Radiological Category Nuclear Principal Modality 1 Nuclear Principal

- Slides: 15
Radiological Category: Nuclear Principal Modality (1): Nuclear Principal Modality (2): Ultrasound Case Report #0083 Submitted by: Neil Bhargava , M. D. Faculty reviewer: Usha Joseph, M. D Date accepted: 13 January 2004

Case History Acute severe right upper quadrant abdominal pain.
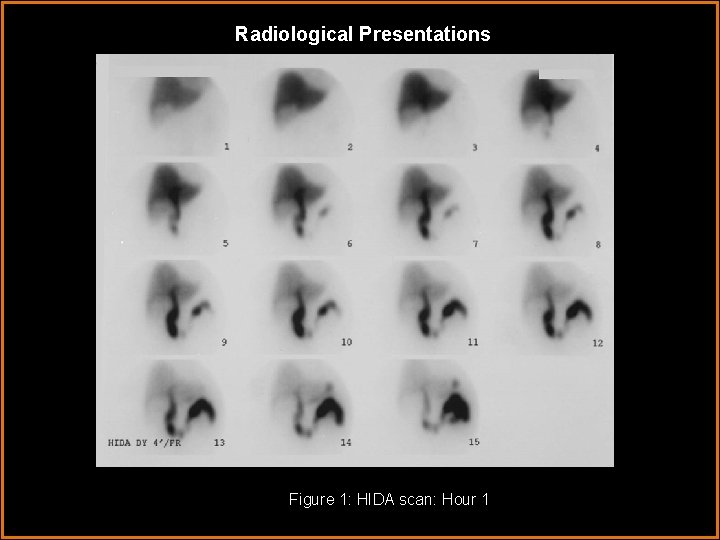
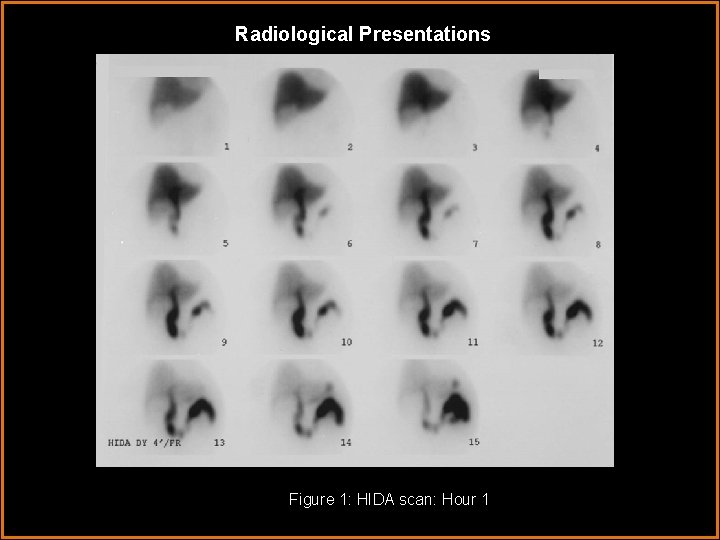
Radiological Presentations Figure 1: HIDA scan: Hour 1
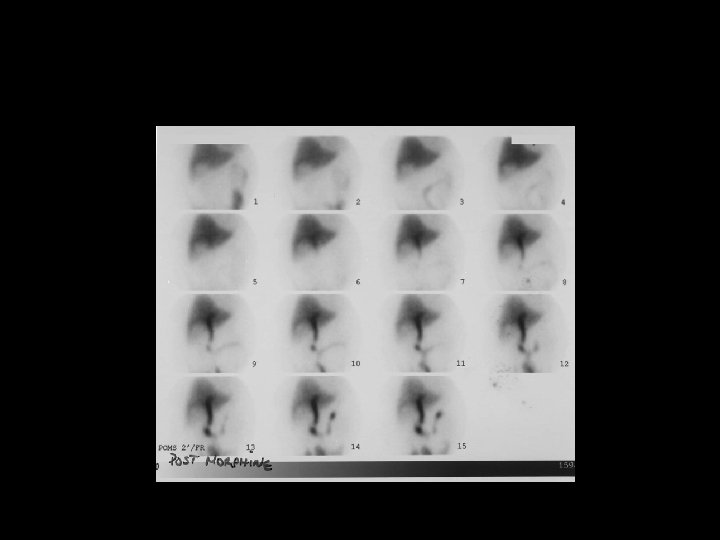
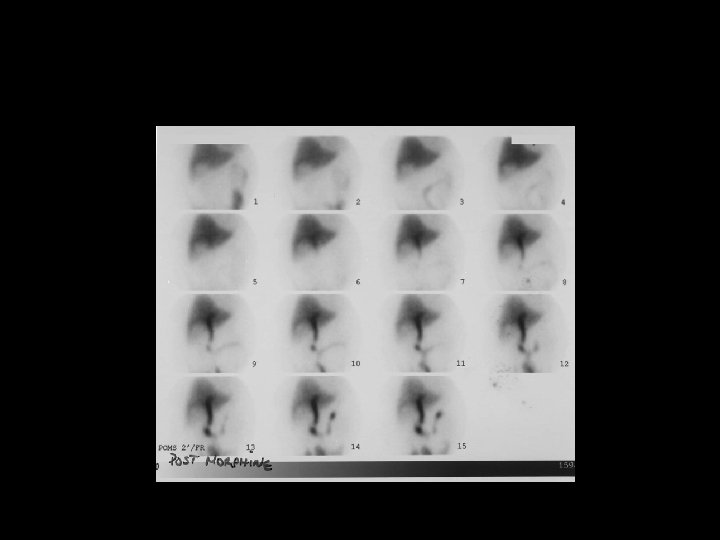
Radiological Presentations
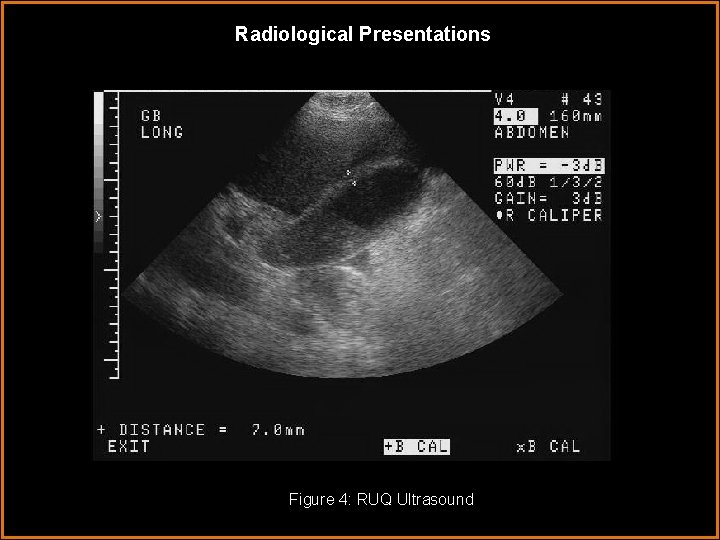
Radiological Presentations Figure 4: RUQ Ultrasound
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Normal HIDA, Sludge on US • Acute Calculous Cholecystitis on HIDA and US • Acute Acalculous Cholecystitis on HIDA and US • Gallbladder Cancer
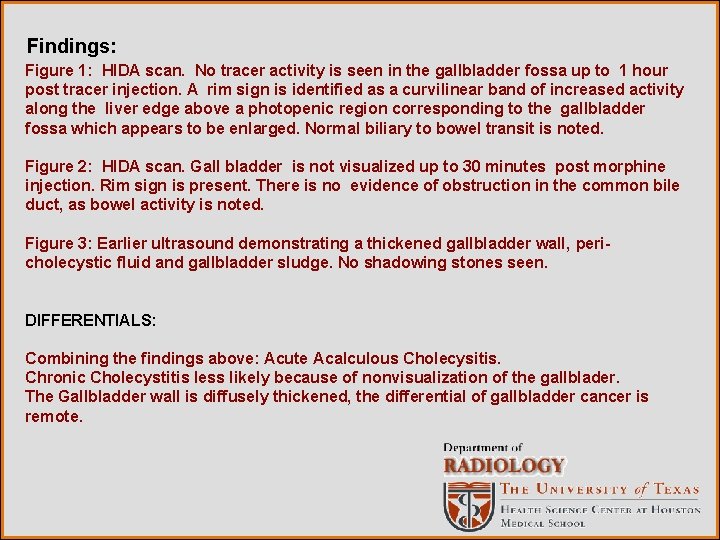
Findings: Figure 1: HIDA scan. No tracer activity is seen in the gallbladder fossa up to 1 hour post tracer injection. A rim sign is identified as a curvilinear band of increased activity along the liver edge above a photopenic region corresponding to the gallbladder fossa which appears to be enlarged. Normal biliary to bowel transit is noted. Figure 2: HIDA scan. Gall bladder is not visualized up to 30 minutes post morphine injection. Rim sign is present. There is no evidence of obstruction in the common bile duct, as bowel activity is noted. Figure 3: Earlier ultrasound demonstrating a thickened gallbladder wall, pericholecystic fluid and gallbladder sludge. No shadowing stones seen. DIFFERENTIALS: Combining the findings above: Acute Acalculous Cholecysitis. Chronic Cholecystitis less likely because of nonvisualization of the gallblader. The Gallbladder wall is diffusely thickened, the differential of gallbladder cancer is remote.
Discussion HEPATOBILIARY IMAGING / BACKGROUND: • Hepatobiliary imaging is used to evaluate acute and chronic cholecystitis, biliary patency, identification of biliary leaks, and in neonates for differentiation of biliary atresia from neonatal hepatitis. Less common uses are for evaluation of biliary dyskinesia and sphincter of Oddi dysfunction. There are several Technetium 99 m labeled imino diacetic acid analogs (Tc 99 m-IDA). All IDA agents have high hepatic extraction, some more than others, based on minor changes in the phenyl ring. They undergo biliary excretion using the same pathway as bilirubin but are subject to competitive inhibition by high serum bilirubin levels. The radiopharmaceutical is typically removed from the circulation due to active transport by hepatocytes and is then excreted into the bile canaliculi, biliary radicals, common bile duct, gallbladder and finally the small intestine. The half-time of liver clearance is 15 to 20 minutes. Persistent visualization of the cardiac blood pool after 5 to 10 minutes and increasing renal excretion are signs of hepatic dysfunction.
Discussion HEPATOBILIARY IMAGING / TECHNIQUE: • A minimum of 4 hours of fasting (an overnight fast is ideal) is suggested, as the presence of food in the upper GI tract stimulates intermittent contraction of the gallbladder which interferes with biliary filling thus potentially rendering a falsepositive result. A typical dose of 3 to 10 m. Ci of Tc 99 m- mebrofenin (Choletec), an IDA analogue with high hepatic extraction, is injected intravenously followed by immediate flow images of the liver. Higher doses of radio tracer are required with elevated serum bilrubin levels. Dynamic anterior images of the abdomen are obtained in the supine position for the next 60 minutes. The gallbladder is usually visualized within 30 minutes and small bowel activity by 30 - 60 minutes. Delayed images should be obtained hourly if the gallbladder is not seen after 60 minutes for up to 4 hours, unless intravenous morphine is used (as discussed below). NORMAL SCAN: • Activity is seen in the liver by 5 minutes. Major hepatic ducts and the common bile duct are visualized by 10 minutes, followed by gallbladder visualization. Twothirds of biliary flow bypasses the gallbladder and enters the duodenum directly. Occasionally, a small amount of biliary reflux into the stomach can be seen as a normal variant.
Discussion HEPATOBILIARY IMAGING / ACUTE CHOLECYSTITIS: • The majority of patients with acute cholecystitis (95%) have cystic duct obstruction, and thus the radiopharmaceutical cannot enter the inflamed gallbladder. Accuracy in diagnosing acute cholecystitis exceeds 95% in fasting individuals. In contrast, the accuracy in ultrasound is 80 to 85%. • The rim sign, also known as the pericholecystic hepatic activity (PCHA) , refers to a curvilinear band of increased activity in the right lobe of liver above the gallbladder fossa, and is seen in 25% of patients with acute cholecystitis. It usually indicates complicated or later stage of acute cholecystitis. These patients are at increased risk of gall bladder perforation and gangrene. The cystic duct sign is seen as a small nubbin of activity in the cystic duct proximal to the site of obstruction.
Discussion HEPATOBILIARY IMAGING / CCK: • Intravenous Cholecystokinin (CCK) results in gallbladder contraction, relaxation of the sphincter of Oddi, increased bowel motility and bile secretion. CCK 8 or Sincalide, a synthetic C-terminal octapeptide of CCK, in a dose of 0. 02 micrograms/kg is typically given intravenously 30 minutes prior to scanning in patients with viscous bile or prolonged fasting , to help reduces the false-positive rate. A potential pitfall is that it may obscure the diagnosis in those with chronic cholecysitis, as it speeds up visualization of the gallbladder in those who other wise would have delayed visualization. This problem can be avoided by administering CCK, 30 -60 minutes into the study followed by a delayed injection of a second dose of Tc 99 m-IDA 15 to 30 minutes afterwards.
Discussion HEPATOBILIARY IMAGING / MORPHINE: • Intravenous Morphine sulfate in a dose of 0. 04 mg/kg or more commonly as a 3 mg total dose can help decrease the study time in select situations. Morphine causes constriction of the sphincter of Oddi resulting in a 10 fold rise in back-pressure in the common bile duct, and hence bile flows into the lower pressure gallbladder, provided the cystic duct is patent. Typically, morphine is injected if the gallbladder is not visualized despite the visualization of the common bile duct and bowel activity at 60 mins post injection of radio tracer. The gallbladder fills in 5 to 10 minutes in normal patients post morphine. Sometimes, the radiopharmaceutical needs to be re-injected if there is not enough tracer activity remaining in the liver and common bile duct. Non-visualization of the gallbladder despite morphine injection is compatible with the diagnosis of acute cholecystitis. If the cystic duct sign is present, morphine can force activity past the obstructed duct, causing an inappropriate change from a true-positive result to a false-negative result. Once morphine is administered, CCK should not be given, as pressure from a contracted gallbladder against a contracted Sphincter of Oddi can cause considerable patient discomfort.
Discussion Delayed gall bladder visualization (greater than one hour post injection) correlates well with a diagnosis of Chronic cholecystitis. However, in the Acute setting, Acalculous cholecystitis with partial Cystic Duct obstruction cannot be excluded. Approximately 85% of patients with Acalculous cholecystitis will have similar findings as the Calculous variety. The difficulty occurs when there is delayed gall bladder visualization. The CCK analogue , Sincalide in a dose of 0. 02 mcg/kg, may help to differentiate these entities. A delayed visualized gall bladder that fails to contract after CCK analog administration is often (but not entirely ) consistent with Acute Acalculous cholecystitis. An ejection fraction (EF) can be obtained by comparing gall bladder activity at time of injection and 20 mins later. (Some use a 30 min count calculation instead). An EF below 35% is considered abnormal. In the chronic setting, a low gall bladder EF would suggest Chronic Biliary Dysfunction, such as chronic cholecystitis or biliary dyskinesia. Therefore a reduced EF by itself is not specific for either entity. Other factors such as poor , but definite visualization of the Gall bladder or common bile duct and less than optimal contractile response to CCK analogue augmentation, have been reported in patients with chronic cholecystitis. However, delayed gall bladder visualization and poor response to secretagogue, in the ACUTE setting are hallmarks for Acalculous Cholecystitis.
Discussion HEPATOBILIARY IMAGING / PITFALLS AND CAVEATS: • 100% of normally functioning gall bladders are seen by 60 minutes. 10% of normal functioning gall bladders are seen only by 50 -60 minutes, hence morphine is given after 60 minutes. If the gallbladder is seen by 30 minutes post morphine, there is abnormal gall bladder function, but not acute cholecystitis. • In patients with increased renal excretion due to impaired biliary function, an extrarenal pelvis may be confused for gallbladder activity. This situation can easily be differentiated by obtaining a right lateral image. The gallbladder should lie anteriorly. • Activity in the gallbladder may be obscured by overlying duodenal activity. An additional view in the left anterior oblique or right lateral position or upright position may help differentiate these two structures. • False positive results have been reported in patients with alcoholism, some cases of pancreatitis, hepatocellular dysfunction, cholangiocarcinoma of the cystic duct, or from prolonged fasting for 24 hours or total parentral nutrition. False-negative results have been reported in patients with acalculous cholecystitis, a duodenal diverticulum simulating a gallbladder, an accessory cystic duct or a biliary duplication cyst.
Diagnosis Acute acalculous cholecystitis. Reference: Mettler FA, Guiberteau MJ. Essentials of Nuclear Medicine Imaging. Fourth Edition. Saunders. 1998: 260 -7. Thrall JH and Zeissman HA. Nuclear Medicine : The Requisites. Second Edition. Mosby. 2001: 228 -247
 Erate category 1
Erate category 1 Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Lesson 15 nuclear quest nuclear reactions
Lesson 15 nuclear quest nuclear reactions Fisión nuclear vs fision nuclear
Fisión nuclear vs fision nuclear Epistemic modality
Epistemic modality Viqt
Viqt Modality in statistics
Modality in statistics Stefan savi
Stefan savi Modality in software engineering
Modality in software engineering Deontic and epistemic modality exercises
Deontic and epistemic modality exercises Modality in software engineering
Modality in software engineering Data modeling fundamentals
Data modeling fundamentals Modality
Modality