Radiological Category Musculoskeletal Principal Modality 1 MRI Principal
- Slides: 10
Radiological Category: Musculoskeletal Principal Modality (1): MRI Principal Modality (2): None Case Report # 0839 Submitted by: Megan Kalambo, M. D. Faculty reviewer: Larry Kramer, M. D. Date accepted: 01 December 2011
Case History 8 year old with proximal muscle weakness, heliotrope rash on eyelids and orbital puffiness
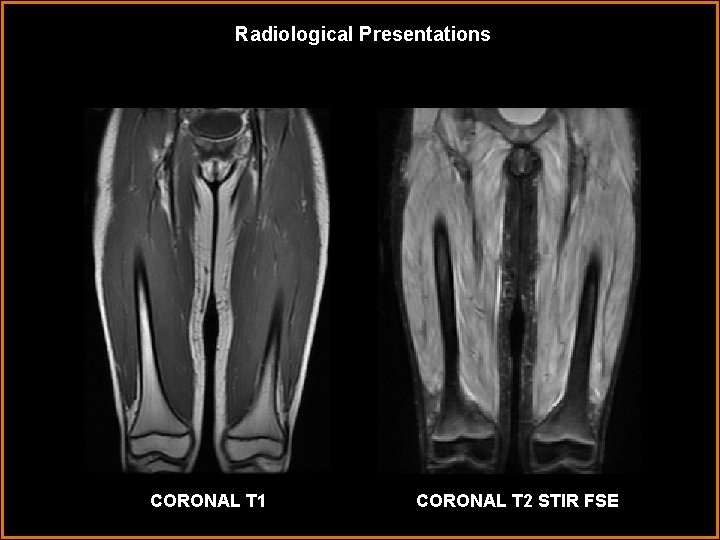
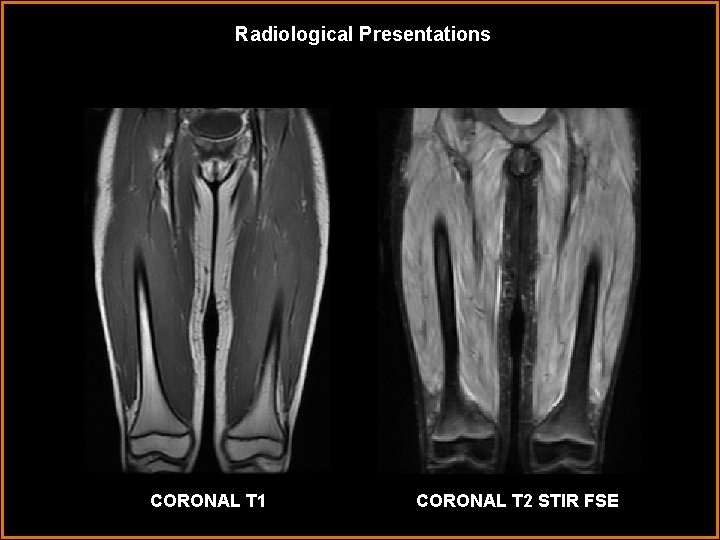
Radiological Presentations CORONAL T 1 CORONAL T 2 STIR FSE
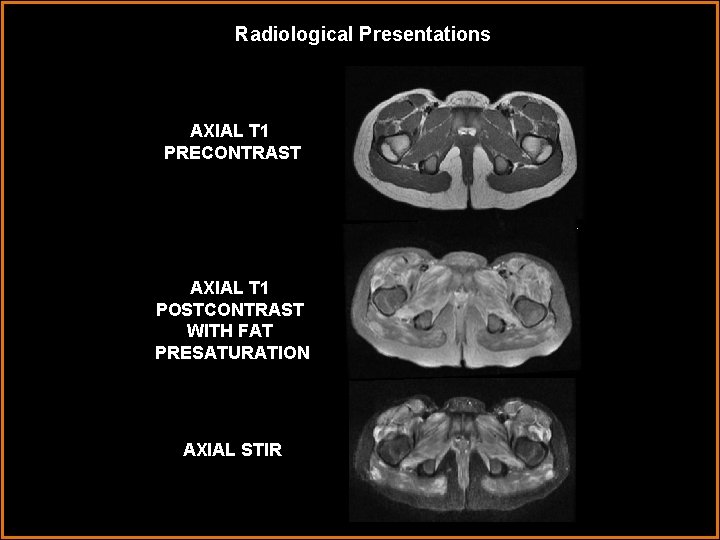
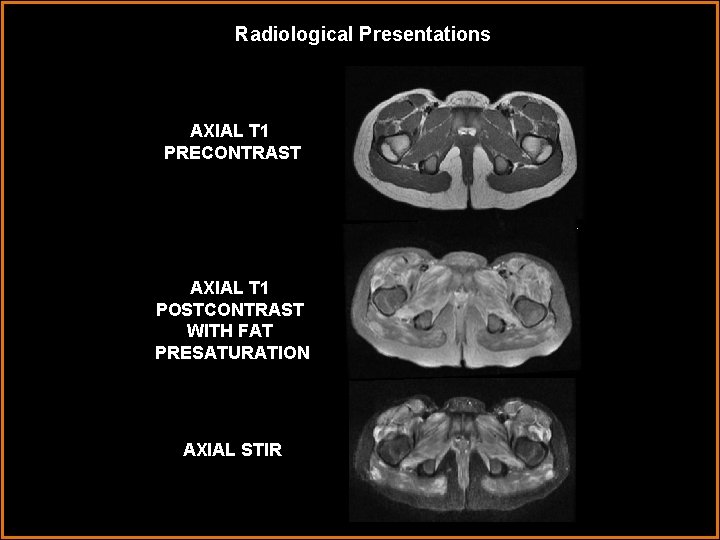
Radiological Presentations AXIAL T 1 PRECONTRAST AXIAL T 1 POSTCONTRAST WITH FAT PRESATURATION AXIAL STIR
Test Your Diagnosis Which one of the following is your choice for the appropriate diagnosis? After your selection, go to next page. • Radiation Therapy • Dermatomyositis • Eosinophilic Fasciitis • Subacute Muscle Denervation
Findings and Differentials Findings: Coronal T 1 imaging demonstrates normal muscle volume without fascial thickening. Coronal T 2 STIR images reveal bilaterally symmetric markedly abnormal T 2 signal hyper intensity within the anterior compartment of the thigh. Axial STIR, T 1 pre and post gadolinium imaging demonstrates abnormal enhancement in the pelvic musculature and to a lesser extent in the gluteal muscles. Differentials: • Radiation Therapy • Dermatomyositis • Eosinophilic Fasciitis • Traumatic Muscle Injury • Subacute Muscle Denervation
Discussion Eosinophilic fasciitis is characterized by abnormal hyperintense T 2 weighted signal and enhancement predominantly within the muscle fascia and to a lesser extent in the adjacent musculature. Thickening of the fascia may be apparent on T 1 weighted imaging. Patients typically have an elevated ESR and peripheral eosinophilia. Patients with dermatomyositis characteristically present with symmetric T 2 hyperintense signal in the musculature of the pelvis and anterior compartment of the thigh. Vastus lateralis and intermedius muscles are most commonly involved. MRI imaging in patients with radiation therapy appear as well delineated, sharp margins of edema corresponding to the radiation field of treatment. Muscle injury typically presents with a contusion and subsequent development of hematoma. These injuries are typically asymmetric and do not follow a muscle distribution. Muscle denervation is typically asymmetric. Imaging reveals T 2 hyperintensity and increased muscle volume in the acute phase with subsequently increased T 1 signal in the chronic phase secondary to fatty replacement. It predominately involves the paraspinal and iliopsoas muscles.
Diagnosis • Juvenile Dermatomyositis
Discussion Juvenile Dermatomyositis (JDMS) is a relatively rare systemic autoimmune vasculopathy with an estimated incidence of 3 cases per 1 million children each year and an average of onset of 7 years. Although uncommon, the disease is classified as the most common of idiopathic inflammatory myopathies in childhood. JDMS is characterized by a pathognomonic skin rash and symmetric weakness in the proximal skeletal muscles predominantly in the neck, abdomen and hip flexors. Rash is the first symptom recognized in roughly 50% of children, presenting as a distinctive pink-purple “heliotrope” rash affecting the face and eyelids. Small bumps, referred to as “Gottron’s papules” may also cover the extensor joint surfaces. Criteria for diagnosis of JDMS include symmetric proximal muscle weakness, the presence of at least one characteristic rash, increased serum muscle enzymes, positive EMG and characteristic changes on muscle biopsy. Patients with muscle weakness and at least two of the additional above-mentioned criteria are considered to have probable JDMS. When diagnosis is in question, particularly in the presence of atypical rash or absence of skin findings, an MRI directed biopsy may be performed. Disease control and overall prognosis is considered good with early initiation of a combination of oral corticosteroids, methotrexate and other immunosuppressive agents. Spontaneous remission has been reported in roughly 20% of cases.
References Feldman BM, Rider LG, Reed AM, Pachman LM (June 2008). "Juvenile Dermatomyositis and other idiopathic inflammatory myopathies of childhood“. Lancet 371 (9631): 2201– 2212. LG Rider and FW Miller, Classification and treatment of the juvenile idiopathic inflammatory myopathies. Rheum Dis Clin North Am, 23 (1997), pp. 619– 655. Mendez EP et al: US incidence of juvenile dermatomyositis, 1995 -1998: results from the National Institute of Arthritis and Musculoskeletal and Skin Diseases Registry. Arthritis Rheum. 49(3): 300 -5, 2003 Moulton SJ et al: Eosinophilic fasciitis: spectrum of MRI findings. AJR Am J Roentgenology. 184(3): 975 -8, 2005 Steiner RM, Glassman L, Schwartz MW, Vanace P. The radiological findings in dermatomyositis of childhood. Radiology 1974; 11: 385 -393.