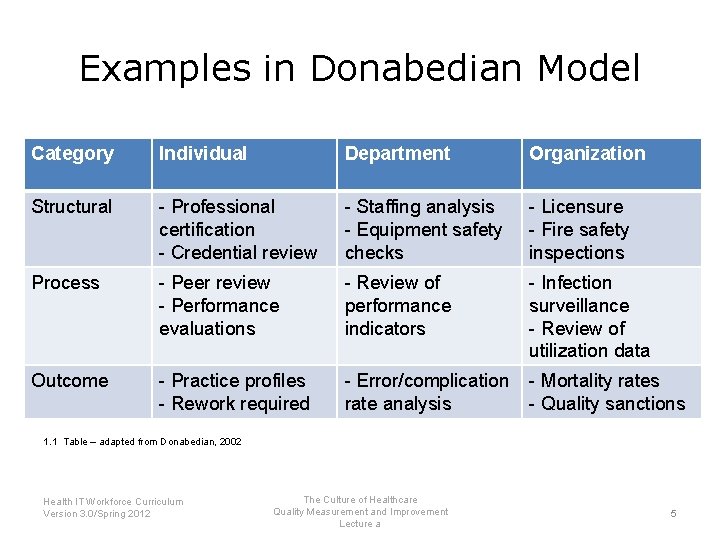
Examples in Donabedian Model Category Individual Department Organization Structural - Professional certification - Credential review - Staffing analysis - Equipment safety checks - Licensure - Fire safety inspections Process - Peer review - Performance evaluations - Review of performance indicators - Infection surveillance - Review of utilization data Outcome - Practice profiles - Rework required - Error/complication rate analysis - Mortality rates - Quality sanctions 1. 1 Table – adapted from Donabedian, 2002 Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 5
Process vs. Outcomes • In general, want to focus on outcomes – Represents what actually happens to patient – But difficult to measure plus confounding factors • Do we know about relationship between them? – In acute coronary syndromes, strong correlation between process and outcome measures (Peterson, 2006) – In other areas, however, not a strong relationship between satisfaction with care (“global ratings”) and its technical quality (Chang, 2006) – The science behind care also changes, e. g. , recognition that too tight of control (Hgb. A 1 C) in diabetes can be detrimental (Aron, 2009) – There is not always consensus, e. g. , “drugs to avoid” in elderly (Steinman, 2009) Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 6
Ideal Quality Measures • Landon, 2003–should be – – – – Evidence-based Agreed-on standards for satisfactory performance Standardized specifications Adequate sample size for reliable estimates Adjustment for confounding patient factors Care attributable to individual physician Feasible to collect Representative of activities of specialty • “In God we trust, all others bring data” – W. Edwards Deming, statistician (1900 -1993) • Adage from business management: An organization can’t improve what it cannot measure Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 7
Other definitions • Pay for performance (P 4 P) (Rowe, 2006) – Often equated with quality assessment but is just one approach (Rosenthal, 2008) – Based on notion that healthcare should be held accountable financially and otherwise • Value-based purchasing (Leapfrog, 2007) – Application of P 4 P • Accountable healthcare (Chassin, 2010) – Healthcare that is accountable to patients, purchasers, and others Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 8

What we know about Healthcare Quality • • Mc. Glynn (2003) and similar studies NCQA annual reports Commonwealth Fund scorecards Agency for Healthcare Research and Quality (AHRQ) annual reports • Other studies Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 9
Quality for Population at Large (Mc. Glynn, 2003) • One of most widely cited studies • Contacted 17, 937 adults in 12 metropolitan areas asking if they would agree to release records for assessment of quality • 6, 712 agreed to do so • Records reviewed for 439 indicators of quality of care for 30 acute and chronic diseases and preventive measures (Mc. Glynn, 2003) • Percentage receiving recommended care varied for different conditions • Overall 54. 9%, varying from atrial fibrillation (24. 7%) to senile cataract (78. 7%) Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 10
Other Results from Mc. Glynn and Related Data • Differences between sociodemographic groups much greater than within groups (Asch, 2006) • From this data and others, quality of care increases with number of chronic conditions (Higashi, 2007) • Similar analysis applied to patients in Veteran’s Health Administration found overall quality higher than national sample for process measures though not outcomes (Asch, 2004; Trivedi, 2011) – In light of history of suboptimal care within VA, transformation called “remarkable” and attributed in part to EHR system (Greenfield, 2004; Perlin, 2006; CBO, 2009) Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 11
NCQA Annual Reports • Reports on quality measure “gaps” to get all health plans to 90 th percentile of current quality shows; latest report (2010) shows – 50, 657 to 186, 512 avoidable deaths – $4. 6 to 7. 4 billion in avoidable medical costs • Also found that – Health plans that spend the most on care do not always deliver the best quality – Vaccination rates have dropped for children in private plans, while rates continue to rise for Medicaid children Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 12
Commonwealth Fund National Scorecard (Schoen, 2011) • Up to 84, 000 fewer Americans would die prematurely from causes amenable to healthcare if US achieved lower mortality rate of three other leading countries • Reducing insurance administrative costs to other best countries would save $114 billion per year • Medicare could save $4. 2 billion per year by reducing hospitalizations for preventable conditions Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 13
Agency for Healthcare Research and Quality (AHRQ) annual reports • Annual AHRQ reports on quality and disparities show progress is being made but is still suboptimal – Annual reports at http: //www. ahrq. gov/qual/measurix. htm – Can view measures by – Indicator – http: //www. ahrq. gov/qual/qrdr 10. htm – State (State Dashboard) – http: //statesnapshots. ahrq. gov/snaps 10/index. jsp Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 14
What else we know – Providers • Decline in deaths from treatable conditions (“amenable to healthcare”) has declined much more slowly in US than other developed countries (Nolte, 2008) • Physicians who score better on maintenance of certification exams have higher rates of quality based on process measures (Holmboe, 2008) • Use of hospitalists associated with better performance on quality indicators in hospitals (Lopez, 2009) • In primary care, visit duration (Chen, 2009) and patient “connectedness” (Atlas, 2009) associated with quality • Patients who are underinsured, minority, and/or non. English-speaking associated with lower-quality rankings from primary care physicians (Hong, 2010) Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 15
What else we know – Organizations • Training at one associated with a “best doctor” rating for cardiac bypass surgeons did not lower adjusted mortality rates (Hartz, 1999) • Being US News & World Report “Best Hospitals” associated with lower 30 -day mortality from acute MI, but some best hospitals had worse mortality and three times as many non-ranked hospitals had comparable low mortality (Wang, 2007) • Organizations that have direct leadership, accountability for quality and safety, and culture of collaboration have measureable differences in quality measures (Keroack, 2007) • Higher quality seen in larger (more integrated) large subspecialty medical groups (Weeks, 2010) Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 16
Relationship between expenditures and quality • Medicare data – There is great variation in cost among patients but little relationship to quality (Fisher 2003; Fisher, 2003) – Inverse relationship between expenditures per capita and state rank of quality (Baicker, 2004) • No association between per capita expenses and perceptions of quality by patients (Fowler, 2008) • No association between spending and quality measures in annual NCQA (e. g. , 2010) reports Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 17
Quality Measurement and Improvement Summary – Lecture a • Healthcare quality is defined as best possible delivery of care and its resulting outcomes • There are three major types of quality measures: structural, process, and outcome measures • Current state of healthcare quality in the United States shows significant gaps between care as delivered and best possible delivery Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 18
Quality Measurement and Improvement References – Lecture a References • Anonymous. (2007). Value-driven Health Care: A Purchase Guide, Version 2. 0. Washington, DC: The Leapfrog Group. Retrieved from http: //www. leapfroggroup. org/media/file/Employer_Purchaser_Guide_05_11_07. pdf. • Aron, D. , & Pogach, L. (2009). Transparency standards for diabetes performance measures. Journal of the American Medical Association, 301, 210 -212. • Asch, S. , Kerr, E. , Keesey, J. , Adams, J. , Setodji, C. , Malik, S. , & Mc. Glynn, E. (2006). Who is at greatest risk for receiving poor-quality health care? New England Journal of Medicine, 354, 1147 -1156. • Asch, S. , Mc. Glynn, E. , Hogan, M. , Hayward, R. , Shekelle, P. , Rubenstein, L. , . . . Kerr, E. (2004). Comparison of quality of care for patients in the Veterans Health Administration and patients in a national sample. Annals of Internal Medicine, 141, 938 -945. • Atlas, S. , Grant, R. , Ferris, T. , Chang, Y. , & Barry, M. (2009). Patient-physician connectedness and quality of primary care. Annals of Internal Medicine, 150, 325 -335. • Baicker, K. , & Chandra, A. (2004). Medicare spending, the physician workforce, and beneficiaries’ quality of care. Health Affairs. Retrieved Jan 2012 from http: //www. healthaffairs. org/FIX/10. 1377/hlthaff. W 4. 184 • Chang, J. , Hays, R. , Shekelle, P. , Mac. Lean, C. , Solomon, D. , Reuben, D. , . . . Wenger, N. (2006). Patients' global ratings of their health care not associated with the technical quality of their care. Annals of Internal Medicine, 144, 665 -672. • Chassin, M. , & Loeb, J. (2011). The ongoing quality improvement journey: next stop, high reliability. Health Affairs, 30, 559 -568. • Chassin, M. , Loeb, J. , Schmaltz, S. , & Wachter, R. (2010). Accountability measures--using measurement to promote quality improvement. New England Journal of Medicine, 363, 683 -688. • Chen, L. , Farwell, W. , & Jha, A. (2009). Primary care visit duration and quality: does good care take longer? Archives of Internal Medicine, 169, 1866 -1872. • Donabedian, A. (1988). The quality of care: how can it be assessed? Journal of the American Medical Association, 260, 1743 -1748. Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 19
Quality Measurement and Improvement References – Lecture a References • Donabedian, A. (Ed. ). (2002). An Introduction to Quality Assurance in Healthcare. Cambridge, MA: Oxford University Press. • Fisher, E. , Wennberg, D. , Stukel, T. , Gottlieb, D. , Lucas, F. , & Pinder, E. (2003 a). The implications of regional variations in Medicare spending. Part 1: the content, quality, and accessibility of care. Annals of Internal Medicine, 138, 273 -287. • Fisher, E. , Wennberg, D. , Stukel, T. , Gottlieb, D. , Lucas, F. , & Pinder, E. (2003 b). The implications of regional variations in Medicare spending. Part 2: health outcomes and satisfaction with care. Annals of Internal Medicine, 138, 288 -298. • Fowler, F. , Gallagher, P. , Anthony, D. , Larsen, K. , & Skinner, J. (2008). Relationship between regional per capita Medicare expenditures and patient perceptions of quality of care. Journal of the American Medical Association, 299, 2406 -2412. • Greenfield, S. , & Kaplan, S. (2004). Creating a culture of quality: the remarkable transformation of the Department of Veterans Affairs Health Care System. Annals of Internal Medicine, 141, 316 -318. • Hartz, A. , Kuhn, E. , & Pulido, J. (1999). Prestige of training programs and experience of bypass surgeons as factors in adjusted patient mortality rates. Medical Care, 37, 93 -103. • Higashi, T. , Wenger, N. , Adams, J. , Fung, C. , Roland, M. , Mc. Glynn, E. , . . . Shekelle, P. (2007). Relationship between number of medical conditions and quality of care. New England Journal of Medicine, 356, 2496 -2504. • Holmboe, E. , Wang, Y. , Meehan, T. , Tate, J. , Ho, S. , Starkey, K. , & Lipner, R. (2008). Association between maintenance of certification examination scores and quality of care for Medicare beneficiaries. Archives of Internal Medicine, 168, 1396 -1403. • Hong, C. , Atlas, S. , Chang, Y. , Subramanian, S. , Ashburner, J. , Barry, M. , & Grant, R. (2010). Relationship between patient panel characteristics and primary care physician clinical performance rankings. Journal of the American Medical Association, 304, 1107 -1113. Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 20
Quality Measurement and Improvement References – Lecture a References • Keroack, M. , Youngberg, B. , Cerese, J. , Krsek, C. , Prellwitz, L. , & Trevelyan, E. (2007). Organizational factors associated with high performance in quality and safety in academic medical centers. Academic Medicine, 82, 1178 -1186. • Landon, B. , Normand, S. , Blumenthal, D. , & Daley, J. (2003). Physician clinical performance assessment: prospects and barriers. Journal of the American Medical Association, 290, 1183 -1189. • Lohr, K. (Ed. ). (1990). Medicare: A Strategy for Quality Assurance. Washington, DC: National Academies Press. • López, L. , Hicks, L. , Cohen, A. , Mc. Kean, S. , & Weissman, J. (2009). Hospitalists and the quality of care in hospitals. Archives of Internal Medicine, 169, 1389 -1394. • Mc. Glynn, E. , Asch, S. , Adams, J. , Keesey, J. , Hicks, J. , De. Cristofaro, A. , & Kerr, E. (2003). The quality of healthcare delivered to adults in the United States. New England Journal of Medicine, 348, 2635 -2645. • Nolte, E. , & Mc. Kee, C. (2008). Measuring the health of nations: updating an earlier analysis. Health Affairs, 27, 5871. • Peterson, E. , Roe, M. , Mulgund, J. , De. Long, E. , Lytle, B. , Brindis, R. , . . . Ohman, E. (2006). Association between hospital process performance and outcomes among patients with acute coronary syndromes. Journal of the American Medical Association, 295, 1912 -1920. • Rosenthal, M. (2008). Beyond pay for performance--emerging models of provider-payment reform. New England Journal of Medicine, 359, 1197 -1200. • Rowe, J. (2006). Pay-for-performance and accountability: related themes in improving health care. Annals of Internal Medicine, 145, 695 -699. • Steinman, M. , Rosenthal, G. , Landefeld, C. , Bertenthal, D. , & Kaboli, P. (2009). Agreement between drugs-toavoid criteria and expert assessments of problematic prescribing. Archives of Internal Medicine, 169, 1326 -1332. Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 21
Quality Measurement and Improvement References – Lecture a References • Trivedi, A. , Matula, S. , Miake-Lye, I. , Glassman, P. , Shekelle, P. , & Asch, S. (2011). Systematic review: comparison of the quality of medical care in Veterans Affairs and non-Veterans Affairs settings. Medical Care, 49, 76 -88. • Wang, T. , Fonarow, G. , Hernandez, A. , Liang, L. , Ellrodt, G. , Nallamothu, B. , . . . Peterson, E. (2009). The dissociation between door-to-balloon time improvement and improvements in other acute myocardial infarction care processes and patient outcomes. Archives of Internal Medicine, 169, 1411 -1419. • Weeks, W. , Gottlieb, D. , Nyweide, D. , Sutherland, J. , Bynum, J. , Casalino, L. , . . . Fisher, E. (2010). Higher health care quality and bigger savings found at large multispecialty medical groups. Health Affairs, 29, 991 -997. Table • 1. 1 Adapted from Donabedian, A. (Ed. ). (2002). An Introduction to Quality Assurance in Healthcare. Cambridge, MA: Oxford University Press. Health IT Workforce Curriculum Version 3. 0/Spring 2012 The Culture of Healthcare Quality Measurement and Improvement Lecture a 22
 Process of nursing audit
Process of nursing audit Compliance vs quality
Compliance vs quality Healthcare and the healthcare team chapter 2
Healthcare and the healthcare team chapter 2 Sports medicine definition
Sports medicine definition Characteristics of quality culture
Characteristics of quality culture You are what you measure quote
You are what you measure quote Quality improvement vs research
Quality improvement vs research Patient centered care qsen examples
Patient centered care qsen examples Quality improvement paradigm
Quality improvement paradigm Continuous quality improvement plan example
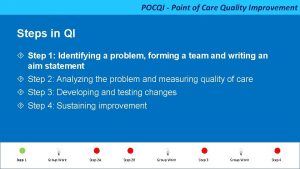
Continuous quality improvement plan example Pocqi ppt
Pocqi ppt Define continuous quality improvement
Define continuous quality improvement Efmd quality improvement system
Efmd quality improvement system Indiana perinatal quality improvement collaborative
Indiana perinatal quality improvement collaborative Continuous quality improvement program planning worksheet
Continuous quality improvement program planning worksheet Tea quality improvement
Tea quality improvement Xerox problem solving process
Xerox problem solving process Sus qi
Sus qi Cotinuous
Cotinuous Quality improvement
Quality improvement Juran 10 steps to quality improvement
Juran 10 steps to quality improvement Swot analysis for quality
Swot analysis for quality Malnutrition quality improvement initiative
Malnutrition quality improvement initiative