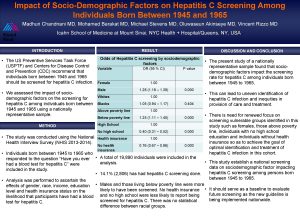
Sociodemographic Factors Associated With Choice of Primary Care


- Slides: 29
Sociodemographic Factors Associated With Choice of Primary Care Provider In Siem Reap, Cambodia Brett M. Schmitz MD MPH Family Medicine Global Health Workshop Denver, CO September 11, 2009
Background The unique challenges faced by the Cambodian health care system from over 30 years of political instability. 2 million persons were killed during the Khmer Rouge regime from 1975 -1979 leaving only 30 healthcare professionals alive. Lanjouw & Macrae, 1999; Heng, 1995
Background Specific issues that have limited past utilization of HCs include: Lack of training Corruption/side payments Staff absenteeism Lack of infrastructure Poor quality of services Variability of service offerings Soeters and Griffiths, 2003; Jacobs and Price, 2004; Akashi, et al 2004
Background In 1995 the Cambodian government introduced two major reforms: Established health care specific Operational Districts distinct from political Administrative districts Mandated a universal list of services called the Minimum Package of Activities (MPA) Walford, 2000; Ministry of Health, 1997
Background The Operational Health District is the primary organizational level in the Cambodian health system ODs provide services through health centers and a single referral hospital ODs contain between 100, 000 and 200, 000 people, with one health center per 10, 000– 12, 000 population Soeters and Griffiths, 2003; Jacobs and Price, 2004; Akashi, et al 2004
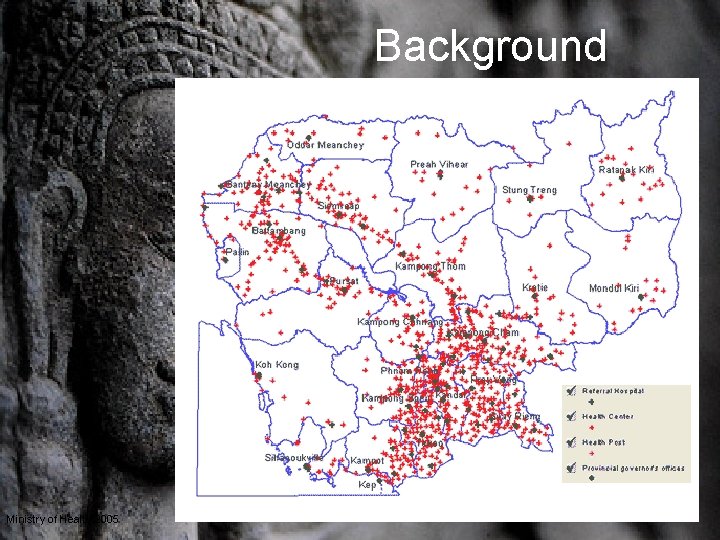
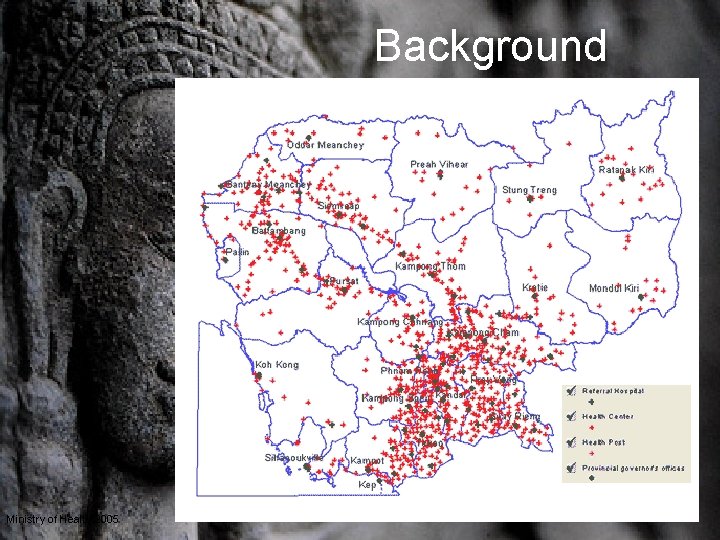
Background Ministry of Health 2005
Background The MPA includes the following service categories: Primary care Childbirth Prenatal care Birth spacing Minor surgery TB treatment Leprosy treatment Gynecology Transitional Services Soeters and Griffiths, 2003; Jacobs and Price, 2004; Akashi, et al 2004
Background The Capacity Building and Health Education Program (CBHEP) is a local NGO working with the Ministry of Health to develop the capacity and increase utilization of local health centers.
Background CBHEP’s interventions have focused on: Training of HC personnel Infrastructure improvements Community Outreach efforts by CBHEP and the Ministry of health have targeted poor, rural populations and focused on educating people about the availability of services (MPA) and improvements in service quality.
Background CBHEP had been successful in improving utilization in some HCs, but some districts remained static or lagged behind others even though capacity and quality of services was similar.
Questions Is it any better for people to use the public system? Pharmacies are often family businesses with no trained pharmacist on hand Studies from Vietnam show that public providers adhere more closely to best practices and have better outcomes than their unregulated private counterparts. Gollogly, 2002; Tuan et al, 2005;
Questions What factors underlie health seeking behaviors? Studies in other developing countries have shown socioeconomic status, gender, age, ethnic background, and geographic location to be important factors. Develay et al, 1996; Russell S, 2005, Ahmed et al, 2005, Uzochukwu and Onwujekwe, 2004; Toan et al, 2002; Suraratdecha et al, 2005; Taffa and Chepngeno, 2005; Thompson et al, 2003; Gulliforda and Mahabirb, 2001; Lonnroth et al, 2001
Goals To assess what factors are important in determining primary care provider choice To get descriptive data for those living in the service areas of the 6 health centers CBHEP is currently aiding. To provide strategic guidance to CBHEP, the Cambodian Ministry of Health, and other organizations in their capacity building activities.
Methods 16 Village Health Volunteers (VHVs), trained by CBHEP, served as survey administrators. Cross-sectional survey was orally administered in Khmer.
Methods 618 heads of household representing 4005 individuals were surveyed in 102 different villages served by the 6 HCs partnered with CBHEP. Survey assessed health seeking behavior, provider utilization, as well as socioeconomic factors.
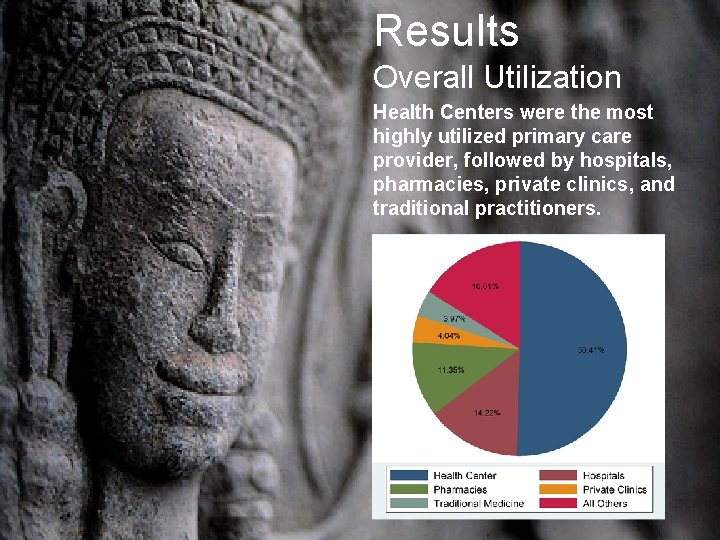
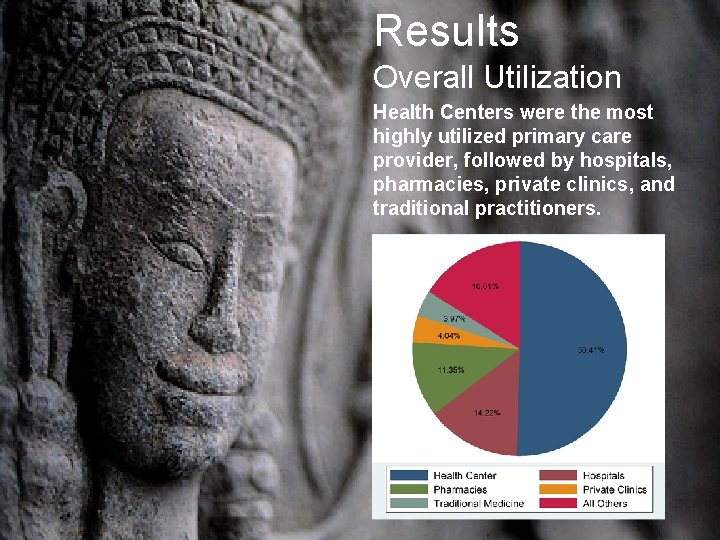
Results Overall Utilization Health Centers were the most highly utilized primary care provider, followed by hospitals, pharmacies, private clinics, and traditional practitioners.
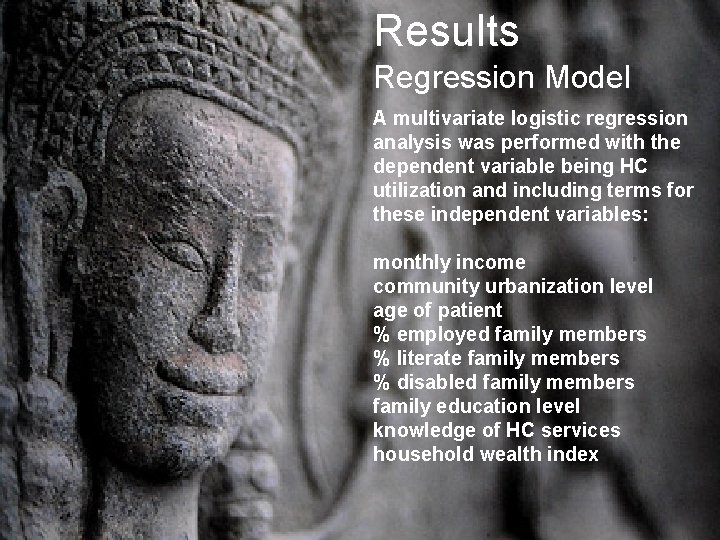
Results Regression Model A multivariate logistic regression analysis was performed with the dependent variable being HC utilization and including terms for these independent variables: monthly income community urbanization level age of patient % employed family members % literate family members % disabled family members family education level knowledge of HC services household wealth index
Results Health Centers The factor correlating most powerfully with health center utilization is the urbanization of the community, with higher levels of urbanization correlating to lower utilization of the health center (B = -20. 954, p <0. 001, 95% CI = -25. 210, -16. 99).
Results Health Centers Higher incomes also correlated with lower health center utilization (B = -5. 992, p =0. 015, 95% CI = -10. 823, -1. 161) A separate regression analysis revealed that exposure to negative rumors about private clinics in the area correlated very strongly with increased utilization of health centers (B = 21. 986, p <0. 001, 95% CI = 10. 823, 33. 149)
Results Private Clinics For every MPA service known by the respondent, there is a decrease in private clinic utilization by 1. 410% (p < 0. 001, 95% CI = -2. 016, -. 804) Household wealth index is positively correlated with increased utilization of private clinics, with every 1 point increase in the index associated with a 0. 5% increase in private clinic utilization (p = 0. 001, 95% CI =. 199, . 801)
Results Hospitals There is an increase of 6. 727% in hospital utilization for each increase in level of urbanization (p < 0. 001, 95% CI = 3. 876, 9. 578) No other factors had a significant association with hospital utilization.
Results Pharmacies There is an increase of 8. 846% in pharmacy utilization for each increase in level of urbanization (p < 0. 001, 95% CI = 6. 617, 11. 074) For every MPA service known by the respondent, there is a decrease in pharmacy utilization by 1. 129% (p < 0. 01, 95% CI = -1. 929, -0. 329)

Results Traditional Medicine Urbanization (B = 1. 302, p <. 05, 95% CI =. 113, 2. 491) % Family members < age 18 (B = -0. 056, p <. 05, 95% CI = -. 110, -. 002) % Family members employed (B = -0. 061, p <. 05, 95% CI = -. 119, -. 002) % Family Members Literate (B = 0. 039, p <. 05, 95% CI = -. 072, . 006).
Summary Urbanization of the community plays a large role in determining the utilization of all major primary care providers. It is associated with decreases in HC utilization, increases all others.
Summary Higher levels of monthly income are also strongly associated with decreased utilization of HCs. Negative rumors about Private services are associated with increases in HC utilization, but not the other way around. Knowledge of HC MPA offerings was not associated with increased HC utilization, but are associated with a lower utilization of pharmacies and private clinics for primary care.
Implications Future outreach interventions aimed at increasing utilization of HCs should focus on those underutilizing the resource: middle and higher income individuals living in urban areas. Also, the focus of outreach needs to change from only educating individuals about HC service offerings and increased quality to additionally highlighting the dangers of utilizing unregulated private practitioners and drug sellers.

Thank You!
References Ahmed SM, Tomson G, Petzold M, Kabir ZN. 2005. Socioeconomic status overrides age and gender in determining health-seeking behaviour in rural Bangladesh. Bulletin of the World Health Organization; 83: 109 -117. Akashi H, Yamada T, Huot E, Kanal K, Sugimoto T. 2004. User fees at a public hospital in Cambodia: effects on hospital performance and provider attitudes. Social Science & Medicine; 58: 553– 564. Develay A, Saurborn R, Diesfeld HJ. 1996. Utilization of health care in an African urban area: Results from a household survey in Ouagadougou, Burkina-Faso. Social Science and Medicine; 43(11): 16111619. Filmer D, Pritchett L. 1998. Estimating wealth effects without expenditure data -- or tears: An application to educational enrolments in States of India, World Bank Policy Research Working Paper No. 1994; Washington. Gollogly L. 2002. The dilemmas of aid: Cambodia 1992– 2002. The Lancet; 360: 793 -798. Gulliforda MC, Mahabirb D. 2001. Utilisation of private care by public primary care clinic attenders with diabetes: relationship to health status and social factors. Social Science & Medicine; 53: 1045– 1056. Hardeman W, Van Damme W, Van Pelt M, Por I, Kimvan H, Meessen B. 2004. Access to health care for all? User fees plus a Health Equity Fund in Sotnikum, Cambodia. Health Policy and Planning; 19: 22– 32. Heng M, Key PJ. 1995. Cambodian health in transition. British Medical Journal; 311: 435 -437. Jacobs B, Price N. 2004. The impact of the introduction of user fees at a district hospital in Cambodia. Health Policy and Planning; 19: 311– 22. Jacobs B, Price N. 2006. Improving access for the poorest to public sector health services: insights from Kirivong Operational Health District in Cambodia. Health Policy and Planning; 21(1): 27 -39. Lanjouw S, Macrae J, Zwi A. 1999. Rehabilitating health services in Cambodia: the challenge of coordination in chronic political emergencies. Health Policy and Planning; 14(3): 229 -242. Leighton, C. 1995. Overview: Health financing reforms in Africa. Health Policy and Planning, 10(3): 213– 222. Lonnroth K, Minh Thoung LE, Linh PD, Diwan VK. 2001. Utilization of private and public health-care providers for tuberculosis symptoms in Ho Chi Minh City, Vietnam. Health Policy and Planning; 16(1): 47– 54. Ministry of Health Cambodia. 1997. Guidelines for Developing Operational Districts. Ministry of Health Cambodia, Phnom Penh. National Center for HIV/AIDS, Dermatology, and STDs (NCHADS). 2003. Health Facility Assessment in Seven Provinces of Cambodia. Ministry of Health Cambodia, Phnom Penh.
References Portero Navio JL, Rubio Yuste M, Pasicatan MA. 2002. Socio-economic determinants of knowledge and attitudes about tuberculosis among the general population of Metro Manila, Philippines. International Journal of Tuberculosis and Lung Disease ; 6(4): 301– 306. Russell S. 2005. Treatment-seeking behaviour in urban Sri Lanka: Trusting the state, trusting private providers. Social Science & Medicine; 61: 1396– 1407 Soeters R, Griffiths F. 2003. Improving government health services through contract management: a case from Cambodia. Health Policy and Planning; 18(1): 74– 83. Suraratdecha C, Saithanu S, Tangcharoensathien V. 2005. Is universal coverage a solution for disparities in health care? Findings from three low-income provinces of Thailand. Health Policy; 73: 272– 284. Taffa N, Chepngeno G. 2005. Determinants of health care seeking for childhood illnesses in Nairobi slums. Tropical Medicine and International Health ; 10(3): 240– 245. Thompson R, Miller N, Witter S. 2003. Health-seeking behaviour and rural/urban variation in Kazakhstan. Health Economics; 12: 553– 564. Toan NV, Trong LN, Hojer B, Persson LA. 2002. Public health services use in a mountainous area, Vietnam: implications for health policy. Scandinavian Journal of Public Health ; 30: 86 -93. Tuan T, Dung VT, Neu I, Dibley MJ. 2005. Comparative quality of private and public health services in rural Vietnam. Health Policy and Planning; 20(5): 319 -27. UNDP. 1997. Capacity development and UNDP: Supporting Sustainable Human Development Uzochukwu B, Onwujekwe OE. 2004. Socio-economic differences and health seeking behaviour for the diagnosis and treatment of malaria: a case study of four local government areas operating the Bamako initiative programme in south-east Nigeria. International Journal for Equity in Health ; 3: 6. Walford, V. 2000. Cambodia: Country Health Briefing Paper. Department for International Development Health Systems Resource Center (DFID HSRC), London.
 Levels of care primary secondary tertiary quaternary
Levels of care primary secondary tertiary quaternary Good choice or bad choice
Good choice or bad choice Contingency factors affecting structural choice
Contingency factors affecting structural choice Functional strategy and strategic choice
Functional strategy and strategic choice Functional strategy and strategic choice
Functional strategy and strategic choice Intrathecal route advantages and disadvantages
Intrathecal route advantages and disadvantages Factors influencing the choice of programming language
Factors influencing the choice of programming language Stimulus-based questions examples
Stimulus-based questions examples Site v situation
Site v situation Abiotic factors example
Abiotic factors example Abiotic vs biotic factors
Abiotic vs biotic factors Abiotic vs biotic factors
Abiotic vs biotic factors Abiotic vs biotic factors
Abiotic vs biotic factors Site vs. situation
Site vs. situation Highest common factor of 36 and 48
Highest common factor of 36 and 48 Factors if 7
Factors if 7 Gcf 15 and 20
Gcf 15 and 20 Magenta cyan and yellow are the ____ color. *
Magenta cyan and yellow are the ____ color. * The factors of care that patient can expect
The factors of care that patient can expect Trafford primary care trust
Trafford primary care trust Uccs health circle
Uccs health circle Australian primary health care research institute
Australian primary health care research institute Starfield primary care
Starfield primary care Functional nursing
Functional nursing Dc primary care association
Dc primary care association Pengertian primary health care
Pengertian primary health care Principles of primary health care
Principles of primary health care Site:slidetodoc.com
Site:slidetodoc.com Defination of primary health care
Defination of primary health care Concepts of primary health care
Concepts of primary health care