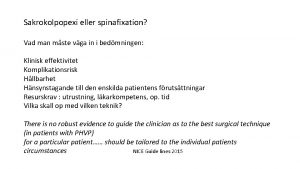
Sakrokolpopexi eller spinafixation Vad man mste vga in
- Slides: 7
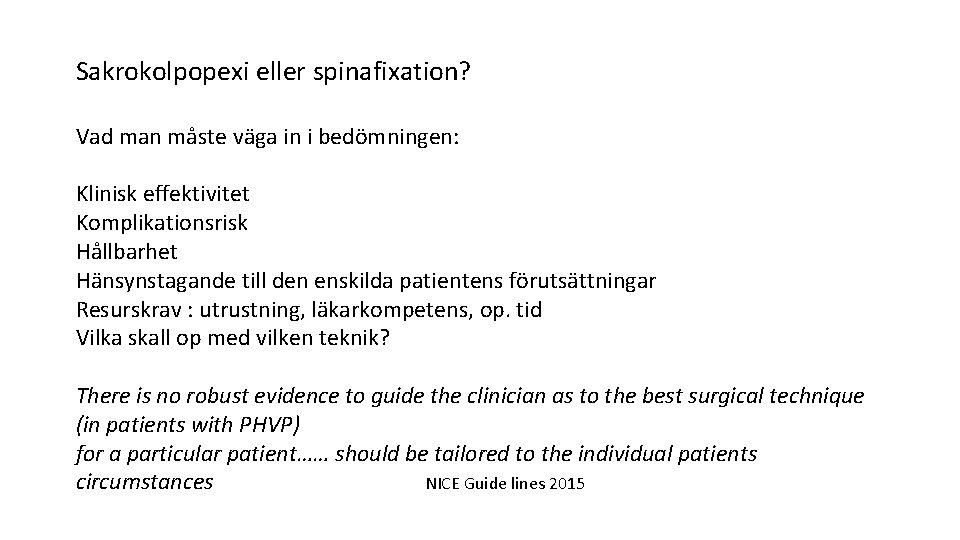
Sakrokolpopexi eller spinafixation? Vad man måste väga in i bedömningen: Klinisk effektivitet Komplikationsrisk Hållbarhet Hänsynstagande till den enskilda patientens förutsättningar Resurskrav : utrustning, läkarkompetens, op. tid Vilka skall op med vilken teknik? There is no robust evidence to guide the clinician as to the best surgical technique (in patients with PHVP) for a particular patient…… should be tailored to the individual patients circumstances NICE Guide lines 2015
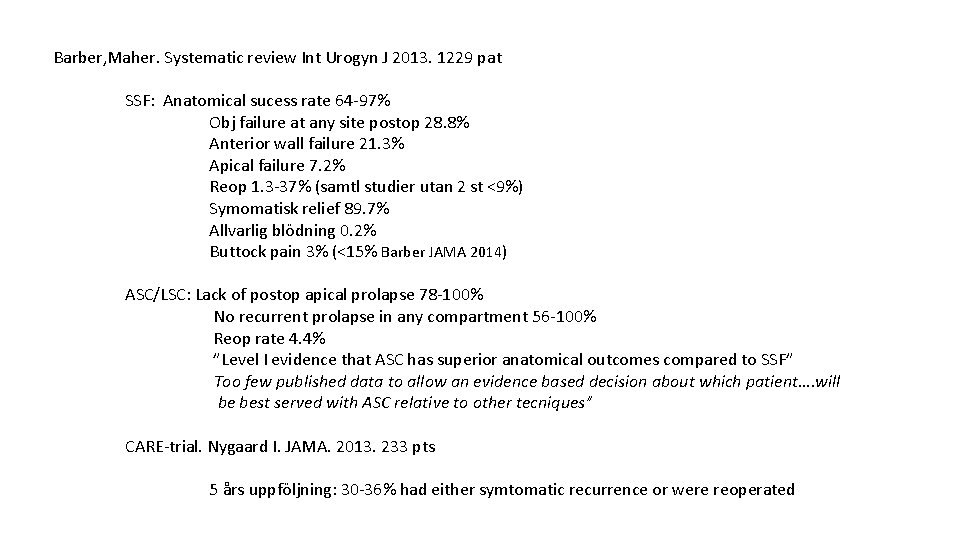
Barber, Maher. Systematic review Int Urogyn J 2013. 1229 pat SSF: Anatomical sucess rate 64 -97% Obj failure at any site postop 28. 8% Anterior wall failure 21. 3% Apical failure 7. 2% Reop 1. 3 -37% (samtl studier utan 2 st <9%) Symomatisk relief 89. 7% Allvarlig blödning 0. 2% Buttock pain 3% (<15% Barber JAMA 2014) ASC/LSC: Lack of postop apical prolapse 78 -100% No recurrent prolapse in any compartment 56 -100% Reop rate 4. 4% ”Level I evidence that ASC has superior anatomical outcomes compared to SSF” Too few published data to allow an evidence based decision about which patient…. will be best served with ASC relative to other tecniques” CARE-trial. Nygaard I. JAMA. 2013. 233 pts 5 års uppföljning: 30 -36% had either symtomatic recurrence or were reoperated
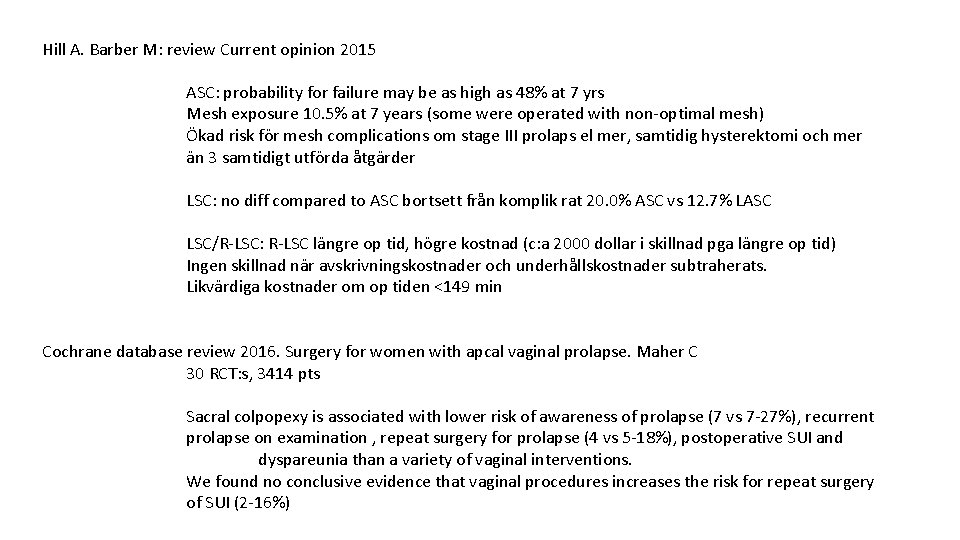
Hill A. Barber M: review Current opinion 2015 ASC: probability for failure may be as high as 48% at 7 yrs Mesh exposure 10. 5% at 7 years (some were operated with non-optimal mesh) Ökad risk för mesh complications om stage III prolaps el mer, samtidig hysterektomi och mer än 3 samtidigt utförda åtgärder LSC: no diff compared to ASC bortsett från komplik rat 20. 0% ASC vs 12. 7% LASC LSC/R-LSC: R-LSC längre op tid, högre kostnad (c: a 2000 dollar i skillnad pga längre op tid) Ingen skillnad när avskrivningskostnader och underhållskostnader subtraherats. Likvärdiga kostnader om op tiden <149 min Cochrane database review 2016. Surgery for women with apcal vaginal prolapse. Maher C 30 RCT: s, 3414 pts Sacral colpopexy is associated with lower risk of awareness of prolapse (7 vs 7 -27%), recurrent prolapse on examination , repeat surgery for prolapse (4 vs 5 -18%), postoperative SUI and dyspareunia than a variety of vaginal interventions. We found no conclusive evidence that vaginal procedures increases the risk for repeat surgery of SUI (2 -16%)
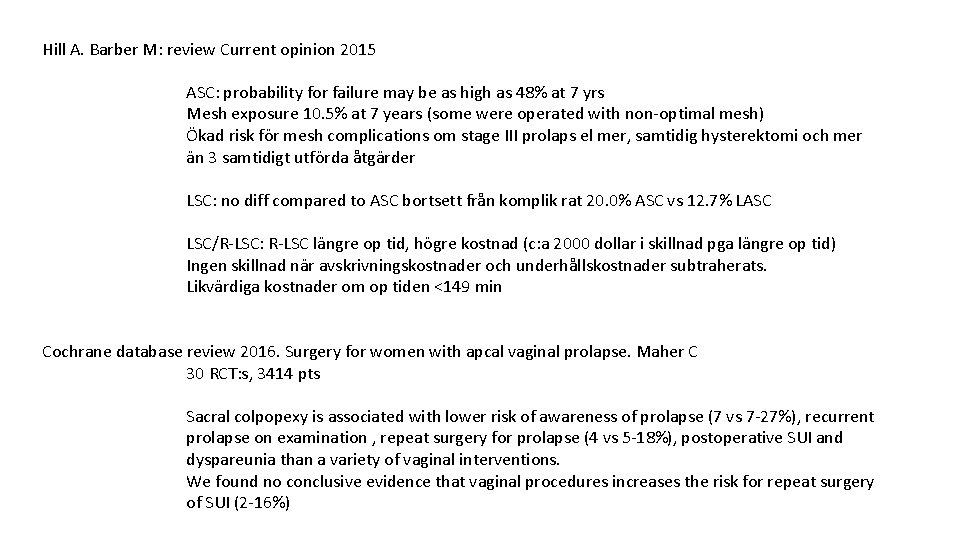
Hill A. Barber M: review Current opinion 2015 ASC: probability for failure may be as high as 48% at 7 yrs Mesh exposure 10. 5% at 7 years (some were operated with non-optimal mesh) Ökad risk för mesh complications om stage III prolaps el mer, samtidig hysterektomi och mer än 3 samtidigt utförda åtgärder LSC: no diff compared to ASC bortsett från komplik rat 20. 0% ASC vs 12. 7% LASC LSC/R-LSC: R-LSC längre op tid, högre kostnad (c: a 2000 dollar i skillnad pga längre op tid) Ingen skillnad när avskrivningskostnader och underhållskostnader subtraherats. Likvärdiga kostnader om op tiden <149 min Cochrane database review 2016. Surgery for women with apcal vaginal prolapse. Maher C 30 RCT: s, 3414 pts Sacral colpopexy is associated with lower risk of awareness of prolapse (7 vs 7 -27%), recurrent prolapse on examination , repeat surgery for prolapse (4 vs 5 -18%), postoperative SUI and dyspareunia than a variety of vaginal interventions. We found no conclusive evidence that vaginal procedures increases the risk for repeat surgery of SUI (2 -16%)
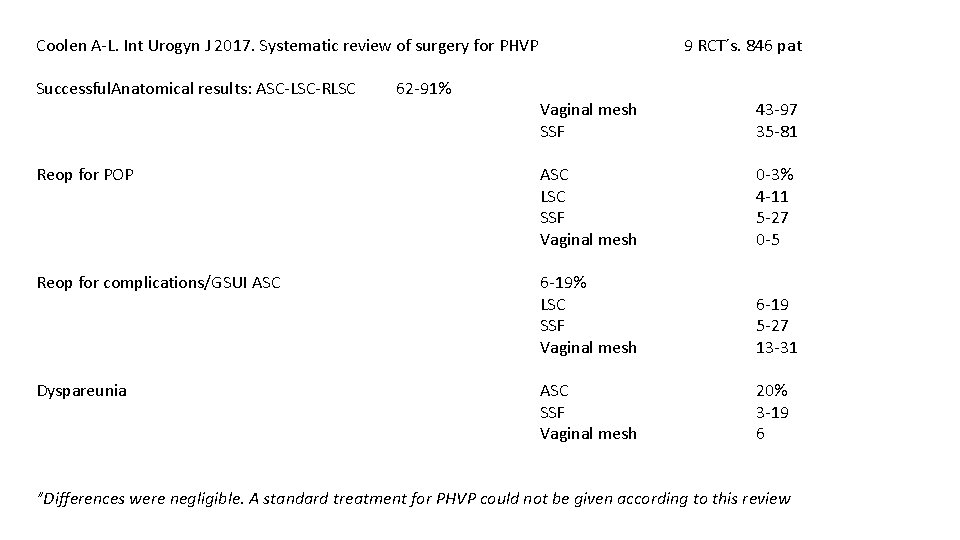
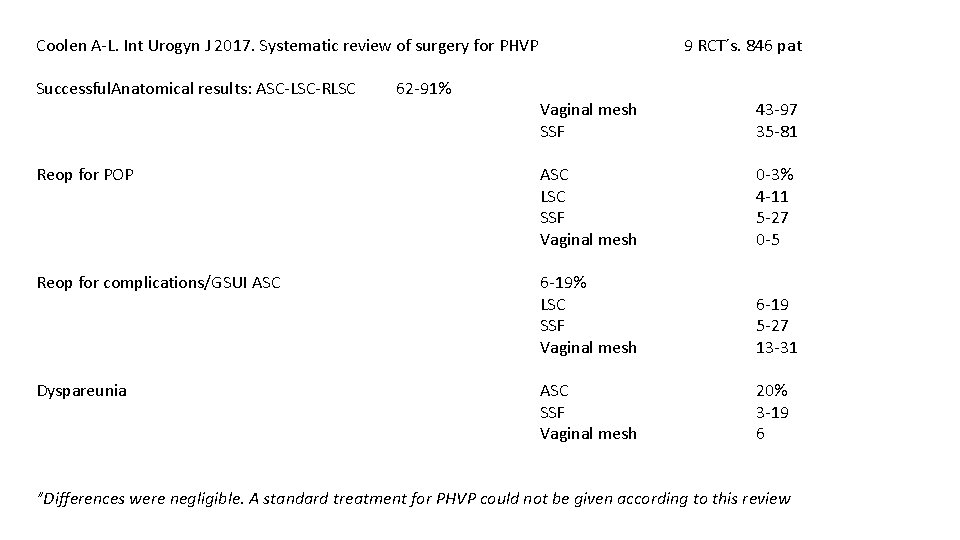
Coolen A-L. Int Urogyn J 2017. Systematic review of surgery for PHVP Successful. Anatomical results: ASC-LSC-RLSC 62 -91% 9 RCT´s. 846 pat Vaginal mesh SSF 43 -97 35 -81 Reop for POP ASC LSC SSF Vaginal mesh 0 -3% 4 -11 5 -27 0 -5 Reop for complications/GSUI ASC 6 -19% LSC SSF Vaginal mesh 6 -19 5 -27 13 -31 Dyspareunia ASC SSF Vaginal mesh 20% 3 -19 6 ”Differences were negligible. A standard treatment for PHVP could not be given according to this review
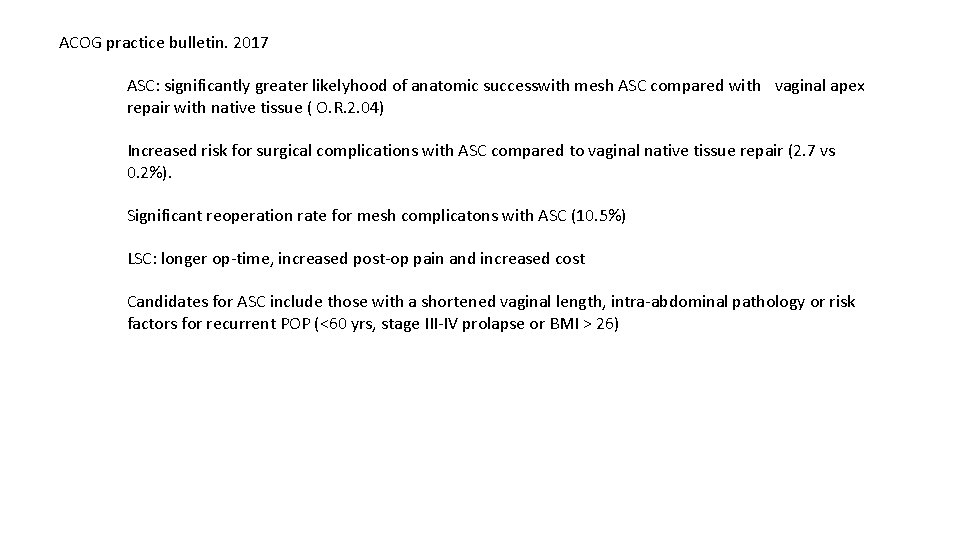
ACOG practice bulletin. 2017 ASC: significantly greater likelyhood of anatomic successwith mesh ASC compared with vaginal apex repair with native tissue ( O. R. 2. 04) Increased risk for surgical complications with ASC compared to vaginal native tissue repair (2. 7 vs 0. 2%). Significant reoperation rate for mesh complicatons with ASC (10. 5%) LSC: longer op-time, increased post-op pain and increased cost Candidates for ASC include those with a shortened vaginal length, intra-abdominal pathology or risk factors for recurrent POP (<60 yrs, stage III-IV prolapse or BMI > 26)
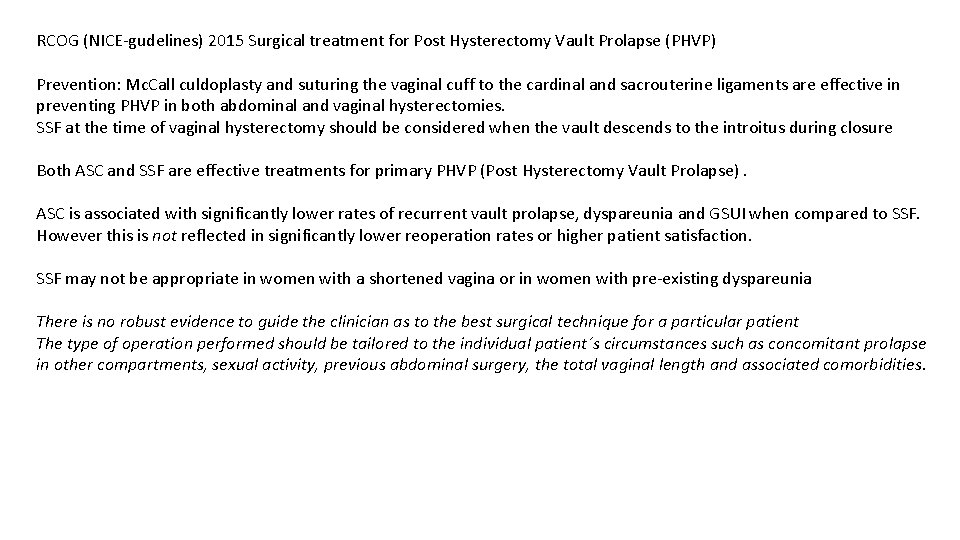
RCOG (NICE-gudelines) 2015 Surgical treatment for Post Hysterectomy Vault Prolapse (PHVP) Prevention: Mc. Call culdoplasty and suturing the vaginal cuff to the cardinal and sacrouterine ligaments are effective in preventing PHVP in both abdominal and vaginal hysterectomies. SSF at the time of vaginal hysterectomy should be considered when the vault descends to the introitus during closure Both ASC and SSF are effective treatments for primary PHVP (Post Hysterectomy Vault Prolapse). ASC is associated with significantly lower rates of recurrent vault prolapse, dyspareunia and GSUI when compared to SSF. However this is not reflected in significantly lower reoperation rates or higher patient satisfaction. SSF may not be appropriate in women with a shortened vagina or in women with pre-existing dyspareunia There is no robust evidence to guide the clinician as to the best surgical technique for a particular patient The type of operation performed should be tailored to the individual patient´s circumstances such as concomitant prolapse in other compartments, sexual activity, previous abdominal surgery, the total vaginal length and associated comorbidities.