Radiological Category Musculoskeletal Principal Modality 1 MRI Principal

- Slides: 15
Radiological Category: Musculoskeletal Principal Modality (1): MRI Principal Modality (2): None Case Report # 0840 Submitted by: Megan Kalambo, M. D. Faculty reviewer: Larry Kramer, M. D. Date accepted: 01 December 2011
Case History 31 year old post-partum female with elevated LFTs and right upper quadrant pain.
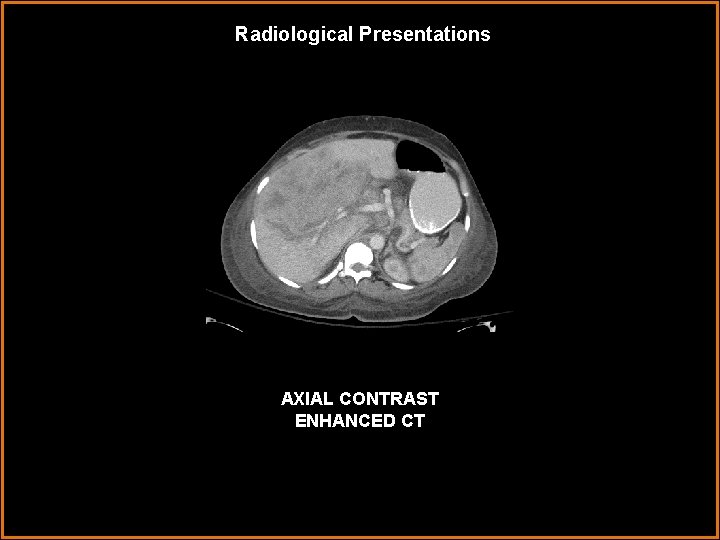
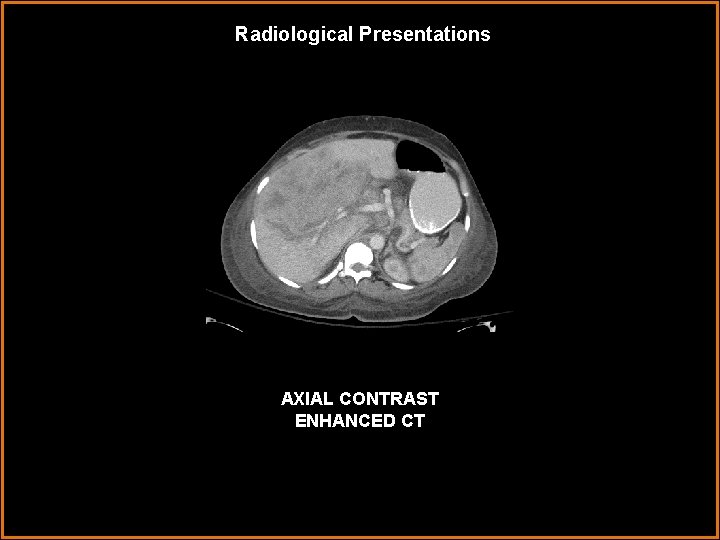
Radiological Presentations AXIAL CONTRAST ENHANCED CT
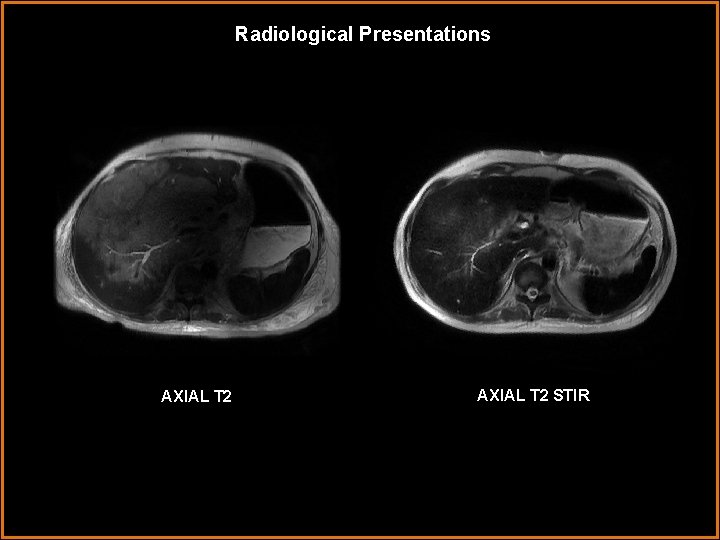
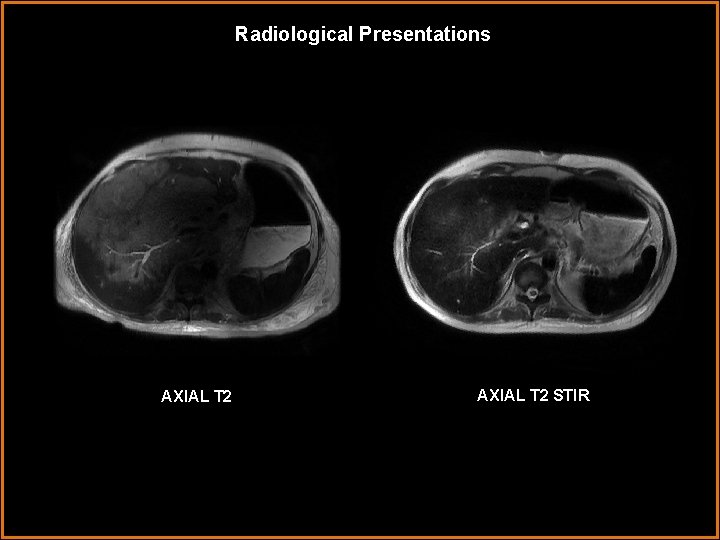
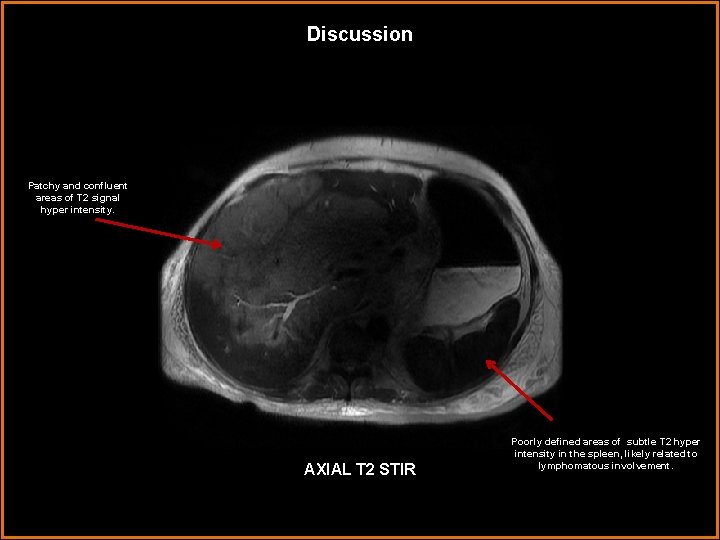
Radiological Presentations AXIAL T 2 STIR
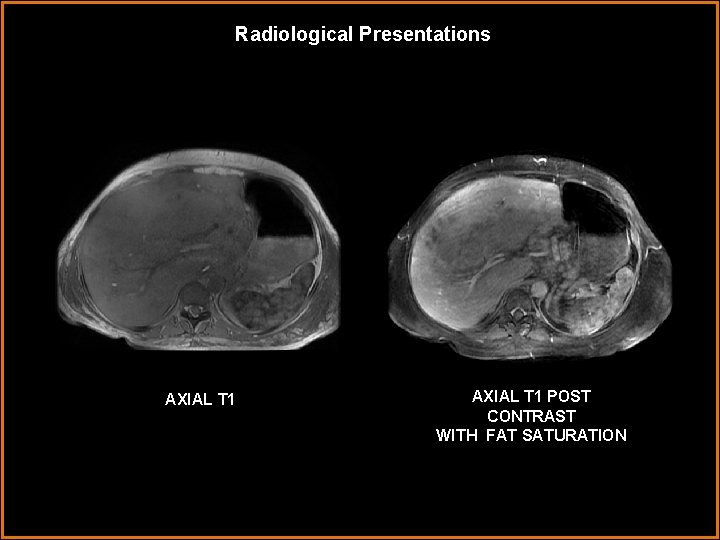
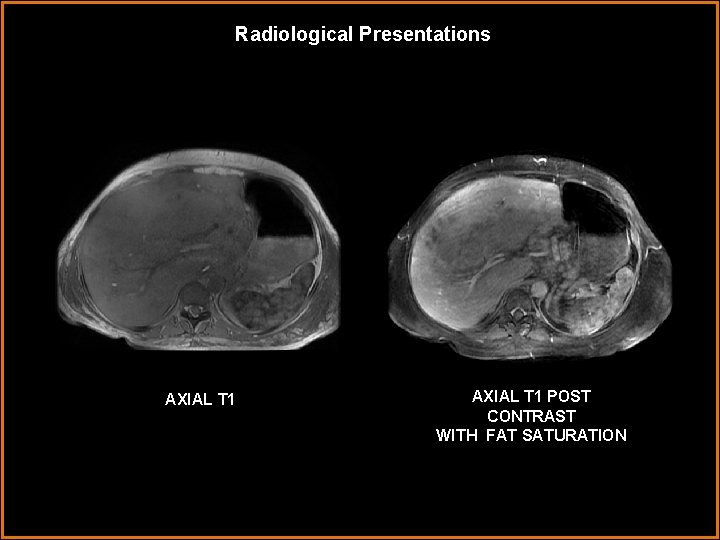
Radiological Presentations AXIAL T 1 POST CONTRAST WITH FAT SATURATION
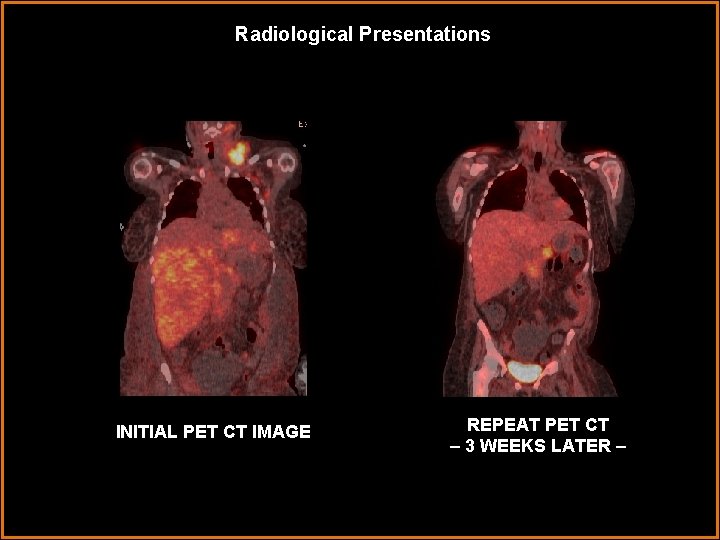
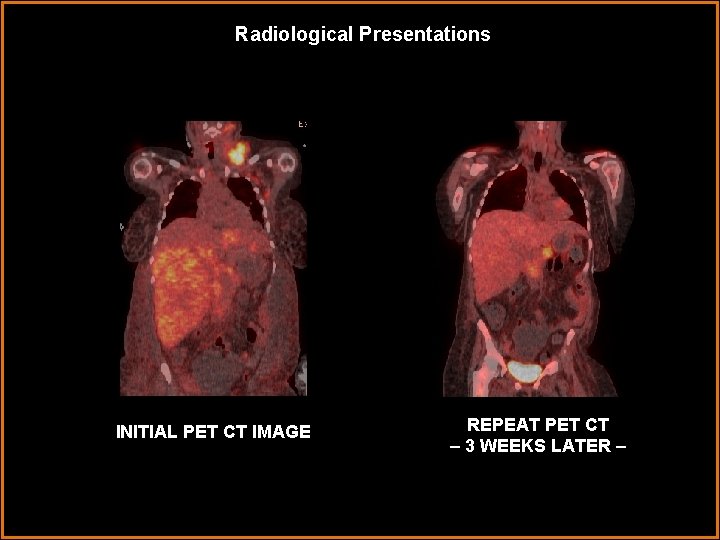
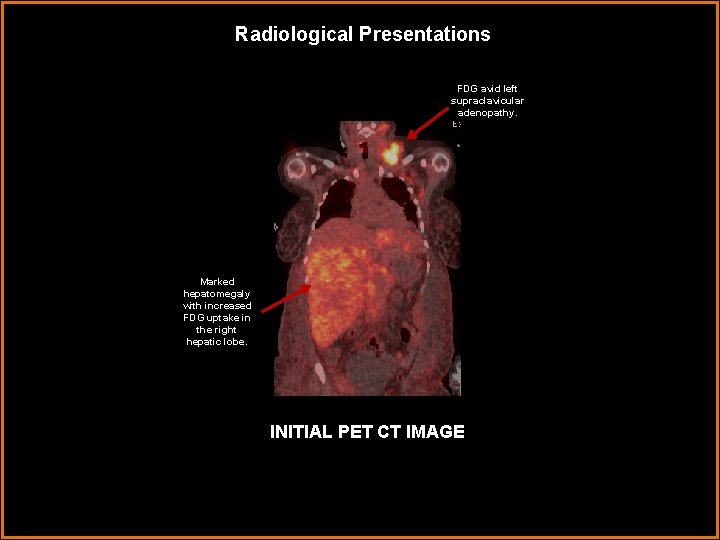
Radiological Presentations INITIAL PET CT IMAGE REPEAT PET CT – 3 WEEKS LATER –
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Inflammatory Pseudotumor • Primary Hepatic Lymphoma • Hepatic Metastases • Cholangiocarcinoma
Findings and Differentials Findings: Axial contrast enhanced CT imaging demonstrates a heterogeneous liver with multiple large confluent hypodense lesions, predominantly involving the right hepatic lobe centrally. There is no apparent neovascularity. Periportal and aortocaval adenopathy is also noted. Poorly defined hypointensities are also present in the spleen. There is no splenomegaly. Axial T 1 and T 2 weighted MRI images demonstrate multifocal areas of patchy T 2 hyper-intensity, predominantly involving the right hepatic lobe and to a lesser extent in the spleen. There is no significant enhancement on post contrast imaging. PET imaging reveals gross hepatomegaly with markedly increased FDG avidity throughout the liver and left supraclavicular lymph nodes. Follow-up PET imaging following treatment demonstrates a dramatic reduction in FDG avidity throughout the liver parenchyma and resolution of the FDG avid left supraclavicular adenopathy. Differentials: • Inflammatory Pseudotumor • Primary Hepatic Lymphoma • Hepatic Metastases • Cholangiocarcinoma
Differentials Inflammatory hepatic pseudotumor characteristically presents as a large solid peripheral mass arising from the right hepatic lobe with low attenuation on contrast enhanced portal venous phase CT imaging. It is commonly T 1 hypointense and T 2 iso/hyperintense to liver parenchyma on MR imaging and virtually indistinguishable from hilar cholangiocarcinoma on PET CT. The majority of hepatic inflammatory pseudotumors occur in children and young adults. Patients typically present with vague abdominal pain, weight loss and abnormal LFTs. Peripheral Cholangiocarcinoma is an infiltrative hepatic mass with capsular retraction. It’s hallmark appearance is that of persistent enhancement on delayed phase CECT. Calcification may be seen in up to 20%. Hepatic metastases are the most common malignant tumor of the liver and classically present as multiple hypo or hyper dense lesions scattered throughout the liver parenchyma in a random distribution. Hypo vascular metastases characteristically present with low density centrally and peripheral rim or target-like enhancement. In contrast, hyper vascular metastases are hyper intense on arterial phase CT and MR. Primary hepatic lymphoma can present as a diffusely infiltrative hypo attenuating mass or as discrete hypo attenuating nodules on CT imaging. The diffuse infiltrative form can be indistinguishable from normal liver parenchyma on T 1 weighted imaging and appears T 2 iso- to slightly hyper intense. There is typically marked FDG avidity on PET imaging and minimal enhancement following contrast administration.
Diagnosis • Primary Hepatic Lymphoma
Discussion Primary Hepatic Lymphoma (PHL) is a extremely rare variant form of non-Hodgkins lymphoma and is defined as lymphoma either confined to the liver or with major liver involvement. According to the Ann Arbor staging system, involvement of the bone marrow, lung or liver constitute Stage IV disease. The prevalence of PHL is 0. 4% among extranodal non-Hodgkin's lymphoma, and 0. 016% among all non-Hodgkin's lymphoma. The vast majority of PHL patients are middle-aged men presenting with hepatomegaly, abdominal pain, nausea and constitutional symptoms. The etiology of PHL remains unclear although there has been a weak association with Hepatitis B, C and Epstein Barr virus, and immuno-compromised states. Cancer complicating pregnancy is a rare occurrence, with an incidence ranging between 0. 07 to 0. 1%. The most common pregnancy associated malignancies include breast and cervical cancer, leukemia, lymphoma and melanoma in decreasing order. The incidence of Hodgkin’s disease diagnosed in pregnancy ranges between 1 in 1000 to 1 in 6000 pregnancies per year, with non Hodgkin’s disease being exceedingly rare. In an effort to avoid excessive fetal exposure, the staging workup is typically limited during pregnancy to include physical exam, serology, bone marrow biopsy and abdominal ultrasound. PHL often presents similarly to hepatoma and metastases from gastro-intestinal (mostly colon) carcinoma, both of which present very similarly and are much more common. Normal levels of the tumor markers, AFP and CEA are found in almost 100% of patients with PHL facilitating the differential diagnosis. Definitive diagnosis is with biopsy, however, pathologic specimen is typically unusual, and initial misdiagnoses, particularly of carcinoma and inflammatory pseudotumor, have been reported quite frequently.

Discussion At pathology, inflammatory pseudotumor is characterized by an intense, predominantly plasma cell infiltrate associated with whorls of myofibroblastic spindle cells, often mimicking lymphoma. These findings may further delay definite diagnosis and treatment and can account for similar imaging findings. In these cases, findings from a thorough history and physical exam should be communicated to the pathologist. Chemotherapy is the main treatment modality although standard treatment can be challenging with severe hepatic dysfunction, and substantial dose reduction may be required. In this case, the patient responded remarkably well both clinically and radiographically to a short term chemotherapy regimen. Mean survival is reported to be 8 -16 months with overall survival of roughly 20%. Studies have shown that there are no significant differences in maternal, pregnancy, or fetal outcomes between pregnant women with Hodgkin’s disease or NHL and matched controls. In most cases, toxic effects were reported when treatment was given during embryogenesis in the first trimester and less often when administered during later trimesters. There has been no evidence suggesting significant teratogenic effect of local treatment with supradiaphragmatic radiotherapy, especially in early trimesters, or chemotherapy administered during the second or third trimester of pregnancy
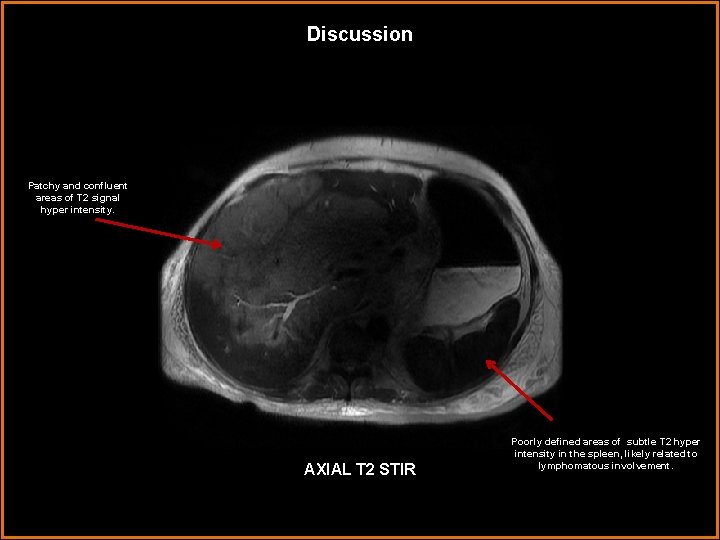
Discussion Patchy and confluent areas of T 2 signal hyper intensity. AXIAL T 2 STIR Poorly defined areas of subtle T 2 hyper intensity in the spleen, likely related to lymphomatous involvement.
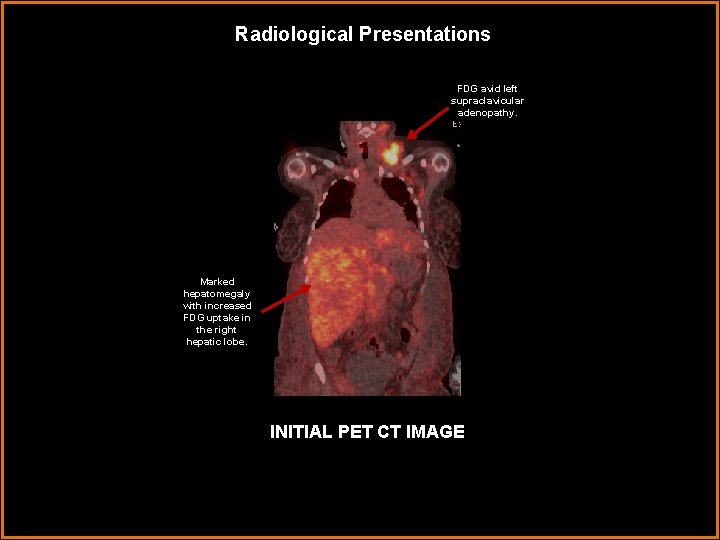
Radiological Presentations FDG avid left supraclavicular adenopathy. Marked hepatomegaly with increased FDG uptake in the right hepatic lobe. INITIAL PET CT IMAGE
References Gazelle, GS, Lee, MJ, Hahn, PF, et al. US, CT, and MRI of primary and secondary liver lymphoma. Journal of Computed Assist Tomography 1994; 18: 412– 415. Guermazi, A. Brice, P. et al. Extranodal Hodgkin Disease: Spectrum of Disease. Radiographics. January 2001, 21, 161 -179. Matano, S, Nakamura, S. et al. Primary hepatic lymphoma in a patient with chronic hepatitis B. American Journal of Gastroenterology. 1998. 93, 2301– 2302. Narla, L. Inflammatory Pseudotumor. Radio. Graphics. May 2003 , 23, 719 -729. Pavlidis, N. Coexistence of Pregnancy and Malignancy. The Oncologist. August 2002, 7: 279 -287 Ryan, J, Straus, DJ, Lange, C, et al. Primary lymphoma of the liver. Cancer 1988; 61: 370– 375.
 Musculoskeletal mri anatomy
Musculoskeletal mri anatomy Aerohive erate
Aerohive erate Radiological dispersal device
Radiological dispersal device Tennessee division of radiological health
Tennessee division of radiological health Center for devices and radiological health
Center for devices and radiological health National radiological emergency preparedness conference
National radiological emergency preparedness conference Mri principal
Mri principal One to many relationship line
One to many relationship line Cardinality and modality
Cardinality and modality Epistemic modality
Epistemic modality Modality in software engineering
Modality in software engineering What is modality in statistics
What is modality in statistics Birafs
Birafs Stefan savi
Stefan savi Deontic and epistemic modality exercises
Deontic and epistemic modality exercises Modality in software engineering
Modality in software engineering