Sports Medicine Sports Related Concussion Return to Learn

- Slides: 29
Sports Medicine Sports Related Concussion Return to Learn Return to Play Susanna Gadsby, RN, BSN, MBA, ONC Sports Medicine Dartmouth Hitchcock Medical Center
Sports Medicine Concussion 101
Sports Medicine Conflict of Interest Disclosure I and/or my spouse/legally recognized domestic partner have no financial interest/arrangements in any amount within the past 12 months with one or more organization(s), which could be perceived as a real or apparent conflict of interest and which would reasonably appear to influence my role as a potential faculty/committee member for any CME or CNE activity.
Sports Medicine Objectives 1) Define Sports Related Concussion. 2) Identify implications for personnel involved with studentathletes who may be exposed to possible injury. 3) Identify 3 symptoms of sports related concussion 4) Identify 2 potential catastrophic complications of sports related concussion
Sports Medicine Defining Concussion Incidence: 1. 6 to 3. 8 million people sustain sport or recreation related concussions each year. Despite this number definitions and diagnostic criteria vary widely. Neuroanatomic and physiologic measures are non-existent. Functional vs. structural injury, can make it challenging for students to convince others they are really injured.
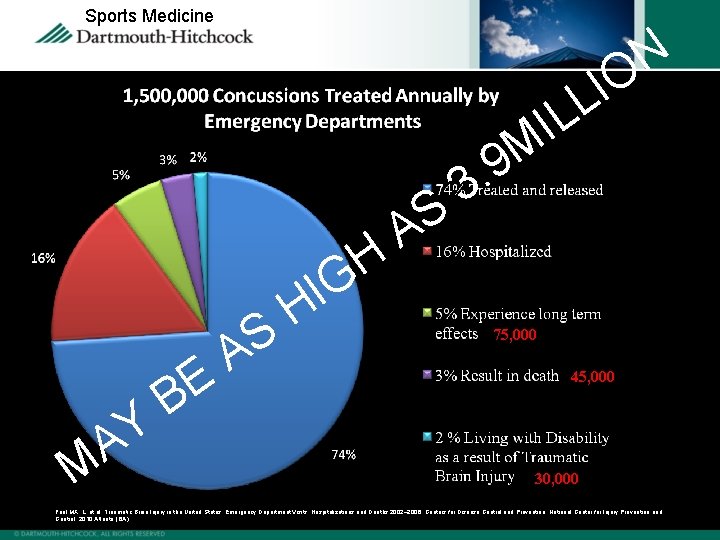
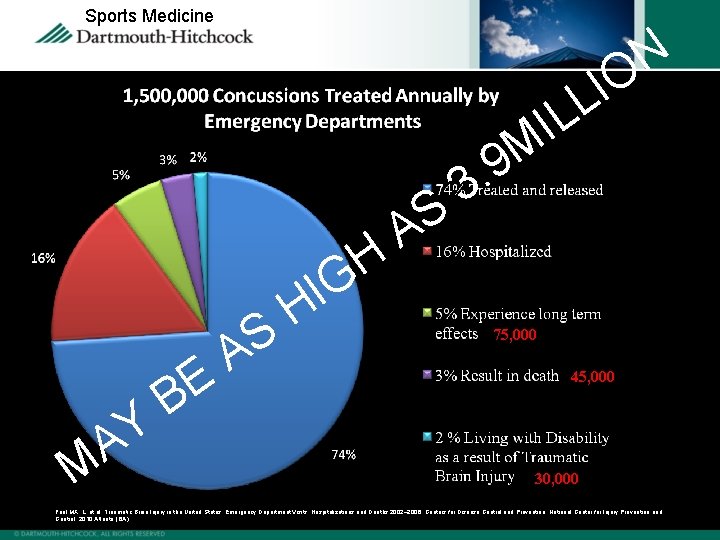
Sports Medicine N O I L H G Y A M E B S A I H S A L I M 9. 3 75, 000 45, 000 30, 000 Faul MX, L. et al. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations and Deaths 2002– 2006. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. 2010; Atlanta (GA).
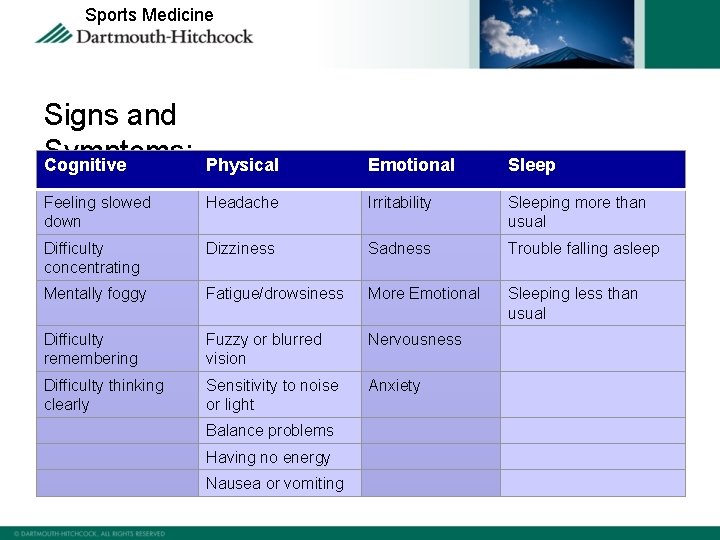
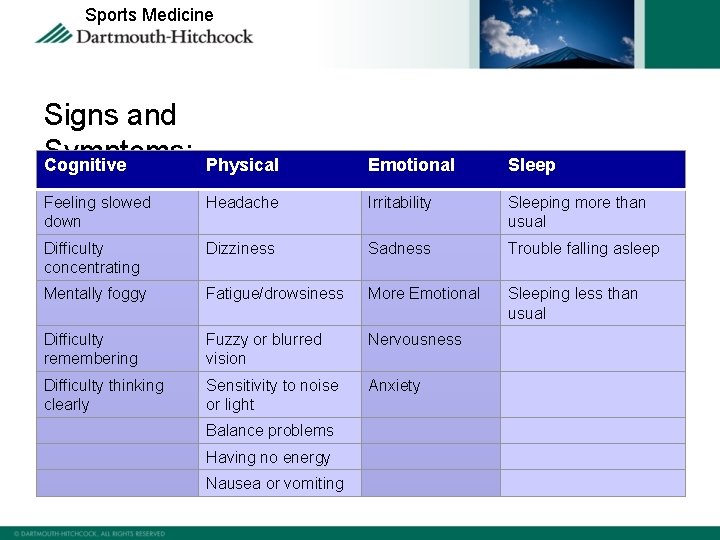
Sports Medicine Signs and Symptoms: Cognitive Physical Emotional Sleep Feeling slowed down Headache Irritability Sleeping more than usual Difficulty concentrating Dizziness Sadness Trouble falling asleep Mentally foggy Fatigue/drowsiness More Emotional Sleeping less than usual Difficulty remembering Fuzzy or blurred vision Nervousness Difficulty thinking clearly Sensitivity to noise or light Anxiety Balance problems Having no energy Nausea or vomiting
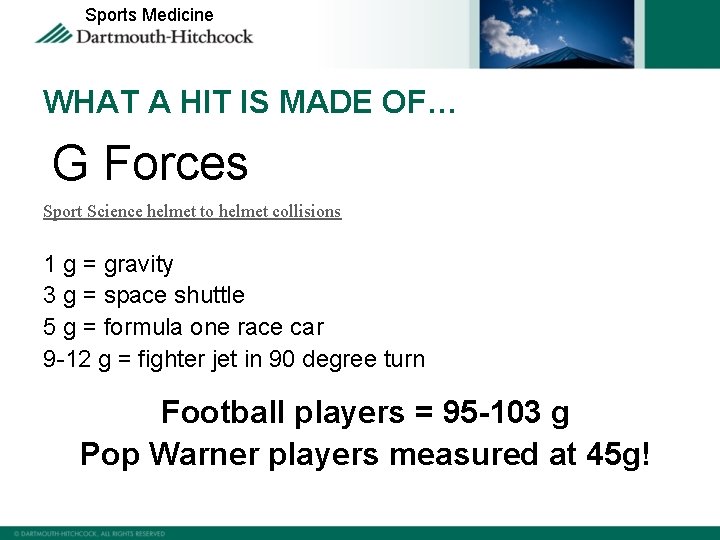
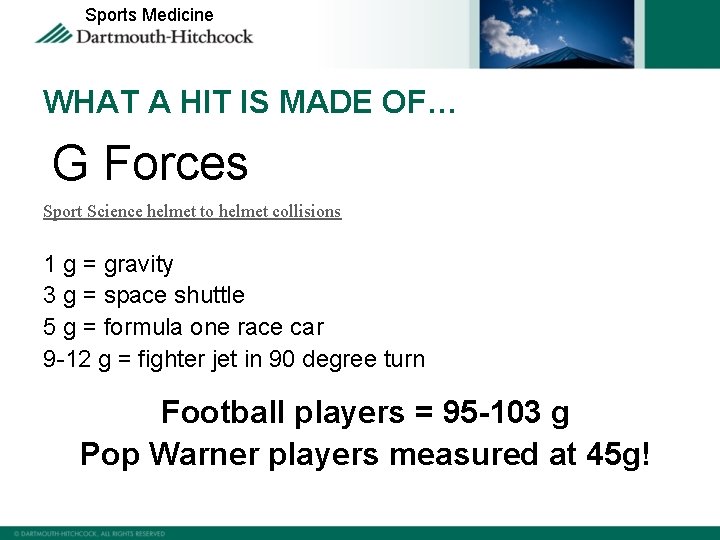
Sports Medicine WHAT A HIT IS MADE OF… G Forces Sport Science helmet to helmet collisions 1 g = gravity 3 g = space shuttle 5 g = formula one race car 9 -12 g = fighter jet in 90 degree turn Football players = 95 -103 g Pop Warner players measured at 45 g!
Sports Medicine • • • Recognition and proper management of concussions when they first occur can help prevent further injury or even death. Athletes should NEVER return to activity on the same day as a concussion. Keep the athlete out of play until a health care professional, experienced in evaluating for concussion, has clearer him/her to return to activity. WHEN IN DOUBT, SIT IT OUT!
Sports Medicine Second Impact Syndrome: • When an athlete returns to play, and sustains a second concussion before the first concussion has subsided. • Because the brain is more vulnerable, only a minimal force is needed to cause irreversible damage. • Although SIS is rare, it is most often deadly.
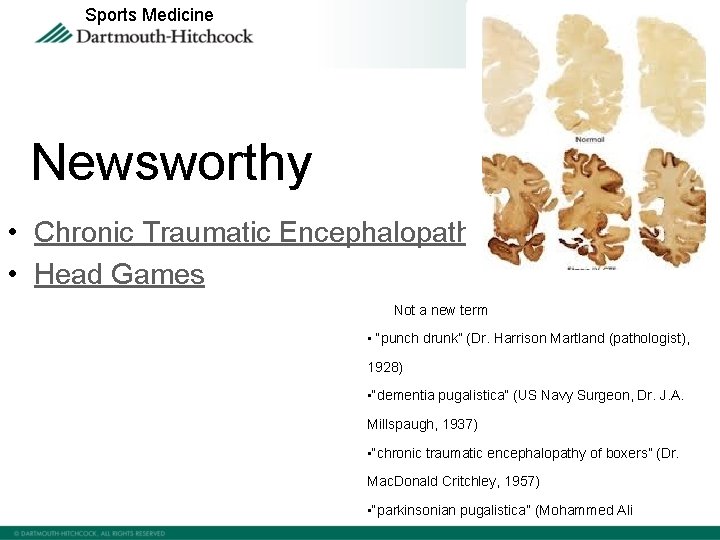
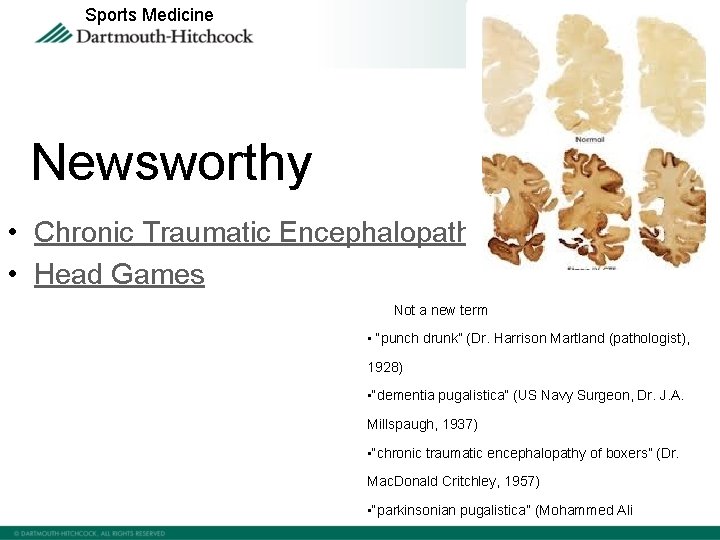
Sports Medicine Newsworthy • Chronic Traumatic Encephalopathy • Head Games • Not a new term • “punch drunk” (Dr. Harrison Martland (pathologist), 1928) • “dementia pugalistica” (US Navy Surgeon, Dr. J. A. Millspaugh, 1937) • “chronic traumatic encephalopathy of boxers” (Dr. Mac. Donald Critchley, 1957) • “parkinsonian pugalistica” (Mohammed Ali)
Sports Medicine How to get better: • Physical rest; avoid physical activity including gym class, after school play, sports, etc. • Mental rest; avoid tests, computer use, television, video games, texting, reading, studying, etc. • Emotional rest • Get plenty of sleep at night, and rest during the day. • Ask your doctor if you can
Sports Medicine Sleep Hygiene ü Consistent bedtime and wake-up time ü Avoid excessive daytime napping ü Dim lights, calm atmosphere ü Avoid computers, TV, and texting for one hour prior to bedtime ü Sleep-promoting environment ü No exercise 3 hrs prior to bedtime ü Mornings with bright light, breakfast, and
Sports Medicine Healing time: Unfortunately there is no way to tell how long it will take to heal from a concussion. Recovery depends on numerous factors: How severe the concussion was Age of the athlete How healthy the athlete was before the concussion How the athlete takes care of themselves after the injury History of previous concussions Individual biology
Sports Medicine Children are not plastic… • Recovery times longer than previously thought • Higher incidence for long-term physical, cognitive and emotional sequelae when not managed appropriately. • Medical management necessary to ensure appropriate school-based treatment planning • Developing skills such as executive control processes are particularly vulnerable. • Some parents may find it hard to access appropriate care, no ATC, access to doctor who is knowledgeable in sports concussion management • Girls may be more susceptible (theory of weaker neck muscles)
Sports Medicine Assessing Executive Function in Younger Student. Athletes 1) 2) 3) 4) 5) 6) Keeping track of time and finishing work on time: have homework done in an hour Meaningfully include past knowledge in discussions: remember when we went to the park and we saw that dog Evaluate ideas and reflect on work: coloring, making a sand castle, playing with blocks Change our minds and make mid-course corrections while thinking, reading, and writing: do you want popcorn or chocolate at the movies, what movie to see, deciding what to have for dinner, or wear to school on a cold or warm day Engage in group dynamics: play group, watching TV with family Asking for help or seek more information when needed: where is the bathroom, can’t tie shoe laces.
Sports Medicine Return to learn before Return to play!

Sports Medicine SCHOOL ACCOMMODATIONS Students must be back to school fully before being allowed back to play. ü ü ü Extended time to turn in assignments Workload reduction Systematic plan with support and supervision Note takers Reduce multi-tasking Allow for breaks and quiet time Extend test time Testing in quiet environment Fewer and shorter tests Defer standardized or high-stakes tests No more than one test per day Multiple choice or cueing, rather than free response format
Sports Medicine Incidence (www. cdc. gov) • During the last decade, Emergency Department (ED) visits for sports/recreationrelated TBIs, including concussions, among children and adolescents increased by 60%. • Overall, the activities associated with the greatest number of TBI-related ED visits included bicycling, football, playground activities, basketball, and soccer. • 71% of all sports/recreation-related TBI ED visits were males. • 70% of sports/recreation-related TBI ED visits were persons aged 10 -19 years. • For males aged 10 -19 years, sports- and recreation-related TBIs occurred most often while playing football or bicycling. • Females aged 10 -19 years sustained sports- and recreation-related TBIs most often while playing soccer or basketball or while bicycling.
Sports Medicine Return to Play: How to know if the Doctor is up to date? • • Mild, Moderate, or Severe. Grade I, II, or III. Must have a loss of consciousness. Return to play after headache disappears. Sit out 7 days, then return to play. Repeatedly wake up the concussed person. Must have a MRI or CT scan.
Sports Medicine Support & Resources http: //www. cdc. gov/concussion/ http: //patients. dartmouth-hitchcock. org/ortho/sports_concussion_program. html www. impacttest. com Online Coaches Training: http: //cdc. gov/concussion/Heads. Up/online_training. html
Sports Medicine Red Flags! Go to an emergency department right away if: • Look very drowsy or cannot be awakened. • Have one pupil (the black part in the middle of the eye) larger than the other. • Have convulsions or seizures. • Cannot recognize people or places. • Getting increasingly confused, restless, or agitated, rapidly worsening headache. • Have unusual behavior. • Lose consciousness (a brief loss of consciousness should be taken seriously and the person should be carefully monitored). • Weakness, numbness or decreased coordination. • Repeated vomiting or nausea. • Slurred speech.
Sports Medicine Pieces of the diagnostic puzzle: • • Sideline recognition/on field assessment Neurocognitive screening (Im. PACT) Vestibular assessment (balance) Physical exam with coordination assessment
Sports Medicine Sports Concussion Assessment Tool 2 (SCAT 2): A standardized method of evaluating injured athletes for concussion and can be used in athletes aged from 10 years and older. Assessment Includes: Symptoms: 22 possible Cognitive & Physical Assessment LOC? Glasgow coma scale: eye, verbal, motor Orientation: Month, Date, Day of the week, year, time? Immediate Memory recall: 5 word recall: (elbow, apple, carpet, saddle, bubble) Concentration: Repeat Digits Backwards: 3 -9 -7, 4 -6 -1 -0, 2 -9 -6 -1 -4 Months of the year in reverse order Balance Coordination *Now available to download as an app onto a smart phone.
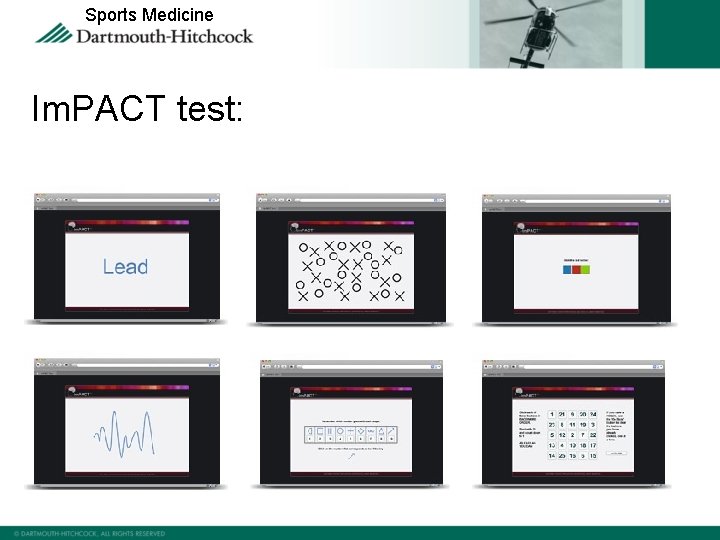
Sports Medicine Immediate Post-Concussion Assessment and Cognitive Testing v. Im. PACT testing is a 30 -45 minute neurocognitive test battery that has been scientifically validated to measure the effects of sports related concussion. v. Im. PACT is available for athletes age 11 to 65 v. All athletes should have a baseline test prior to playing sports: Middle School & High School: test every two years College: test once Professional athletes: test once v. Athletes with no Baseline test: Athletes should be retested within 2472 hours of sustaining a possible concussion. v. Athletes with a Baseline test: Athletes should be retested when they are completely symptom free.
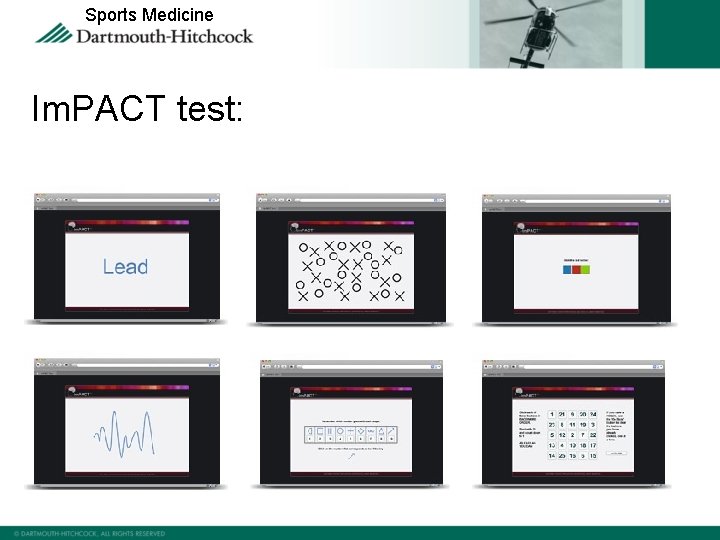
Sports Medicine Im. PACT test:
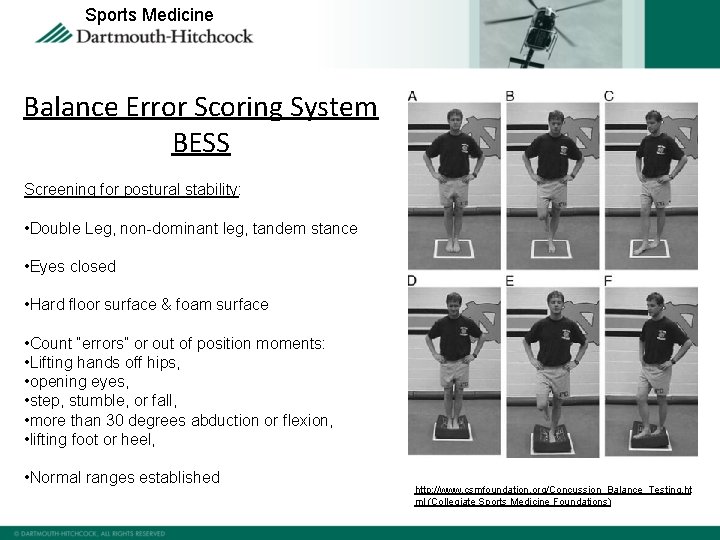
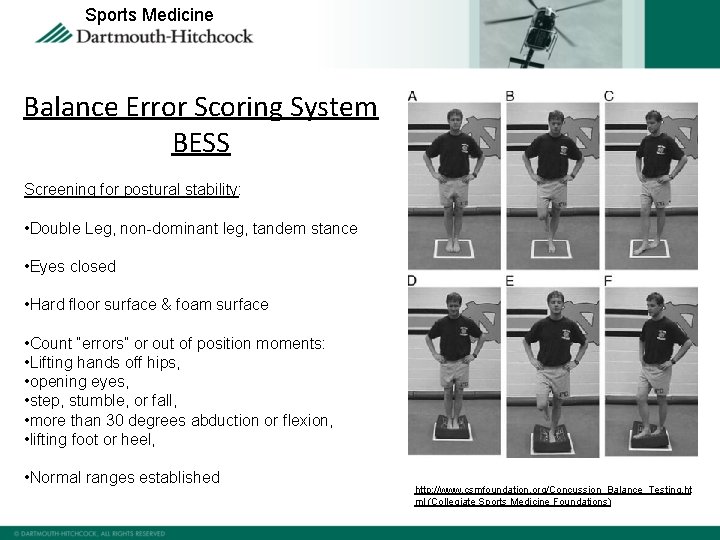
Sports Medicine Balance Error Scoring System BESS Screening for postural stability: • Double Leg, non-dominant leg, tandem stance • Eyes closed • Hard floor surface & foam surface • Count “errors” or out of position moments: • Lifting hands off hips, • opening eyes, • step, stumble, or fall, • more than 30 degrees abduction or flexion, • lifting foot or heel, • Normal ranges established http: //www. csmfoundation. org/Concussion_Balance_Testing. ht ml (Collegiate Sports Medicine Foundations)
Sports Medicine Videos: Physiology of a concussion: 3: 30 minutes Play Smart: Brain Injury Assoc. of Mass. : understanding sports concussion with Dr. Cantu ADAM Concussion animation: 20 seconds Concussion 101 white board: 5: 51 minutes ESPN Sport Science: 1: 28 shows g force in helmet to helmet collisions College football: 1 minute (endzone) Barcelona soccer player: April 24, 2012: He got back up and continued to play. Eight minutes later he signaled to the coaching staff of the sidelines that he could no longer play. He was removed from the game. He was transported to a hospital where he was admitted for observation. Sidney Crosby hit behind the play: 17 seconds Soccer player: 47 seconds NHL concussion epidemic: starts at 5: 29 approx 3 minutes long
Sports Medicine Thank-you for this opportunity. concussion@hitchcock. org Susanna
 Ohsaa concussion return to play protocol
Ohsaa concussion return to play protocol Concussion and contusion
Concussion and contusion Grade 2 concussuon
Grade 2 concussuon Pwcs concussion training answers
Pwcs concussion training answers Grade 2 concussion
Grade 2 concussion Concussion betekenis
Concussion betekenis Concussion
Concussion Concussion protocol gaa
Concussion protocol gaa Kinesthetic learner
Kinesthetic learner Assume risk and return are positively related
Assume risk and return are positively related Skill related fitness
Skill related fitness Two type of physical fitness
Two type of physical fitness The manager of a sports arena wants to learn
The manager of a sports arena wants to learn The manager of a sports arena wants to learn
The manager of a sports arena wants to learn Objective of sports medicine
Objective of sports medicine Soap sports med
Soap sports med Hops definition sports medicine
Hops definition sports medicine Chapter 2 sports medicine
Chapter 2 sports medicine Sports medicine team definition
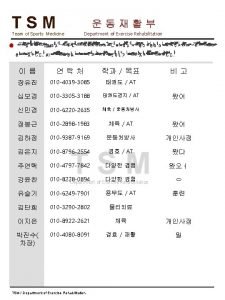
Sports medicine team definition Meditouch sports medicine
Meditouch sports medicine Athletic training sports medicine
Athletic training sports medicine What is the importance of taping and wrapping?
What is the importance of taping and wrapping? Hops sports medicine examples
Hops sports medicine examples Sports medicine umbrella
Sports medicine umbrella Sports medicine taping techniques
Sports medicine taping techniques Sports venues vocabulary
Sports venues vocabulary Rop sports medicine
Rop sports medicine Scope of sports medicine
Scope of sports medicine Sports medicine meaning
Sports medicine meaning Heel raise
Heel raise