Risks of Psychotropics Clinical Toxicology Pharmacology Newcastle Mater
![TCAs: Pharmacokinetic Interactions Elevated [TCAs] Lower [TCAs] Elevated [Interacting Drugs] Cimetidine Ethanal acute ingestion TCAs: Pharmacokinetic Interactions Elevated [TCAs] Lower [TCAs] Elevated [Interacting Drugs] Cimetidine Ethanal acute ingestion](https://slidetodoc.com/presentation_image_h/37899eeb20d518b164da304b0c2faa82/image-4.jpg)

- Slides: 32
Risks of Psychotropics Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 1
The Risks N N N Antidepressants Antipsychotics Adverse Effects Toxicity Significant Interactions Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 2
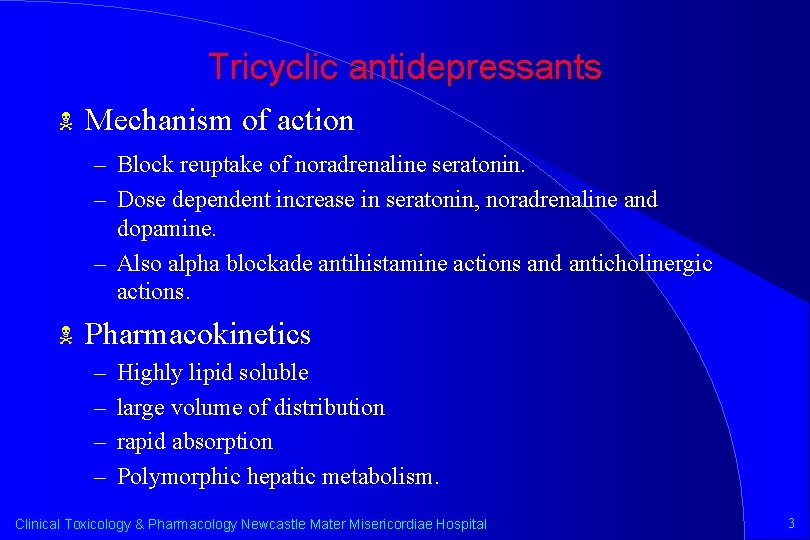
Tricyclic antidepressants N Mechanism of action – Block reuptake of noradrenaline seratonin. – Dose dependent increase in seratonin, noradrenaline and dopamine. – Also alpha blockade antihistamine actions and anticholinergic actions. N Pharmacokinetics – – Highly lipid soluble large volume of distribution rapid absorption Polymorphic hepatic metabolism. Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 3
![TCAs Pharmacokinetic Interactions Elevated TCAs Lower TCAs Elevated Interacting Drugs Cimetidine Ethanal acute ingestion TCAs: Pharmacokinetic Interactions Elevated [TCAs] Lower [TCAs] Elevated [Interacting Drugs] Cimetidine Ethanal acute ingestion](https://slidetodoc.com/presentation_image_h/37899eeb20d518b164da304b0c2faa82/image-4.jpg)
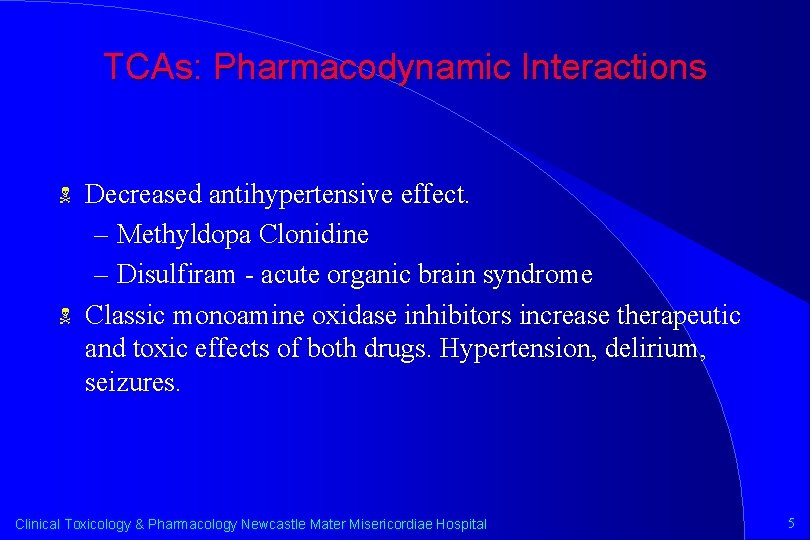
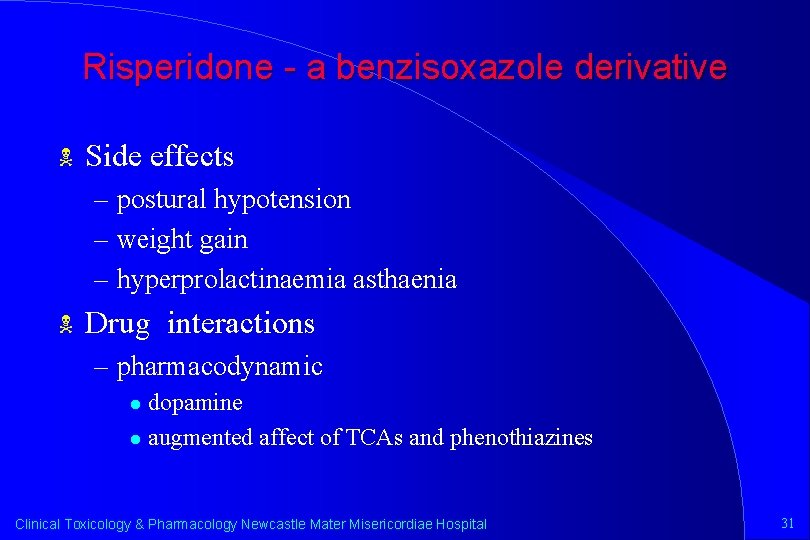
TCAs: Pharmacokinetic Interactions Elevated [TCAs] Lower [TCAs] Elevated [Interacting Drugs] Cimetidine Ethanal acute ingestion Haloperidol Phenothiazine Propoxyphene Fluoxetine Chronic ethanol Barbiturates Carbamazepine Phenytoin Warfarin Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 4
TCAs: Pharmacodynamic Interactions N N Decreased antihypertensive effect. – Methyldopa Clonidine – Disulfiram - acute organic brain syndrome Classic monoamine oxidase inhibitors increase therapeutic and toxic effects of both drugs. Hypertension, delirium, seizures. Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 5
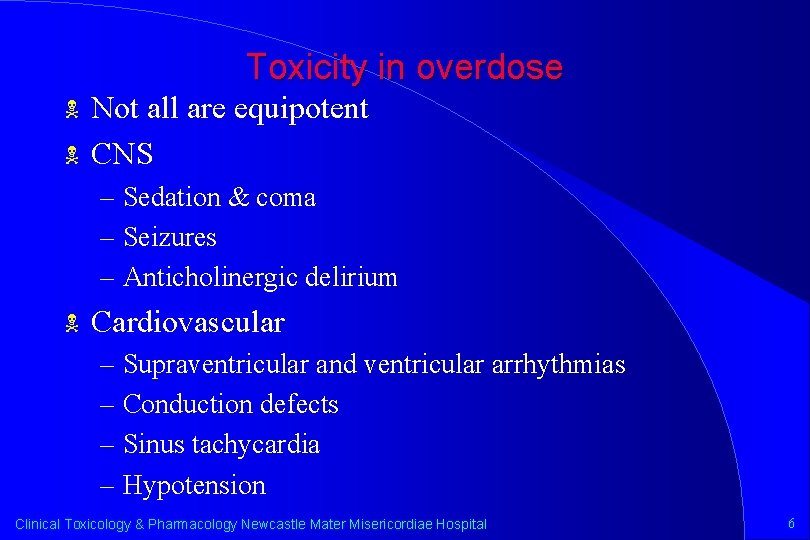
Toxicity in overdose N N Not all are equipotent CNS – Sedation & coma – Seizures – Anticholinergic delirium N Cardiovascular – Supraventricular and ventricular arrhythmias – Conduction defects – Sinus tachycardia – Hypotension Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 6
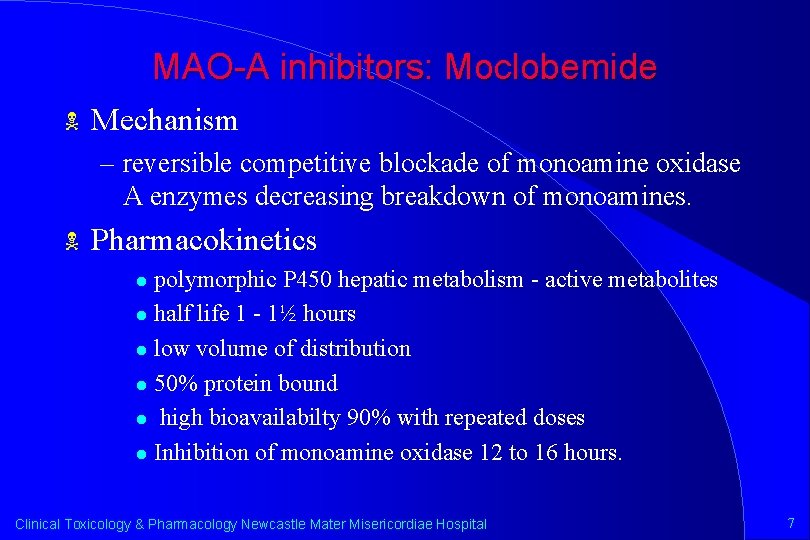
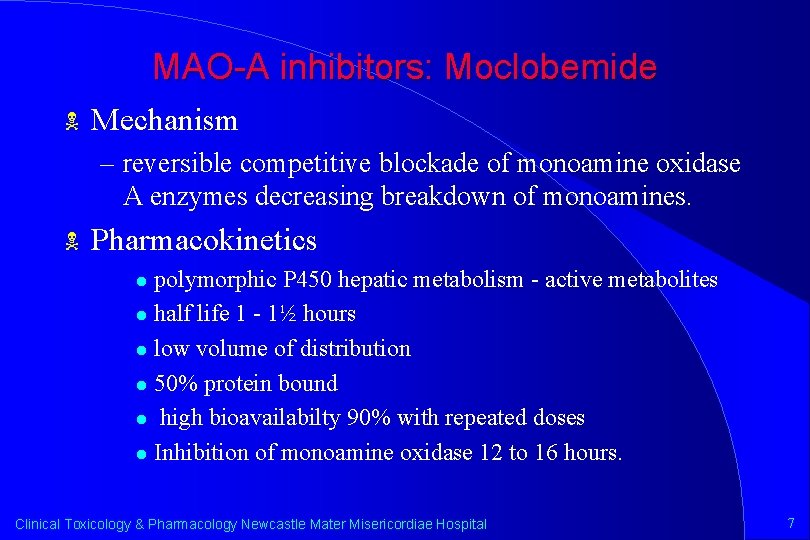
MAO-A inhibitors: Moclobemide N Mechanism – reversible competitive blockade of monoamine oxidase A enzymes decreasing breakdown of monoamines. N Pharmacokinetics polymorphic P 450 hepatic metabolism - active metabolites l half life 1 - 1½ hours l low volume of distribution l 50% protein bound l high bioavailabilty 90% with repeated doses l Inhibition of monoamine oxidase 12 to 16 hours. l Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 7
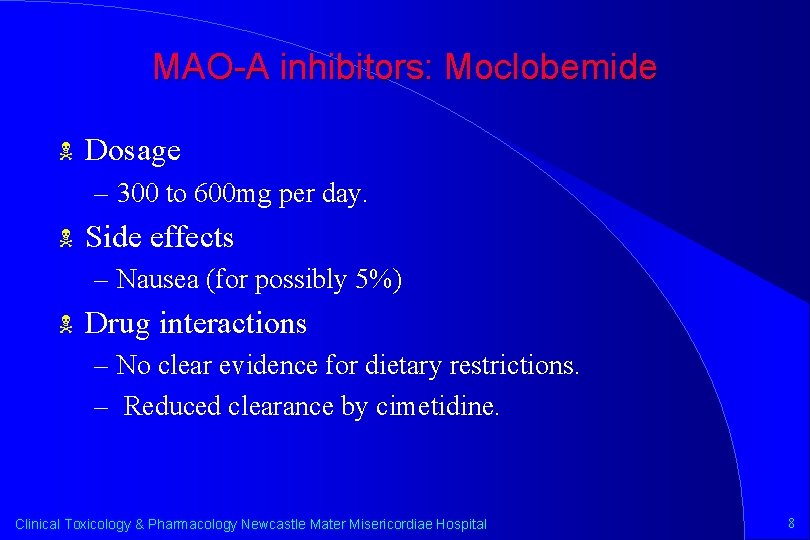
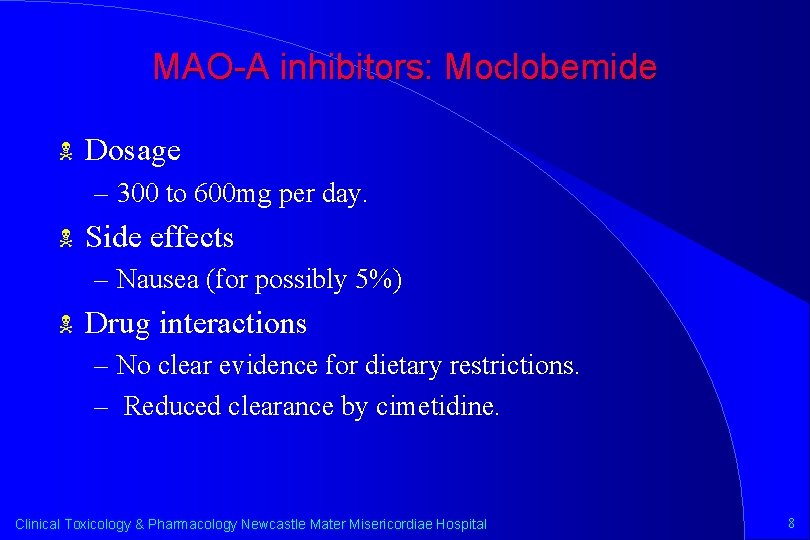
MAO-A inhibitors: Moclobemide N Dosage – 300 to 600 mg per day. N Side effects – Nausea (for possibly 5%) N Drug interactions – No clear evidence for dietary restrictions. – Reduced clearance by cimetidine. Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 8
MAO-A inhibitors: Moclobemide N Toxicity – Minimal toxicity in overdose – CNS depression and confusion, nausea, hyperreflexia, hypotension and occasional hyperthermia. Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 9
Fluoxetine N Mechanism – Inhibition of presynaptic seratonin reuptake plus probably altering sensitivity to serotonin. Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 10
Fluoxetine N Pharmacokinetics – High bioavailability and volume of distribution – High protein binding. – P 450 hepatic metabolism, less than 5% renal metabolism. – Half life of fluoxetine approximately 70 hours. – Half life of active metabolite desmethylfluoxetine 330 hours, therefore steady state concentrations take 2 to 4 weeks. Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 11
Fluoxetine N Efficacy – In moderate depression similar to tricyclic antidepressants – some analgesic and anorectic effects, no sedative effects or alpha effects. N N Not proarrhythmic. No evidence of psychomotor changes subjectively or objectively Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 12
Fluoxetine N Side effects – Approximately 20% of patients experience nervousness, insomnia or nausea. Treatment failure due to side effects approximately 5%. N Drug interaction – Kinetic: Increased concentration of TCA, carbamazepine, haloperidol, metoprolol & terfenadine N Toxicity – Minimal cardiotoxicity, ataxia, CNS depression, occasional seizures. Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 13
Antipsychotics: Phenothiazines and butyrophenones N Mechanism – Antipsychotic effect probably due to dopamine blockade. – Dirty drugs with alpha effects, antihistamine effects, anticholinergic effects (except haloperidol) direct membrane stabilising effects. Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 14
Antipsychotics: Phenothiazines and butyrophenones N Metabolism – Predominantly Polymorphic hepatic P 450 enzyme metabolism. – Conjugation – High volume of distribution, long half life Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 15
Antipsychotics: Phenothiazines and butyrophenones N Side effects – Similar to those of tricyclic antidepressants – Attributed to dopamine blockade Parkinsonian states l Tardive dyskinesia l Neuroleptic malignant syndrome l Acute dystonia (early) l Akathesia l Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 16
Antipsychotics: Phenothiazines and butyrophenones – Lowered seizure threshold – Hypersensitivity reactions – Hyperpigmentation – Retinal toxicity (especially thioridazine >800 mg/day) – Lowered seizure threshold for phenothiazines – Endocrine Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 17
Antipsychotics: Phenothiazines and butyrophenones N Drug interactions – Enzyme inducers some self induction. – Heavy smoking may decrease levels. – Antipsychotics may inhibit antidepressant metabolism. – Inhibits phenytoin metabolism. Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 18
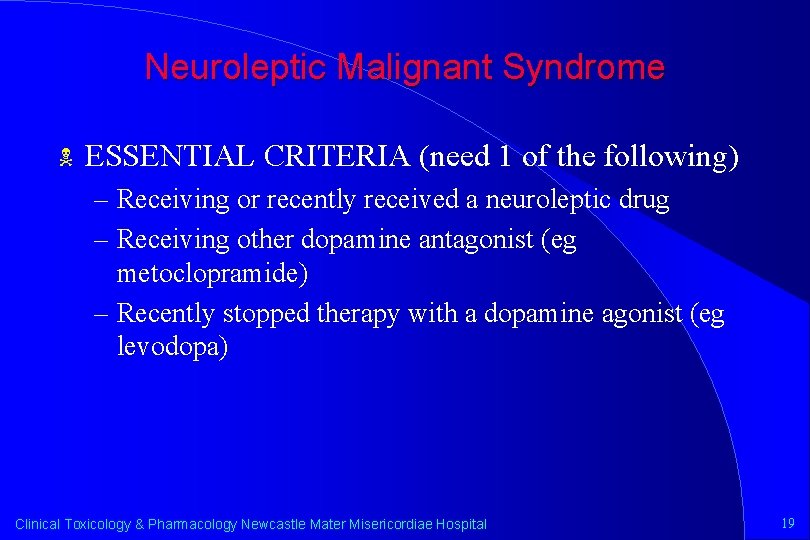
Neuroleptic Malignant Syndrome N ESSENTIAL CRITERIA (need 1 of the following) – Receiving or recently received a neuroleptic drug – Receiving other dopamine antagonist (eg metoclopramide) – Recently stopped therapy with a dopamine agonist (eg levodopa) Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 19
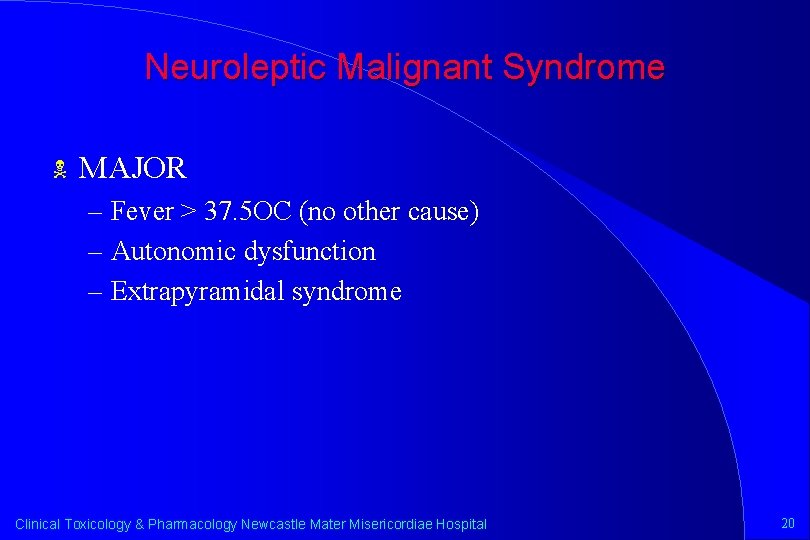
Neuroleptic Malignant Syndrome N MAJOR – Fever > 37. 5 OC (no other cause) – Autonomic dysfunction – Extrapyramidal syndrome Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 20
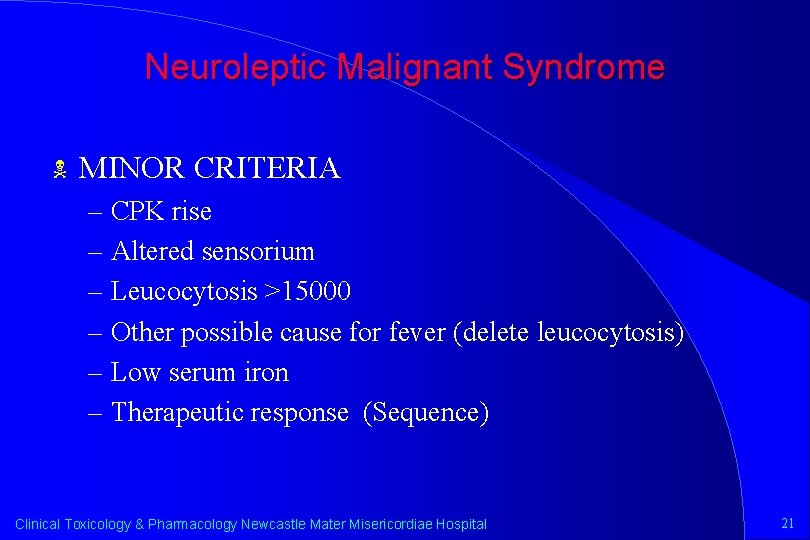
Neuroleptic Malignant Syndrome N MINOR CRITERIA – CPK rise – Altered sensorium – Leucocytosis >15000 – Other possible cause for fever (delete leucocytosis) – Low serum iron – Therapeutic response (Sequence) Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 21
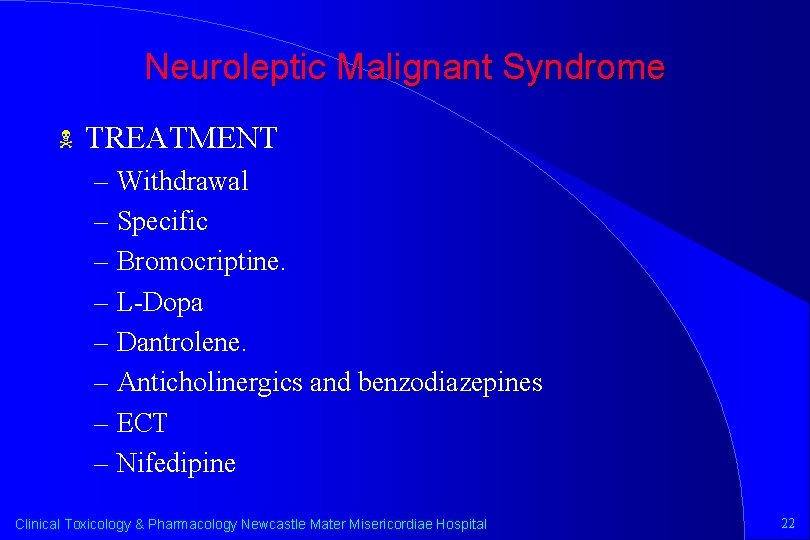
Neuroleptic Malignant Syndrome N TREATMENT – Withdrawal – Specific – Bromocriptine. – L-Dopa – Dantrolene. – Anticholinergics and benzodiazepines – ECT – Nifedipine Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 22
Neuroleptic Malignant Syndrome N Recommencement of Neuroleptics. – with caution after complete recovery from NMS Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 23
Clozapine – A Diebenzodizepine Antipsychotic – A Low Affinity Dopamine Antagonist – A High Affinity Serotonin Antagonist N Indications – Treatment Resistant Schizophrenia Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 24
Clozapine N Pharmacokinetics – Bioavailability 50% – Protein Binding 95% – Half Life 12 Hours – Hepatic Metabolism Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 25
Clozapine N Adverse Effects – Neuroleptic Malignanct Syndrome – Seizures 5% of Patients > 600 Mg a Day – Hypersalivation – Agranulocytosis 0. 8% In One Year (95% in First Six Months) l Increased Risk in the Elderly and Female l Increased Risk in Ashkenazi Jews l Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 26
Clozapine N Drug Interactions – Enhance Sedation With Other Sedatives – Metabolism Inhibited by Cimetidine Leading to Clozapine Toxicity – Clozapine Metabolism Induced by Phenytoin Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 27
Clozapine N Overdose – Delirium, Coma, Seizures – Tachycardia, Hypotension – Respiratory Depression – Hypersalivation Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 28

Risperidone - a benzisoxazole derivative N Indications – schizophrenia Negative symptoms l Movement disorders on conventional therapy l N Mechanism – Low affinity D 2 antagonism – High affinity 5 H 2 antagonism – Some alpha 1 and antihistamine effect Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 29
Risperidone - a benzisoxazole derivative N Pharmacokinetics – rapid absorption and high bioavailability – risperidone metabolised to 9 hydroxy resperidone – P 450 to D 6 half life of risperidone (fast acetylators 2 -4 hours) – Half life hydroxyrisperidone (fast acetylators 27 hours) – Protein binding (albumin and alpha glycoprotein) l risperidone 88%, 9 hydroxyrisperidone 77% Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 30
Risperidone - a benzisoxazole derivative N Side effects – postural hypotension – weight gain – hyperprolactinaemia asthaenia N Drug interactions – pharmacodynamic dopamine l augmented affect of TCAs and phenothiazines l Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 31
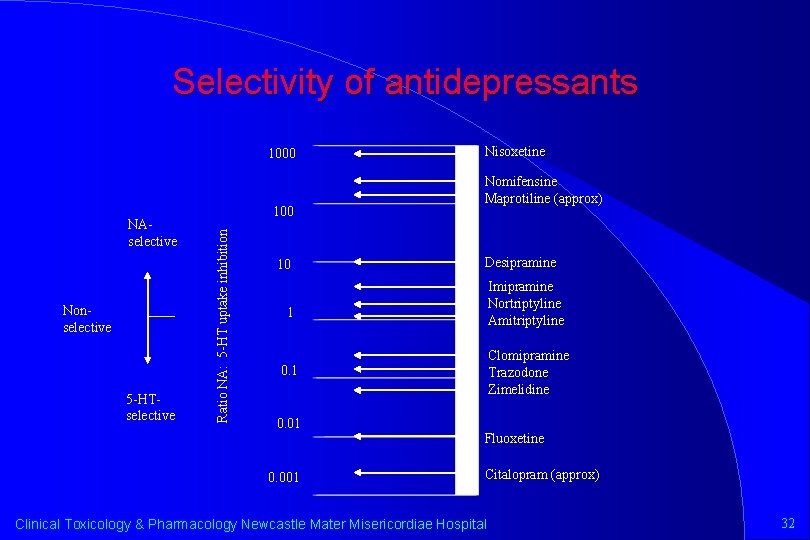
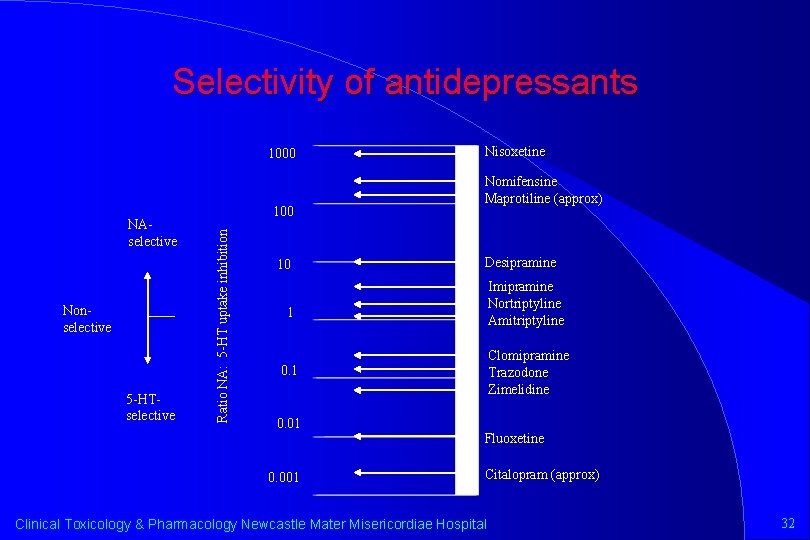
Selectivity of antidepressants 1000 Nonselective 5 -HTselective 100 Ratio NA: 5 -HT uptake inhibition NAselective 10 Nisoxetine Nomifensine Maprotiline (approx) Desipramine Imipramine Nortriptyline Amitriptyline 1 Clomipramine Trazodone Zimelidine 0. 1 0. 001 Fluoxetine Citalopram (approx) Clinical Toxicology & Pharmacology Newcastle Mater Misericordiae Hospital 32
 Psychotropics
Psychotropics Toxicology and applied pharmacology
Toxicology and applied pharmacology Annual review of pharmacology and toxicology
Annual review of pharmacology and toxicology Pharmacology newcastle
Pharmacology newcastle Maria mater gratiae mater misericordiae
Maria mater gratiae mater misericordiae Clinical pharmacology
Clinical pharmacology Clinical pharmacology residency
Clinical pharmacology residency Basic & clinical pharmacology
Basic & clinical pharmacology Clinical pharmacology seminar
Clinical pharmacology seminar Dopamine synthesis
Dopamine synthesis Clinical pharmacology seminar
Clinical pharmacology seminar Clinical pharmacology powered by clinicalkey
Clinical pharmacology powered by clinicalkey Basic & clinical pharmacology
Basic & clinical pharmacology Receptors in pharmacology
Receptors in pharmacology What is ion trapping in pharmacology
What is ion trapping in pharmacology Fish pharmacology
Fish pharmacology Venipuncture for radiologic technologists
Venipuncture for radiologic technologists Reverse pharmacology
Reverse pharmacology Parkinson's disease definition
Parkinson's disease definition Pharmacology pay
Pharmacology pay Pharmacology introduction
Pharmacology introduction Basic principles of pharmacology
Basic principles of pharmacology Focus on pharmacology essentials for health professionals
Focus on pharmacology essentials for health professionals What is pharmacology
What is pharmacology Guaifenasin
Guaifenasin Tachyphylaxis in pharmacology
Tachyphylaxis in pharmacology Pharmacology tutor anderson
Pharmacology tutor anderson Pharmacology module
Pharmacology module First pass effect in pharmacology
First pass effect in pharmacology Metabolism definition in pharmacology
Metabolism definition in pharmacology Pharmacology definition
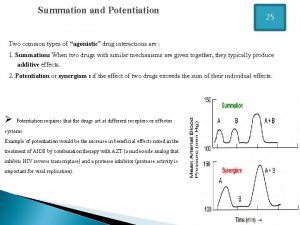
Pharmacology definition Potentiation example
Potentiation example Glomerular
Glomerular