Radiological Category Neuroradiology Principal Modality 1 Fetal and

- Slides: 17
Radiological Category: Neuroradiology Principal Modality (1): Fetal and Neonatal MRI Principal Modality (2): Conventional Radiography Case Report # 763 Submitted by: Mary Kristen Jesse, M. D. Faculty reviewer: Emilio Supsupin, M. D. , The University of Texas Medical School at Houston Date accepted: 15 February, 2011 .

Case History 41 -year-old, G 4 P 3 female with abnormal fetal ultrasound.
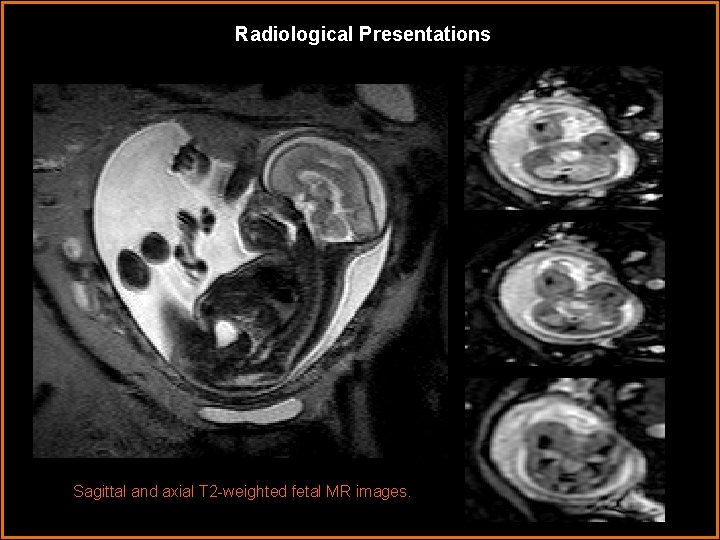
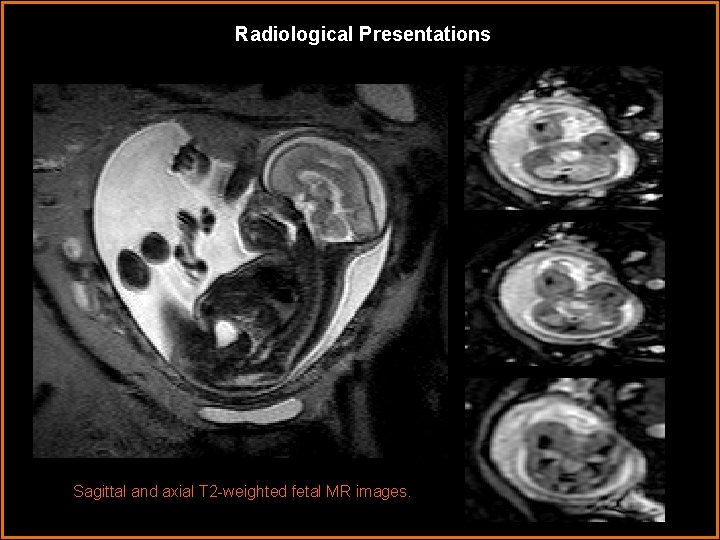
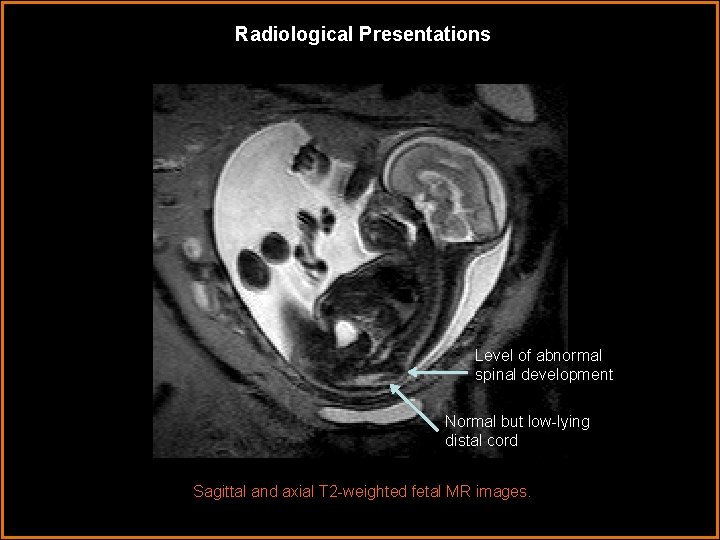
Radiological Presentations Sagittal and axial T 2 -weighted fetal MR images.
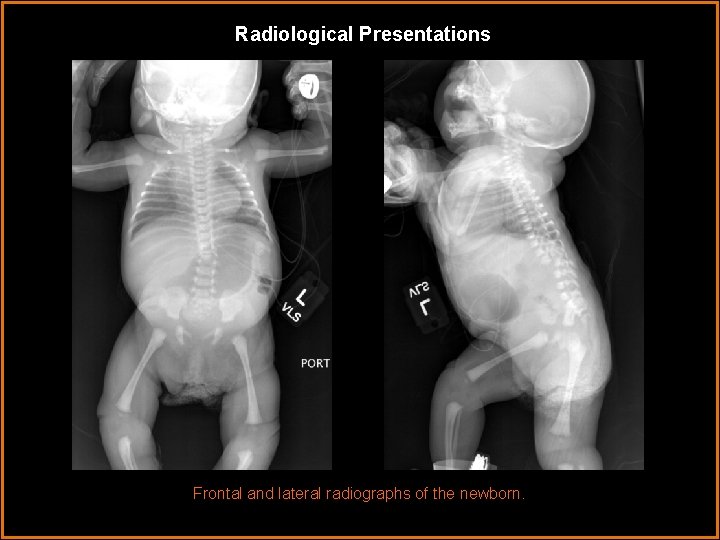
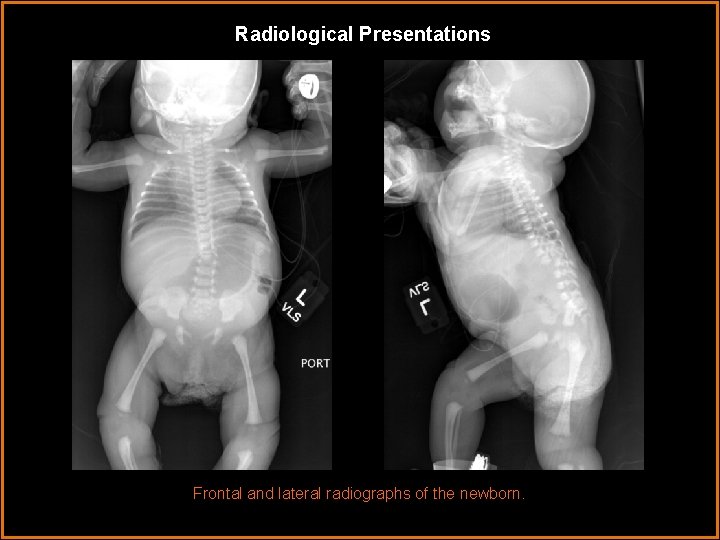
Radiological Presentations Frontal and lateral radiographs of the newborn.
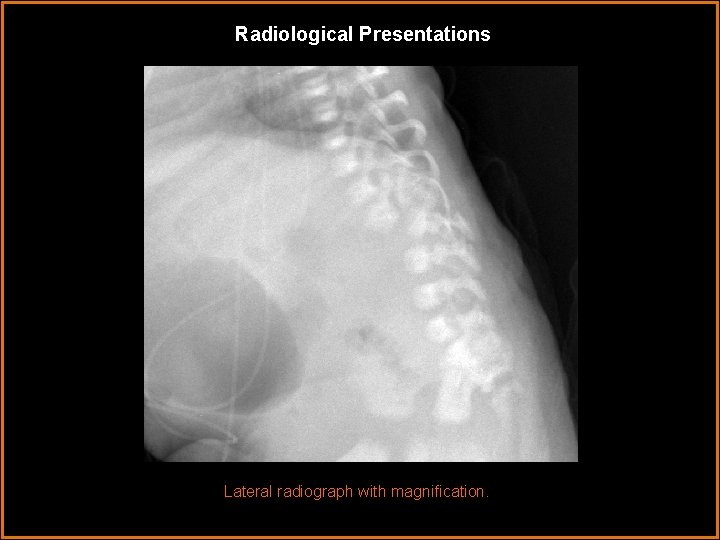
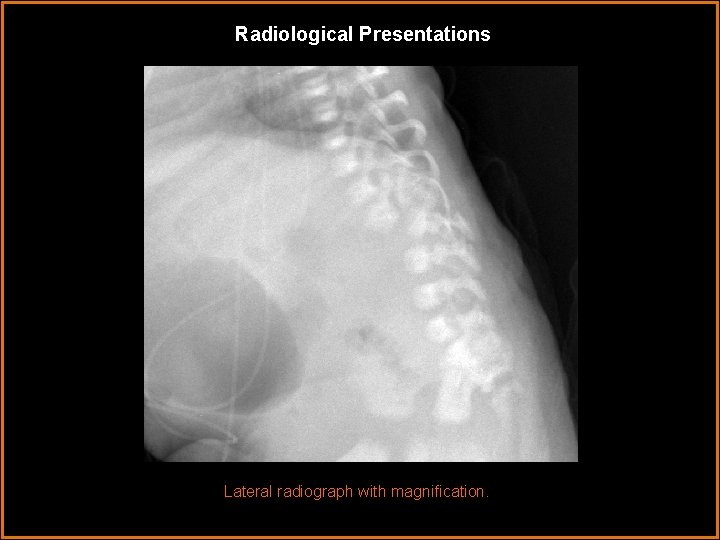
Radiological Presentations Lateral radiograph with magnification.
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Segmental spinal dysgenesis • Posttraumatic myelomalacia • Segmental vertebra-hemivertebra/butterfly vertebra • Caudal regression syndrome
Findings and Differentials Findings: Fetal MRI demonstrates severe kyphoscoliosis with the vertex at L 1. Axial T 2 weighted images show complete interruption of the normal spinal canal at this level. A normal-appearing cord is visualized both cranial and caudal to the level of cord disruption. No abnormal T 2 signal is seen in the cord. The spinal cord terminates abnormally low, in the region of the sacral spine. Neonatal radiographs again demonstrate severe kyphoscoliosis with marked anterolisthesis of T 12 on L 1. Differentials: • Segmental spinal dysgenesis • Hemivertebra/butterfly vertebra • Posttraumatic myelomalacia • Caudal regression syndrome
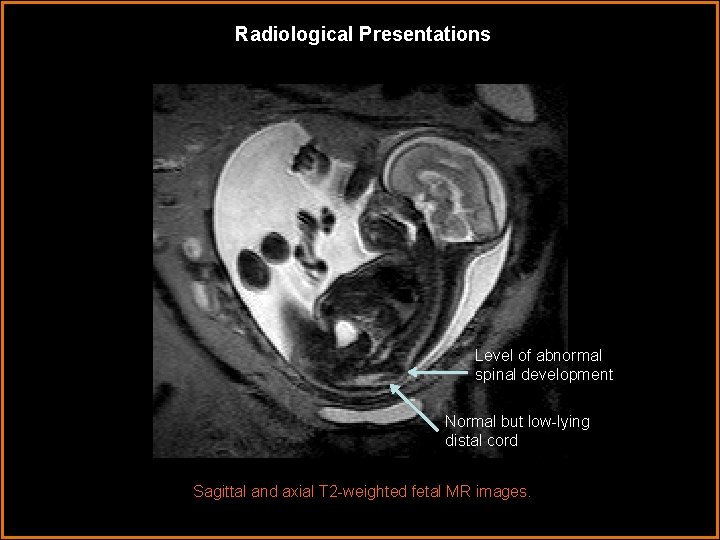
Radiological Presentations Level of abnormal spinal development Normal but low-lying distal cord Sagittal and axial T 2 -weighted fetal MR images.
Discussion Segmental spinal dysgenesis is a rare abnormality in which the spinal canal fails to develop properly. This abnormality is thought to result from abnormal segmental gene expression during fetal development. These deformities lie on a morphologic continuum, with physical presentations ranging from a mild segmental defect to complete spinal dysgenesis, as in this case. This abnormality is typically discovered on prenatal ultrasound and further characterized on fetal MRI. Common radiographic findings include severe kyphoscoliosis and listhesis of the lower thoracic or upper lumbar spine with complete disruption of the spinal cord. The spinal cord terminates abnormally high or low, often in the mid-thoracic or sacral spine, but otherwise has a near-normal appearance both above and below the level of disruption. In the postnatal period, this congenital abnormality can be differentiated from posttraumatic causes by the absence of cord edema. The T 2 cord signal appears normal where the cord is visible.
Discussion The exact embryology involved in segmental spinal dysgenesis is not entirely known, however in the article by Tortori-Donati et al, several hypotheses are presented. It is believed that the abnormality occurs early, during gastrulation, and is a result of inaccurately specified cells with respect to their rostrocaudal location. This inaccurate specification leads to detrimental apoptosis and spinal canal disruption in a lower thoracic/upper lumbar spine. The gastrulation in the lower canal and cord is not disrupted explaining the normal appearance of the distal cord. Theories to explain the common finding of low-lying or sacral cord are also presented in this article. One theory is that abnormal gene specification in the distal cord is also abnormal, leading to distal formation of a spinal cord. The second theory postulates that the low-lying cord is a response by chordamesenchymal cells to a perceived proximal “injury”, stimulating proliferation of neural cells in the caudal direction.
Discussion Common clinical presentations of SSD include, lower extremity paraplegia, spasticity and progressive weakness. Most patients with preserved lower extremity function at birth, rapidly progress to complete lower extremity paralysis. Severe kyphoscoliosis, lower extremity deformity and equinocavovarus feet are also common physical manifestations. Genitourinary abnormalities are associated with spinal dysgenesis. Horseshoe kidney, renal dysgenesis and crossed-fused renal ectopia have all been described in conjunction with spinal dysgenesis. Neurogenic bladder is present in all patients. Cutaneous stigmata, including sacral dimples/tufts and angiomata, have also been described.
Discussion Treatment of segmental spinal dysgenesis is controversial, and no single method has proven overwhelmingly successful in restoring lower extremity function. The current standard of care includes bracing followed by spinal fusion. According to the article by Flynn et al, in the few reported cases in which partial lower extremity function was preserved, spinal fusion was performed immediately upon diagnosis. Complications from neurogenic bladder, including recurrent urinary tract infections, bacteremia/sepsis and renal failure, cause the greatest morbidity in these children.
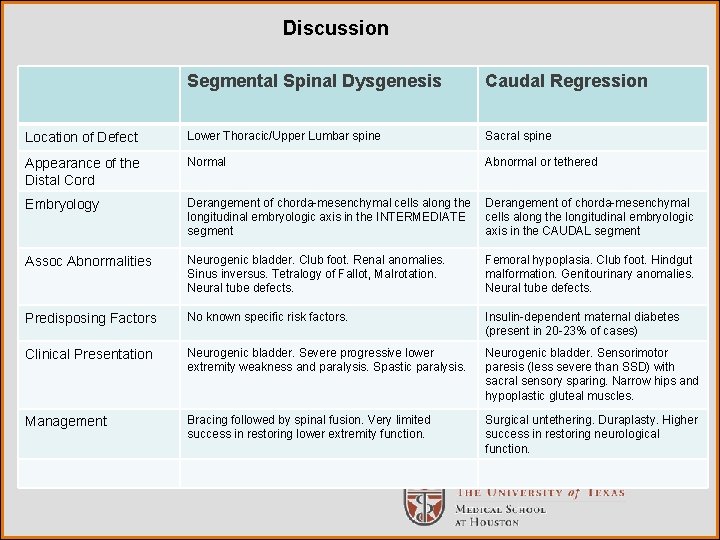
Discussion Caudal regression syndrome (CRS), also known as caudal dysgenesis, would be a probable diagnosis if the abnormality was present in the sacral spine. In CRS, the lumbosacral spine is dysgenic and the distal cord, abnormal. Caudal regression syndrome and segmental spinal dysgenesis are abnormalities that result from similar embryologic malformations differentiated only by the level of abnormal gene expression. Further differentiating characteristics are illustrated in the following table.
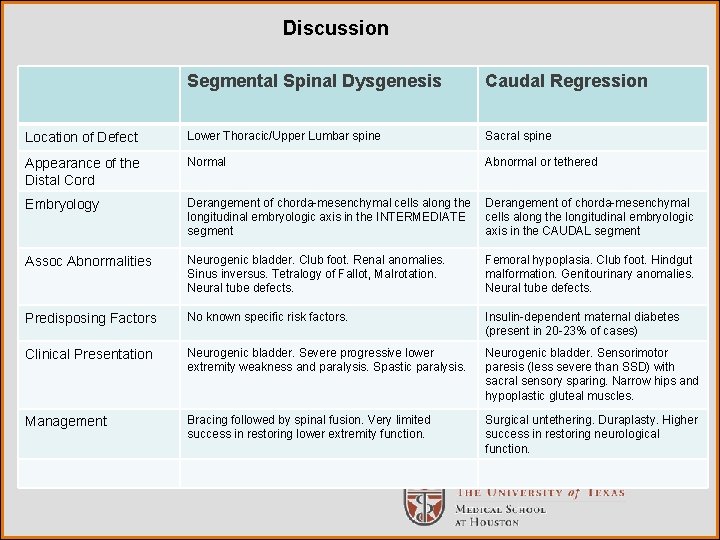
Discussion Segmental Spinal Dysgenesis Caudal Regression Location of Defect Lower Thoracic/Upper Lumbar spine Sacral spine Appearance of the Distal Cord Normal Abnormal or tethered Embryology Derangement of chorda-mesenchymal cells along the longitudinal embryologic axis in the INTERMEDIATE segment Derangement of chorda-mesenchymal cells along the longitudinal embryologic axis in the CAUDAL segment Assoc Abnormalities Neurogenic bladder. Club foot. Renal anomalies. Sinus inversus. Tetralogy of Fallot, Malrotation. Neural tube defects. Femoral hypoplasia. Club foot. Hindgut malformation. Genitourinary anomalies. Neural tube defects. Predisposing Factors No known specific risk factors. Insulin-dependent maternal diabetes (present in 20 -23% of cases) Clinical Presentation Neurogenic bladder. Severe progressive lower extremity weakness and paralysis. Spastic paralysis. Neurogenic bladder. Sensorimotor paresis (less severe than SSD) with sacral sensory sparing. Narrow hips and hypoplastic gluteal muscles. Management Bracing followed by spinal fusion. Very limited success in restoring lower extremity function. Surgical untethering. Duraplasty. Higher success in restoring neurological function.
Discussion Other diagnostic considerations, including posttraumatic or infectious etiologies, can be easily differentiated by the presence of the abnormality on fetal imaging and the lack of edema in the spinal cord. Butterfly vertebra/hemivertebra may lie on the morphologic continuum with spinal dysgenesis, but in this case, the presence of spinal cord disruption makes the diagnosis of segmental spinal dysgenesis more likely.
Diagnosis Segmental spinal dysgenesis.
References 1. Flynn JM, Otsuka NY, Emans JB, Hall JE, Hresko MT, “Segmental spinal dysgensesis: early neurologic deterioration and treatment. “Journal of Pediatric Orthopaedics. 1997 Jan-Feb: 17(1): 100 -4. 2. Mahomen, N, Nardoo, J. “ Case Series: Segmental Spinal Dysgenesis“. SA Journal of Radiology. June 2009. 29 -32. 3. Tortori-Donati, P, Maria Paola Fondelli, Andrea Rossi, Charles A. Raybaud, Armando Cama, and Valeria Capra “Segmental Spinal Dysgenesis: Neuroradiologic Findings with Clinical and Embryologic Correlation American Journal of Neuroradiology. March 1999: 20: 445– 456. 4. Barkovich, James “Segmental Spinal Dysgenesis“ Stat. DX 5. Letts, RM, Jawadi, AH. “Congenital Spinal Deformity. “ www. emedicine. com
 Ohsu neuroradiology
Ohsu neuroradiology Center for devices and radiological health
Center for devices and radiological health Erate category 2 eligible equipment
Erate category 2 eligible equipment National radiological emergency preparedness conference
National radiological emergency preparedness conference Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Cardinality and modality
Cardinality and modality Data modeling fundamentals
Data modeling fundamentals Deontic and epistemic modality exercises
Deontic and epistemic modality exercises One to many relationship line
One to many relationship line Cardinality and modality
Cardinality and modality Epistemic modality
Epistemic modality Epistemic modality
Epistemic modality Pacs modality workstation
Pacs modality workstation Modality in statistics
Modality in statistics Exteroceptors
Exteroceptors Tom arbuthnot
Tom arbuthnot Entity class in software engineering
Entity class in software engineering