STROKE DYSPHAGIA AGEING POPULATION IN THE UK Office


- Slides: 20

STROKE & DYSPHAGIA
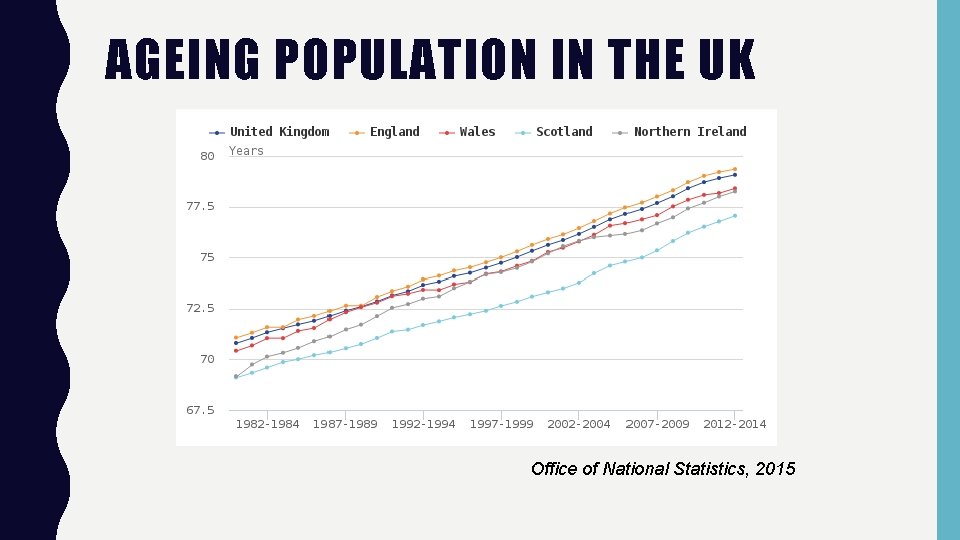
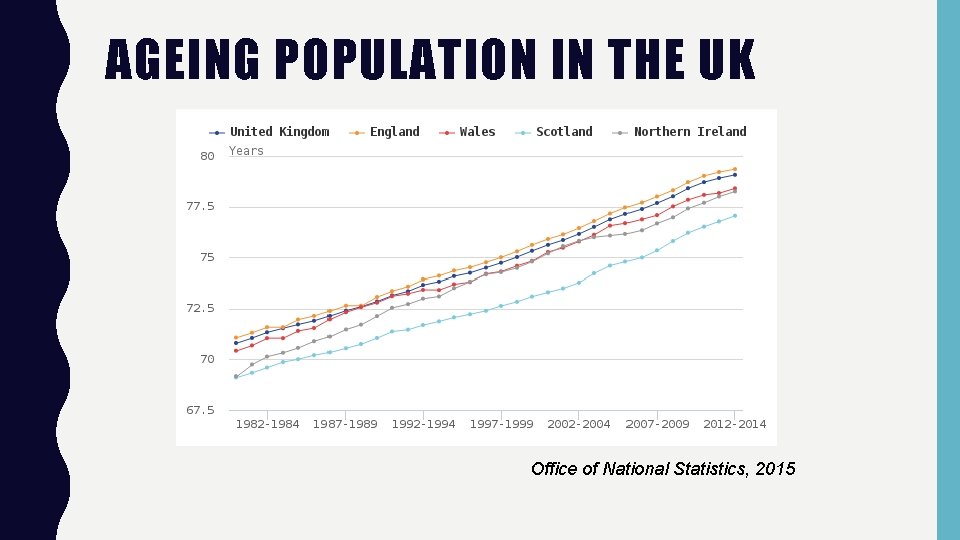
AGEING POPULATION IN THE UK Office of National Statistics, 2015
AGEING POPULATION IN THE UK • In 1948, 45% of the population died before the age of 65 years. • Today the life expectance for females is 86 years and 84 years for males • Number of people over the age of 85 years has doubled in the past three decades • By 2030 1 in 5 people will be over 65 years • The risk of health problems increases with age The King’s Fund, 2014
STROKE & AGEING • Age is the single biggest risk factor for stroke • The risk of stroke doubles each decade over the age of 55 years • Stroke service provision must account for the ageing population – give us more money! Stroke association, 2016
STROKE • Types of stroke: – Ischaemic stroke (the most common type) is caused by a blockage in a blood vessel in the brain – Haemorrhagic stroke is caused by a bleed on the brain • Results of stroke: – Lack of oxygen to the brain – Cell atrophy, tissue damage – Impaired function of affected areas of the brain (this may or may not be irreversible. )
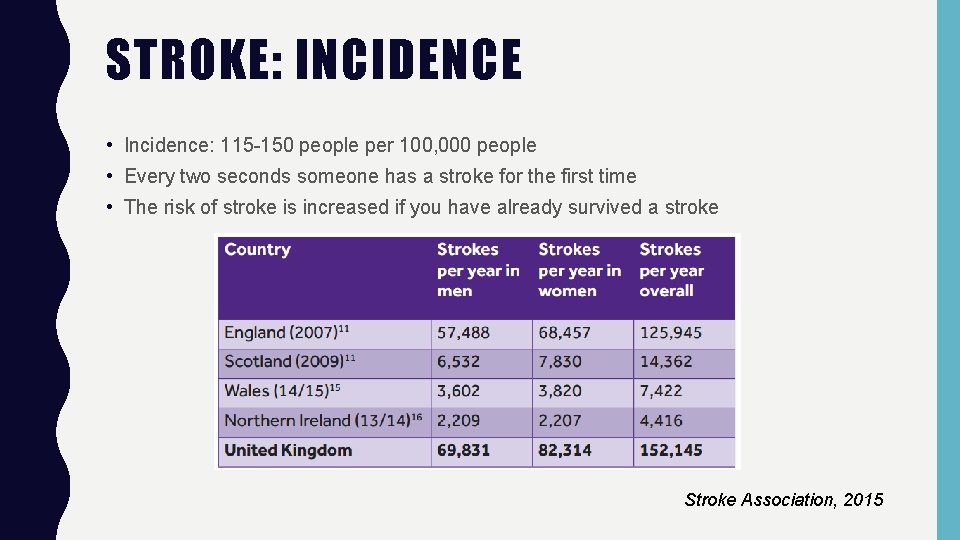
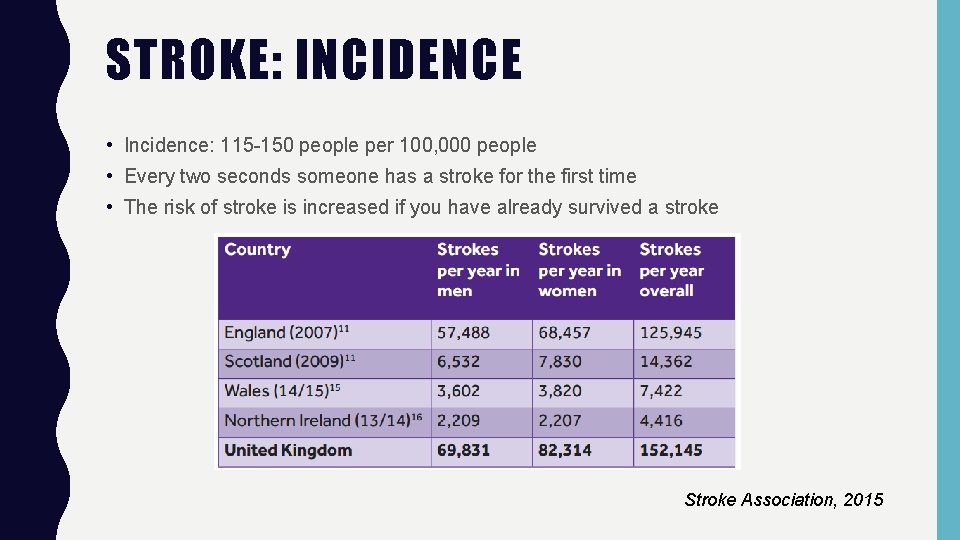
STROKE: INCIDENCE • Incidence: 115 -150 people per 100, 000 people • Every two seconds someone has a stroke for the first time • The risk of stroke is increased if you have already survived a stroke Stroke Association, 2015
STROKE: IMPACT • The impacts of stroke requiring treatment by SLT include: – Swallowing difficulties, dysphagia – Communication • Dysarthria • Aphasia • Apraxia of Speech • Only 25% of stroke rehabilitation units are adequately staffed for rehabilitation (Department of Health and Royal College of Physicians, 2007).
DYSPHAGIA – WHAT IS IT? • Disorders of “the total process of feeding, eating, drinking and swallowing”. RCSLT (2005) • Caused by tissue damage or deterioration in the brain which leads to: – weakened musculature – Sensory impairment – Interruption to the coordination of the swallowing motor sequence Kendall (2008)
DYSPHAGIA – SIGNS OF DYSPHAGIA • • • Coughing or choking when eating or drinking Bringing food back up, sometimes through the nose (nasal regurgitation) Food or drink “going down the wrong hole” Feeling like food is “getting stuck” in the throat Not keeping food in the mouth through oral preparatory stage Having food left in the mouth after swallowing Not chewing food Having a wet or croaky sounding voice Dribbling Taking a long time to swallow or finish a meal Having to swallow a lot to clear your throat Breathlessness when swallowing. Stroke Association, 2015
DYSPHAGIA ASSESSMENT • Initial clinical evaluation of swallowing and nutrition after stroke - All stroke patients should be screened for dysphagia before being given food or drink - Risk of pneumonia should be assessed based on aspiration risk and clinical case history • Swallow screening - Patients with dysphagia should be monitored daily in the first week - Initial observations of consciousness, posture, oral hygiene, control of oral secretions and water swallow test • Nutritional screening - Nutritional risk should be established and assessed within 48 hours of stroke, with regular re-assessment • Assessment - Clinical bedside assessment - Instrumental assessment (SIGN Guidelines, 2010)
DYSPHAGIA – INCIDENCE • 27 -64% of people who have a stroke have dysphagia (Geeganage et al 2012). • 15% of these people will still have dysphagia a month later (Geeganage et al 2012). • Previous data suggested that as many as 76% of people will continue to have moderate to severe dysphagia (Mann et al 1999) • 64 -90% of stroke patients present with dysphagia in the acute phase, with aspiration confirmed in 22 -42% of cases (SIGN, 2010)
DYSPHAGIA – IMPACT • Aspiration – food or liquid passes into the airway below the vocal folds. – Aspiration was found using instrumental screening methods in 22 -42% of conscious acute stroke patients (SIGN, 2010) • Pneumonia – Infection resulting from aspiration of fluids, food, reflux or oral secretions. – 30% of post stroke deaths are due to pneumonia (Heuschmann et al 2004) • Choking – Fear of choking increases anxiety and reduces enjoyment at mealtimes (Costa Bandeira et al 2008) • Dehydration – 75% of individuals have been found to be dehydrated due to dysphagia (Leibovitz et al 2007) – Dehydration can lead to increased risk of falls, UTIs, impaired mental status, and ulcers (Wotton et al 2008)
DYSPHAGIA – IMPACT • Malnutrition – 22% of patients found to be undernourished up to 6 months post stroke (Byrnningsen et al 2007) – Increased likelihood of tube feeding • Weight Loss – 57% of stroke patients found to have lost weight in the first 6 weeks post stroke (Byrnningsen et al 2007) – This was due to loss of independence when eating, and a disordered swallow. • Reduced general health – Dysphagia found to aggravate previous conditions, such as diabetes and wound healing (Carrau and Murray, 1998) • Reduced quality of life – Fear of choking increases anxiety and reduces enjoyment at mealtimes (Costa Bandeira et al 2008) – Patients who were PEG fed for their own safety were grateful for the nutrition but ambivalent to the process (SIGN, 2010), therefore solely providing sustenance does not increase Qo. L. – “When a person is unable to swallow, the ability to enjoy almost all other aspects of life is affected. Even minor, intermittent dysphagia can lead to psychological and social stresses. Episodes of choking can lead to a fear of eating that can lead to malnutrition and social withdrawal” (Mc. Culloch et al, 1997). – Dysphagia may result in PEG feeding, which may have a significant negative impact on quality of life for both patients and carers as well as significantly increased costs to the NHS (NICE, 2013).
DYSPHAGIA – COST • Pneumonia increases cost of care due to increased longevity of stay in the hospital (Katzan et al. , 2007) – prevention of this is vital for money saving – therefore we need more SLTs to carry out timely and effective assessments. • A stroke patient with dysphagia stays in hospital longer than those without dysphagia (Odderson et al. , 1995) • A person with dysphagia is twice as likely to be placed in a nursing home following a stroke than someone without dysphagia, which puts the social system under further financial pressure (Odderson et al. , 1995). RCSLT (2005)
DYSPHAGIA – COST Savings of: • £ 2. 30 in healthcare savings for adults with dysphagia – avoided chest infections • The savings made by having proper SLT provision exceed the cost of the SLT service by £ 13. 3 million. Not only do we save £ 13. 3 million for the NHS but we improve quality of life, avoid malnutrition and death. • A chest infection requiring hospital treatment costs £ 5, 084 due to inpatient days. With proper SLT care, minor chest infections can be cared for in the community which cost only £ 150. (Marsh et al. , 2010)
DYSPHAGIA – INTERVENTION • Speech and Language Therapist play a unique role in the assessment and management of dysphagia as part of the wider MDT care for stroke patients. • NICE recommendations are to “offer swallowing therapy at least 3 times a week to people with dysphagia after stroke who are able to participate, for as long as they continue to make functional gains. Swallowing therapy could include compensatory strategies, exercises and postural advice. ” (NICE 3. 1. 9. 2013). • Indirect/ compensatory strategies – Education and training for individuals and carers – Fluid and diet modification – Swallowing postures and manoeuvres • Direct/ rehabilitative strategies – Manoeuvers – Oro-motor exercises – Transcutaneous Neuromuscular Electrical Stimulation (TNMES) RCSLT, 2014
DYSPHAGIA – EFFICACY • Diet and fluid modification is widely used in the UK in the management of dysphagia (RCSLT, 2014) • Efficacy of diet and fluid modification is inconclusive, two RCT conducted in USA: • Robbins et al (2008) – 515 elderly participants in total – 3 groups: chin-tuck, nectar consistency fluids and honey consistency fluids – The lowest incidence of aspiration pneumonia was seen in the chin-tuck group – The rate of aspiration pneumonia was higher in the thicker (honey consistency) fluids group • Logemann et al (2008) – 711 participants with PD and/ or Dementia – 3 conditions: chin-tuck, nectar consistency fluids and honey consistency fluids – Videofluroscopy found lowest incidence of aspiration when drinking thickest fluids – The chin-tuck condition was least effective in preventing aspiration
DYSPHAGIA – EFFICACY • Direct intervention strategies like TNMES are not routinely used in the UK but are widely used in the USA in the treatment of dysphagia (RCSLT, 2014). • There has been recent interest in TNMES, with lots of literature supporting its efficacy • TNMES involves using electrodes position on the neck and head to stimulate peripheral nerves and innervate muscles when swallowing • A systematic review by NICE found support for the efficacy of TNMES when compared to traditional dysphagia therapies (e. g. diet and fluid modification) • A recent meta-analysis of the evidence for TNMES by Tan et al (2013) also found support for TNMES when compared with other treatments for dysphagia. • To provide state of the art interventions – WE NEED MONEY! (NICE, 2014)

CONCLUSION • Short term benefits of SLT: the prevention of aspiration pneumonia, dehydration and death (NICE, 2013). • Long term benefits of SLT: a return to a normal diet – which has a significant impact on quality of life for both patients and carers (NICE, 2013). WE NEED YOUR MONEY BECAUSE…. • Every £ 1 you invest in us will save the NHS £ 2. 30 • The older you get the more at risk of having a stroke you are…. and you’re not getting any younger…. . ! • How would you feel if you were no longer able to enjoy eating the sweets you love!
REFERENCES • Brynningsen, P. K. , Damsgaard, E. M. , & Husted, S. E. (2007). Improved nutritional status in elderly patients 6 months after stroke. Journal of Nutritional Health and Aging, 11(1), 75 -79. • Carrau, R. , & Murray, T. (1998). Comprehensive Management of Swallowing Disorders. San. Diego: Singular Publishing Group. • Department of Health and Royal College of Physicians, 2007, Survey of Stroke Unit Staffing and Patient Dependency, London, DH • Geeganage, C. , Beavan, J. , Ellender, S. & Bath, P. M. W. (2012). Interventions for dysphagia and nutritional support in acute and subacute stroke. The Cochrane Collaboration, John Wiley & Sons. • Katzan, I. L. , Dawson, N. V. , Thomas, M. E. , Votruba, M. E. , & Cebul, R. D. (2007). The Cost of Pneumonia after Acute Stroke. Neurology, 68, 1938 -1943. • Kendall, K. (2008). Anatomy and physiology of deglutition. In R. Leonard & K. Kendall, Dysphagia assessment and treatment planning: a team approach. 2 nd edition. San. Diego: Plural Publishing, pp. 17 -22. • Leibovitz A, Baumoehl Y, Lubart E, Yaina A, Platinovitz N, Segal R. (2007). Dehydration among long-term care elderly patients with oropharyngeal dysphagia. J Gerontol. 2007; 53: 179– 183. doi: 10. 1159/000099144. • Mann, G. Hankey, G. and Cameron, D. 1999. Swallowing Function After Stroke Prognosis and Prognostic Factors at 6 Months. Stroke. 30: 744 -748. • Martino, R. , Foley, N. , Bhogal, S. , Diamant, N. , Speechley, M. and Teasell, R. (2005). Dysphagia after stroke: Incidence, diagnosis, and pulmonary complications. Stroke. 36(12), 2756 -2763. • Marsh, K. , Bertranou, E. , Suominen, H. & Venkatachalam, M. (2010). An economic evaluation of speech and language therapy. Matrix Evidence. Available online at: http: //www. rcslt. org/delete/giving_voice/matrix_report • National Institute for Health and Care Excellence (NICE) (2014). Transcutaneous Neuromuscular Electrical Stimulation for Oropharyngeal Dysphagia: Intervention Procedures Guidelines. NICE • National Institute for Health and Care Excellence (NICE) (2013). Stroke Rehabilitation Long term rehabilitation after stroke. Clinical guideline 162 Methods, evidence and recommendations. NICE. • Odderson, R. , Keaton, J. , & Mc. Kenna, B. (1995). Swallowing Management in Patients on Acute Stroke Pathway: Quality is cost-effective. Arichives of physical medicine and rehabilitation, 76(12), 1130 -1113. • Perlman, A. L. , & Schulze Delrieu, K. (1997). Degluition and its disorders. San. Diego: Singular Publishing. • RCSLT (2005). Clinical Guidelines. Bicester, Oxon: Speechmark. Available at www. rcslt. org/docs/competencies_project. pdf • RCSLT (2014) RCSLT Resource Manual for Commissioning and Planning Services in SLCN: Dysphagia. London: RCSLT • Robbins, J. , Gensler, G. , Hind, J. , Logemann, J. A. , Lindblad, A. S. , Brandt, D. , Baum, H. , Lilienfeld, D. , Kosek, S. , Lundy, D. , Dikeman, K. , Kazandjian, M. , Gramigna, G. D. , Garvey- Toler, S. and Miller Gardner, P. J. 2008. Comparison of 2 interventions for liquid aspiration on pneumonia incidence: a randomized trial. Annals of Internal Medicine, 148 (7): 509 -518. • Scottish Intercollegiate Guidelines Network (2010). Management of patients with stroke: identification and management of dysphagia, a national clinical guideline. Edinburgh: SIGN. • Tan, C. , Liu, Y. , Li, W. , Liu, J. , & Chen, L. (2013). Transcutaneous neuromuscular electrical stimulation can improve swallowing function in patients with dysphagia caused by non‐stroke diseases: a meta‐analysis. Journal of oral rehabilitation, 40(6), 472 -480. • Wotton K, Crannitch K, Munt R. Prevalence, risk factors and strategies to prevent dehydration in older adults. Contemp Nurse. 2008; 31: 44– 56. doi: 10. 5172/conu. 673. 31. 1. 44.