Secondary Amenorrhea District I ACOG Medical Student Education
- Slides: 20
Secondary Amenorrhea District I ACOG Medical Student Education Module 2011
Definitions • Amenorrhea: absence of menses – Primary: absence of menarche by age 16 – Secondary: absence of menses in women who previously had menses. Absence must be for • > 3 cycles according to certain sources • > 6 months according to most sources
Etiologies • Don’t forget PREGNANCY! – Most common cause of secondary amenorrhea – Rule out with a urine or serum hcg before proceeding • Consider each level of the control of the menstrual cycle: – Hypothalamus – Pituitary – Ovary – Uterus – Cervix – Vagina Involved in endocrine regulation of the menstrual cycle Responds to endocrine cues from the HPO axis Involved structurally in the outflow of menstrual blood
Most Common Etiologies of Secondary Amenorrhea (after excluding Pregnancy) • Ovarian disease (40%) • Hypothalamic dysfunction (35%) • Pituitary disease (19%) • Uterine disease (5%) • Other (1%)
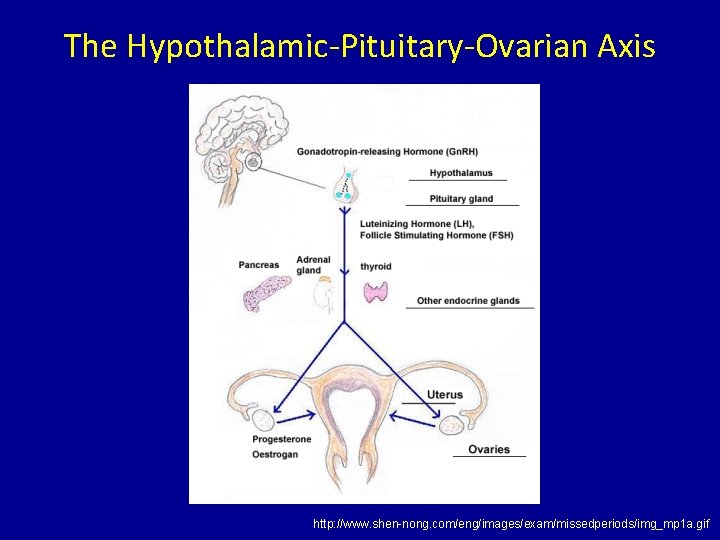
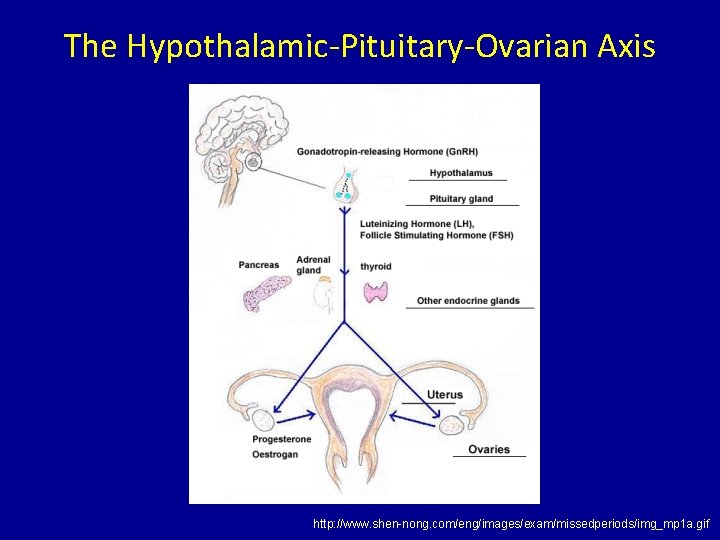
The Hypothalamic-Pituitary-Ovarian Axis http: //www. shen-nong. com/eng/images/exam/missedperiods/img_mp 1 a. gif
Dysfunction of the H-P-O Axis • Hypothalamic dysfunction – Functional hypothalamic amenorrhea – Inflammatory or infiltrative diseases of the hypothalamus (lymphoma, Langerhans cell histiocytosis, sarcoidosis) – Systemic Disease (e. g. Celiac disease) Adapted from “Etiology, diagnosis and treatment of secondary amenorrhea”, Up. To. Date 2010
Functional Hypothalamic Amenorrhea • Absence of menses due to suppression of HPO axis in which no anatomic or organic disease is identified – Suppression of Gn. RH pulsitility ( in Gn. RH ) – Suppression of LH, FSH – Suppression of estradiol • Causes – – Weight Loss, eating disorders Frequent/vigorous exercise Stress Severe/prolonged illness
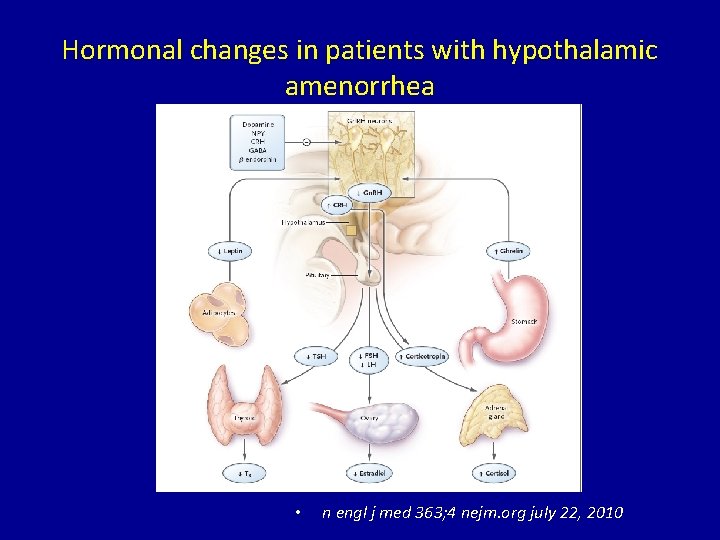
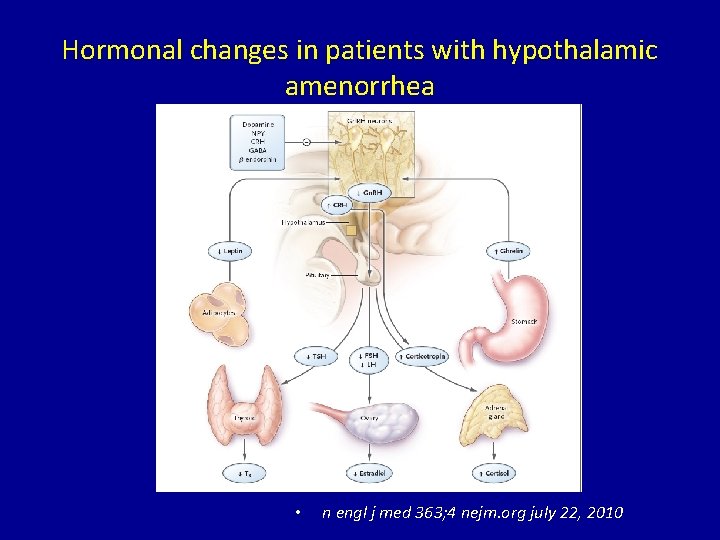
Hormonal changes in patients with hypothalamic amenorrhea • n engl j med 363; 4 nejm. org july 22, 2010
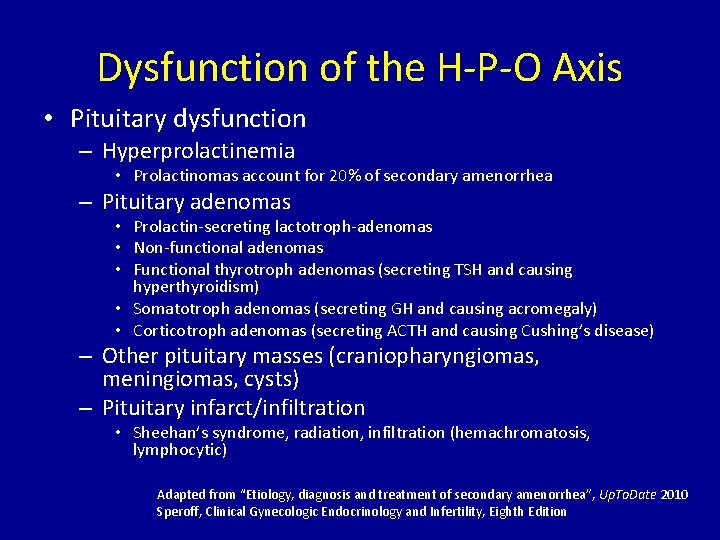
Dysfunction of the H-P-O Axis • Pituitary dysfunction – Hyperprolactinemia • Prolactinomas account for 20% of secondary amenorrhea – Pituitary adenomas • Prolactin-secreting lactotroph-adenomas • Non-functional adenomas • Functional thyrotroph adenomas (secreting TSH and causing hyperthyroidism) • Somatotroph adenomas (secreting GH and causing acromegaly) • Corticotroph adenomas (secreting ACTH and causing Cushing’s disease) – Other pituitary masses (craniopharyngiomas, meningiomas, cysts) – Pituitary infarct/infiltration • Sheehan’s syndrome, radiation, infiltration (hemachromatosis, lymphocytic) Adapted from “Etiology, diagnosis and treatment of secondary amenorrhea”, Up. To. Date 2010 Speroff, Clinical Gynecologic Endocrinology and Infertility, Eighth Edition
Dysfunction of the H-P-O Axis • Ovarian dysfunction – Ovarian failure (menopause): 1 year of amenorrhea due to depletion of oocytes • Spontaneous: typically occurs at age 52 in American women • Premature: < 40 years old – Autoimmune conditions » lymphocytic infiltrate in theca cells of ovarian follicles – Chemotherapy/radiation – Fragile X premutation – Karyotypic abnormalities » Turner Syndrome, loss of small portion of X chromosome, mosaic Turner Syndrome, presence of Y chromatin material • Surgical – Hyperandrogenism • Polycystic Ovary Syndrome (PCOS) Adapted from “Etiology, diagnosis and treatment of secondary amenorrhea”, Up. To. Date 2010 Speroff, Clinical Gynecologic Endocrinology and Infertility, Eighth Edition
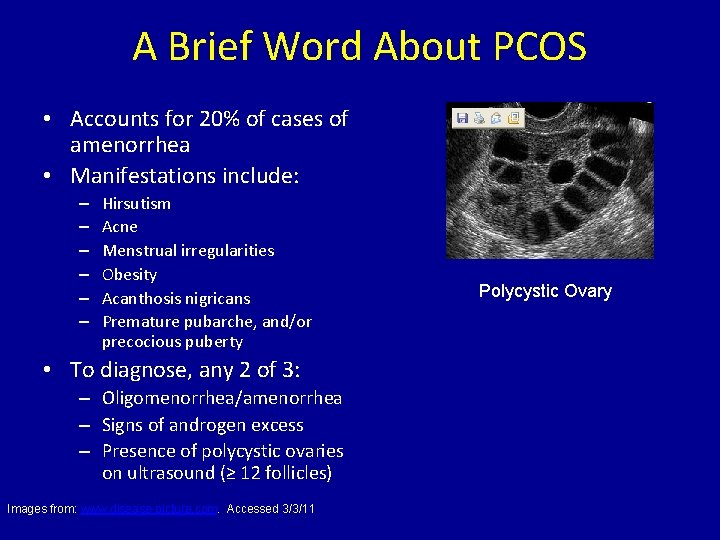
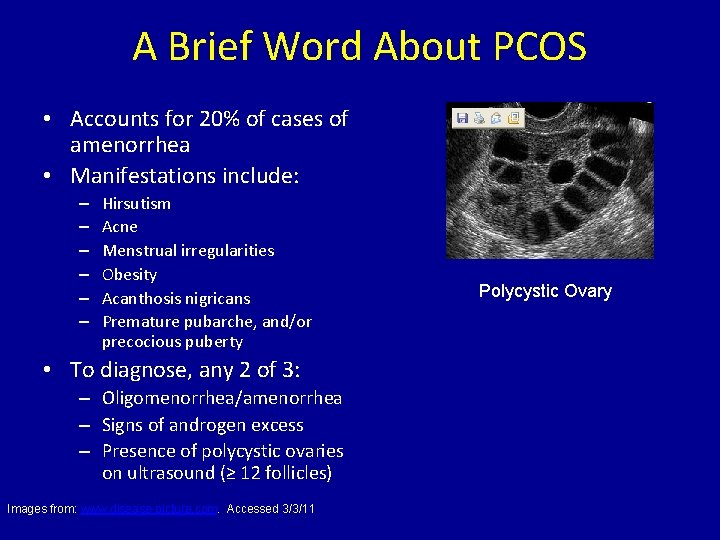
A Brief Word About PCOS • Accounts for 20% of cases of amenorrhea • Manifestations include: – – – Hirsutism Acne Menstrual irregularities Obesity Acanthosis nigricans Premature pubarche, and/or precocious puberty • To diagnose, any 2 of 3: – Oligomenorrhea/amenorrhea – Signs of androgen excess – Presence of polycystic ovaries on ultrasound (≥ 12 follicles) Images from: www. disease-picture. com. Accessed 3/3/11 Polycystic Ovary
Other Endocrine Etiologies of Amenorrhea • Hyperthyroidism/hypothyroidism • Diabetes Mellitus • Exogenous androgen use
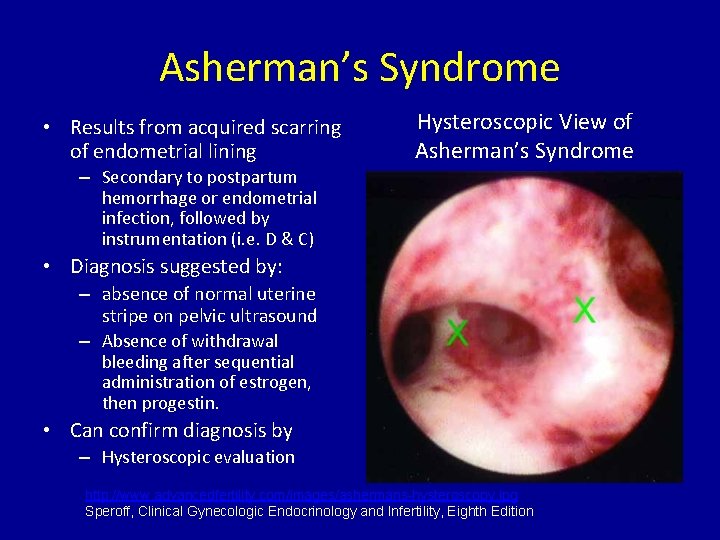
Structural Etiologies of Secondary Amenorrhea • Uterine Scarring – Asherman’s Syndrome – Endometrial Ablation • Cervical Stenosis, often due to instrumentation – LEEP – Conization
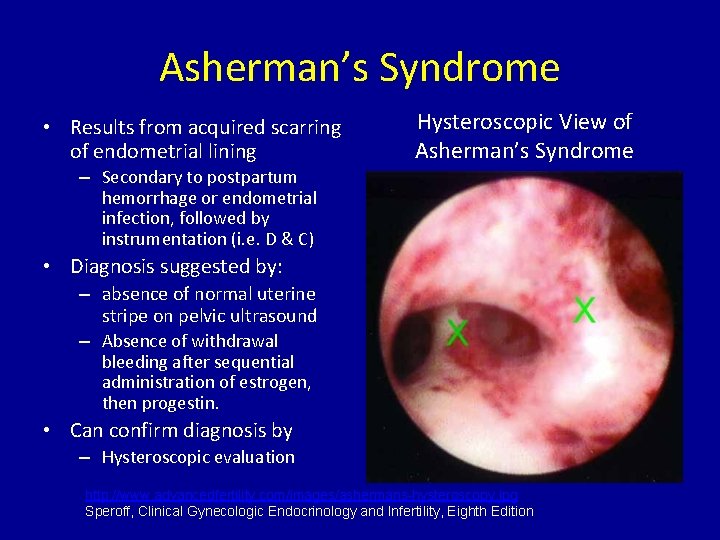
Asherman’s Syndrome • Results from acquired scarring of endometrial lining Hysteroscopic View of Asherman’s Syndrome – Secondary to postpartum hemorrhage or endometrial infection, followed by instrumentation (i. e. D & C) • Diagnosis suggested by: – absence of normal uterine stripe on pelvic ultrasound – Absence of withdrawal bleeding after sequential administration of estrogen, then progestin. • Can confirm diagnosis by – Hysteroscopic evaluation http: //www. advancedfertility. com/images/ashermans-hysteroscopy. jpg Speroff, Clinical Gynecologic Endocrinology and Infertility, Eighth Edition
Diagnosis • Exclude Pregnancy • History: – Recent stress, weight change, new diet or exercise habits, illness? – New acne, hirsutism, voice deepening? – New medications? • • Recent initiation or discontinuation of OCPs Danazol/androgenic drugs High-dose progestins Metoclopramide and antipsychotics – Can increase serum prolactin amenorrhea Adapted from “Etiology, diagnosis and treatment of secondary amenorrhea”, Up. To. Date 2010
Diagnosis • History: – Symptoms of hypothalamic-pituitary disease? • • • Headaches Galactorrhea Visual field defects Fatigue Polyuria, polydipsia – Symptoms of estrogen deficiency? • • Hot flashes Vaginal dryness Poor sleep Decreased libido – History of obstetrical catastrophe, severe bleeding, infection, D&C? (Possible Asherman’s Syndrome) Adapted from “Etiology, diagnosis and treatment of secondary amenorrhea”, Up. To. Date 2010
Diagnosis • Physical Exam – BMI • BMI > 30 kg/m 2 seen in 50% of women with PCOS • BMI < 18. 5 kg/m 2 may have functional hypothalamic amenorrhea – Signs of systemic illness/cachexia – Evaluate genital tissue for signs of estrogen deficiency – Palpate breasts/attempt to express galactorrhea – Neuro exam for visual field defects – Skin exam, evaluating for • Stigmata of PCOS: Hirsutism, acne, acanthosis nigricans • Stigmata of thyroid disorders: thin/dry skin, skin thickening • Stigmata of Cushing’s disease: striae Adapted from “Etiology, diagnosis and treatment of secondary amenorrhea”, Up. To. Date 2010
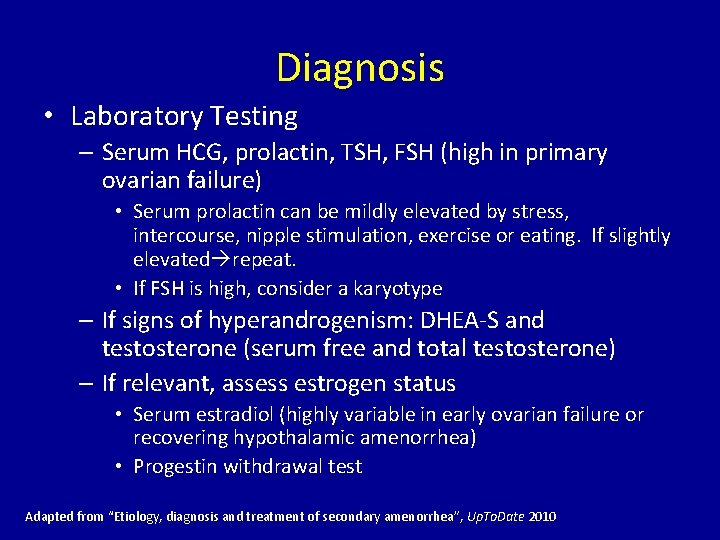
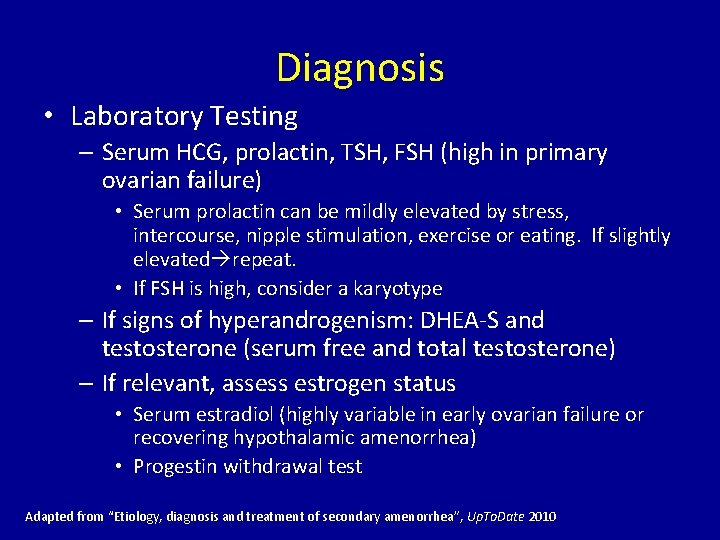
Diagnosis • Laboratory Testing – Serum HCG, prolactin, TSH, FSH (high in primary ovarian failure) • Serum prolactin can be mildly elevated by stress, intercourse, nipple stimulation, exercise or eating. If slightly elevated repeat. • If FSH is high, consider a karyotype – If signs of hyperandrogenism: DHEA-S and testosterone (serum free and total testosterone) – If relevant, assess estrogen status • Serum estradiol (highly variable in early ovarian failure or recovering hypothalamic amenorrhea) • Progestin withdrawal test Adapted from “Etiology, diagnosis and treatment of secondary amenorrhea”, Up. To. Date 2010
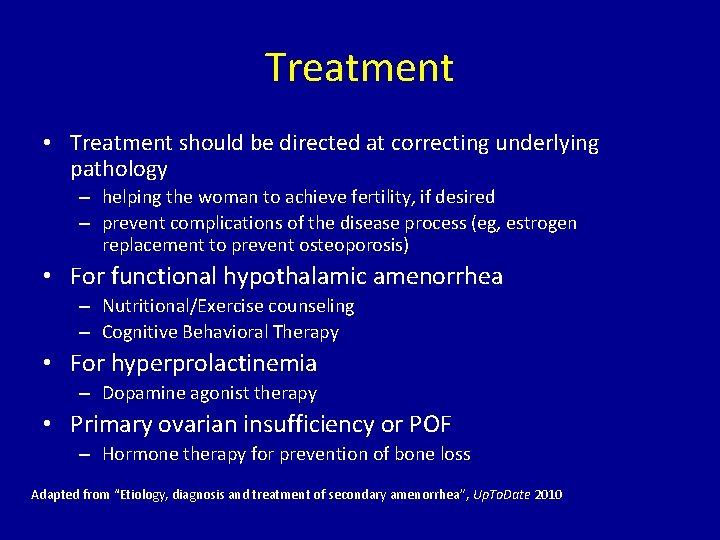
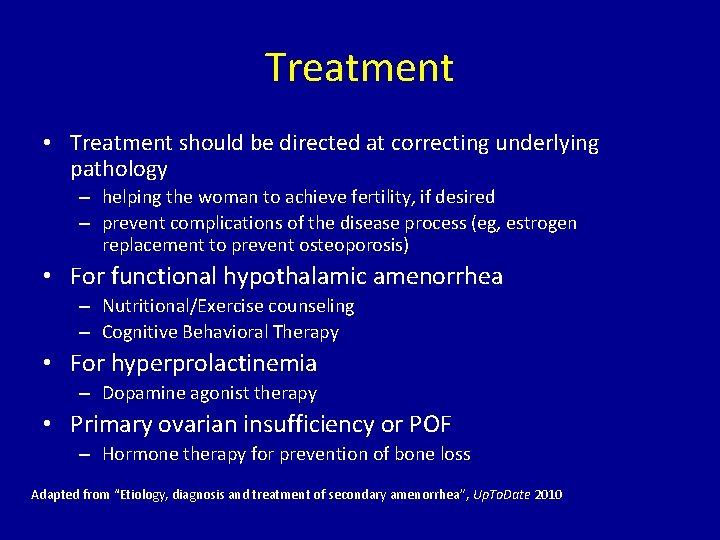
Treatment • Treatment should be directed at correcting underlying pathology – helping the woman to achieve fertility, if desired – prevent complications of the disease process (eg, estrogen replacement to prevent osteoporosis) • For functional hypothalamic amenorrhea – Nutritional/Exercise counseling – Cognitive Behavioral Therapy • For hyperprolactinemia – Dopamine agonist therapy • Primary ovarian insufficiency or POF – Hormone therapy for prevention of bone loss Adapted from “Etiology, diagnosis and treatment of secondary amenorrhea”, Up. To. Date 2010
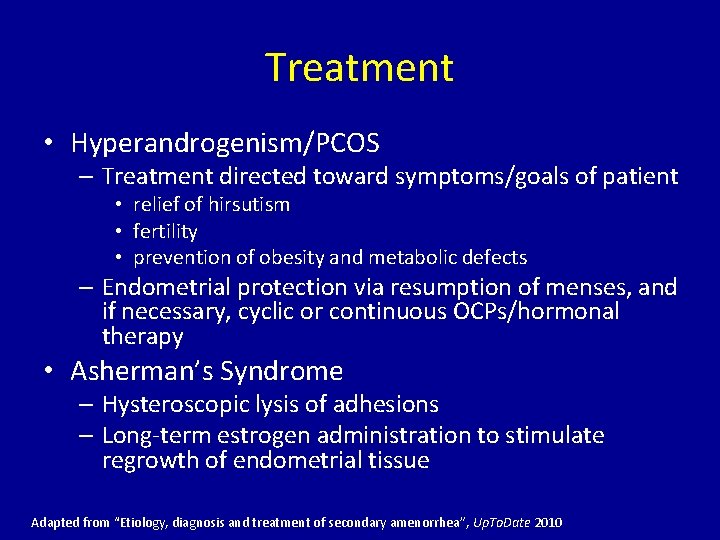
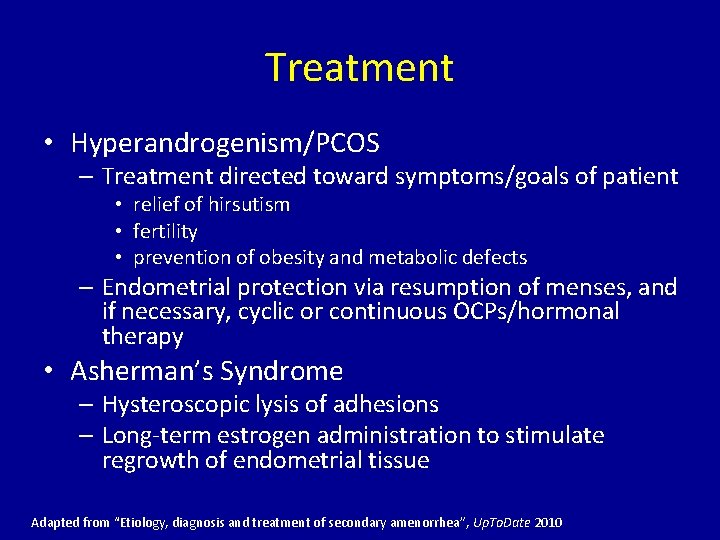
Treatment • Hyperandrogenism/PCOS – Treatment directed toward symptoms/goals of patient • relief of hirsutism • fertility • prevention of obesity and metabolic defects – Endometrial protection via resumption of menses, and if necessary, cyclic or continuous OCPs/hormonal therapy • Asherman’s Syndrome – Hysteroscopic lysis of adhesions – Long-term estrogen administration to stimulate regrowth of endometrial tissue Adapted from “Etiology, diagnosis and treatment of secondary amenorrhea”, Up. To. Date 2010
 Helper in shoulder dystocia
Helper in shoulder dystocia Endometriosis amenorrhea
Endometriosis amenorrhea Causes of secondary amenorrhea
Causes of secondary amenorrhea Palm coein acog
Palm coein acog Palm coien
Palm coien Acog classificazione ctg
Acog classificazione ctg Acog flowsheet
Acog flowsheet Blighted ovum criteria acog
Blighted ovum criteria acog Acog thyroid pregnancy
Acog thyroid pregnancy Anovulation who classification
Anovulation who classification Primary amenorrhea
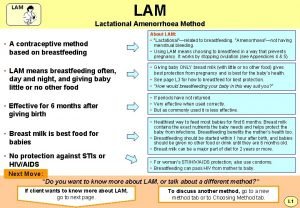
Primary amenorrhea Lactational amenorrhea
Lactational amenorrhea Lactational amenorrhea
Lactational amenorrhea What is lactational amenorrhea method
What is lactational amenorrhea method Lactational amenorrhea
Lactational amenorrhea Empty sella
Empty sella Progesterone challenge test
Progesterone challenge test Primary amenorrhea most common cause
Primary amenorrhea most common cause Amenorrhea
Amenorrhea Elmira district secondary school
Elmira district secondary school Granite sd portal
Granite sd portal