Radiological Category Ultrasound Principal Modality 1 Ultrasound Principal







- Slides: 17
Radiological Category: Ultrasound Principal Modality (1): Ultrasound Principal Modality (2): None Case Report #0586 Submitted by: J. Austin Hancock, M. D. Faculty reviewer: Chitra Chandrasekhar, M. D. Date accepted: 15 March 2009
Case History 20 -year-old woman, G 4 P 1 A 2, with last menstrual period 8 weeks prior to presentation. She currently complains of vaginal bleeding and abdominal cramping.
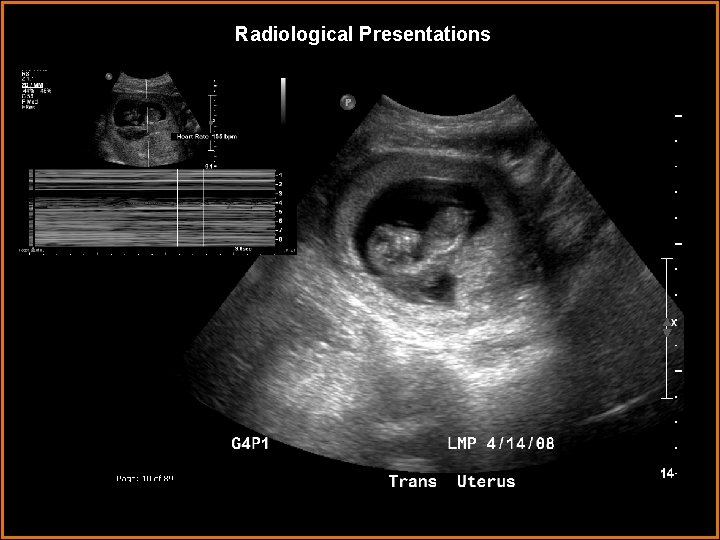
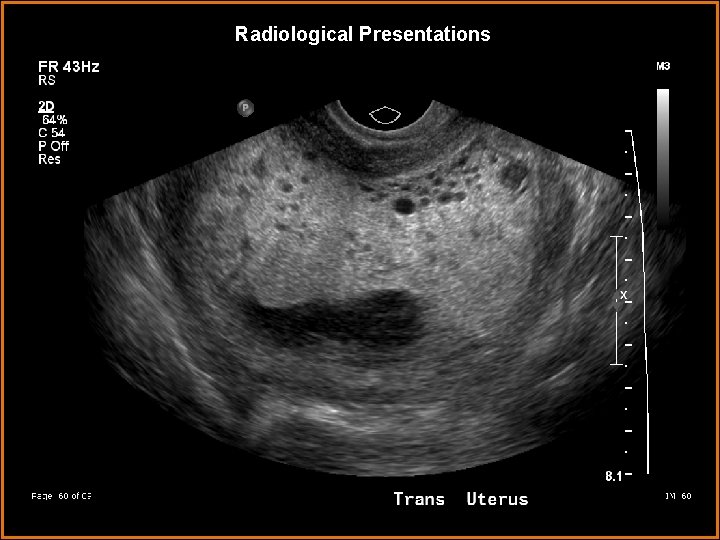
Radiological Presentations
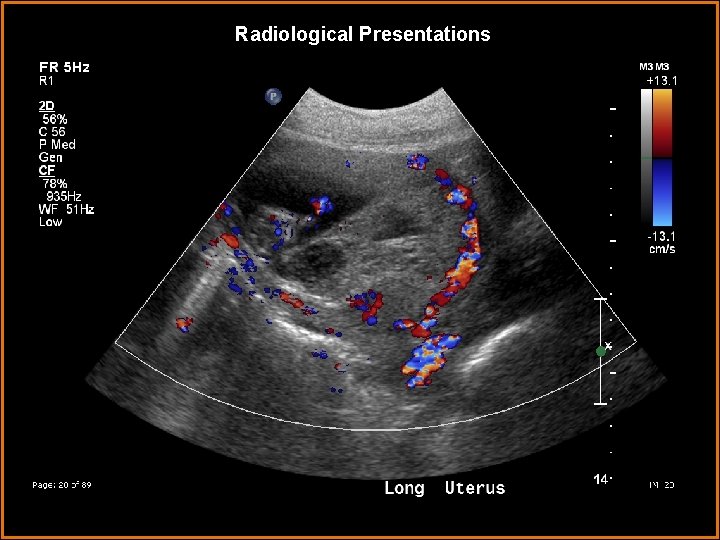
Radiological Presentations
Radiological Presentations

Radiological Presentations
Radiological Presentations

Radiological Presentations
Radiological Presentations
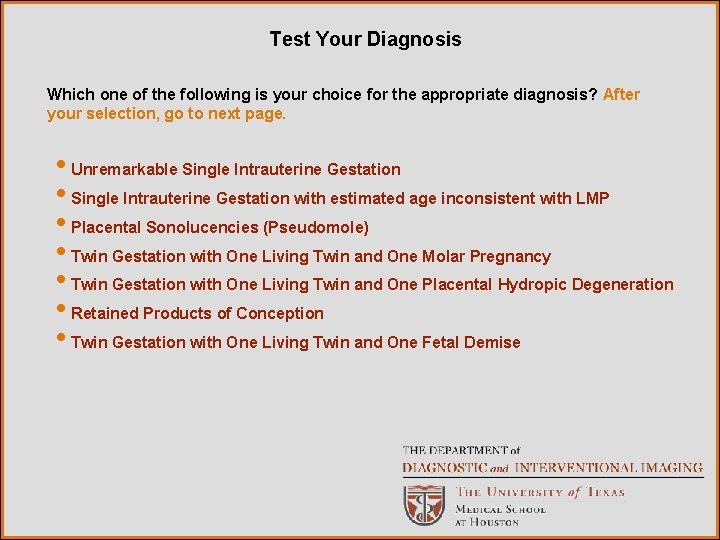
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Unremarkable Single Intrauterine Gestation • Single Intrauterine Gestation with estimated age inconsistent with LMP • Placental Sonolucencies (Pseudomole) • Twin Gestation with One Living Twin and One Molar Pregnancy • Twin Gestation with One Living Twin and One Placental Hydropic Degeneration • Retained Products of Conception • Twin Gestation with One Living Twin and One Fetal Demise

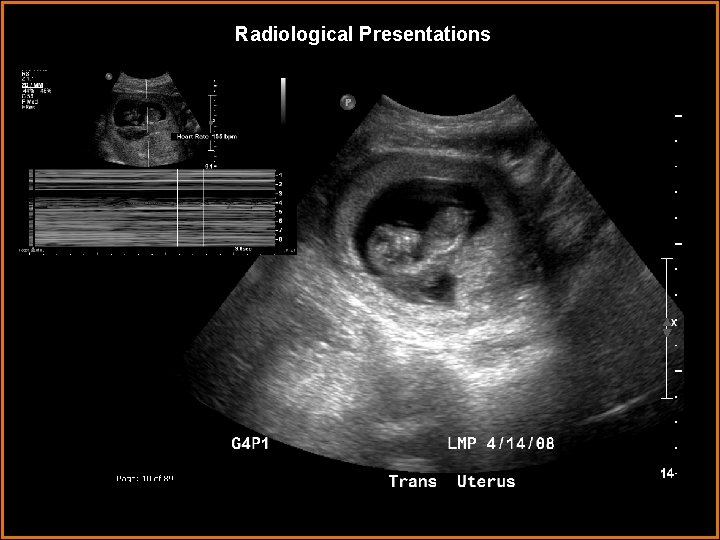
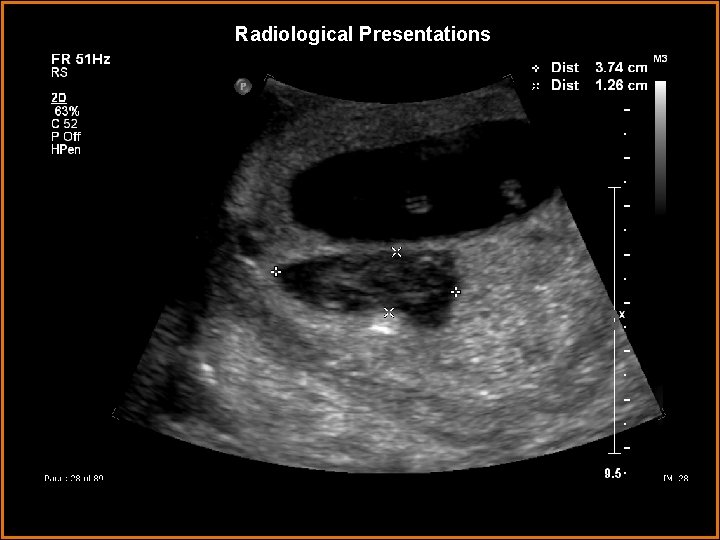
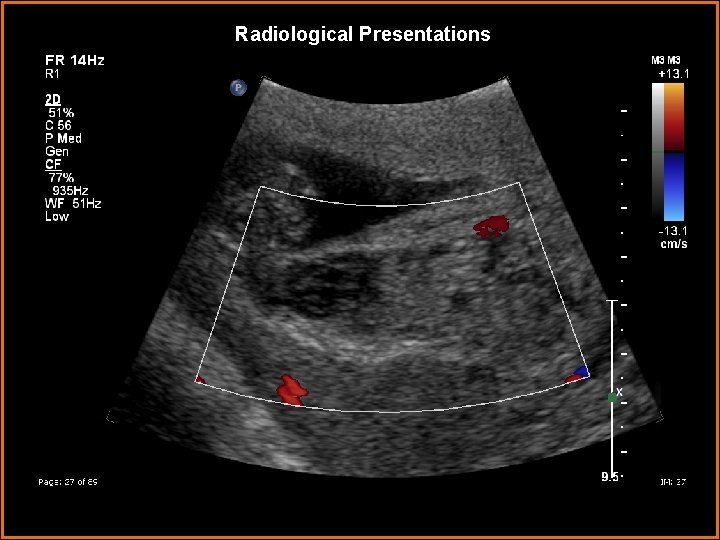
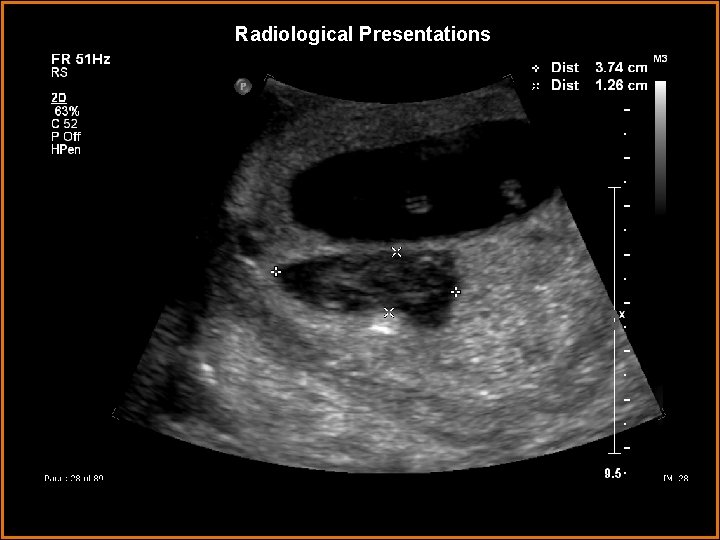
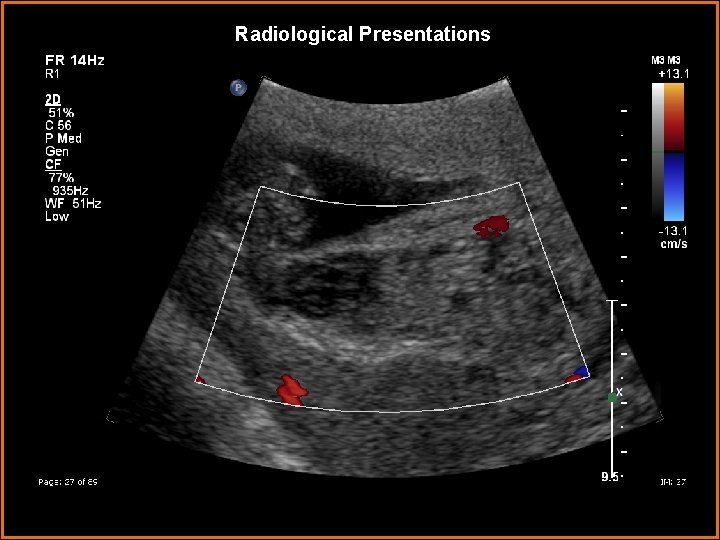
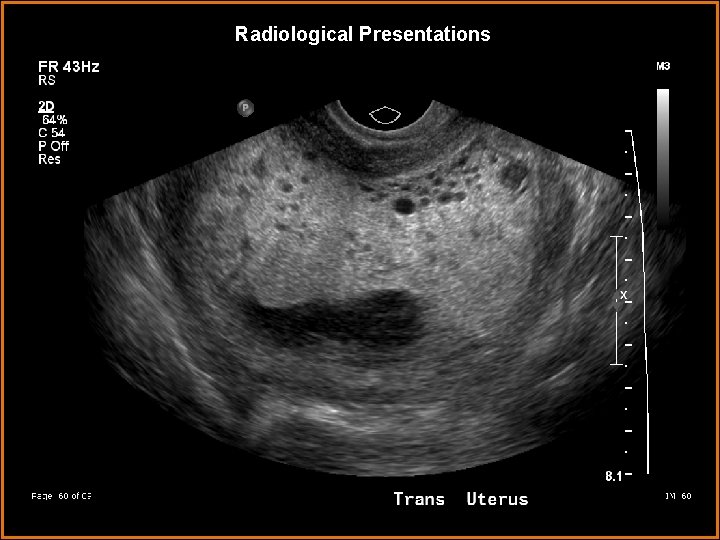
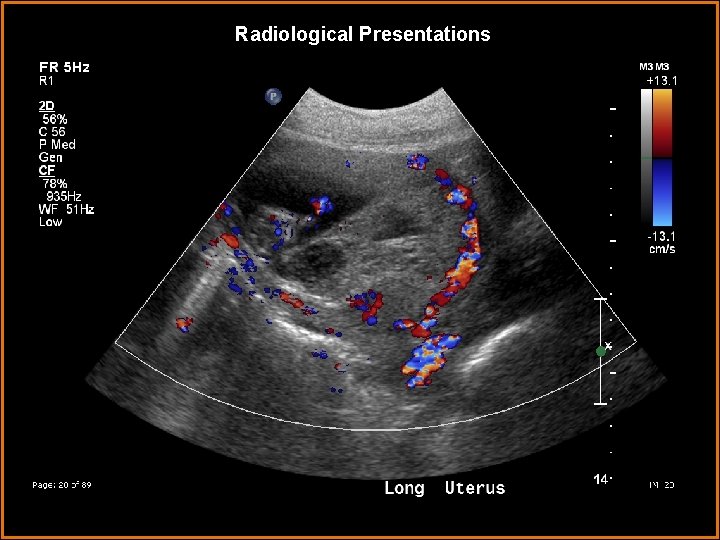
Findings and Differentials Findings: A single intrauterine cavity is present with two gestational sacs. One contains a living fetus consistent with 11 w 4 d gestation, the other contains a complexcystic mass with low density and increased peripheral vascularity. Differentials: • Twin Gestation with One Living Twin and One Molar Pregnancy • Twin Gestation with One Living Fetus and One Placental Hydropic Degeneration

Discussion Gestational trophoblastic disease is characterized by the proliferation of trophoblastic tissue (the tissue surrounding the blastocyst that develops into the chorion and amnion) in pregnant or recently pregnant women. There are two primary genetic subtypes: Complete hydatidiform mole and Partial hydatidiform mole. Complete hydatidiform moles are the most common variant. Genetically, most are monospermic, arising from the fertilization of an anucleated egg by a normal haploid sperm cell with resulting endoreduplication. About 20% of cases are dispermic, arising from fertilization of an anucleated egg by either two sperm or a single diploid sperm cell. Cytogenetically, 90% are 46 XX, 10% are 46 XY. In either case, all complete hydatiform moles have a diploid karyotype that is entirely paternal in origin. Partial hydatidiform moles are, in contrast, triploid, typically arising from the simultaneous fertilization of a normal haploid ovum by two haploid sperm cells (or less commonly, a diploid ovum and single haploid sperm). Tetraploidy may be rarely be encountered. Cytogenetically, partial moles are 69 XXX or 69 XXY.

Discussion Hydatidiform moles become Invasive hydatidiform moles (Gestational Trophoblastic Neoplasm) as they grow into the myometrium or metastasize, no longer being confined simply to the endometrium. This form of gestational trophoblastic disease shares the same histology as the hydatiform mole from which it arose. Gestational trophoblastic neoplasm is diagnosed in 15 -20% of patients with a complete hydatidiform mole and 2% of partial hydatidiform moles. The most frequent sites of metastases are the lungs, lower genital tract, brain, liver, kidney and gastrointestinal tract. Choriocarcinomas are nonseminomatous germ cell tumors composed of malignant trophoblastic cells that lack hydropic villi (differentiating them from hydatidiform moles). Choriocarcinomas are preceded by a hydatidiform mole 50% of the time; 25% are preceded by an abortion, 3% by ectopic pregnancy and the remaining 22% by a full-term pregnancy.

Discussion Manifestations of gestational trophoblastic disease include excessive uterine enlargement, vomiting, vaginal bleeding and preeclampsia. Diagnosis includes measurement of the β subunit of human chorionic gonadotropin (which is extremely elevated) and pelvic ultrasonography with confirmation by biopsy. Tumors are removed by dilation and curettage. Chemotherapy is indicated if disease persists after removal. In cases of twin gestation with one living fetus and one complete hydatidiform mole, multiple case reports from the obstetric literature demonstrate that the living fetus can grow to full term, though the risk of fetal demise increases approximately 29%. It is unclear if allowing the gestation to progress increases the risk of gestational trophoblastic neoplasm, but at least one study reports the risk as increased by about 35%. The ultrasonographic findings with a complete hydatidiform mole include a cystic intrauterine mass representing a hydropic placenta, lack of any fetal anatomy and marked hypervascularity with high velocity, low-impedance flow. The intrauterine mass is often associated with adjacent sonolucent hematoma and hemorrhage within the mass itself. In an invasive (malignant) hydatiform mole (gestational trophoblastic neoplasm) there is invasion of the myometrium with a heterogeneous cystic mass seen in the myometrium itself. A coexistent dizygotic twin can be present with a separate normal placenta.

Discussion A partial hydatidiform mole will have an abnormal fetus with profound intrauterine growth restriction and multiple anomalies. If the extra chromosomes are parental in origin there will be a large cystic placenta; if maternal, the placenta will be small. There are three primary differential diagnostic considerations. 1. Placental Hydropic Degeneration – Hydropic change of the placenta without proliferation. This occurs after pregnancy failure from embryonic demise or anembryonic gestation. While it is less vascular than gestational trophoblastic disease (having low velocity with low impedance), its appearance can look identical to a complete hydatidiform mole. It is associated with low β-HCG levels but must be differentiated histologically. 2. Placental Sonolucencies (Pseudomole) – Often associated with placentomegaly, placental lakes and intervillous thrombus can mimic the cystic spaces seen in a complete hydatidiform mole. Pseudomole is associated with oligohydramniosis, preeclampsia and intrauterine growth restriction. 3. Retained Products of Conception –Incomplete uterine evacuation after pregnancy, abortion or miscarriage, retained products of conception can present as a complex endometrial mass demonstrating prominent vascularity (high velocity with low impedance). β-HCG levels are usually normal to slightly elevated.
Diagnosis Dizygotic twin gestation. Single living intrauterine fetus consistent with 11 w 4 d gestation. Complete hydatidiform molar pregnancy in a second gestational sac. (β-HCG level was greater than 280, 000. )
References Ahuja, Anil T. (2007). Diagnostic Imaging: Ultrasound. Manitoba, Canada: Amirsys. http: //www. humpath. com/hydatiform-moles Piura, B. Twin Pregnancy With a Complete Hydatidiform Mole and Surviving Co-existent Fetus. Archives of Gynecology and Obstetrics. 2008 Oct; 278(4): 377 -82 Porter, Robert S. (2008). The Merk Manual Online. Whitehouse Station, NJ: Merk Research Laboratories. Vaisbuch, E. Twin Pregnancy Consisting of a Complete Hydatidiform Mole and Coexistent Fetus: Report of Two Cases and Review of the Literature. Gynecologic Oncology. 2005 July; 98(1): 19 -23 Wee, L. Prenatal diagnosis and management of twin pregnancies complicated by a coexisting molar pregnancy. Prenatal Diagnosis. 2006 Apr; 26(4): 373
 Ferriman–gallwey score
Ferriman–gallwey score Erate category 2 eligible equipment
Erate category 2 eligible equipment National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health Epistemic modality
Epistemic modality Modality in software engineering
Modality in software engineering Cardinality and modality
Cardinality and modality Lexical vs auxiliary verbs
Lexical vs auxiliary verbs Skill focus: persuasion
Skill focus: persuasion Callendreasonlocaluserinitiated
Callendreasonlocaluserinitiated Epistemic modality
Epistemic modality Diplode
Diplode What is modality in statistics
What is modality in statistics Sodality vs modality
Sodality vs modality Cardinality and modality
Cardinality and modality Deontic and epistemic modality exercises
Deontic and epistemic modality exercises