Primary hyperaldosteronism 2016 8 22 Clinical suspicion of
- Slides: 14
Primary hyperaldosteronism 2016. 8. 22 내과 학생컨퍼런스
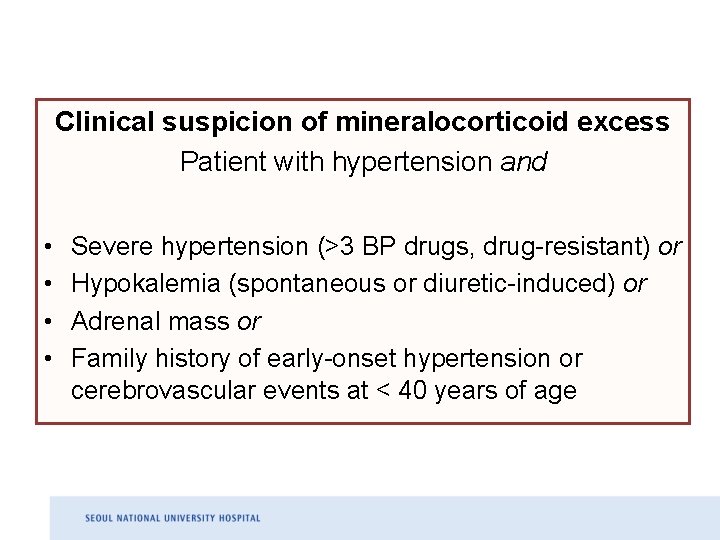
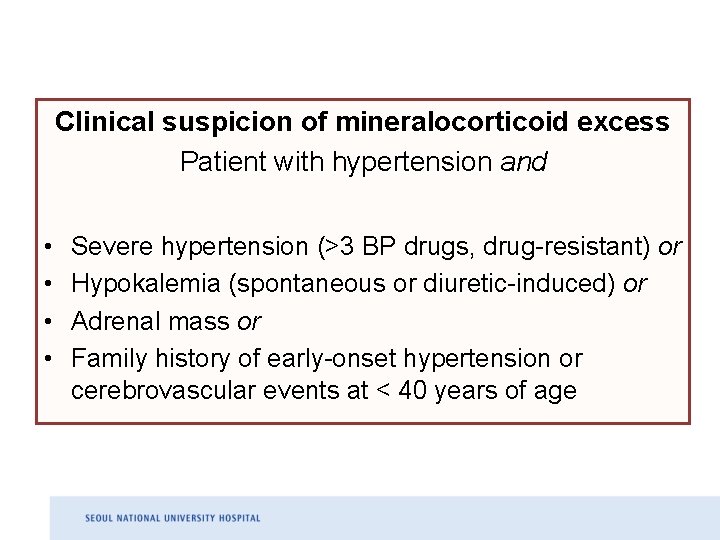
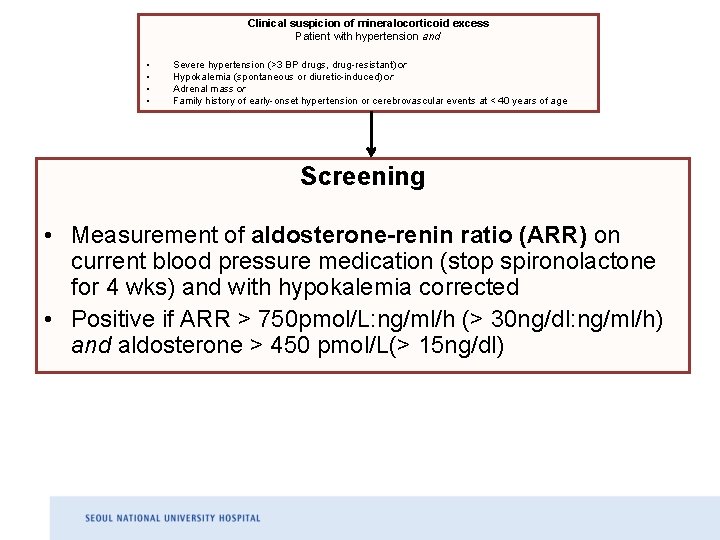
Clinical suspicion of mineralocorticoid excess Patient with hypertension and • • Severe hypertension (>3 BP drugs, drug-resistant) or Hypokalemia (spontaneous or diuretic-induced) or Adrenal mass or Family history of early-onset hypertension or cerebrovascular events at < 40 years of age
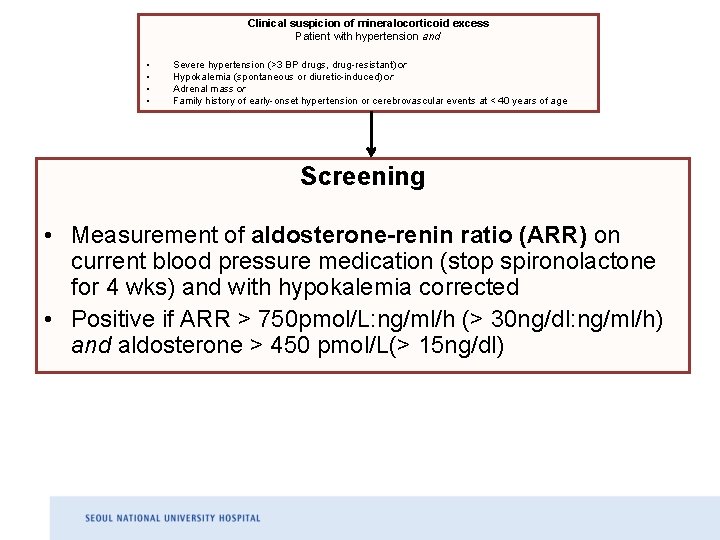
Clinical suspicion of mineralocorticoid excess Patient with hypertension and • • Severe hypertension (>3 BP drugs, drug-resistant) or Hypokalemia (spontaneous or diuretic-induced) or Adrenal mass or Family history of early-onset hypertension or cerebrovascular events at < 40 years of age Screening • Measurement of aldosterone-renin ratio (ARR) on current blood pressure medication (stop spironolactone for 4 wks) and with hypokalemia corrected • Positive if ARR > 750 pmol/L: ng/ml/h (> 30 ng/dl: ng/ml/h) and aldosterone > 450 pmol/L(> 15 ng/dl)
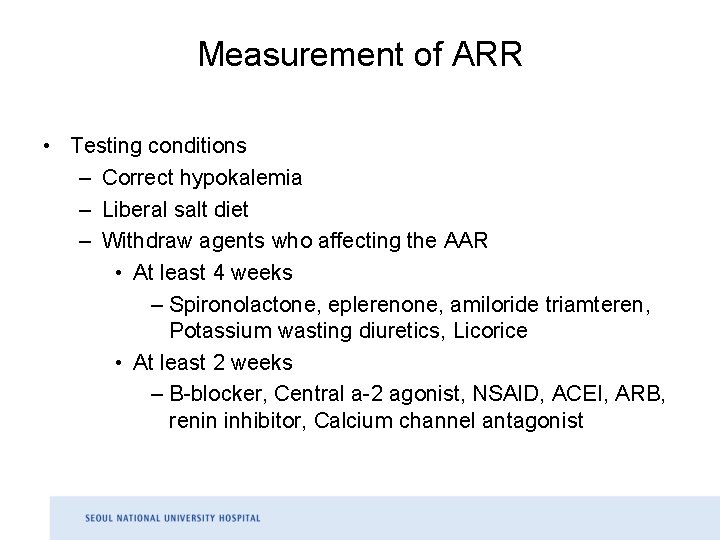
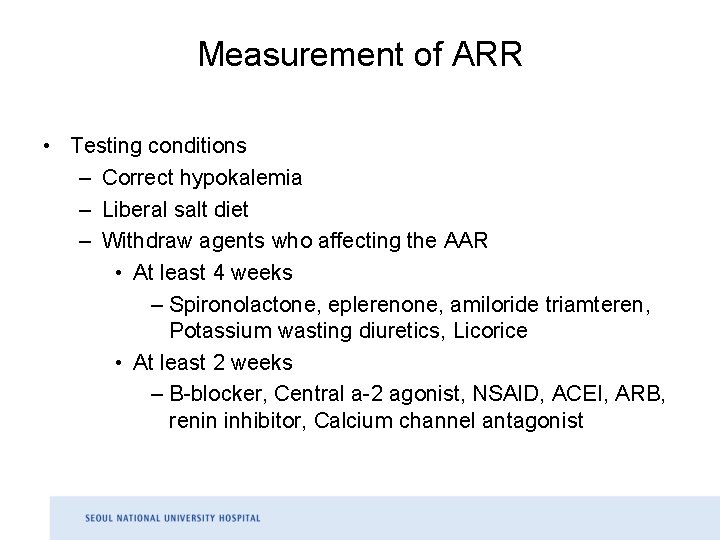
Measurement of ARR • Testing conditions – Correct hypokalemia – Liberal salt diet – Withdraw agents who affecting the AAR • At least 4 weeks – Spironolactone, eplerenone, amiloride triamteren, Potassium wasting diuretics, Licorice • At least 2 weeks – B-blocker, Central a-2 agonist, NSAID, ACEI, ARB, renin inhibitor, Calcium channel antagonist
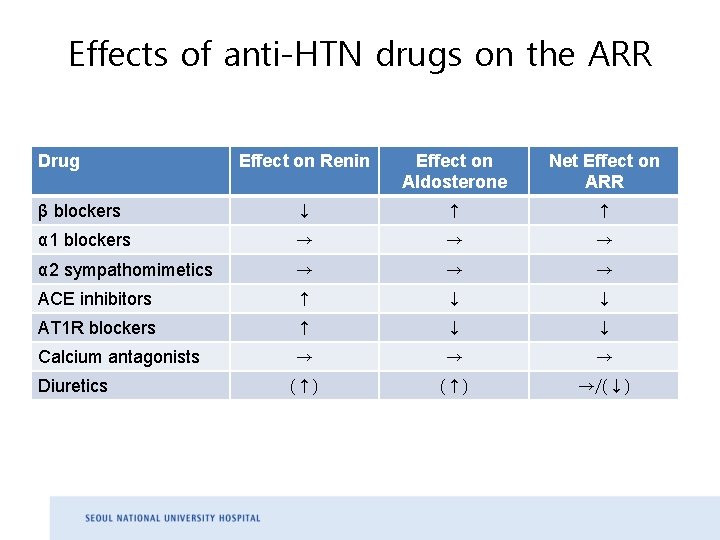
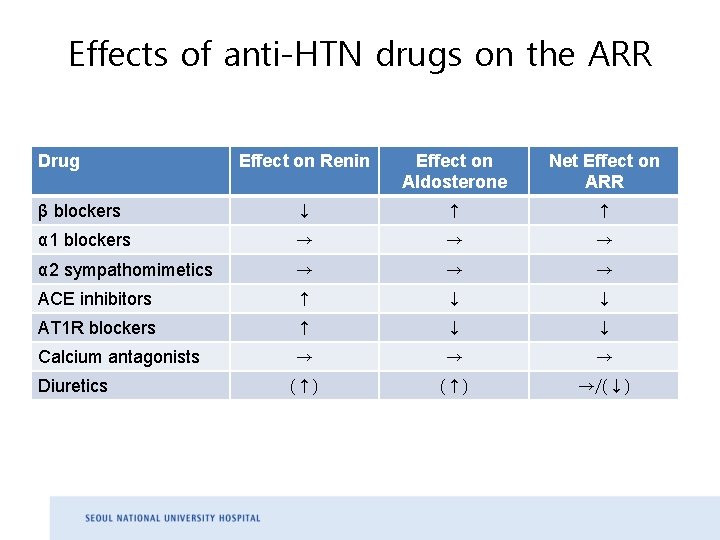
Effects of anti-HTN drugs on the ARR Drug Effect on Renin Effect on Aldosterone Net Effect on ARR β blockers ↓ ↑ ↑ α 1 blockers → → → α 2 sympathomimetics → → → ACE inhibitors ↑ ↓ ↓ AT 1 R blockers ↑ ↓ ↓ Calcium antagonists → → → (↑) →/(↓) Diuretics
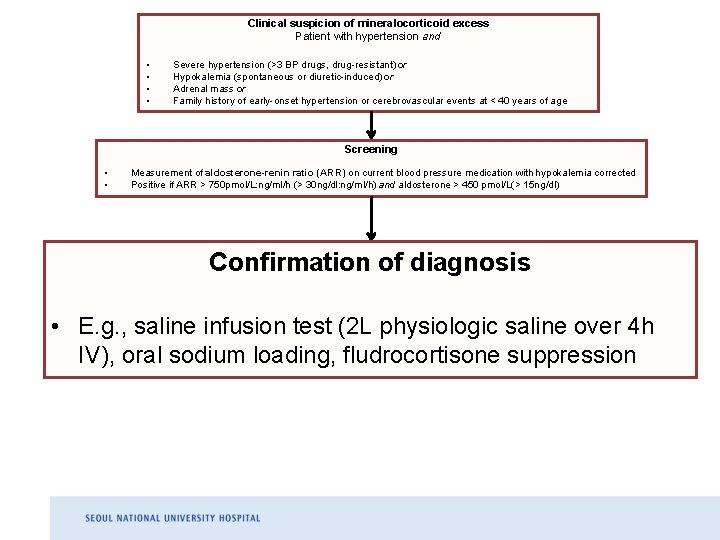
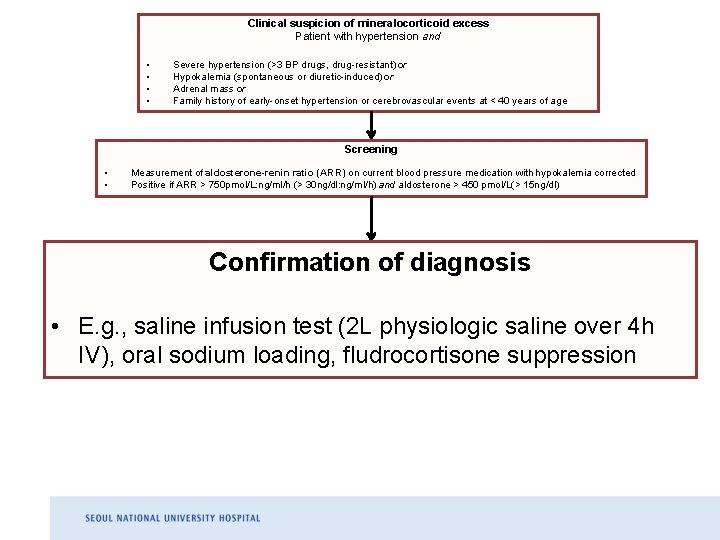
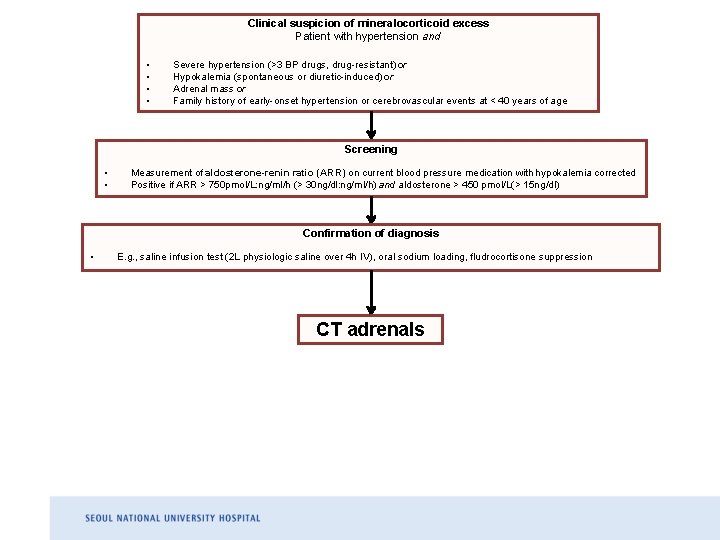
Clinical suspicion of mineralocorticoid excess Patient with hypertension and • • Severe hypertension (>3 BP drugs, drug-resistant) or Hypokalemia (spontaneous or diuretic-induced) or Adrenal mass or Family history of early-onset hypertension or cerebrovascular events at < 40 years of age Screening • • Measurement of aldosterone-renin ratio (ARR) on current blood pressure medication with hypokalemia corrected Positive if ARR > 750 pmol/L: ng/ml/h (> 30 ng/dl: ng/ml/h) and aldosterone > 450 pmol/L(> 15 ng/dl) Confirmation of diagnosis • E. g. , saline infusion test (2 L physiologic saline over 4 h IV), oral sodium loading, fludrocortisone suppression
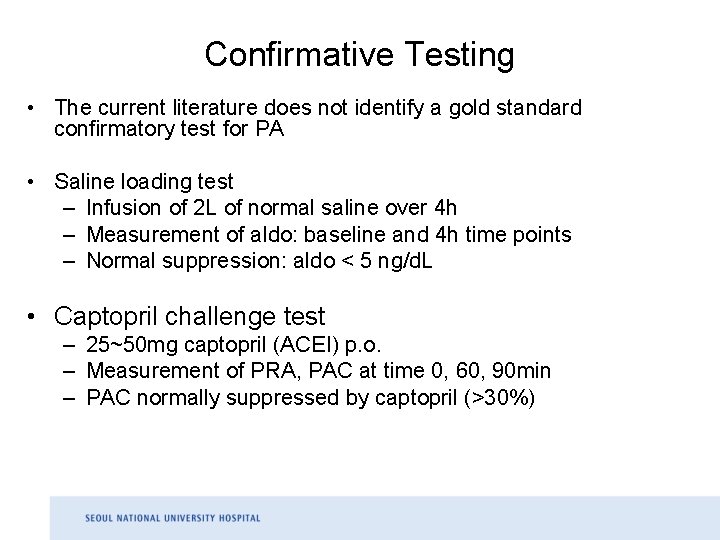
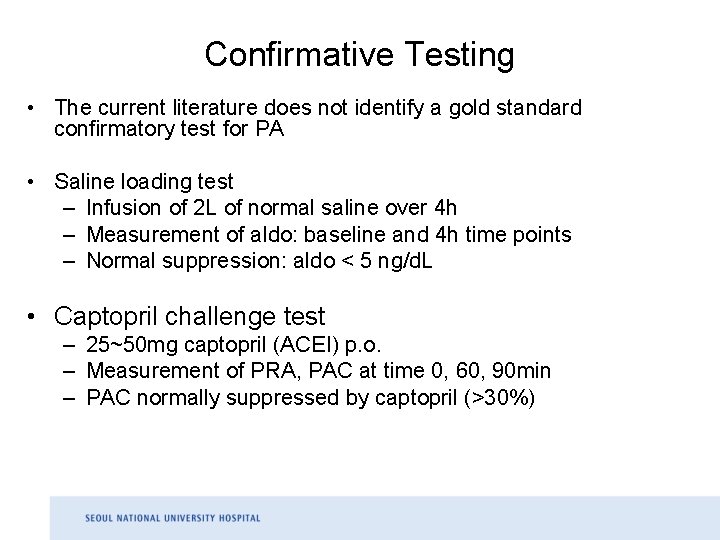
Confirmative Testing • The current literature does not identify a gold standard confirmatory test for PA • Saline loading test – Infusion of 2 L of normal saline over 4 h – Measurement of aldo: baseline and 4 h time points – Normal suppression: aldo < 5 ng/d. L • Captopril challenge test – 25~50 mg captopril (ACEI) p. o. – Measurement of PRA, PAC at time 0, 60, 90 min – PAC normally suppressed by captopril (>30%)
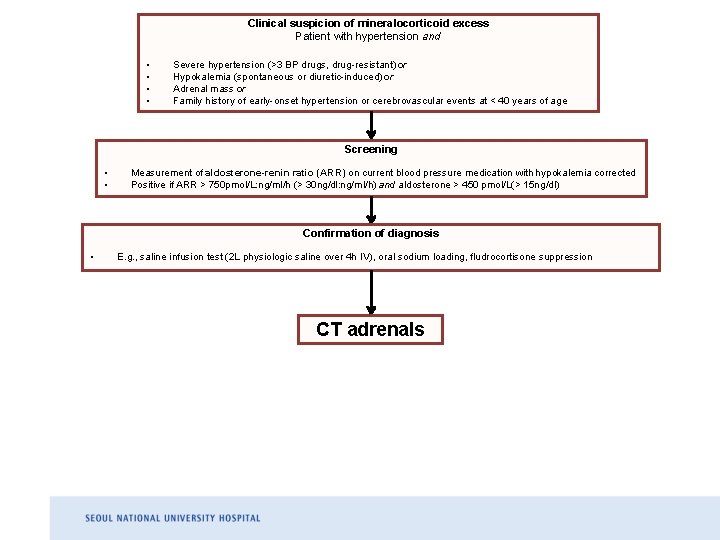
Clinical suspicion of mineralocorticoid excess Patient with hypertension and • • Severe hypertension (>3 BP drugs, drug-resistant) or Hypokalemia (spontaneous or diuretic-induced) or Adrenal mass or Family history of early-onset hypertension or cerebrovascular events at < 40 years of age Screening • • Measurement of aldosterone-renin ratio (ARR) on current blood pressure medication with hypokalemia corrected Positive if ARR > 750 pmol/L: ng/ml/h (> 30 ng/dl: ng/ml/h) and aldosterone > 450 pmol/L(> 15 ng/dl) Confirmation of diagnosis • E. g. , saline infusion test (2 L physiologic saline over 4 h IV), oral sodium loading, fludrocortisone suppression CT adrenals
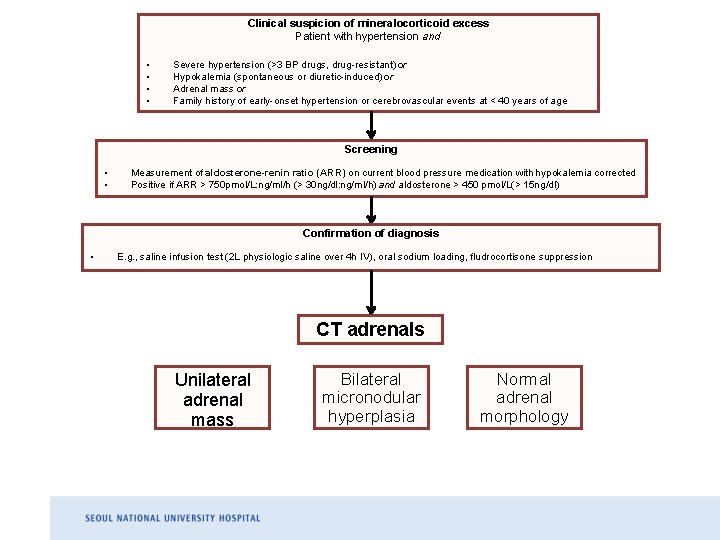
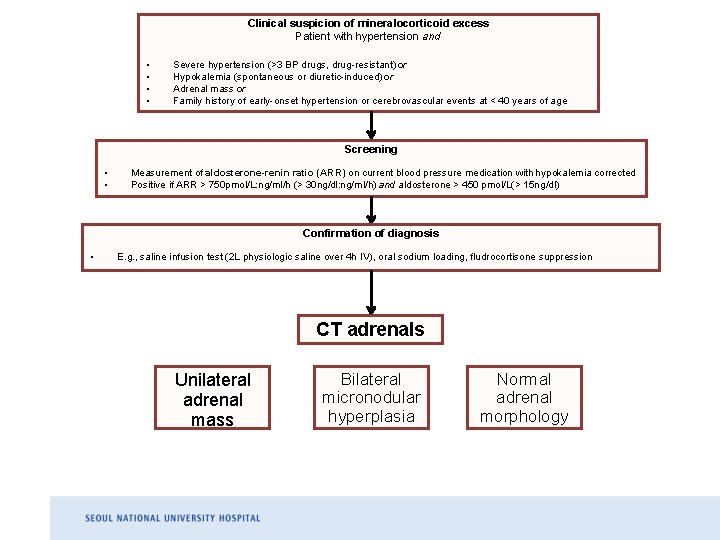
Clinical suspicion of mineralocorticoid excess Patient with hypertension and • • Severe hypertension (>3 BP drugs, drug-resistant) or Hypokalemia (spontaneous or diuretic-induced) or Adrenal mass or Family history of early-onset hypertension or cerebrovascular events at < 40 years of age Screening • • Measurement of aldosterone-renin ratio (ARR) on current blood pressure medication with hypokalemia corrected Positive if ARR > 750 pmol/L: ng/ml/h (> 30 ng/dl: ng/ml/h) and aldosterone > 450 pmol/L(> 15 ng/dl) Confirmation of diagnosis • E. g. , saline infusion test (2 L physiologic saline over 4 h IV), oral sodium loading, fludrocortisone suppression CT adrenals Unilateral adrenal mass Bilateral micronodular hyperplasia Normal adrenal morphology
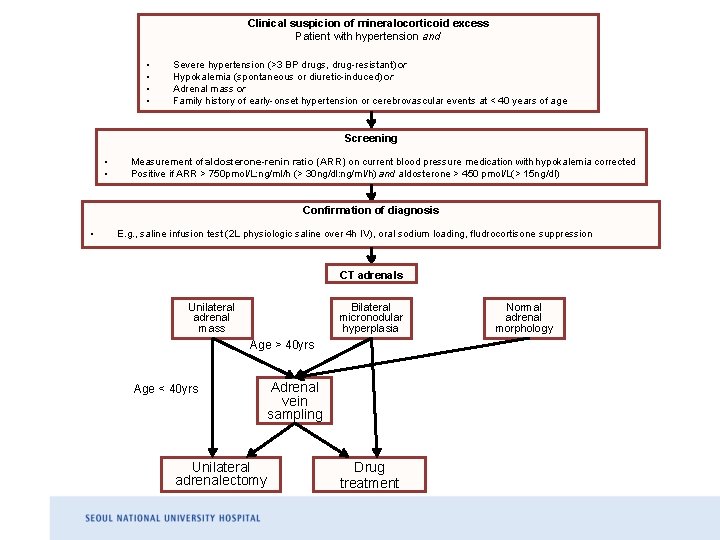
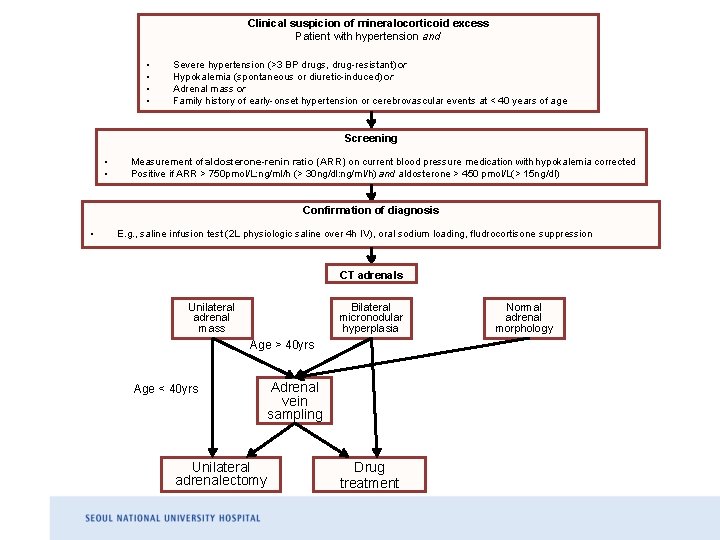
Clinical suspicion of mineralocorticoid excess Patient with hypertension and • • Severe hypertension (>3 BP drugs, drug-resistant) or Hypokalemia (spontaneous or diuretic-induced) or Adrenal mass or Family history of early-onset hypertension or cerebrovascular events at < 40 years of age Screening • • Measurement of aldosterone-renin ratio (ARR) on current blood pressure medication with hypokalemia corrected Positive if ARR > 750 pmol/L: ng/ml/h (> 30 ng/dl: ng/ml/h) and aldosterone > 450 pmol/L(> 15 ng/dl) Confirmation of diagnosis • E. g. , saline infusion test (2 L physiologic saline over 4 h IV), oral sodium loading, fludrocortisone suppression CT adrenals Unilateral adrenal mass Bilateral micronodular hyperplasia Age > 40 yrs Age < 40 yrs Adrenal vein sampling Unilateral adrenalectomy Drug treatment Normal adrenal morphology
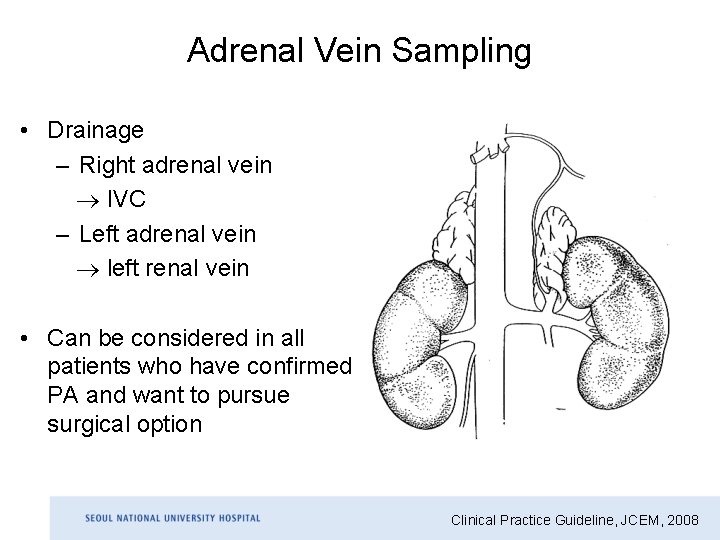
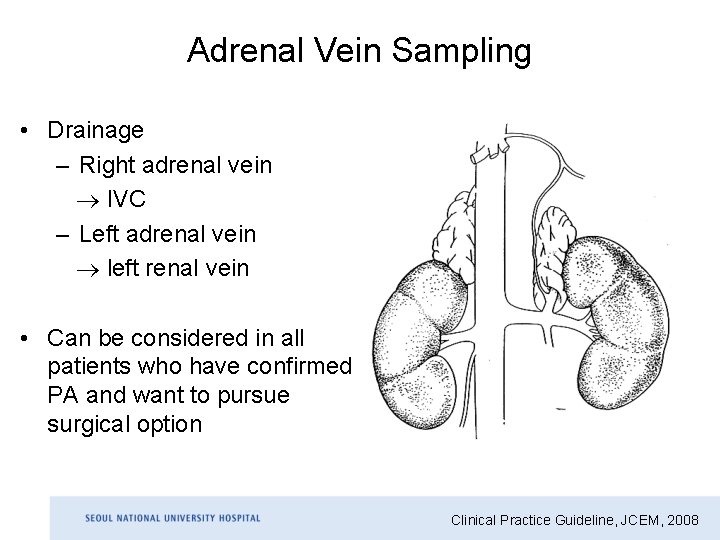
Adrenal Vein Sampling • Drainage – Right adrenal vein IVC – Left adrenal vein left renal vein • Can be considered in all patients who have confirmed PA and want to pursue surgical option Clinical Practice Guideline, JCEM, 2008
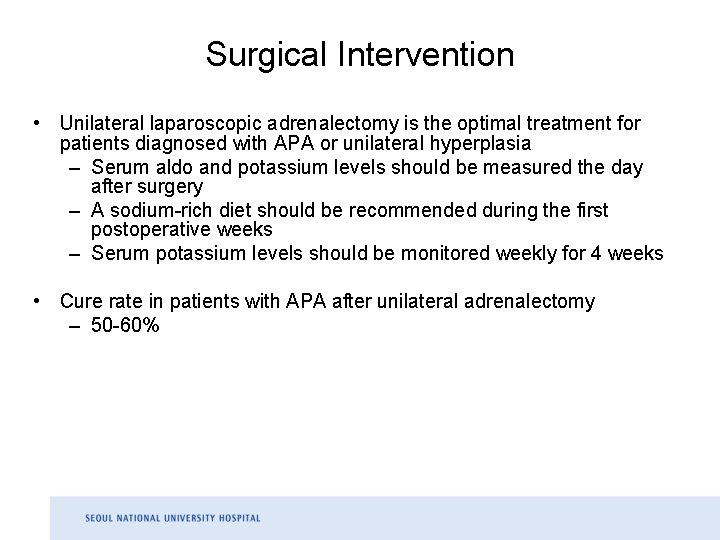
Surgical Intervention • Unilateral laparoscopic adrenalectomy is the optimal treatment for patients diagnosed with APA or unilateral hyperplasia – Serum aldo and potassium levels should be measured the day after surgery – A sodium-rich diet should be recommended during the first postoperative weeks – Serum potassium levels should be monitored weekly for 4 weeks • Cure rate in patients with APA after unilateral adrenalectomy – 50 -60%
Factors Associated with Resolution of Hypertension in the Postoperative Period • Lack of a family history of hypertension • Pre operative use of no more than two antihypertensive drugs • Young age • Short duration of hypertension (<5 years) • Positive response to spironolactone • High pre operative ARR • high urinary aldosterone excretion
Pharmacological Therapy • Patients with IHA, and those with APA or unilateral hyperplasia who are not candidates for or who decline surgery • MR antagonists – Effective at controlling BP and to provide BP-independent target organ protection – Spironolactone: Primary agent – Eplerenone: Alternative • Epithelial sodium channel antagonists – Amiloride: Potassium sparing diuretic, No beneficial effects on endothelial function • Low dose glucocorticoid or additional MR antagonists for GRA • Other hypertensive agents as 3 rd or 4 th line agents for adequate BP control
 Hyperaldosteronism
Hyperaldosteronism Duties of wife in islam
Duties of wife in islam Suspicion de phlébite
Suspicion de phlébite Fta reasonable suspicion training
Fta reasonable suspicion training Torch infection
Torch infection Quotes about elizabeth proctor being honest
Quotes about elizabeth proctor being honest Different bones
Different bones Magenta cyan and yellow are the ____ color. *
Magenta cyan and yellow are the ____ color. * The prodigal elizabeth bishop
The prodigal elizabeth bishop Article le monde 2016
Article le monde 2016 Advocaat petitat
Advocaat petitat Opsionel
Opsionel Nys ela 2015
Nys ela 2015 Cad 2016
Cad 2016 Programowanie żywieniowe we wczesnym okresie życia
Programowanie żywieniowe we wczesnym okresie życia