STROKE AND DYSPHAGIA STROKE There are two types


- Slides: 19
STROKE AND DYSPHAGIA
STROKE There are two types of strokes – ischaemic (clot) and haemorrhagic (bleed). About 85% of all strokes are ischaemic and 15% haemorrhagic How often does stroke strike? Occurs 152, 00 times a year in the UK – equivalent to one stroke every 3 minutes and 27 seconds in the UK Men are at a 25% higher risk of having a stroke and at a younger age compared to women The greatest risk of recurrent stroke is in the first 30 days Every two seconds someone in the world will have a stroke for the first time There were almost 17 million incidences of first-time stroke worldwide in 2010 Stroke occurs in up to 13 per 100, 000 children in the UK. It is thought there around 400 childhood strokes a year in the UK 1 in 4, 000 babies have a stroke at birth worldwide - this translates to around 200 strokes in babies a year in the UK alone
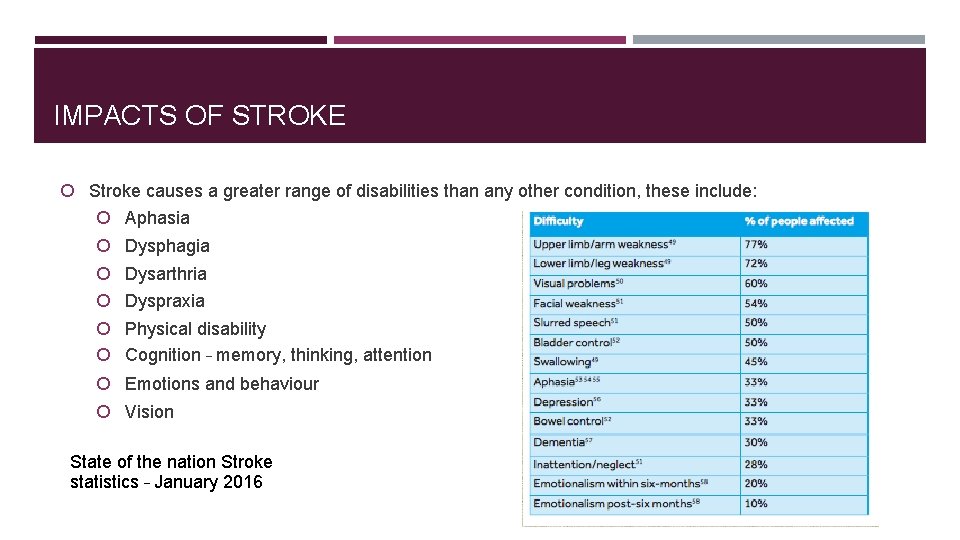
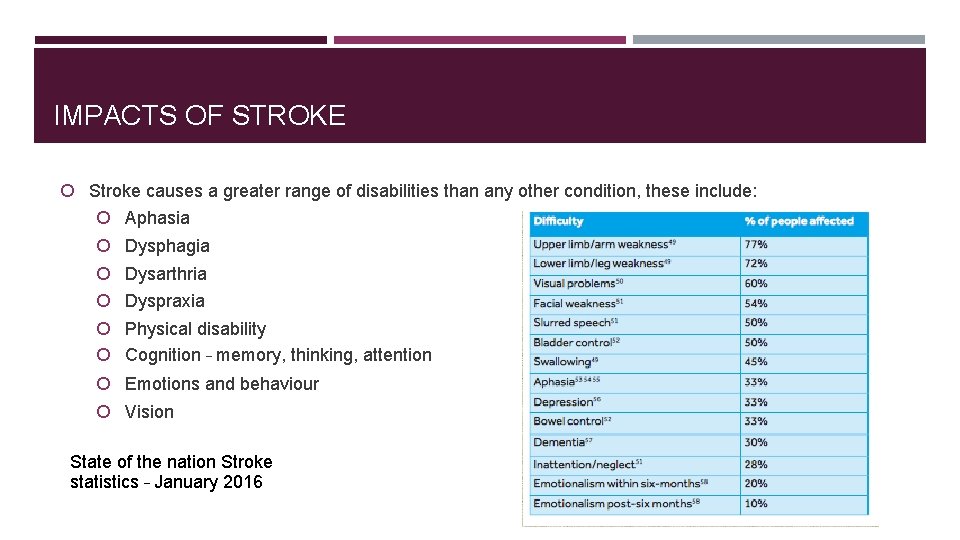
IMPACTS OF STROKE Stroke causes a greater range of disabilities than any other condition, these include: Aphasia Dysphagia Dysarthria Dyspraxia Physical disability Cognition – memory, thinking, attention Emotions and behaviour Vision State of the nation Stroke statistics – January 2016
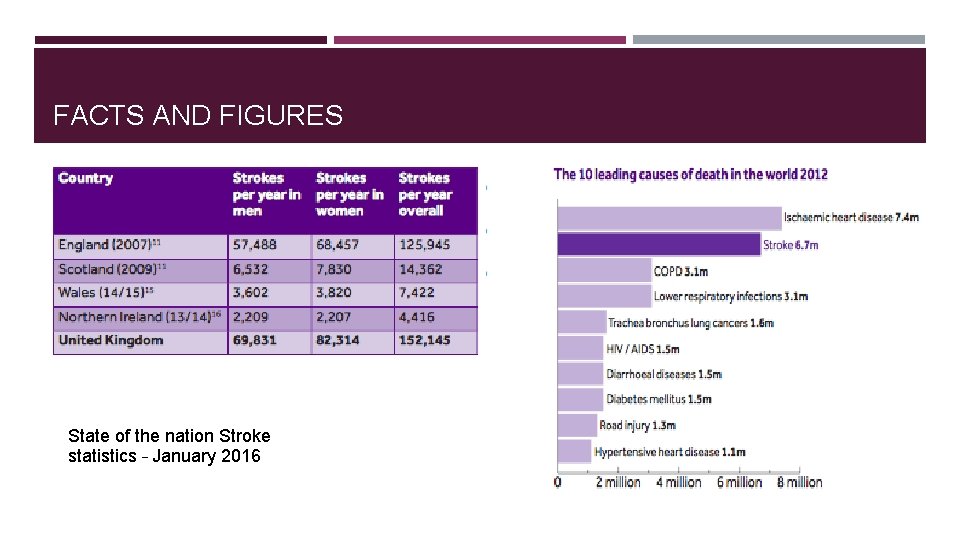
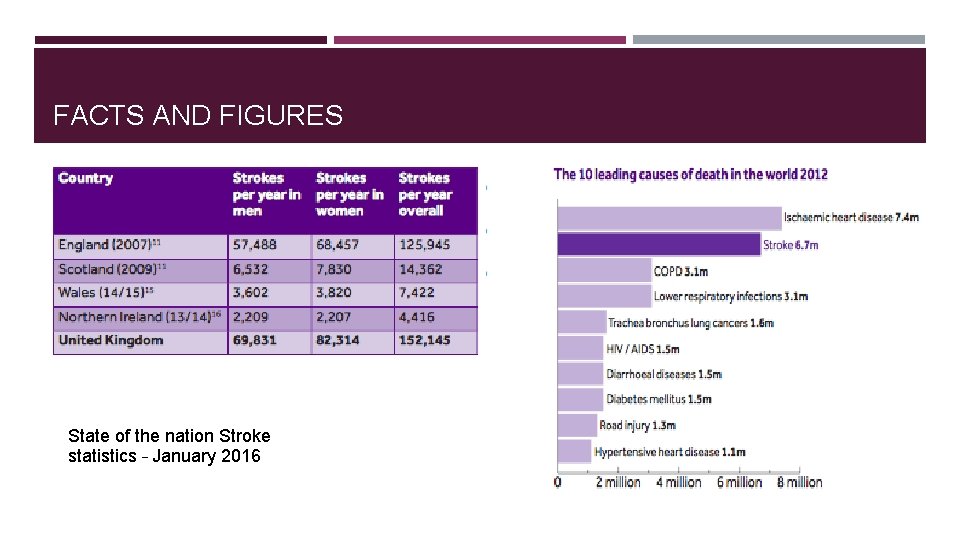
FACTS AND FIGURES State of the nation Stroke statistics – January 2016
ADVANTAGES OF STROKE UNITS Expert early assessment and diagnostic tests Early referral for surgery Expert nursing care Temperature, oxygenation, hydration Nutrition DVT prophylaxis Positioning Early rehab (Physiotherapy, SALT, OT) NICE Dysphagia screen within 4 hours, SLT r/v in 72 hours SLT for 45 mins 5 days / week for those making gains Dysphagia training 3 days /week for those making gains
GUIDELINES – STROKE (NICE, 2013) Assessment of communication § Within 72 hours of onset of stroke symptoms Intensity of therapy Speech therapy services should offer 45 minutes of the relevant therapy per day, 5 days per week. Consider more than 45 minutes per day for those who are able to participate and make functional gains. Patients can be seen for less than 45 minutes per day if required, but therapy should still be offered 5 days per week. Therapy § Impairment based; enhance remaining abilities; coach others including family members/carers; other methods of communication (i. e. gesture, alphabet boards, i. Pad + apps) ; supporting to access information/ decision making. § Review 6 months and Annually.
DYSPHAGIA § Dysphagia is the term used to describe a swallowing disorder usually resulting from a neurological or physical impairment of the oral, pharyngeal or oesophageal mechanisms (RCSLT, 2009). § Dysphagia in adults is associated with a number of different conditions, including: § Stroke § Progressive neurological disorders, including dementia § Parkinson disease, motor neurone disease, multiple § sclerosis, and muscular dystrophy § cancer, including head and neck, lung, and oesophageal § respiratory conditions, including chronic obstructive § pulmonary disease, emphysema, and asthma § learning disability, developmental and acquired disorders § disorders of the immune system § traumatic brain injury
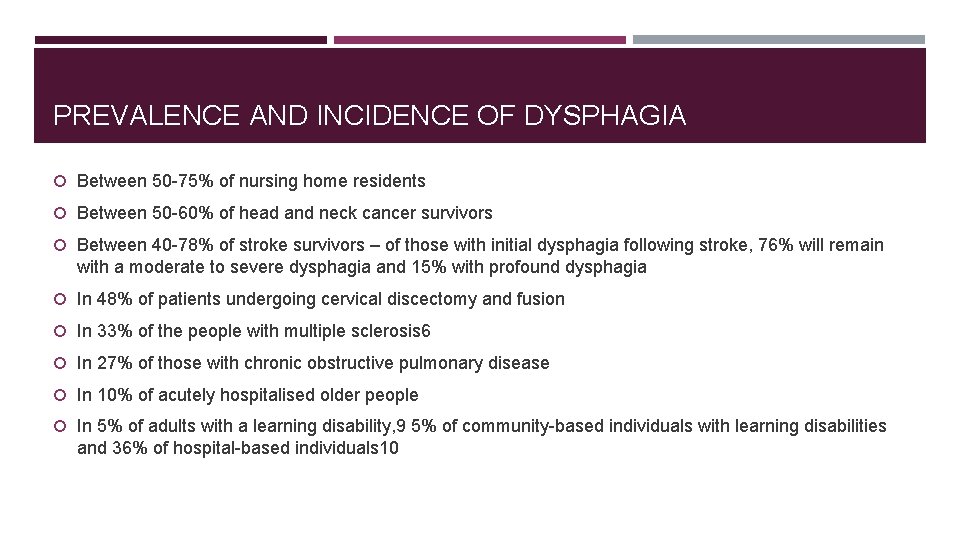
PREVALENCE AND INCIDENCE OF DYSPHAGIA Between 50 -75% of nursing home residents Between 50 -60% of head and neck cancer survivors Between 40 -78% of stroke survivors – of those with initial dysphagia following stroke, 76% will remain with a moderate to severe dysphagia and 15% with profound dysphagia In 48% of patients undergoing cervical discectomy and fusion In 33% of the people with multiple sclerosis 6 In 27% of those with chronic obstructive pulmonary disease In 10% of acutely hospitalised older people In 5% of adults with a learning disability, 9 5% of community-based individuals with learning disabilities and 36% of hospital-based individuals 10
IMPACT OF DYSPHAGIA Life threatening consequences Malnutrition Dehydration Impaired quality of life Psychosocial problems Aspiration pneumonia – major cause of morbidity and mortality after stroke
SYMPTOMS OF DYSPHAGIA Dysphagia can present in many ways, and the patient may demonstrate one or several of the following symptoms (RCSLT, 2009): Food spillage from lips Taking a long time to finish a meal Poor chewing ability Dry mouth Drooling Nasal regurgitation Food sticking in the throat Poor oral hygiene Coughing and choking Regurgitation Weight loss Repeated chest infections

GUIDELINES – DYSPHAGIA (NICE, 2008; 2013) Assessment of Swallowing By SLT within 24 hours and no more than 72 hours post stroke if the initial screen suggests swallowing difficulties. If aspiration is suspected and dietary modification or tube feeding is required for 3 days or more, the patient should be re-assessed, considered for instrumental examination and referred for dietary advice. Patients who cannot take adequate nutrition and fluids orally should receive tube feeding within 24 hours (nasogastric tube), have individualised advice and monitoring and be referred for nutritional assessment. If long term feeding is required (>4 weeks), PEG feeding should be recommended (SIGN, 2010) Therapy § Food and liquid modifications should be made to ensure the patient with dysphagia can swallow safely and without aspiration. Specialist assessment of this should be ongoing. § Offer dysphagia therapy 3 times per week for those able to access therapy and make functional gains. § Therapy may include - compensatory strategies, exercises and postural advice. § Mouth care should be given regularly to prevent aspiration pneumonia.
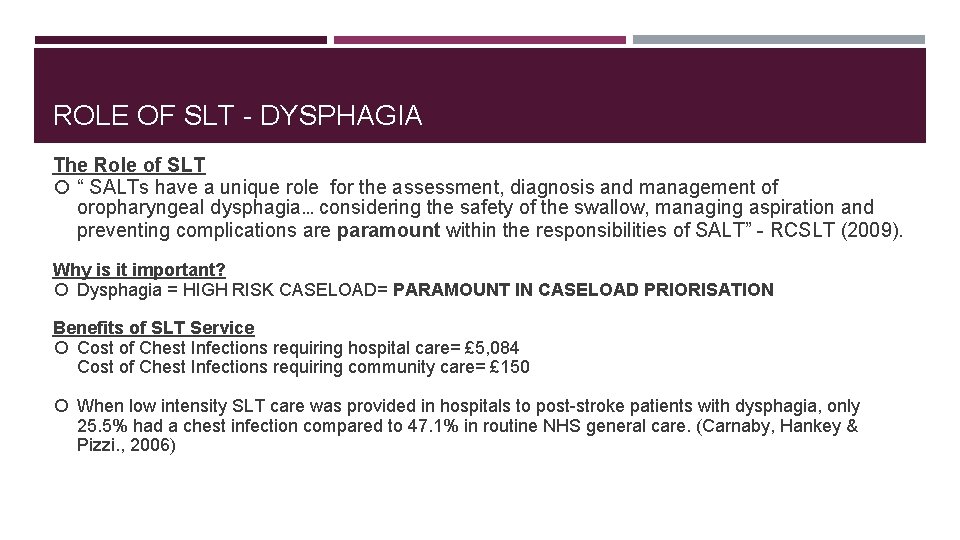
ROLE OF SLT - DYSPHAGIA The Role of SLT “ SALTs have a unique role for the assessment, diagnosis and management of oropharyngeal dysphagia… considering the safety of the swallow, managing aspiration and preventing complications are paramount within the responsibilities of SALT” - RCSLT (2009). Why is it important? Dysphagia = HIGH RISK CASELOAD= PARAMOUNT IN CASELOAD PRIORISATION Benefits of SLT Service Cost of Chest Infections requiring hospital care= £ 5, 084 Cost of Chest Infections requiring community care= £ 150 When low intensity SLT care was provided in hospitals to post-stroke patients with dysphagia, only 25. 5% had a chest infection compared to 47. 1% in routine NHS general care. (Carnaby, Hankey & Pizzi. , 2006)
ROLE OF SLT-COMMUNICATION DIFFICULTIES The Role of an SLT “Speech and language therapists play a unique role in identification and assessment of those with aphasia. The ability to identify levels of comprehension and expression as well as retained communication abilities are unique skills of speech and language therapists” – RCSLT (2009) SLT’s created patient-centered management plans, unique to the individual and their own goals and needs. SLT’s have a key role in educating/training, others involved in care of those with aphasia including the family, health, education and social care staff. Efficient comprehension of language and effective spoken language production are VITAL in today’s fast-paced world. Without such skills, Qo. L can be drastically negatively effected and the overall well-being of the patient can decline (Beukelman & Mirenda, 1998) Benefits of SLT Service 45566 aphasic patients require SLT input. It is assumed with enhanced SLT intervention, the patients Qo. L is drastically improved with Quality Adjusted Life Years increasing to 0. 2 yrs compared to 0. 12 yrs in usual SLT therapy. (Marsh, Bertranou, Suominen & Venkatachalam, 2010)
INTERVENTIONS FOR DYSPHAGIA Modification of food/fluid consistencies A common practice in dysphagia management but evidence for effectiveness is limited (RCSLT, 2009) May reduce risk of penetration and aspiration (Logemann et al. , 2008) Issues with compliance (Garcia et al. , 2005) Compensatory strategies Altering bolus size, temperature, taste or speed and presentation of delivery may be used in practice but evidence for effectiveness is limited (Bulow et al. , 2003)
INTERVENTIONS FOR DYSPHAGIA Direct swallowing therapy Aim to change swallowing physiology May not be appropriate for all patients dependent e. g. on respiratory status and ability to follow instructions (Speyer et al. , 2010) Educating and training Increases adherence to swallowing regimes set out by SLT recommendations (Rosenvinge & Starke, 2005) Feeding assistance by trained individuals can improve nutritional uptake (Wright, Cotter & Hickson, 2008)
INTERVENTIONS FOR COMMUNICATION DIFFICULTIES More significant gains made when therapy begins in the acute phase of recovery post-stroke (Bakheit et al. , 2007) Higher intensity intervention leads to more positive outcomes (Beukelman & Mirenda, 1998) Computer based therapy or use of apps can have positive outcomes and are time and cost-effective (requires 2 hours of therapist time per month compared with 12 hours for standard delivery) (Norwich & Grove, 1997; Wright et al. , 2004) Effectiveness of intervention is highly dependent upon client participation and motivation (RCSLT, 2009)
INTERVENTIONS FOR COMMUNICATION DIFFICULTIES Examples of evidence-based interventions for people with communication difficulties following stroke: Impairment-based therapy – Therapy targeting the underlying deficit can be effective in restoring function e. g. improving intelligibility in people with dysarthria (Mackenzie & Lowit, 2007) and improving receptive and expressive language ability in people with aphasia (RCSLT, 2009) Compensatory strategies – e. g. environmental modifications, topic fronting for people with aphasia or use of clear speech strategies for people with dysarthria can improve communicative effectiveness (Sellars et al. , 2005; Palmer & Enderby, 2007). AAC - Provision of assistive devices ranging from low tech aids e. g. alphabet boards to sophisticated computer systems can increase communicative effectiveness (Crow, 1989) Education and training – Training/educating family members in use of strategies to support communication can reduce conversation breakdown and increase the client’s participation in conversation (Cunningham 2003; Clarke et al. , 2001) Participation-based therapy – Assisting with lifestyle changes, increasing access to employment, education and services and signposting to relevant organisations can client increase wellbeing and autonomy (RCSLT, 2009)

REFERENCES Bakheit, A. M. , Shaw, S. , Barrett, L. , Wood, J. , Carrington, S. , Griffiths, S. , Searle, K. , Koutsi, F. , Bakheit, A. M. O. , Shaw, S. , Barrett, L. , Wood, J. , Carrington, S. , Griffiths, S. , Searle, K. , & Koutsi, F. (2007). A prospective, randomized, parallel group, controlled study of the effect of intensity of speech and language therapy on early recovery from post stroke aphasia", Clinical Rehabilitation, 21, 885 -894. Beukelman, D. , Mirenda, P. (1998). Augmentative and Alternative Communication. Management of Severe Communication Disorders in Children and Adults (2 nd ed. ). 1998. Maryland, Paul H Brookes. Bu low, M. , Olsson, R. , & Ekberg, O. (2003). Videoradiographic analysis of how carbonated thin liquids and thickened liquids affect the physiology of swallowing in subjects with aspiration on thin liquids. Acta Radiologica, 44, 366 -372. Carnaby, G. , Hankey, G. J. and Pizzi, J. (2006) “Behavioural interventions for dysphagia in acute stroke: a randomised controlled trial”, Lancet Neurology, 5, 31 -37. Clarke, M. , Mc. Conachie, H. , Price, K. , & Wood, P. (2001). Views of young people using augmentative and alternative communication systems. International Journal of Language and Communication Disorders 36, 107 -115. Crow, E. , & Enderby, P. (1989). The effects of an alphabet chart on the speaking rate and intelligibility of speakers with dysarthria. (pp. 99 -108). In K. M. Yorkston & D. R. Beukelman (Eds. ), Recent advances in clinical dysarthria. Boston: College-Hill. Cunningham, R. & Ward, C. D. (2003) Evaluation of a Training Programme to Facilitate Conversation between People with Aphasia and Their Partners, Aphasiology, 17, 687 -707. Garcia, J. M. , Chambers, E. , & Molander, M. (2005). Thickened Liquids: Practice Patterns of Speech-Language Pathologists. American Journal of Speech-Language Pathology, 14, 4 -13. Logemann, J. A. , Gensler, G. , Robbins, J. A. , Lindblad, A. , Brandt, D. , Hind, J. , Kosek, S. , Dikeman, K. , Kazandjian, M. , Gramigna, G. D. , Lundy, D. , & Mc. Garvey-Toler, S, & Gardner, P. J. M. (2008). A randomized study of three interventions for aspiration of thin liquids in patients with dementia and Parkinson's disease. Journal of Speech, Language, and Hearing Research, 51, 173 - 183.
REFERENCES Mac. Kenzie, C. , & Lowit, A. (2007), Behavioural intervention effects in dysarthria following stroke: communication effectiveness, intelligibility and dysarthria impact, International Journal of Language & Communication Disorders, 42, 131 -153. 1 -K. Marsh, K. , Bertranou, E. , Suominen, H. , Venkatachalam, M. (2010) An economic evaluation of speech and language therapy, Matrix Evidence, December 2010. Nice. (2008). Nice clinical guidelines. Stroke and transient ischemic attack in over 16 s: diagnosis and initial management. Retrieved March 14, 2017, from https: //www. nice. org. uk/guidance/cg 68/resources/stroke-and-transient-ischaemic-attack-in-over-16 s-diagnosis-and-initial-management-975574676437 Nice. (2013) Stroke Rehabilitation in Adults. Retrieved March 14, 2017, from https: //www. nice. org. uk/guidance/cg 162/resources/stroke-rehabilitation-in-adults 35109688408261 Norwich, B. , & Grove, N. (1997). The Use of AAC Systems in London Schools. Institute of Education. Palmer, R. , & Enderby, P. (2007). Methods of speech therapy treatment for stable dysarthria: a review. Advances in Speech-Language Pathology, 9, 140 -153. Rosenvinge, S. and Starke, I. 2005. Improving care for patients with dysphagia. Age and Ageing, 34, 587 -593. 1 -2. K. Marsh, E. Bertranou, H. Suominen, M. Venkatachalam, An economic evaluation and languageand therapy, Matrixservices Evidence, for December Royal College of Speech and Language Therapists. (2009). Resource manual of forspeech commissioning planning SLCN: 2010 Aphasia. Retrieved March 12, 2017, from https: //www. rcslt. org/speech_and_language_therapy/commissioning/aphasia_plus _intro Royal College of Speech and Language Therapists. (2009). Resource manual for commissioning and planning services for SLCN: Dysarthria. Retrieved March 12, 2017, from https: //www. rcslt. org/speech_and_language_therapy/commissioning/dysarthria_plus_intro Royal College of Speech and Language Therapists. (2009). Resource manual for commissioning and planning services for SLCN: Dysphagia. Retrieved March 12, 2017, from https: //www. rcslt. org/speech_and_language_therapy/commissioning/dysphagia_manual_072014 Sellars, C. , Hughes, T. , & Langhorne, , P. (2005), Speech and language therapy for dysarthria due to non-progressive brain damage, Cochrane Database of Systematic Reviews, 4. SIGN (2010) SIGN 119: Management of patients with stroke. Retrieved March 14 th, 2017, from http: //www. sign. ac. uk/pdf/sign 119. pdf Speyer, R. , Baijens, L. , Heijnen, M. , & Zwijnenberg, I. (2010). Effects of therapy in oropharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia, 25, 40 -65. Wright, J. , Clarke, M. , Donlan, C. , Lister, C. , Newton, C. , Cherguit, J. , Newton, E. (2004). Evaluation of the Communication Aids Project. University College London. Wright, L. , Cotter, D. , and Hickson, M. (2008). The effectiveness of targeted feeding assistance to improve the nutritional intake of elderly dysphagic patients in hospital. Journal of Human Nutrition & Dietetics, 21, 555 -562.