REMSA PROTOCOL UPDATE 2016 Misty Plumley EMS Specialist
- Slides: 33
REMSA PROTOCOL UPDATE 2016 Misty Plumley, EMS Specialist �Physician’s Orders for Life Sustaining Treatment (POLST) Update �TXA Update
Objectives �Discuss changes to Physician’s Orders for Life Sustaining Treatment (POLST) form �Review POLST procedures and intent �Identify impacts with POLST changes to prehospital clinical care �Discuss and update Tranexamic Acid (TXA) Trial Study �Review next steps with TXA Trial Study
Physician’s Orders for Life Sustaining Treatment �Developed originally in Oregon to help patients make informed decisions to express their wishes regarding their end of life care. ◦ Went into California Law ( AB 3000, Statutes, Chapter 266) on January 1, 2009 ◦ Voluntary ◦ Designed to assist emergency personnel, healthcare facilities and healthcare staff with care steps ◦ 98% effective in expressing patient’s wishes
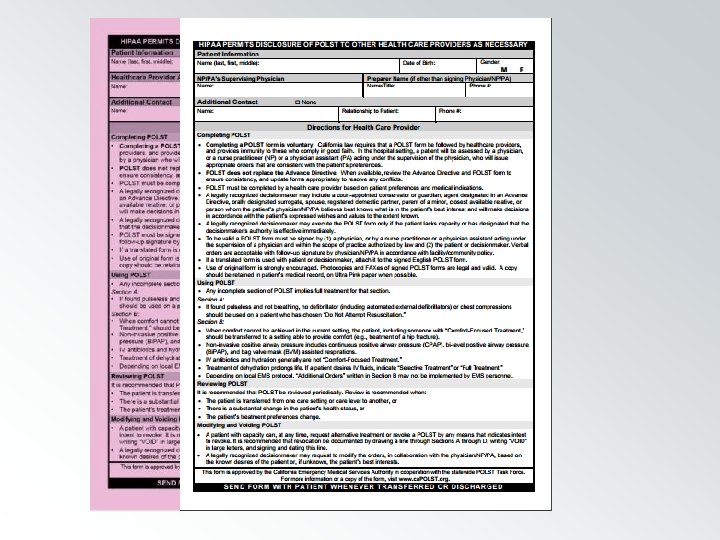
POLST Review �Designed to clearly delineate care the patient wishes to receive, or not receive, in the event they are incapacitated during their serious illness. �Identifies whether or not to attempt/provide: ◦ ◦ CPR Artificial Nutrition High intensity treatments Intubation and artificial ventilations
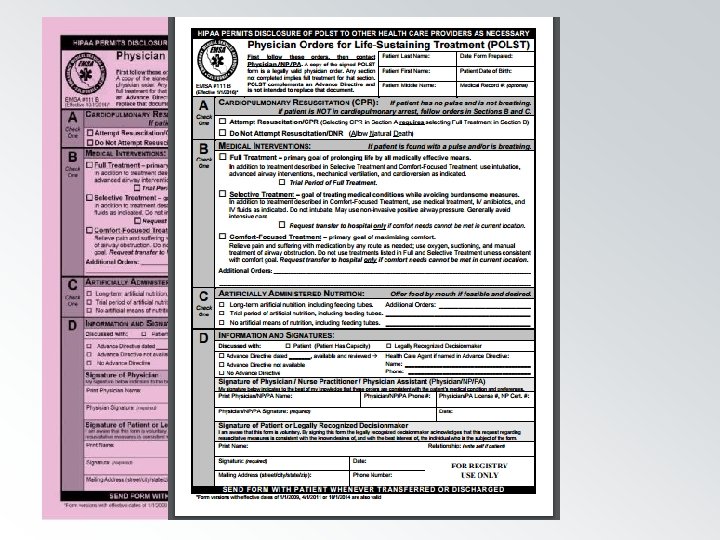
POLST Review �Completed for seriously ill patients �Printed on bright pink paper (revised in 2011 & 2014) ◦ Acceptable in copy form or on any color paper, from any year �Signed by physician* and patient �Different than an advance directive �Goes with the patient from facility to facility
POLST Review �The patient’s wishes are the patient’s wishes, and they should be honored. POLST serves as a formal acknowledgement of those wishes. �Patients have near-absolute authority to refuse resuscitation ◦ From EMSA Guideline #311 (DNR and Other Patient-Designated Directives, October 2014) �Near absolute references competency/informed consent
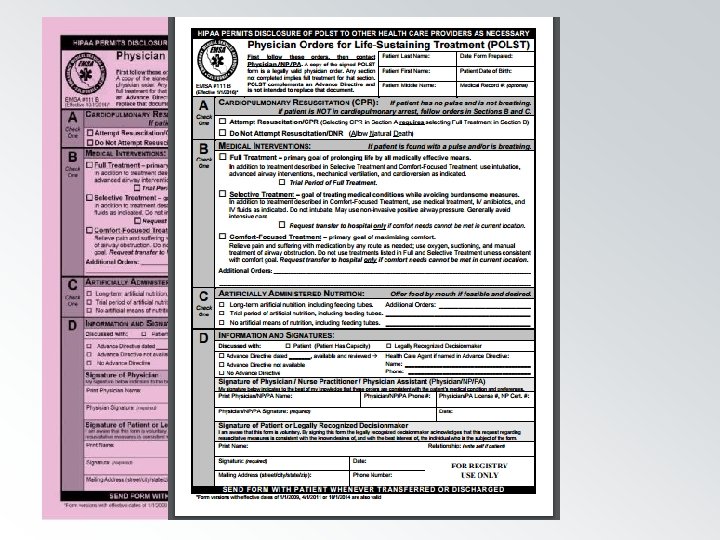
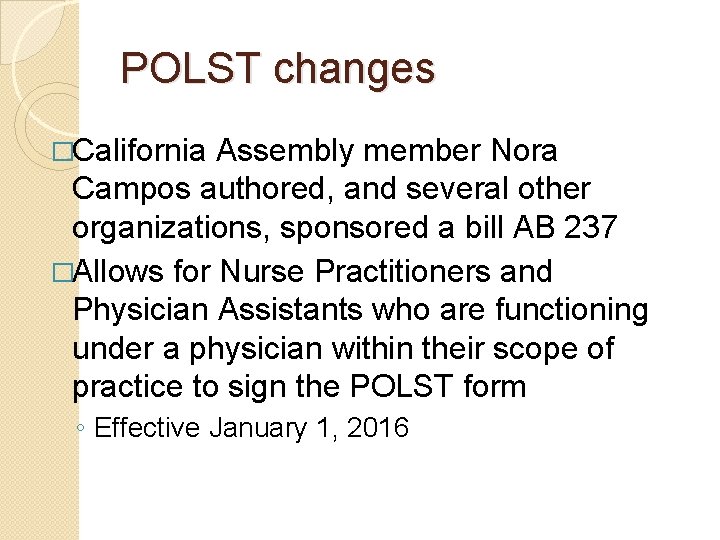
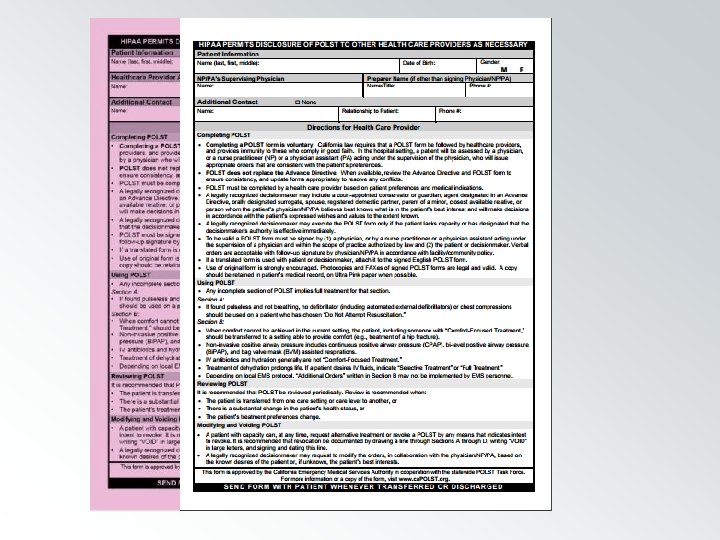
POLST changes �California Assembly member Nora Campos authored, and several other organizations, sponsored a bill AB 237 �Allows for Nurse Practitioners and Physician Assistants who are functioning under a physician within their scope of practice to sign the POLST form ◦ Effective January 1, 2016
Impacts of POLST changes � Increase in non-physician signatures on the POLST form ◦ Nurse Practitioner and Physician Assistant signatures are acceptable ◦ No other healthcare provider levels beyond Physician/NP/PA are acceptable � Advance Directives must have physician signatures on them still
Impact of Using POLST �POLST forms are designed to express a patient’s wishes about their end of life before they are incapacitated �Valid POLST forms are to be honored and utilized as a representation of the patient’s consent (or lack of consent) for procedures
POLST validity �Check boxes in the respective sections indicate the level of care the patient �Not �If just for CPR a box is a treatment section is not checked or filled in, the patient receives the highest level of care available in that section
POLST validity �POLST forms must be signed and dated by the appropriate healthcare staff, as well as the patient ◦ Not valid unless dated. ◦ Healthcare staff member should have license number listed as well. �No expiration �Transfer as valid from facility to facility
POLST in action #1 �My patient is at home on hospice care, has a respiratory rate of 6, a weak carotid pulse, and a POLST form. The home health care staff at scene is uncomfortable, and called 911 because the patient is dying.
POLST in action #1 �POLST say? form is valid. What does it ◦ Comfort measures only. ◦ No transfer unless comfort measures cannot be met in current location ◦ No CPR, no intubation, no artificial nutrition, no artificial ventilation �Do what the POLST form says. Can the patient’s comfort be met at the current location?
POLST in action #1 �Home health care staff have all the currently prescribed medications for the patient’s terminal illness. Supervisor is on the way. Family members are on the way from work. Comfort measures can be met at home. �POLST says no transfer, no CPR, no intubation, no artificial ventilation. �Allow the patient to expire at home as they wished. Document patient response and POLST form decisions on e. PCR.
POLST in action #2 �Respond to a healthcare facility for an unconscious/unresponsive patient. Patient is pulseless and apneic. Staff reports there is a DNR they think.
POLST in action #2 �Next steps? ◦ Assess patient to determine cardiac arrest ◦ Begin BLS efforts while directing staff to obtain the DNR �Need to determine DNR validity �Staff returns with a form that is not a DNR, but is a POLST form
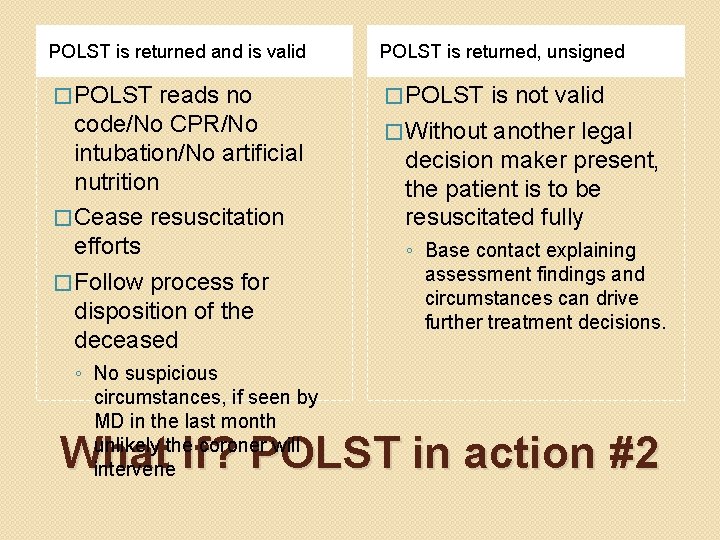
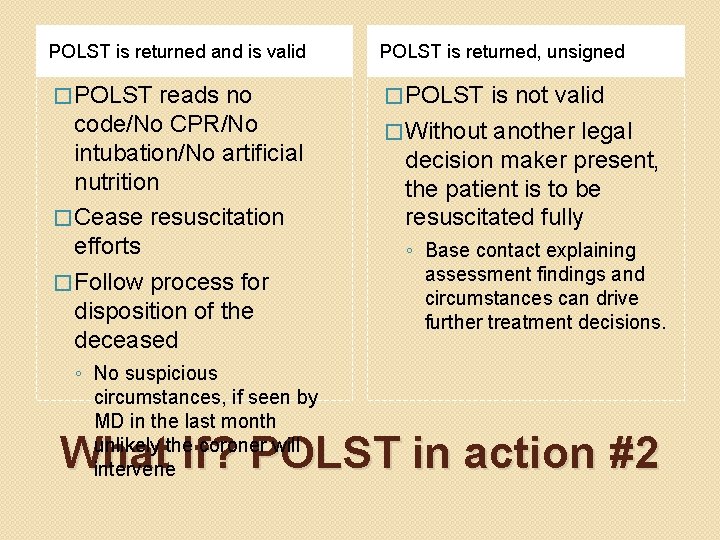
POLST is returned and is valid POLST is returned, unsigned � POLST reads no code/No CPR/No intubation/No artificial nutrition � Cease resuscitation efforts � Follow process for disposition of the deceased ◦ No suspicious circumstances, if seen by MD in the last month unlikely the coroner will intervene is not valid � Without another legal decision maker present, the patient is to be resuscitated fully ◦ Base contact explaining assessment findings and circumstances can drive further treatment decisions. What If? POLST in action #2
What if the POLST and DNR conflict? �POLST is designed to complement a DNR not replace it. �If there is a conflict with the documents, then the most recently signed document prevails ◦ (reference the signature and date lines) �POLST can be for any age ◦ Advance directives are initiated for patients 18 years or older
Changing wishes on a POLST form �Sections of the POLST form can be voided – strikethrough and dated. �Can be re-evaluated by MD/NP/PA or patient or decision maker with changes in condition and amended as needed ◦ Most recent document prevails
Designated Agent for Healthcare Decisions �May not be an operator or employee of a community care facility or a residential care facility where you are receiving care, �May not be your supervising health care provider or employee of the health care institution where you are receiving care, unless your agent is related to you or is a coworker. �Can take effect immediately or only when incapacitated Reference California Probate Code 4701
Designated Agent for Healthcare Decisions �Advance Directive language can limit an agent’s authority ◦ Limit situations or circumstances where the agent’s decisions take precedence �Advance Directive’s can also designate alternate decision makers, if the first/second/third choice is unavailable.
Designated Agent for Healthcare Decisions �Traditional priority (age dependent): ◦ Patient �or legal guardian/court appointed conservator ◦ Spouse/Legal Domestic Partner ◦ Parent ◦ Family member – legally related, closer to the patient is preferable if disagreements arise ◦ *as the need may arise Health care providers use their policies and judgment to make decisions if the patient’s wishes are not known
POLST Resources �http: //csupalliativecare. org/programs/polst/ ◦ Online training program that can provide CEU’s �http: //capolst. org/polst-for-healthcare- providers/ �Coalition for Compassionate Care of California http: //coalitionccc. org/
2016 Protocol Update TRANEXAMIC ACID (TXA) TRIAL STUDY PROGRESS UPDATE
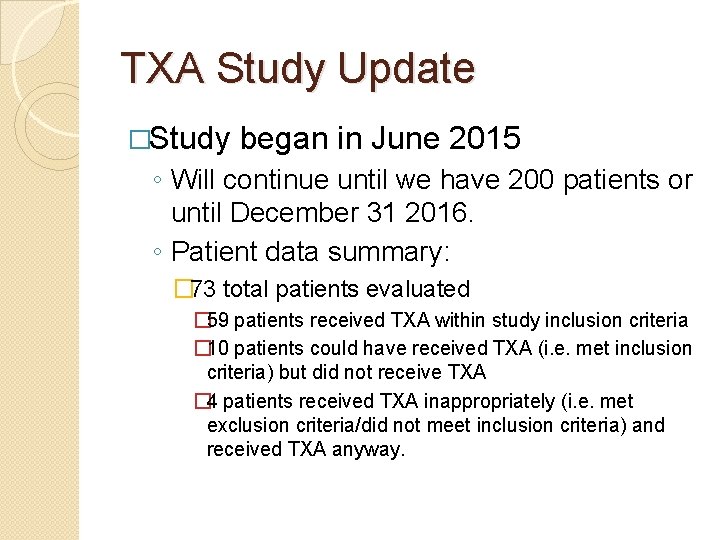
TXA Study Update �Study began in June 2015 ◦ Will continue until we have 200 patients or until December 31 2016. ◦ Patient data summary: � 73 total patients evaluated � 59 patients received TXA within study inclusion criteria � 10 patients could have received TXA (i. e. met inclusion criteria) but did not receive TXA � 4 patients received TXA inappropriately (i. e. met exclusion criteria/did not meet inclusion criteria) and received TXA anyway.
TXA Trial Study Ongoing Needs �Adherence to Inclusion Criteria: ◦ First: Age �Patient must be an adult, at least 18 years of age ◦ Second: Trauma �Does the patient meet REMSA defined Trauma criteria? (REMSA 5301) ◦ Third: Inclusion Criteria �Does the patient meet TXA Trial Study Inclusion Criteria? (REMSA 5801) ◦ A definitive yes is required for all 3 steps before TXA is administered.
TXA Trial Study Ongoing Needs �Continue to document Estimated Blood loss �Documentation to support that trauma triage indicators and TXA inclusion criteria met �Document vital signs: ◦ Pre-TXA ◦ During TXA infusion** ◦ Post-TXA administration �Document PCR arm band number on the
TXA Trial Study Ongoing Needs �TXA vitals ◦ Blood pressure is used as part of inclusion criteria ◦ Diastolic Blood pressure should be measured �Trends mean arterial pressure �Trends response to therapy �Helps predict shock states �If unattainable document 0 (zero) (i. e. 60/0) �Avoid palpating blood pressures
TXA Trial Study Next Steps �Continue to enroll patients based on REMSA Policy 5801 inclusion criteria until we patient quota or meet the time line of the Trial Study �CQI auditing of 100% of TXA patients �Additional education beyond this update not anticipated at this time
Objectives �Discuss changes to Physician’s Orders for Life Sustaining Treatment (POLST) form �Review POLST procedures and intent �Identify impacts with POLST changes to prehospital clinical care �Discuss and update Tranexamic Acid (TXA) Trial Study �Review next steps with TXA Trial Study
QUESTIONS?