Psychotropic Drugs What are psychotropic drugs Psychotropics are






- Slides: 32
Psychotropic Drugs
What are psychotropic drugs? • Psychotropics: are drugs which modify the • behavioral pattern of psychiatric patients. They do not eliminate the disease but prepare the patients to psychotherapy. Psychotropics are classified into: 1. Psychotropic stimulants (mood elevators): – Antidepressants. 2. Psychotropic depressants (mood stabilizers): – Antipsychotics. – Antianxiety drugs.
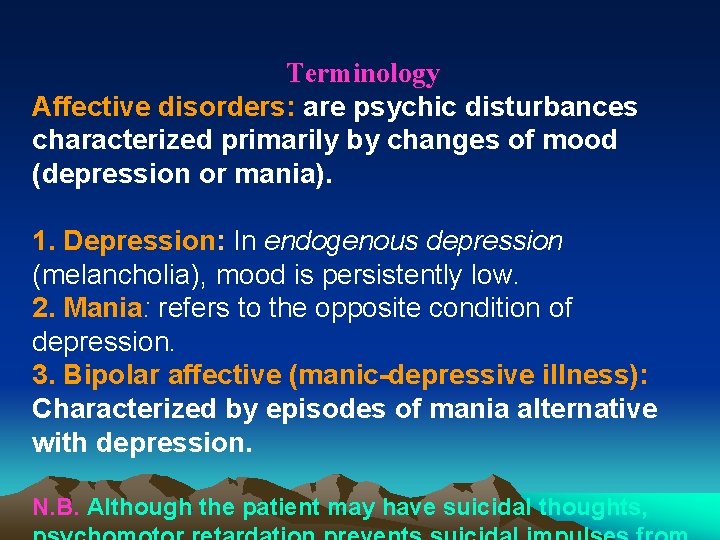
Terminology Affective disorders: are psychic disturbances characterized primarily by changes of mood (depression or mania). 1. Depression: In endogenous depression (melancholia), mood is persistently low. 2. Mania: refers to the opposite condition of depression. 3. Bipolar affective (manic-depressive illness): Characterized by episodes of mania alternative with depression. N. B. Although the patient may have suicidal thoughts,

I- DRUGS USED IN AFFECTIVE DISORDERS: 1. ANTIDEPRESSANTS 2. MOOD STABILISERS
1. ANTIDEPRESSANTS: Drugs used in the treatment of depression
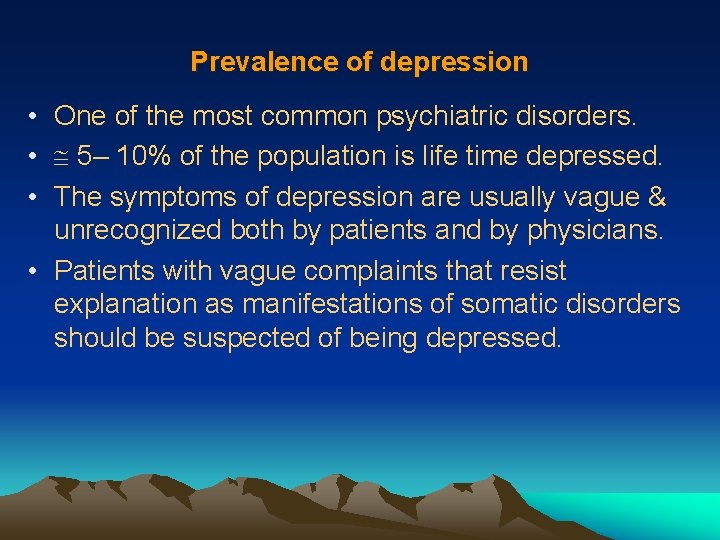
Prevalence of depression • One of the most common psychiatric disorders. • 5– 10% of the population is life time depressed. • The symptoms of depression are usually vague & unrecognized both by patients and by physicians. • Patients with vague complaints that resist explanation as manifestations of somatic disorders should be suspected of being depressed.
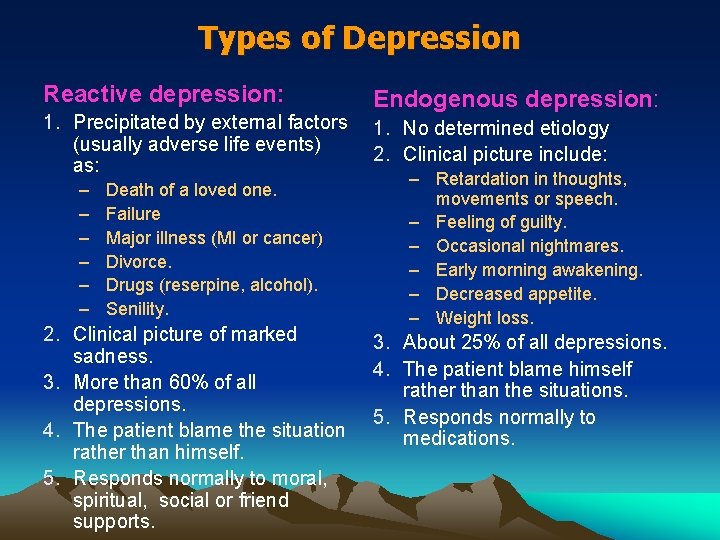
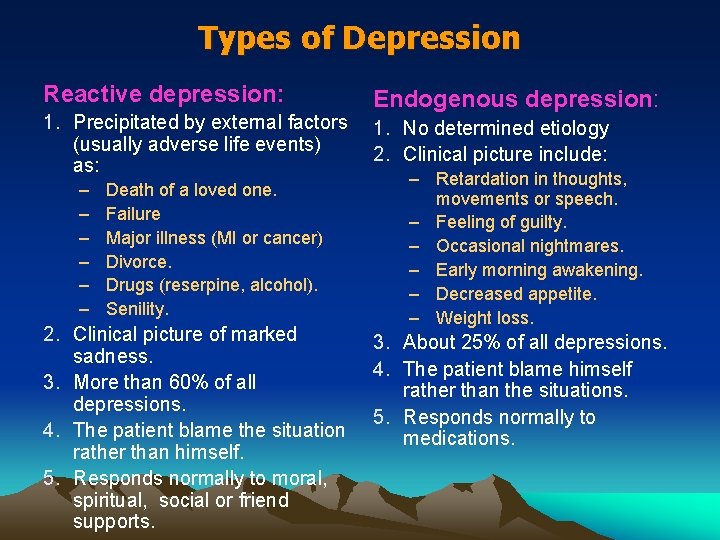
Types of Depression Reactive depression: 1. Precipitated by external factors (usually adverse life events) as: – – – Death of a loved one. Failure Major illness (MI or cancer) Divorce. Drugs (reserpine, alcohol). Senility. 2. Clinical picture of marked sadness. 3. More than 60% of all depressions. 4. The patient blame the situation rather than himself. 5. Responds normally to moral, spiritual, social or friend supports. Endogenous depression: 1. No determined etiology 2. Clinical picture include: – Retardation in thoughts, movements or speech. – Feeling of guilty. – Occasional nightmares. – Early morning awakening. – Decreased appetite. – Weight loss. 3. About 25% of all depressions. 4. The patient blame himself rather than the situations. 5. Responds normally to medications.

Symptoms of depression Emotional symptoms: – Misery & apathy. – Feelings of guilt & inadequacy. – Loss of motivation. Biological symptoms: – Retardation of thought and movements. – Sleep disturbances and loss of appetite.
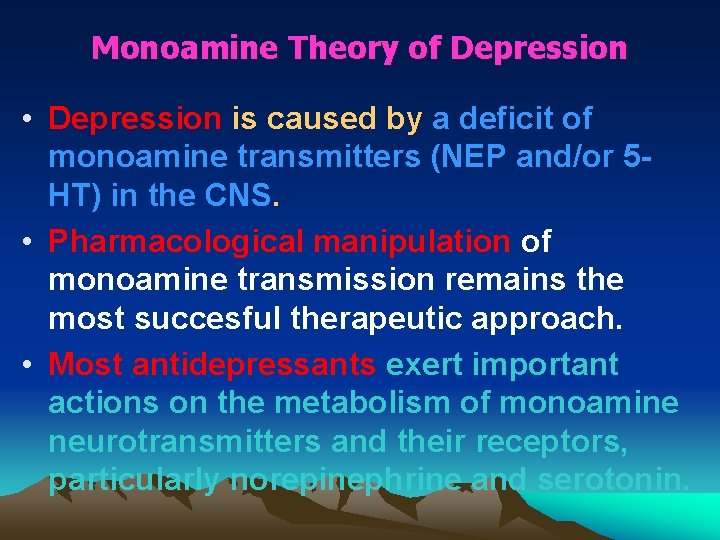
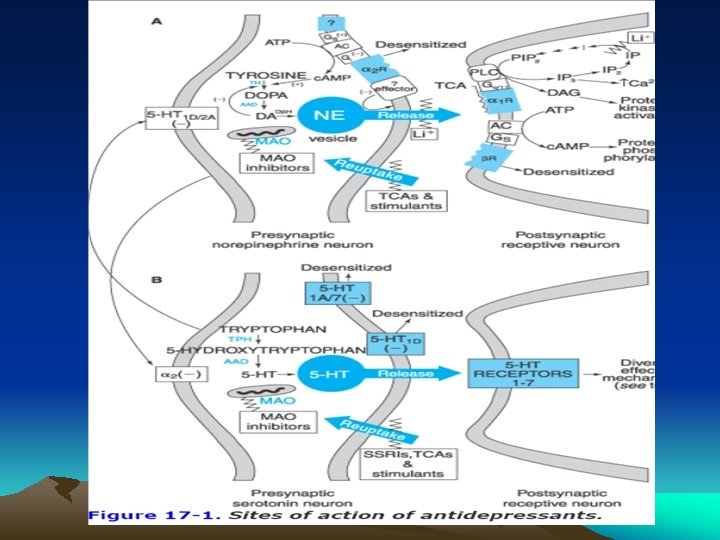
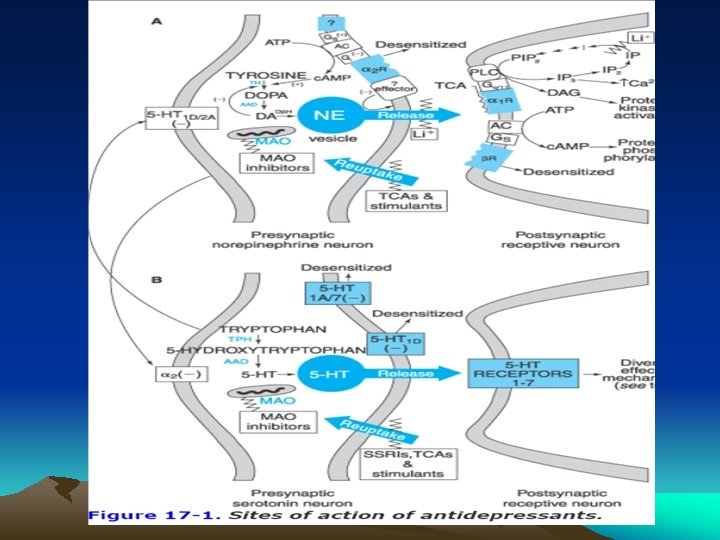
Monoamine Theory of Depression • Depression is caused by a deficit of monoamine transmitters (NEP and/or 5 HT) in the CNS. • Pharmacological manipulation of monoamine transmission remains the most succesful therapeutic approach. • Most antidepressants exert important actions on the metabolism of monoamine neurotransmitters and their receptors, particularly norepinephrine and serotonin.
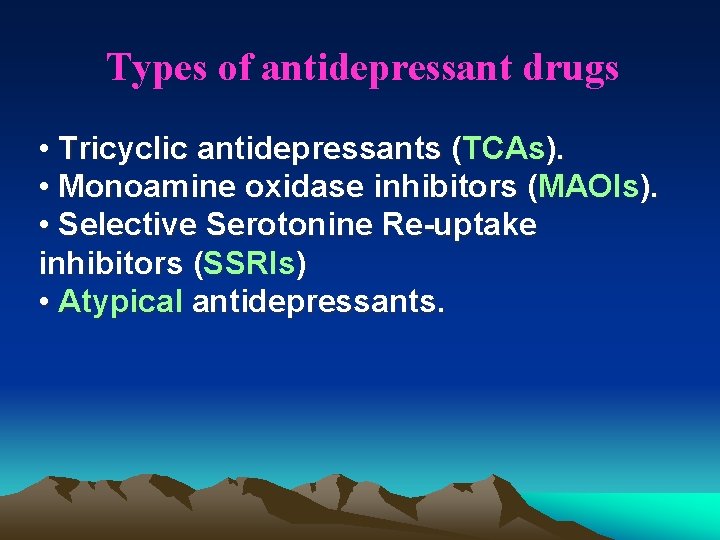
Types of antidepressant drugs • Tricyclic antidepressants (TCAs). • Monoamine oxidase inhibitors (MAOIs). • Selective Serotonine Re-uptake inhibitors (SSRIs) • Atypical antidepressants.
1. Tricyclic Antidepressants (TCAs) Members: Tertiary Amine: Imipramine, Clomipramine, Amitriptyline, Doxepin and Trimipramine. Secondary Amine: Desipramine, nortriptyline, Maprotiline and Amoxapine. N. B. • Most widely used group for the TTT of depression. • All have a three-ring molecular core. So, named “tricyclic antidepressants“. • Most share norepinephrine-reuptake inhibition.
Mechanism of action • TCAs act by inhibiting reuptake of NEP and 5 -HT by the nerve terminals facilitating monoamine transmission in CNS. • The tricyclic antidepressants do not block dopamine transport, thereby differing from CNS stimulants, including cocaine, methylphenidate and amphetamines.
Pharmacological Actions of TCAs 1. CNS: CNS – When given to depressed patients mood elevation within 2 -3 weeks. – The lag period in onset might be due to: • • The side effects which limit the rapid increase in dose and. Possibility of other mechanism of action involving desensitization of autoinhibitory receptors (more acceptable mechanism). – When given to normal subjects anticholinergic side effects, sleepiness & light headedness.
Cont. actions of TCAs 2. Anticholinergic actions: actions both central and peripheral side effects. 3. CVS: – Orthostatic hypotension: due to -blocking effect of TCAs. – Antiarrhythmic properties: with therapeutic doses. – Arrhythmogenic activities: with toxic doses.
Pharmacokinetics • Rapid absorption from the GIT. • Bind strongly to plasma albumin, most being 90 -95% bound at therapeutic plasma concentrations. • Metabolised in liver by two main routes: 1. N-demethylation and ring hydroxylation both metabolites retain biological activity. 2. Inactivation by glucuronide conjugation of the hydroxylated metabolites. • Metabolic pathways undergo genetic polymorphism in metabolism mainly due to CYP 450 2 D 6

rapidly demethylated imipramine desipramine amitriptyline nortriptyline the corresponding secondary amines are themselves active and may be administered in their own right
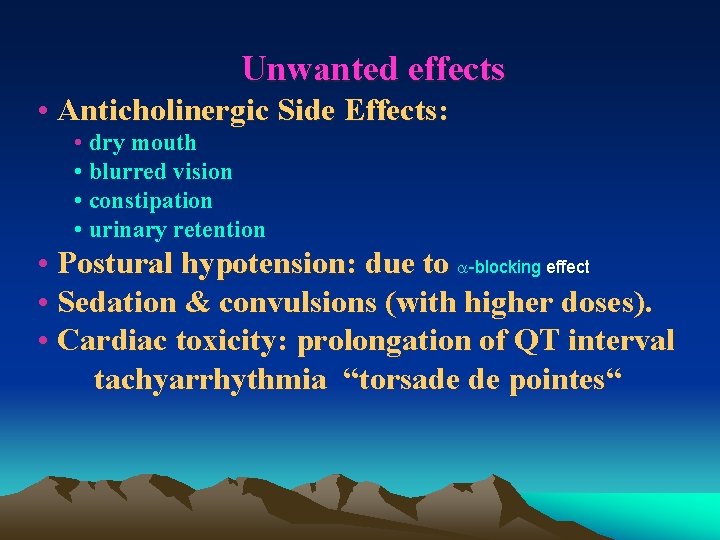
Unwanted effects • Anticholinergic Side Effects: • dry mouth • blurred vision • constipation • urinary retention • Postural hypotension: due to -blocking effect • Sedation & convulsions (with higher doses). • Cardiac toxicity: prolongation of QT interval tachyarrhythmia “torsade de pointes“
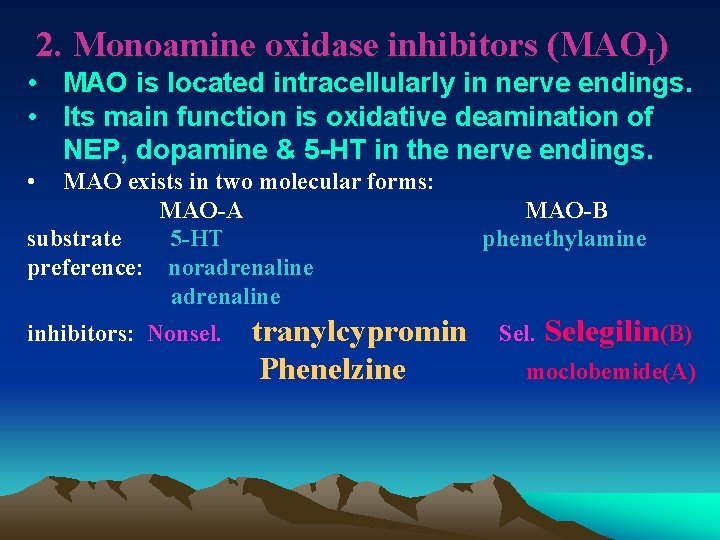
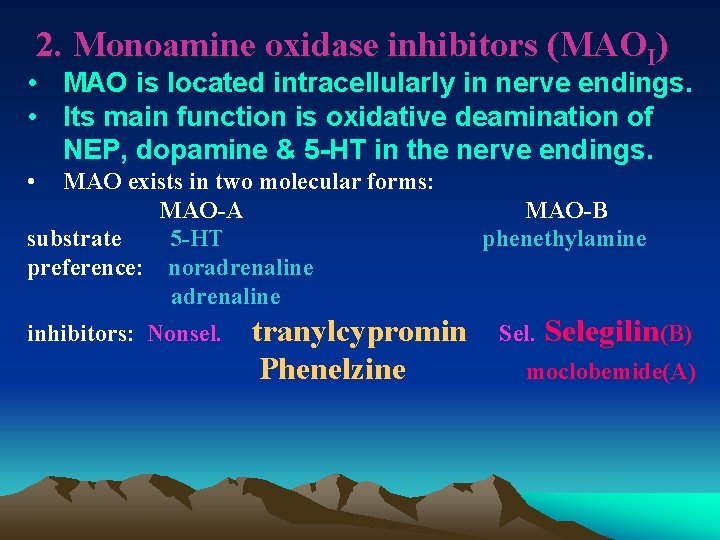
2. Monoamine oxidase inhibitors (MAOI) • MAO is located intracellularly in nerve endings. • Its main function is oxidative deamination of NEP, dopamine & 5 -HT in the nerve endings. • MAO exists in two molecular forms: MAO-A substrate 5 -HT preference: noradrenaline inhibitors: Nonsel. tranylcypromin Phenelzine MAO-B phenethylamine Selegilin(B) moclobemide(A)
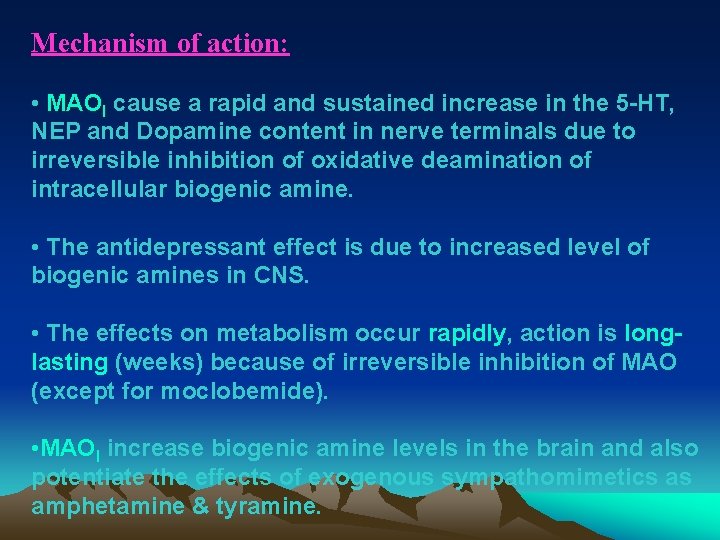
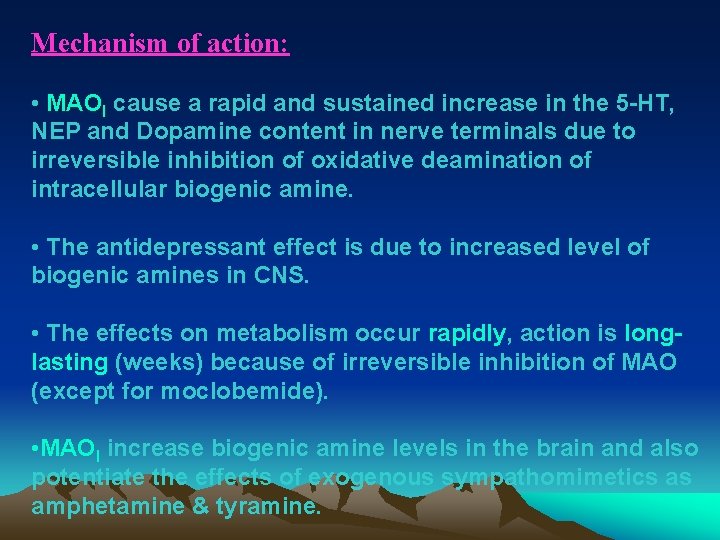
Mechanism of action: • MAOI cause a rapid and sustained increase in the 5 -HT, NEP and Dopamine content in nerve terminals due to irreversible inhibition of oxidative deamination of intracellular biogenic amine. • The antidepressant effect is due to increased level of biogenic amines in CNS. • The effects on metabolism occur rapidly, action is longlasting (weeks) because of irreversible inhibition of MAO (except for moclobemide). • MAOI increase biogenic amine levels in the brain and also potentiate the effects of exogenous sympathomimetics as amphetamine & tyramine.
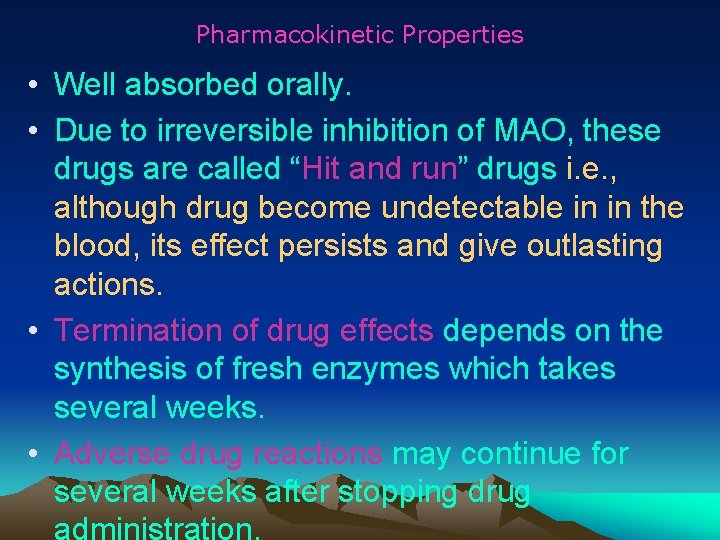
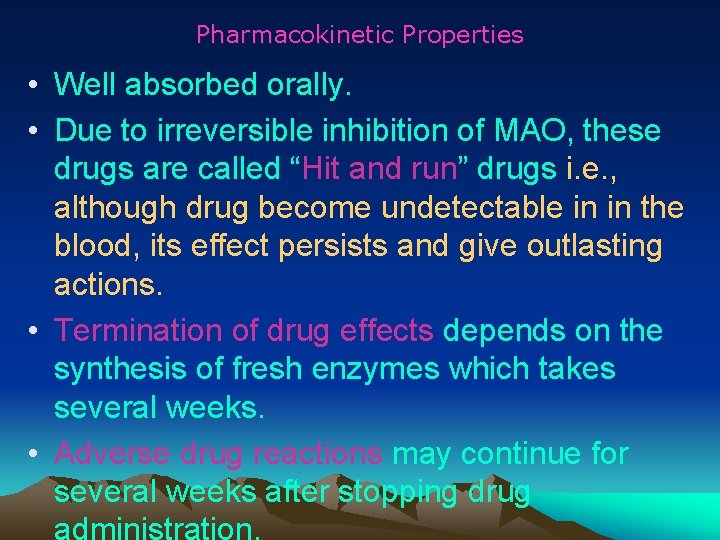
Pharmacokinetic Properties • Well absorbed orally. • Due to irreversible inhibition of MAO, these drugs are called “Hit and run” drugs i. e. , although drug become undetectable in in the blood, its effect persists and give outlasting actions. • Termination of drug effects depends on the synthesis of fresh enzymes which takes several weeks. • Adverse drug reactions may continue for several weeks after stopping drug

Unwanted effects 1. Postural Hypotension: One possible explanation for this effect - opposite of what might have been expected - is that amines such dopamine are able to accumulate within peripheral nerve terminals and displace NORA from the storage vesicles, thus reducing NORA release associated with sympathetic activity. 2. Tremors, excitement, insomnia (even convulsions in overdose): due to excessive central stimulation. 3. Antimuscarinic toxicity: dry mouth, blurred vision. 4. Hepatotoxicity & hepatocellular damage: (rarely). 5. Weight gain & inhibition of ejaculation. .
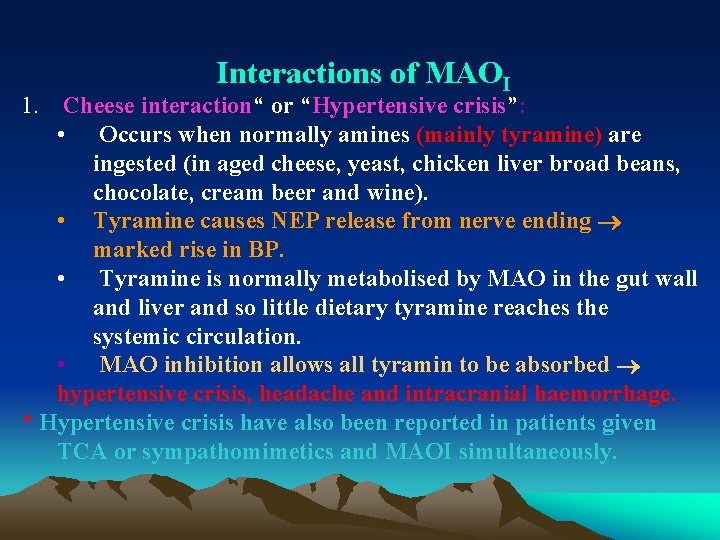
Interactions of MAOI 1. Cheese interaction“ or “Hypertensive crisis”: • Occurs when normally amines (mainly tyramine) are ingested (in aged cheese, yeast, chicken liver broad beans, chocolate, cream beer and wine). • Tyramine causes NEP release from nerve ending marked rise in BP. • Tyramine is normally metabolised by MAO in the gut wall and liver and so little dietary tyramine reaches the systemic circulation. • MAO inhibition allows all tyramin to be absorbed hypertensive crisis, headache and intracranial haemorrhage. * Hypertensive crisis have also been reported in patients given TCA or sympathomimetics and MAOI simultaneously.
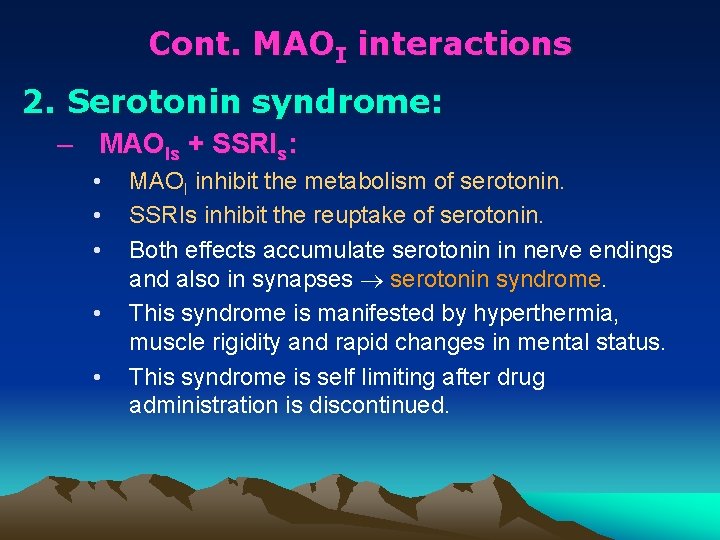
Cont. MAOI interactions 2. Serotonin syndrome: – MAOIs + SSRIs: • • • MAOI inhibit the metabolism of serotonin. SSRIs inhibit the reuptake of serotonin. Both effects accumulate serotonin in nerve endings and also in synapses serotonin syndrome. This syndrome is manifested by hyperthermia, muscle rigidity and rapid changes in mental status. This syndrome is self limiting after drug administration is discontinued.
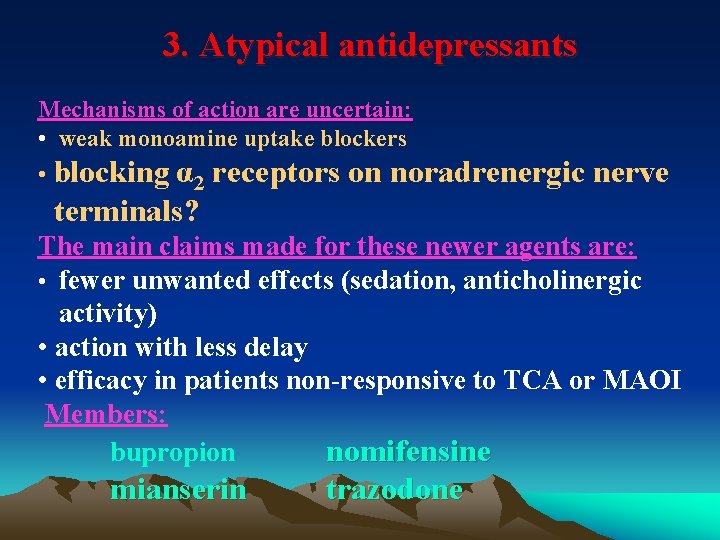
3. Atypical antidepressants Mechanisms of action are uncertain: • weak monoamine uptake blockers • blocking α 2 receptors on noradrenergic nerve terminals? The main claims made for these newer agents are: • fewer unwanted effects (sedation, anticholinergic activity) • action with less delay • efficacy in patients non-responsive to TCA or MAOI Members: bupropion nomifensine mianserin trazodone
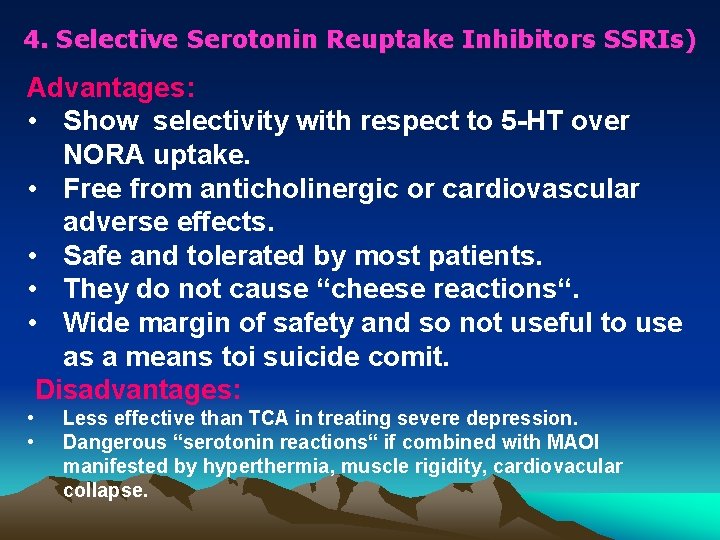
4. Selective Serotonin Reuptake Inhibitors SSRIs) Advantages: • Show selectivity with respect to 5 -HT over NORA uptake. • Free from anticholinergic or cardiovascular adverse effects. • Safe and tolerated by most patients. • They do not cause “cheese reactions“. • Wide margin of safety and so not useful to use as a means toi suicide comit. Disadvantages: • • Less effective than TCA in treating severe depression. Dangerous “serotonin reactions“ if combined with MAOI manifested by hyperthermia, muscle rigidity, cardiovacular collapse.
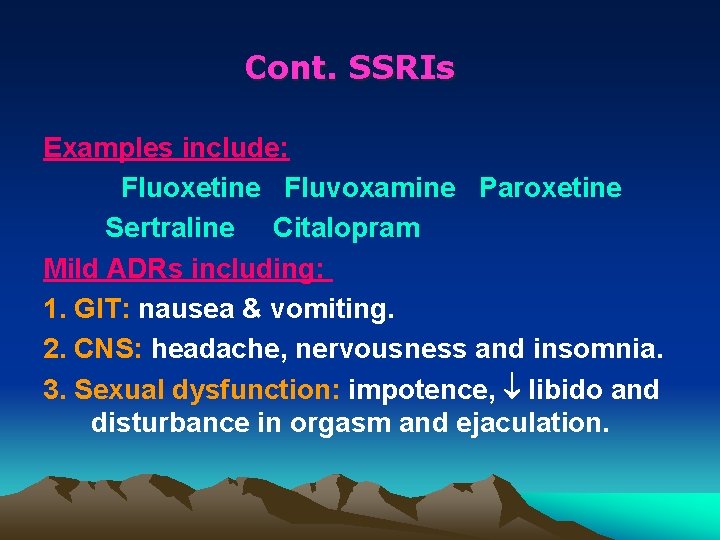
Cont. SSRIs Examples include: Fluoxetine Fluvoxamine Paroxetine Sertraline Citalopram Mild ADRs including: 1. GIT: nausea & vomiting. 2. CNS: headache, nervousness and insomnia. 3. Sexual dysfunction: impotence, libido and disturbance in orgasm and ejaculation.

Clinical Effectiveness of Antidepressants The overall clinical efficacy of antidepressants has been established in many well-controlled clinical studies. However, it is clear that a substantial proportion of patients recover spontaneously, and that 30 -40% of patients fail to improve with drug treatment. The effects of the drugs are significant, but not miraculous
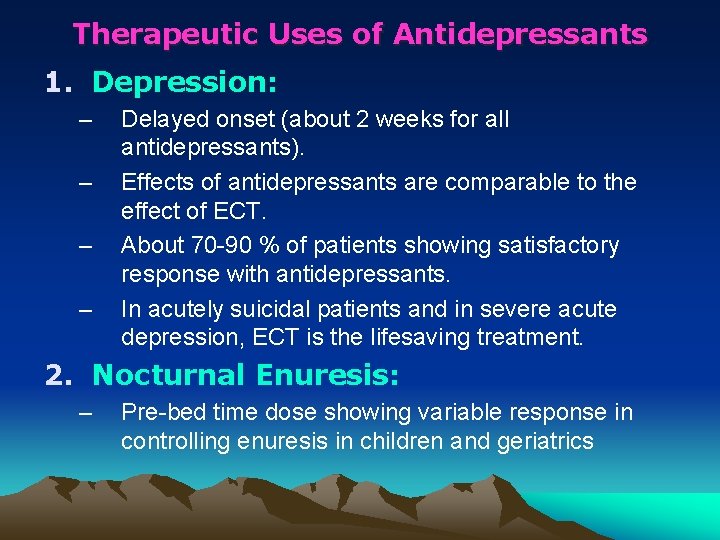
Therapeutic Uses of Antidepressants 1. Depression: – – Delayed onset (about 2 weeks for all antidepressants). Effects of antidepressants are comparable to the effect of ECT. About 70 -90 % of patients showing satisfactory response with antidepressants. In acutely suicidal patients and in severe acute depression, ECT is the lifesaving treatment. 2. Nocturnal Enuresis: – Pre-bed time dose showing variable response in controlling enuresis in children and geriatrics
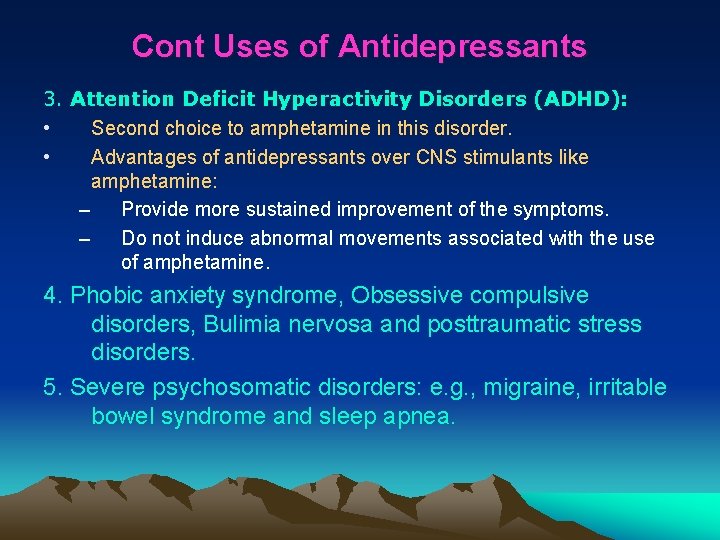
Cont Uses of Antidepressants 3. Attention Deficit Hyperactivity Disorders (ADHD): • Second choice to amphetamine in this disorder. • Advantages of antidepressants over CNS stimulants like amphetamine: – Provide more sustained improvement of the symptoms. – Do not induce abnormal movements associated with the use of amphetamine. 4. Phobic anxiety syndrome, Obsessive compulsive disorders, Bulimia nervosa and posttraumatic stress disorders. 5. Severe psychosomatic disorders: e. g. , migraine, irritable bowel syndrome and sleep apnea.
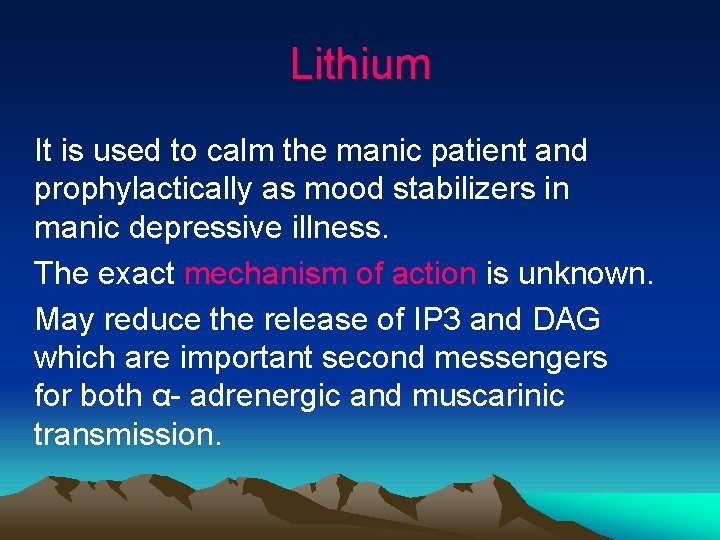
Lithium It is used to calm the manic patient and prophylactically as mood stabilizers in manic depressive illness. The exact mechanism of action is unknown. May reduce the release of IP 3 and DAG which are important second messengers for both α- adrenergic and muscarinic transmission.

Because of its slow onset lithium is used in prevention or prophylaxis of manic depressive illness It has low therapeutic index so need TDM. Its side effects on GIT, CNS, kidney, thyroid, cardic. Lithium toxicity precipitated by loss of water and sodium.
 Psychotropics
Psychotropics Antigentest åre
Antigentest åre Psychotropic medication
Psychotropic medication Dfps psychotropic medication training
Dfps psychotropic medication training Psychotropic medication
Psychotropic medication Lursidone
Lursidone Drugs that alter moods thoughts and sense perceptions
Drugs that alter moods thoughts and sense perceptions Af begets af
Af begets af Premedication drugs list
Premedication drugs list Floor or ward stock system
Floor or ward stock system Reconstitution medication labels
Reconstitution medication labels Muscarinic agonist
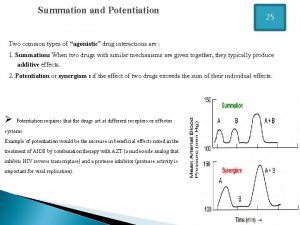
Muscarinic agonist Drug summation examples
Drug summation examples Myeloproliferative disorder
Myeloproliferative disorder Cardioversion anticoagulation
Cardioversion anticoagulation Antithyroid drugs
Antithyroid drugs Types of drugs
Types of drugs Can you buy drugs in gta 5 online
Can you buy drugs in gta 5 online Chapter 15 alcohol other drugs and driving
Chapter 15 alcohol other drugs and driving Cvs costco
Cvs costco Parasympathomimetic drugs
Parasympathomimetic drugs Narrow therapeutic index drugs
Narrow therapeutic index drugs Sulfonylurea drugs
Sulfonylurea drugs Rate and rhythm control drugs
Rate and rhythm control drugs Psychedelic drugs that distort perceptions and evoke
Psychedelic drugs that distort perceptions and evoke Antidiabetic drugs classification
Antidiabetic drugs classification Healio
Healio Psychoactive drugs chart
Psychoactive drugs chart Vasicoselective action
Vasicoselective action British model involved with drugs
British model involved with drugs Ion trapping
Ion trapping Schedule 2 drugs
Schedule 2 drugs Histamine autacoid
Histamine autacoid